Clinical Decision Support Systems in Indian Healthcare Settings: Benefits, Barriers, and Future Implications
Abstract
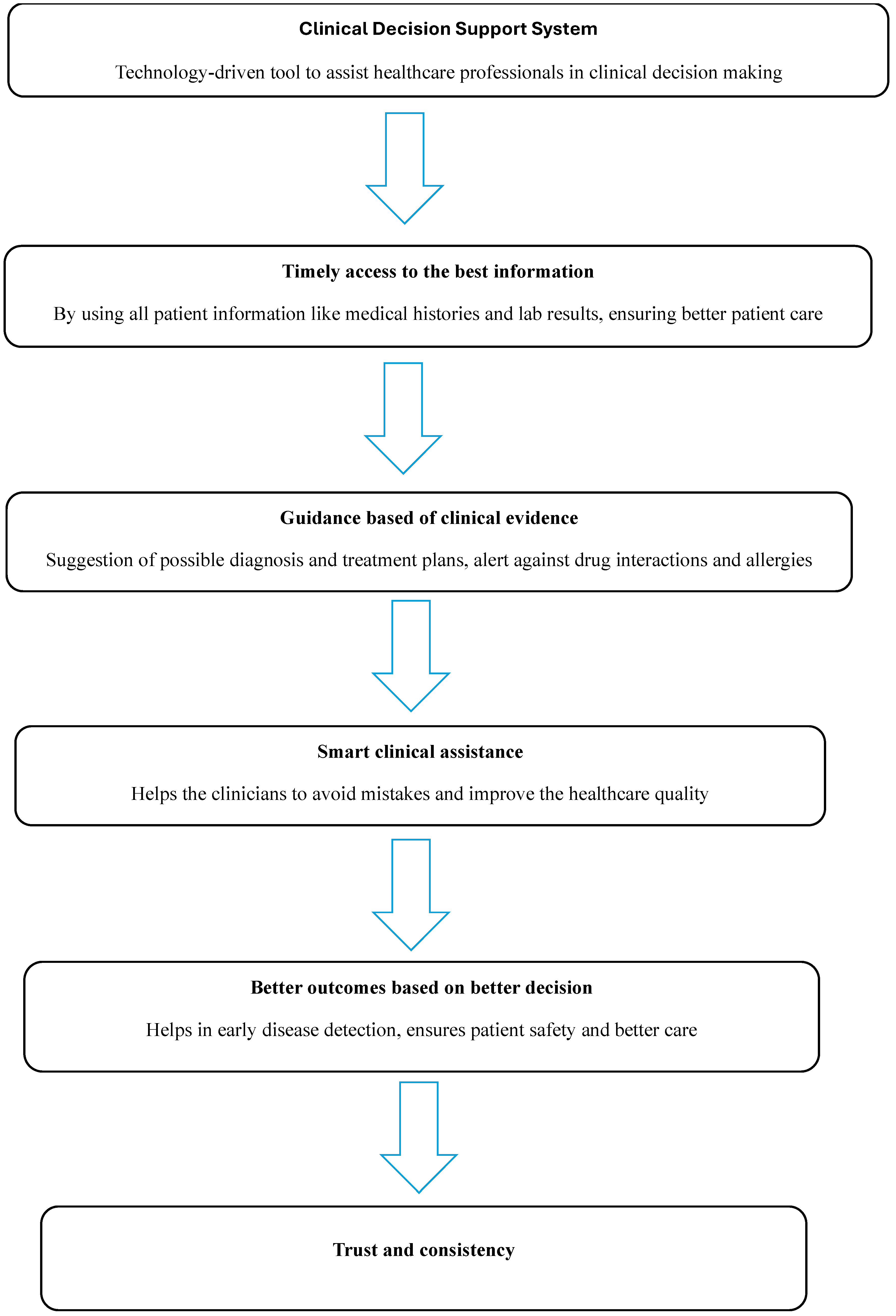
1. Introduction
2. Methodology
3. Benefits of CDSSs in Patient Care
4. Importance of CDSSs in Indian Healthcare
5. Adoption of CDSSs in Indian Healthcare Settings
6. Challenges and Barriers to CDSS Implementation in India
6.1. Technological Challenges
6.2. Financial Challenges
6.3. Data Quality and Availability
6.4. Regulatory and Legal Barriers
6.5. Cultural, Professional, and Organizational Barriers
6.6. Integration with Electronic Health Records
7. Suggestions for Improving CDSS Adoption in India
7.1. Strengthening Technological Infrastructure
7.2. Financial and Policy Interventions
7.3. Regulatory and Legal Reforms
7.4. Capacity Building and Training
7.5. Strategic and Organizational Change
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADRs | Adverse drug reactions |
| AI | Artificial intelligence |
| AIIMS | All India Institute of Medical Sciences |
| AIMS | Amrita Institute of Medical Sciences |
| ASP | Antimicrobial stewardship program |
| CDSS | Clinical Decision Support System |
| CDT | Clinical decision trees |
| COPD | Chronic obstructive pulmonary disorder |
| DI | Drug interactions |
| DRPs | Drug-related problems |
| HER | Electronic health records |
| HCG | HealthCare Global Ltd. |
| HIT | Health information technology |
| HTN | Hypertension |
| I-TREC | The Integrated Tracking, Referral, Electronic Decision Support, and Care Coordination |
| KIMS | Krishna institute of Medical Sciences |
| LMICs | Low-and middle-income countries |
| MDR | Multidrug resistant |
| NICU | Neonatal intensive care unit |
| PGIMER | Postgraduate Institute of Medical Education and Research |
| PICO | Patient, Intervention, Comparison, and Outcome |
| ROI | Return on investment |
| UT | Union Territory |
References
- Cassen, R.; Visaria, P. India: Looking ahead to one and a half billion people. BMJ 1999, 319, 995–997. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Department of Economic and Social Affairs, United Nations. Available online: https://www.un.org/en/desa/world-population-projected-reach-98-billion-2050-and-112-billion-2100 (accessed on 12 August 2025).
- Meunier, P.Y.; Raynaud, C.; Guimaraes, E.; Gueyffier, F.; Letrilliart, L. Barriers and Facilitators to the Use of Clinical Decision Support Systems in Primary Care: A Mixed-Methods Systematic Review. Ann. Fam. Med. 2023, 21, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef]
- Adler-Milstein, J.; Bates, D.W. Paperless healthcare: Progress and challenges of an IT-enabled healthcare system. Bus. Horiz. 2010, 53, 119–130. [Google Scholar] [CrossRef]
- Sheikh, A.; Anderson, M.; Albala, S.; Casadei, B.; Franklin, B.D.; Richards, M.; Taylor, D.; Tibble, H.; Mossialos, E. Health information technology and digital innovation for national learning health and care systems. Lancet Digit. Health 2021, 3, e383–e396. [Google Scholar] [CrossRef]
- Kwan, J.L.; Lo, L.; Ferguson, J.; Goldberg, H.; Diaz-Martinez, J.P.; Tomlinson, G.; Grimshaw, J.M.; Shojania, K.G. Computerised clinical decision support systems and absolute improvements in care: Meta-analysis of controlled clinical trials. BMJ 2020, 370, m3216. [Google Scholar] [CrossRef]
- Chen, Z.; Liang, N.; Zhang, H.; Li, H.; Yang, Y.; Zong, X.; Chen, Y.; Wang, Y.; Shi, N. Harnessing the power of clinical decision support systems: Challenges and opportunities. Open Heart 2023, 10, e002432. [Google Scholar] [CrossRef]
- Dhagarra, D.; Goswami, M.; Kumar, G. Impact of Trust and Privacy Concerns on Technology Acceptance in Healthcare: An Indian Perspective. Int. J. Med. Inform. 2020, 141, 104164. [Google Scholar] [CrossRef]
- Kumar, P.; Dwivedi, Y.K.; Anand, A. Responsible Artificial Intelligence (AI) for Value Formation and Market Performance in Healthcare: The Mediating Role of Patient’s Cognitive Engagement. Inf. Syst. Front. 2023, 25, 2197–2220. [Google Scholar] [CrossRef]
- Fujimori, R.; Liu, K.; Soeno, S.; Naraba, H.; Ogura, K.; Hara, K.; Sonoo, T.; Ogura, T.; Nakamura, K.; Goto, T. Acceptance, Barriers, and Facilitators to Implementing Artificial Intelligence-Based Decision Support Systems in Emergency Departments: Quantitative and Qualitative Evaluation. JMIR Form. Res. 2022, 6, e36501. [Google Scholar] [CrossRef]
- Over 790 mn ABHA Accounts Created, 650 mn Health Records Linked: Centre|India News—Business Standard. 2025. Available online: https://www.business-standard.com/india-news/over-790-mn-abha-accounts-created-650-mn-health-records-linked-centre-125080101224_1.html (accessed on 12 August 2025).
- Grechuta, K.; Shokouh, P.; Alhussein, A.; Müller-Wieland, D.; Meyerhoff, J.; Gilbert, J.; Purushotham, S.; Rolland, C. Benefits of Clinical Decision Support Systems for the Management of Noncommunicable Chronic Diseases: Targeted Literature Review. Interact. J. Med. Res. 2024, 13, e58036. [Google Scholar] [CrossRef]
- Newton, N.; Bamgboje-Ayodele, A.; Forsyth, R.; Tariq, A.; Baysari, M.T. A systematic review of clinicians’ acceptance and use of clinical decision support systems over time. npj Digit. Med. 2025, 8, 309. [Google Scholar] [CrossRef]
- Evans, R.P.; Bryant, L.D.; Russell, G.; Absolom, K. Trust acceptability of data-driven clinical recommendations in everyday practice: A scoping review. Int. J. Med. Inform. 2024, 183, 105342. [Google Scholar] [CrossRef]
- Kux, B.R.; Majeed, R.W.; Ahlbrandt, J.; Röhrig, R. Factors Influencing the Implementation Distribution of Clinical Decision Support Systems (CDSS). In German Medical Data Sciences: Visions and Bridges; IOS Press: Amsterdam, The Netherlands, 2017; Volume 243, pp. 127–131. [Google Scholar]
- Bayor, A.A.; Li, J.; Yang, I.A.; Varnfield, M. Designing Clinical Decision Support Systems (CDSS)-AUser-Centered Lens of the Design Characteristics Challenges Implications: Systematic Review. J. Med. Internet Res. 2025, 27, e63733. [Google Scholar] [CrossRef]
- Chen, W.; Howard, K.; Gorham, G.; O’bRyan, C.M.; Coffey, P.; Balasubramanya, B.; Abeyaratne, A.; Cass, A. Design, effectiveness, and economic outcomes of contemporary chronic disease clinical decision support systems: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2022, 29, 1757–1772. [Google Scholar] [CrossRef] [PubMed]
- White, N.M.; E Carter, H.; Kularatna, S.; Borg, D.N.; Brain, D.C.; Tariq, A.; Abell, B.; Blythe, R.; McPhail, S.M. Evaluating the costs and consequences of computerized clinical decision support systems in hospitals: A scoping review and recommendations for future practice. J. Am. Med. Inform. Assoc. 2023, 30, 1205–1218. [Google Scholar] [CrossRef] [PubMed]
- Ji, M.; Yu, G.; Xi, H.; Xu, T.; Qin, Y. Measures of success of computerized clinical decision support systems: An overview of systematic reviews. Health Policy Technol. 2021, 10, 196–208. [Google Scholar] [CrossRef]
- Jones, C.; Thornton, J.; Wyatt, J.C. Enhancing trust in clinical decision support systems: A framework for developers. BMJ Health Care Inform. 2021, 28, e100247. [Google Scholar] [CrossRef]
- Jacob, V.; Thota, A.B.; Chattopadhyay, S.K.; Njie, G.J.; Proia, K.K.; Hopkins, D.P.; Ross, M.N.; Pronk, N.P.; Clymer, J.M. Cost and economic benefit of clinical decision support systems for cardiovascular disease prevention: A community guide systematic review. J. Am. Med. Inform. Assoc. 2017, 24, 669–676. [Google Scholar] [CrossRef]
- Lewkowicz, D.; Wohlbrandt, A.; Boettinger, E. Economic impact of clinical decision support interventions based on electronic health records. BMC Health Serv. Res. 2020, 20, 871. [Google Scholar] [CrossRef]
- Agarwal, S.; Glenton, C.; Tamrat, T.; Henschke, N.; Maayan, N.; Fønhus, M.S.; Mehl, G.L.; Lewin, S. Decision-support tools via mobile devices to improve quality of care in primary healthcare settings. Cochrane Database Syst. Rev. 2021, 7, Cd012944. [Google Scholar] [CrossRef] [PubMed]
- Zaman, S.B.; Silva, N.D.; Goh, T.Y.; Evans, R.G.; Singh, R.; Singh, R.; Singh, A.; Singh, P.; Thrift, A.G. Design and development of a clinical decision support system for community health workers to support early detection and management of non-communicable disease. BMJ Innov. 2023, 9, 49–56. [Google Scholar] [CrossRef]
- Prakash, A.V.; Das, S. Medical practitioner's adoption of intelligent clinical diagnostic decision support systems: A mixed-methods study. Inf. Manag. 2021, 58, 103524. [Google Scholar] [CrossRef]
- Zapata, T.; Buchan, J.; Tangcharoensathien, V.; Meliala, A.; Karunathilake, I.; Tin, N.; Nandi, S.; Tobgay, T.; Noree, T. Rural Retention Strategies in the South-East Asia Region: Evidence to Guide Effective Implementation. Bull. World Health Organ. 2020, 98, 815–817. [Google Scholar] [CrossRef]
- Sriram, V.; Hariyani, S.; Lalani, U.; Buddhiraju, R.T.; Pandey, P.; Bennett, S. Stakeholder perspectives on proposed policies to improve distribution and retention of doctors in rural areas of Uttar Pradesh, India. BMC Health Serv. Res. 2021, 21, 1027. [Google Scholar] [CrossRef]
- Jindal, D.; Sharma, H.; Gupta, Y.; Ajay, V.S.; Roy, A.; Sharma, R.; Ali, M.; Jarhyan, P.; Gupta, P.; Venkateshmurthy, N.S.; et al. Improving care for hypertension and diabetes in india by addition of clinical decision support system and task shifting in the national NCD program: I-TREC model of care. BMC Health Serv. Res. 2022, 22, 688. [Google Scholar] [CrossRef]
- Clinical Decision Support System for Healthcare Providers. Available online: https://abdm.gov.in:8081/uploads/ABDM_CDSS_Brochure_Doctors_3b3d808b52.pdf (accessed on 12 August 2025).
- Huang, Z.; George, M.M.; Tan, Y.-R.; Natarajan, K.; Devasagayam, E.; Tay, E.; Manesh, A.; Varghese, G.M.; Abraham, O.C.; Zachariah, A.; et al. Are physicians ready for precision antibiotic prescribing? A qualitative analysis of the acceptance of artificial intelligence-enabled clinical decision support systems in India and Singapore. J. Glob. Antimicrob. Resist. 2023, 35, 76–85. [Google Scholar] [CrossRef]
- National Health Authority. Digital Health Progress Report 2023. Available online: https://abdm.gov.in (accessed on 12 August 2025).
- Misro, A.; Mehta, A.; Whittington, P.; Dogan, H.; Mishra, N.; Kadoglou, N.; Theivacumar, S. From Concept to Reality: Examining India’s Clinical Decision Support System (CDSS) Challenges & Opportunities. medRxiv 2023. [Google Scholar] [CrossRef]
- Chandwani, R.; Edacherian, S.; Sud, M. National Digital Infrastructure and India’s Healthcare Sector: Physician’s Perspectives. Qual. Rep. 2023, 28, 360–386. [Google Scholar] [CrossRef]
- Laka, M.; Carter, D.; Milazzo, A.; Merlin, T. Challenges and opportunities in implementing clinical decision support systems (CDSS) at scale: Interviews with Australian policymakers. Health Policy Technol. 2022, 11, 100652. [Google Scholar] [CrossRef]
- Ford, E.; Edelman, N.; Somers, L.; Shrewsbury, D.; Levy, M.L.; van Marwijk, H.; Curcin, V.; Porat, T. Barriers and facilitators to the adoption of electronic clinical decision support systems: A qualitative interview study with UK general practitioners. BMC Med. Inform. Decis. Mak. 2021, 21, 193. [Google Scholar] [CrossRef]
- Papadopoulos, P.; Soflano, M.; Chaudy, Y.; Adejo, W.; Connolly, T.M. A systematic review of technologies and standards used in the development of rule-based clinical decision support systems. Health Technol. 2022, 12, 713–727. [Google Scholar] [CrossRef]
- Ayaz, M.; Pasha, M.F.; Alzahrani, M.Y.; Budiarto, R.; Stiawan, D. The Fast Health Interoperability Resources (FHIR) standard: Systematic literature review of implementations, applications, challenges and opportunities. JMIR Med. Inform. 2021, 9, e21929. [Google Scholar] [CrossRef] [PubMed]
- Stipelman, C.H.; Kukhareva, P.V.; Trepman, E.; Nguyen, Q.-T.; Valdez, L.; Kenost, C.; Hightower, M.; Kawamoto, K. Electronic health record-integrated clinical decision support for clinicians serving populations facing health care disparities: Literature review. Yearb. Med. Inform. 2022, 31, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Mokashi, T.; Nair, A.; Chokshi, M. Mapping Healthcare Data Sources in India. J. Health Manag. 2022, 24, 146–159. [Google Scholar] [CrossRef]
- Pai, M.M.; Ganiga, R.; Pai, R.M.; Sinha, R.K. Standard electronic health record (EHR) framework for Indian healthcare system. Health Serv. Outcomes Res. Methodol. 2021, 21, 339–362. [Google Scholar] [CrossRef]
- Kapur, G.; Hussain, M.A. Building Intelligent Electronic Health Record System for India: Challenges and Opportunities. In International Conference on Research into Design; Springer: Berlin/Heidelberg, Germany, 2023; pp. 405–417. [Google Scholar] [CrossRef]
- Suhaj, A.; Manu, M.K.; Unnikrishnan, M.K.; Vijayanarayana, K.; Mallikarjuna Rao, C. Effectiveness of clinical pharmacist intervention on health-related quality of life in chronic obstructive pulmonary disorder patients—A randomized controlled study. J. Clin. Pharm. Ther. 2016, 41, 78–83. [Google Scholar] [CrossRef]
- Silva, S.T.; Hak, F.; Machado, J. Rule-based Clinical Decision Support System using the OpenEHR Standard. Procedia Comput. Sci. 2022, 201, 726–731. [Google Scholar] [CrossRef]
- Charalambous, S.; Maraba, N.; Jennings, L.; Rabothata, I.; Cogill, D.; Mukora, R.; Hippner, P.; Naidoo, P.; Xaba, N.; Mchunu, L.; et al. Treatment adherence and clinical outcomes amongst in people with drug-susceptible tuberculosis using medication monitor and differentiated care approach compared with standard of care in South Africa: A cluster randomized trial. eClinicalMedicine 2024, 75, 102745. [Google Scholar] [CrossRef]
| Sl. No. | Category | Descriptions |
|---|---|---|
| 1 | Emergency and Critical Care Support | Early warning for sepsis, stroke, and cardiac arrest |
| Triage decision support | ||
| Ventilator management and respiratory monitoring | ||
| 2 | Laboratory and Radiology Decision Support | Automated lab result interpretation (e.g., critical value alerts) |
| AI-assisted imaging analysis | ||
| Radiology order appropriateness checks | ||
| 3 | Infectious Disease Management | ASP (e.g., antimicrobial therapy recommendations) |
| Infection control alerts (e.g., MDR organisms and sepsis detection) | ||
| Outbreak surveillance and early warning systems | ||
| 4 | Preventive Care and Public Health | Immunization reminders (e.g., pediatric and geriatric vaccines) |
| Cancer screening alerts (e.g., mammograms and colonoscopy reminders) | ||
| Smoking cessation and lifestyle modification suggestions | ||
| 5 | Personalized and Precision Medicine | Pharmacogenomics-based drug selection |
| Oncology decision support for target therapies | ||
| AI-driven risk prediction models for individualized treatment | ||
| 6 | Surgical and Anesthesia Support | Preoperative risk assessment tools |
| Anesthesia dose calculation and DI alerts | ||
| Postoperative complication risk prediction | ||
| 7 | Optimization and Administrative Support | Task automation and scheduling |
| Clinical documentation assistance (e.g., voice-to-text transcription and structured note generation) | ||
| Predictive analytics for hospital resource allocation | ||
| 8 | Geriatric Care and Fall Risk Prediction | Polypharmacy risk management |
| Fall risk assessment and prevention strategies | ||
| Cognitive impairment screening (e.g., dementia risk prediction) | ||
| 9 | Pediatric and Neonatal Care | Growth and development monitoring |
| NICU support | ||
| Pediatric drug dose calculation and alerts | ||
| 10 | Medication Management | DI alerts |
| Allergy and ADR warnings | ||
| Dose adjustment recommendations | ||
| Duplicate therapy alerts | ||
| Medication reconciliation | ||
| Automated dispensing support | ||
| 11 | Diagnostic Assistance | CDT for differential diagnosis |
| AI-powered image recognition for radiology and pathology | ||
| Symptom checker tools for early disease detection | ||
| Lab test interpretation and recommendations | ||
| 12 | Chronic Disease Management | Diabetes management (e.g., HbA1c monitoring and insulin dose adjustment) |
| HTN monitoring and control recommendations | ||
| COPD and asthma management | ||
| 13 | Clinical Guidelines | Integration of clinical practice guidelines |
| Personalized treatment recommendations based on patient data | ||
| Best-practice alerts (e.g., sepsis protocols and stroke management) |
| Sl. No. | Place | Health System |
|---|---|---|
| 1 | Bengaluru, Karnataka | Narayana Health |
| Manipal Hospitals | ||
| Cloudnine Hospitals | ||
| Aster DM Healthcare | ||
| HCG | ||
| Sakra World Hospital | ||
| 2 | Chennai, Tamil Nadu | Apollo |
| 3 | Cochin, Kerala | AIMS |
| 4 | Telangana | KIMS |
| 5 | Mumbai | Tata Memorial Hospital |
| 6 | Gurgaon, Haryana | Medanta |
| 7 | Chandigarh (UT) | PGIMER |
| 8 | New Delhi | AIIMS |
| Armed Forces | ||
| Max Healthcare |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thorakkattil, S.A.; Sridhar, S.B.; Abdulsalim, S.; Karattuthodi, M.S.; Chandra, P.; Unnikrishnan, M.K. Clinical Decision Support Systems in Indian Healthcare Settings: Benefits, Barriers, and Future Implications. Healthcare 2025, 13, 2220. https://doi.org/10.3390/healthcare13172220
Thorakkattil SA, Sridhar SB, Abdulsalim S, Karattuthodi MS, Chandra P, Unnikrishnan MK. Clinical Decision Support Systems in Indian Healthcare Settings: Benefits, Barriers, and Future Implications. Healthcare. 2025; 13(17):2220. https://doi.org/10.3390/healthcare13172220
Chicago/Turabian StyleThorakkattil, Shabeer Ali, Sathvik Belagodu Sridhar, Suhaj Abdulsalim, Mohammed Salim Karattuthodi, Prashant Chandra, and Mazhuvanchery Kesavan Unnikrishnan. 2025. "Clinical Decision Support Systems in Indian Healthcare Settings: Benefits, Barriers, and Future Implications" Healthcare 13, no. 17: 2220. https://doi.org/10.3390/healthcare13172220
APA StyleThorakkattil, S. A., Sridhar, S. B., Abdulsalim, S., Karattuthodi, M. S., Chandra, P., & Unnikrishnan, M. K. (2025). Clinical Decision Support Systems in Indian Healthcare Settings: Benefits, Barriers, and Future Implications. Healthcare, 13(17), 2220. https://doi.org/10.3390/healthcare13172220







