Guidelines for Reducing the Adverse Effects of Shift Work on Nursing Staff: A Systematic Review
Abstract
1. Introduction
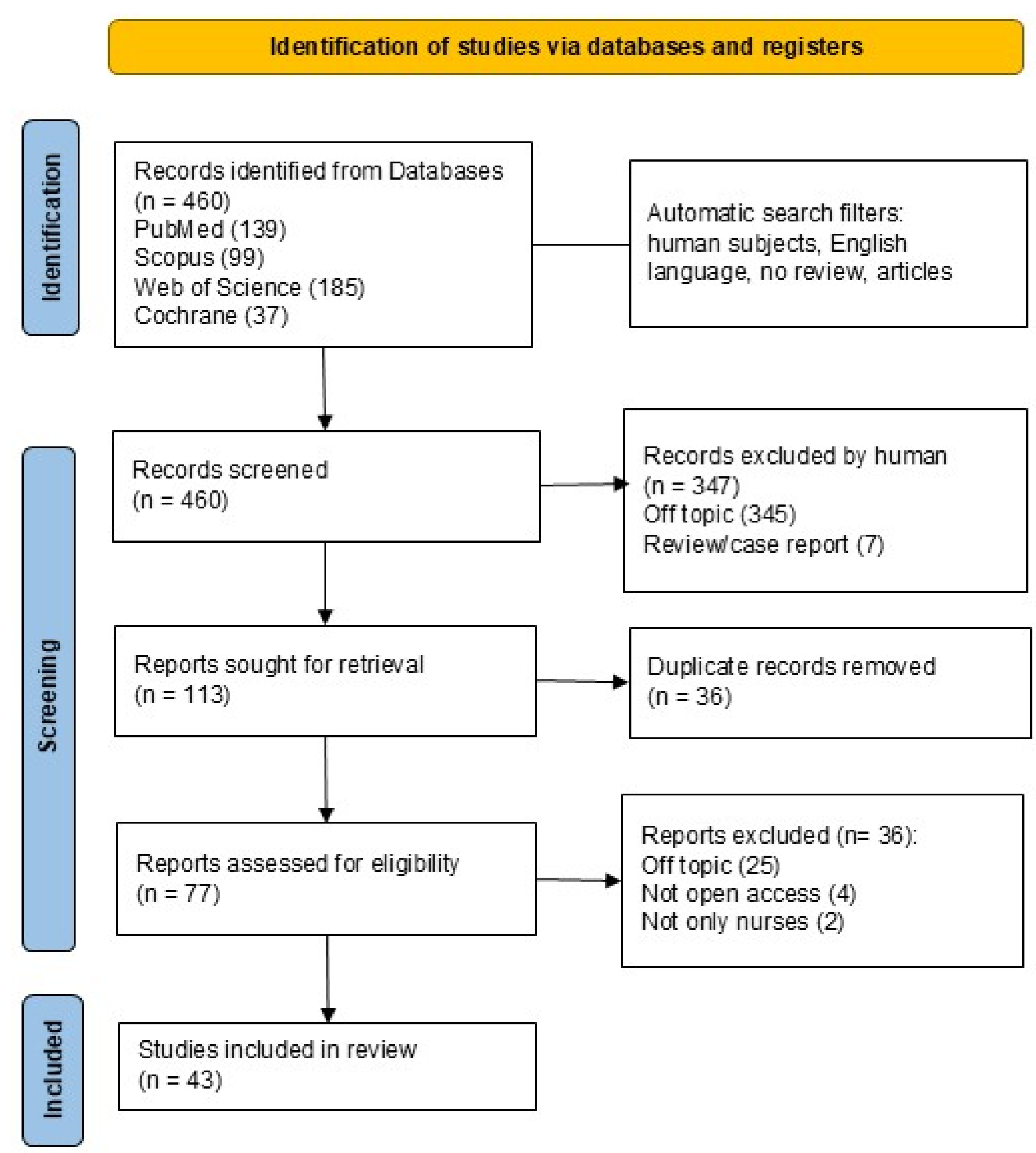
2. Materials and Methods
2.1. PICO Question
2.2. Research Protocol
2.3. Search Processing
2.4. Inclusion and Exclusion Criteria
2.5. Data Processing
2.6. Quality Assessment
3. Results
3.1. Characteristics of the Included Articles
3.2. Quality Assessment and Risk of Bias of Included Articles
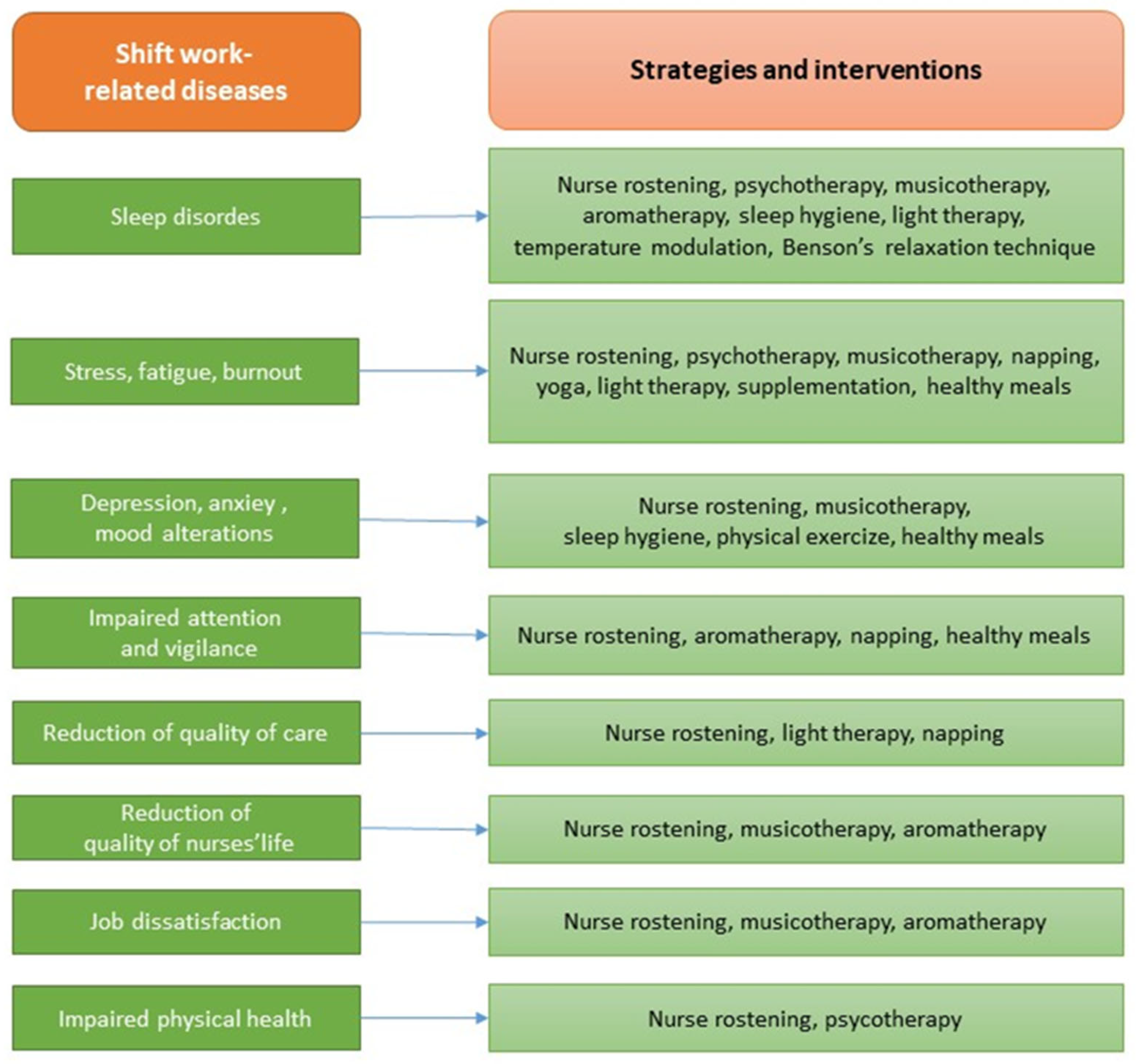
4. Discussion
4.1. Shift Planning
4.1.1. Work Schedules, Flexibility, and Recovery Time
4.1.2. Individual Factors and Chronotype in Shift Tolerance
4.1.3. Satisfaction Questionnaires
4.2. Light and Temperature Modulation
4.3. Supplementation
4.4. Meal Management
4.5. Physical Activity, Relaxation Techniques, and Yoga
4.6. Psychotherapy
4.7. Sleep Education
4.8. Music Therapy and Aromatherapy
4.9. Strengths and Limitations
- Chronotype-aware and flexible scheduling supported by mathematical or digital rostering tools;
- Structured opportunities for restorative napping;
- Integration of low-GI nutritional options during night shifts;
- Access to supervised or digitally supported physical activity programs;
- Incorporation of evidence-based psychological support programs, potentially AI-assisted;
- Availability of low-cost, low-risk complementary interventions such as music therapy or aromatherapy.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| CHD | Coronary Heart Disease |
| CI | Confidence Interval |
| COVID-19 | Coronavirus Disease 2019 |
| CVD | Cardiovascular Disease |
| DNA | Deoxyribonucleic Acid |
| GI | Glycemic Index |
| KSS | Karolinska Sleepiness Scale |
| ICU | Intensive Care Unit |
| MetS | Metabolic Syndrome |
| MS | Multiple Sclerosis |
| RCT | Randomized Controlled Trial |
| SW | Shift Work |
| SWD | Shift-Work-Related Diseases |
References
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic Review of Shift Work and Nurses’ Health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef]
- Imes, C.C.; Barthel, N.J.; Chasens, E.R.; Dunbar-Jacob, J.; Engberg, S.J.; Feeley, C.A.; Fennimore, L.A.; Godzik, C.M.; Klem, M.L.; Luyster, F.S.; et al. Shift Work Organization on Nurse Injuries: A Scoping Review. Int. J. Nurs. Stud. 2023, 138, 104395. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, J.T.; Karlsen, S.; Stayner, L.; Hansen, J.; Andersen, Z.J. Shift Work and Overall and Cause-Specific Mortality in the Danish Nurse Cohort. Scand. J. Work. Environ. Health 2017, 43, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Hong, H.C.; Kim, Y.M. Work Schedule Characteristics and Occupational Fatigue/Recovery among Rotating-Shift Nurses: A Cross-Sectional Study. J. Nurs. Manag. 2022, 30, 463–472. [Google Scholar] [CrossRef]
- Di Muzio, M.; Dionisi, S.; Di Simone, E.; Cianfrocca, C.; Di Muzio, F.; Fabbian, F.; Barbiero, G.; Tartaglini, D.; Giannetta, N. Can Nurses’ Shift Work Jeopardize the Patient Safety? A Systematic Review. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4507–4519. [Google Scholar] [CrossRef]
- Cooper, P.G. A Call for a Paradigm Shift in Nursing and Healthcare Leadership. Nurs. Forum 2008, 43, 1. [Google Scholar] [CrossRef]
- Barton, J.; Spelten, E.R.; Smith, L.R.; Totterdell, P.A.; Folkard, S. A Classification of Nursing and Midwifery Shift Systems. Int. J. Nurs. Stud. 1993, 30, 65–80. [Google Scholar] [CrossRef]
- White, E. A Comparison of Nursing Education and Workforce Planning Initiatives in the United States and England. Policy Politics Nurs. Pract. 2017, 18, 173–185. [Google Scholar] [CrossRef]
- Beckman, R.J.; Hutton, S.; Czekanski, E.; Vance, K.; Mohr, D.C. A Comparison of Shift Length and Nursing and Quality Outcomes in Acute Inpatient Mental Health Units. J. Nurs. Adm. 2022, 52, 560–565. [Google Scholar] [CrossRef]
- Niu, S.-F.; Chu, H.; Chen, C.-H.; Chung, M.-H.; Chang, Y.-S.; Liao, Y.-M.; Chou, K.-R. A Comparison of the Effects of Fixed- and Rotating-Shift Schedules on Nursing Staff Attention Levels: A Randomized Trial. Biol. Res. Nurs. 2013, 15, 443–450. [Google Scholar] [CrossRef]
- Ashraf, H.; Bodapati, A.; Hanif, A.; Okafor, D.K.; Katyal, G.; Kaur, G.; Khan, S. Safety and Efficacy of Biologic Therapies (Ustekinumab and Vedolizumab) in the Treatment of Inflammatory Bowel Disease (IBD): A Systematic Review. Cureus 2023, 15, e48338. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Virtanen, M.; Elovainio, M.; Väänänen, A.; Keltikangas-Järvinen, L.; Vahtera, J. Prevalent Cardiovascular Disease, Risk Factors and Selection out of Shift Work. Scand. J. Work. Environ. Health 2006, 32, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Feng, T.; Booth, B.M.; Baldwin-Rodríguez, B.; Osorno, F.; Narayanan, S. A Multimodal Analysis of Physical Activity, Sleep, and Work Shift in Nurses with Wearable Sensor Data. Sci. Rep. 2021, 11, 8693. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.-E.; Kim, T.-Y.; Yoo, H.-S.; Chae, M.S. A Postanaesthesia Workload Instrument Can Provide Objective Information Promoting Appropriate Workload Distribution between Day and Evening Shift Nursing Staff in the Postanaesthesia Care Unit: A Prospective Observational Cohort Study. Eur. J. Anaesthesiol. 2022, 39, 722–724. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Corelli, R.; Inchingolo, A.M.; Dipalma, G. Surgical treatment of depressed scar: A simple technique. Int. J. Med. Sci. 2011, 8, 377–379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Manias, E.; Aitken, R.; Peerson, A.; Parker, J.; Wong, K. Agency-Nursing Work: Perceptions and Experiences of Agency Nurses. Int. J. Nurs. Stud. 2003, 40, 269–279. [Google Scholar] [CrossRef]
- Lim, S.; Han, K.; Cho, H.; Baek, H. Shift-Work Nurses’ Work Environments and Health-Promoting Behaviours in Relation to Sleep Disturbance: A Cross-Sectional Secondary Data Analysis. J. Clin. Nurs. 2019, 28, 1538–1545. [Google Scholar] [CrossRef]
- Silva, R.M.d.; Zeitoune, R.C.G.; Lenz, F.C.D.; Pretto, C.R.; Santos, K.M.D.; Magnago, T.S.B.d.S.; Centenaro, A.P.F.C. Sleep Duration and Quality of Brazilian Nursing Staff Who Work in Shifts. Rev. Bras. Enferm. 2024, 77, e20230167. [Google Scholar] [CrossRef]
- Niu, S.-F.; Miao, N.-F.; Liao, Y.-M.; Chi, M.-J.; Chung, M.-H.; Chou, K.-R. Sleep Quality Associated with Different Work Schedules: A Longitudinal Study of Nursing Staff. Biol. Res. Nurs. 2017, 19, 375–381. [Google Scholar] [CrossRef]
- Buja, A.; Zampieron, A.; Mastrangelo, G.; Petean, M.; Vinelli, A.; Cerne, D.; Baldo, V. Strain and Health Implications of Nurses’ Shift Work. Int. J. Occup. Med. Environ. Health 2013, 26, 511–521. [Google Scholar] [CrossRef]
- Wakui, T. Study on Work Load of Matrons under Shift Work in a Special Nursing Home for the Elderly. Ind. Health 2000, 38, 280–288. [Google Scholar] [CrossRef]
- Congdon, J.; Craft, J.; Christensen, M. Are We Measuring Nursing Workflow Correctly? A Literature Review. Br. J. Nurs. 2020, 29, 1252–1259. [Google Scholar] [CrossRef]
- Bae, S.-H.; Fabry, D. Assessing the Relationships between Nurse Work Hours/Overtime and Nurse and Patient Outcomes: Systematic Literature Review. Nurs. Outlook 2014, 62, 138–156. [Google Scholar] [CrossRef] [PubMed]
- Buss, J. Associations between Obesity and Stress and Shift Work among Nurses. Workplace Health Saf. 2012, 60, 453–458, quiz 459. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, F.; Mattei, A.; Notarnicola, I.; Petrucci, C.; Lancia, L. Can Sleep Quality and Burnout Affect the Job Performance of Shift-Work Nurses? A Hospital Cross-Sectional Study. J. Adv. Nurs. 2018, 74, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Morse, L.; Duncan, H.; Apen, L.V.; Reese, K.; Crawford, C.L. Centralized Scheduling of Nursing Staff: A Rapid Review of the Literature. Nurs. Adm. Q. 2024, 48, 347–358. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Servili, A.; Inchingolo, A.M.; Dipalma, G. A Hypothetical Correlation between Hyaluronic Acid Gel and Development of Cutaneous Metaplastic Synovial Cyst. Head Face Med. 2010, 6, 13. [Google Scholar] [CrossRef]
- Malcangi, G.; Patano, A.; Morolla, R.; De Santis, M.; Piras, F.; Settanni, V.; Mancini, A.; Di Venere, D.; Inchingolo, F.; Inchingolo, A.D.; et al. Analysis of Dental Enamel Remineralization: A Systematic Review of Technique Comparisons. Bioengineering 2023, 10, 472. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Carpentiere, V.; Garofoli, G.; Azzollini, D.; Campanelli, M.; Paduanelli, G.; Palermo, A.; et al. Artificial Intelligence and Its Clinical Applications in Orthodontics: A Systematic Review. Diagnostics 2023, 13, 3677. [Google Scholar] [CrossRef]
- Banning, J.A. Chronic fatigue and shift work. Can. Nurse 1991, 87, 3. [Google Scholar]
- Kalra, Y. Chronotype and Nursing Shift Work. Am. J. Nurs. 2025, 125, 64. [Google Scholar] [CrossRef] [PubMed]
- Tuominen, O.; Lundgren-Laine, H.; Teperi, S.; Salanterä, S. Comparing the Two Techniques for Nursing Staff Rescheduling to Streamline Nurse Managers’ Daily Work in Finland. Comput. Inform. Nurs. 2020, 38, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Albert-Sabater, J.A.; Martínez, J.M.; Baste, V.; Moen, B.E.; Ronda-Perez, E. Comparison of Menstrual Disorders in Hospital Nursing Staff According to Shift Work Pattern. J. Clin. Nurs. 2016, 25, 3291–3299. [Google Scholar] [CrossRef]
- Inchingolo, F.; Santacroce, L.; Ballini, A.; Topi, S.; Dipalma, G.; Haxhirexha, K.; Bottalico, L.; Charitos, I.A. Oral Cancer: A Historical Review. Int. J. Environ. Res. Public Health 2020, 17, 3168. [Google Scholar] [CrossRef] [PubMed]
- Coffey, L.C.; Skipper, J.K.J.; Jung, F.D. Nurses and Shift Work: Effects on Job Performance and Job-Related Stress. J. Adv. Nurs. 1988, 13, 245–254. [Google Scholar] [CrossRef]
- Stimpfel, A.W.; Fatehi, F.; Kovner, C. Nurses’ Sleep, Work Hours, and Patient Care Quality, and Safety. Sleep Health 2020, 6, 314–320. [Google Scholar] [CrossRef]
- Amritzer, M.A.; Muntlin, Å.; Berg, L.M.; Göransson, K.E. Nursing Staff Ratio and Skill Mix in Swedish Emergency Departments: A National Cross-Sectional Benchmark Study. J. Nurs. Manag. 2021, 29, 2594–2602. [Google Scholar] [CrossRef]
- Kalisch, B.J.; Lee, H. Nursing Teamwork, Staff Characteristics, Work Schedules, and Staffing. Health Care Manag. Rev. 2009, 34, 323–333. [Google Scholar] [CrossRef]
- Zverev, Y.P.; Misiri, H.E. Perceived Effects of Rotating Shift Work on Nurses’ Sleep Quality and Duration. Malawi Med. J. 2009, 21, 19–21. [Google Scholar] [CrossRef][Green Version]
- Haghayegh, S.; Liu, Y.; Zhang, Y.; Strohmaier, S.; Papantoniou, K.; Markt, S.; Giovannucci, E.; Schernhammer, E. Rotating Night Shift Work and Bladder Cancer Risk in Women: Results of Two Prospective Cohort Studies. Int. J. Environ. Res. Public Health 2023, 20, 2202. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Patano, A.; Di Pede, C.; Inchingolo, A.D.; Palmieri, G.; de Ruvo, E.; Campanelli, M.; Buongiorno, S.; Carpentiere, V.; Piras, F.; et al. Autologous Tooth Graft: Innovative Biomaterial for Bone Regeneration. Tooth Transformer® and the Role of Microbiota in Regenerative Dentistry. A Systematic Review. J. Funct. Biomater. 2023, 14, 132. [Google Scholar] [CrossRef] [PubMed]
- Malcangi, G.; Patano, A.; Ciocia, A.M.; Netti, A.; Viapiano, F.; Palumbo, I.; Trilli, I.; Guglielmo, M.; Inchingolo, A.D.; Dipalma, G.; et al. Benefits of Natural Antioxidants on Oral Health. Antioxidants 2023, 12, 1309. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Paracchini, L.; de Angelis, F.; Cielo, A.; Orefici, A.; Spitaleri, D.; Santacroce, L.; Gheno, E.; Palermo, A. Biomechanical Behaviour of a Jawbone Loaded with a Prosthetic System Supported by Monophasic and Biphasic Implants. Oral Implantol. 2016, 9, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Minetti, E.; Dipalma, G.; Palermo, A.; Patano, A.; Inchingolo, A.D.; Inchingolo, A.M.; Inchingolo, F. Biomolecular Mechanisms and Case Series Study of Socket Preservation with Tooth Grafts. J. Clin. Med. 2023, 12, 5611. [Google Scholar] [CrossRef]
- Bellocchio, L.; Inchingolo, A.D.; Inchingolo, A.M.; Lorusso, F.; Malcangi, G.; Santacroce, L.; Scarano, A.; Bordea, I.R.; Hazballa, D.; D’Oria, M.T.; et al. Cannabinoids Drugs and Oral Health-From Recreational Side-Effects to Medicinal Purposes: A Systematic Review. Int. J. Mol. Sci. 2021, 22, 8329. [Google Scholar] [CrossRef]
- Parhizkar, S.; Holtzman, D.M. The Night’s Watch: Exploring How Sleep Protects against Neurodegeneration. Neuron 2025, 113, 817–837. [Google Scholar] [CrossRef]
- Jørgensen, J.T.; Hansen, J.; Westendorp, R.G.J.; Nabe-Nielsen, K.; Stayner, L.T.; Simonsen, M.K.; Andersen, Z.J. Shift Work and Incidence of Dementia: A Danish Nurse Cohort Study. Alzheimer’s Dement. 2020, 16, 1268–1279. [Google Scholar] [CrossRef]
- Esmaily, A.; Jambarsang, S.; Mohammadian, F.; Mehrparvar, A.H. Effect of Shift Work on Working Memory, Attention and Response Time in Nurses. Int. J. Occup. Saf. Ergon. 2022, 28, 1085–1090. [Google Scholar] [CrossRef]
- Papantoniou, K.; Massa, J.; Devore, E.; Munger, K.L.; Chitnis, T.; Ascherio, A.; Schernhammer, E.S. Rotating Night Shift Work and Risk of Multiple Sclerosis in the Nurses’ Health Studies. Occup. Environ. Med. 2019, 76, 733–738. [Google Scholar] [CrossRef]
- Simunić, A.; Gregov, L. Conflict between Work and Family Roles and Satisfaction among Nurses in Different Shift Systems in Croatia: A Questionnaire Survey. Arh. Hig. Rada Toksikol. 2012, 63, 189–197. [Google Scholar] [CrossRef]
- Minelli, A.; Di Palma, M.; Rocchi, M.B.L.; Ponzio, E.; Barbadoro, P.; Bracci, M.; Pelusi, G.; Prospero, E. Cortisol, Chronotype, and Coping Styles as Determinants of Tolerance of Nursing Staff to Rotating Shift Work. Chronobiol. Int. 2021, 38, 666–680. [Google Scholar] [CrossRef]
- Feldman, K.; Rohan, A.J. Data-Driven Nurse Staffing in the Neonatal Intensive Care Unit. MCN Am. J. Matern. Child. Nurs. 2022, 47, 249–264. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G. Comparison between traditional surgery, CO2 and Nd:Yag laser treatment for generalized gingival hyperplasia in Sturge-Weber syndrome: A retrospective study. J. Investig. Clin. Dent. 2010, 1, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Pisarski, A.; Bohle, P.; Callan, V.J. Effects of Coping Strategies, Social Support and Work-Nonwork Conflict on Shift Worker’s Health. Scand. J. Work. Environ. Health 1998, 24 (Suppl. 3), 141–145. [Google Scholar] [PubMed]
- Min, A.; Kim, Y.M.; Yoon, Y.S.; Hong, H.C.; Kang, M.; Scott, L.D. Effects of Work Environments and Occupational Fatigue on Care Left Undone in Rotating Shift Nurses. J. Nurs. Scholarsh. 2021, 53, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Onrubia, I.M.; Resta Sánchez, E.J.; Cabañero Contreras, T.; Perona Moratalla, A.B.; Molina Alarcón, M. Emergency Nursing Staff’s Well-Being, Burnout, and Sleep on 12-Hour Shifts. Enferm. Clin. 2025, 35, 102141. [Google Scholar] [CrossRef]
- Jørgensen, J.T.; Rozing, M.P.; Westendorp, R.G.J.; Hansen, J.; Stayner, L.T.; Simonsen, M.K.; Andersen, Z.J. Shift Work and Incidence of Psychiatric Disorders: The Danish Nurse Cohort Study. J. Psychiatr. Res. 2021, 139, 132–138. [Google Scholar] [CrossRef]
- Vitale, E.; Lupo, R.; Artioli, G.; Mea, R.; Lezzi, P.; Conte, L.; De Nunzio, G. How Shift Work Influences Anxiety, Depression, Stress and Insomnia Conditions in Italian Nurses: An Exploratory Study. Acta Biomed. 2023, 94, e2023102. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ejebu, O.-Z.; Ball, J.; Griffiths, P. Shift Work Characteristics and Burnout among Nurses: Cross-Sectional Survey. Occup. Med. 2023, 73, 199–204. [Google Scholar] [CrossRef]
- Camerino, D.; Conway, P.M.; Sartori, S.; Campanini, P.; Estryn-Béhar, M.; van der Heijden, B.I.J.M.; Costa, G. Factors Affecting Work Ability in Day and Shift-Working Nurses. Chronobiol. Int. 2008, 25, 425–442. [Google Scholar] [CrossRef]
- Kim, M.; Kim, J.-H.; Jung, Y.W.; Seong, S.J.; Kim, S.-Y.; Yoon, H.-J.; Lee, S.-S.; Kim, H.-J.; Ku, B.-S.; Cho, H.-Y. Gynecologic Problems and Healthcare Behavior by Shift Patterns in Korean Nursing Staff. PLoS ONE 2022, 17, e0276282. [Google Scholar] [CrossRef] [PubMed]
- Stimpfel, A.W.; Aiken, L.H. Hospital Staff Nurses’ Shift Length Associated with Safety and Quality of Care. J. Nurs. Care Qual. 2013, 28, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.M.; Hobbs, B.B. Impact of Shift Work on the Health and Safety of Nurses and Patients. Clin. J. Oncol. Nurs. 2006, 10, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Gonge, H.; Buus, N. Individual and Workplace Factors That Influence Psychiatric Nursing Staff’s Participation in Clinical Supervision: A Survey Study and Prospective Longitudinal Registration. Issues Ment. Health Nurs. 2010, 31, 345–354. [Google Scholar] [CrossRef]
- Saksvik-Lehouillier, I.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Moen, B.E.; Magerøy, N.; Akerstedt, T.; Pallesen, S. Individual, Situational and Lifestyle Factors Related to Shift Work Tolerance among Nurses Who Are New to and Experienced in Night Work. J. Adv. Nurs. 2013, 69, 1136–1146. [Google Scholar] [CrossRef]
- Galanti, T.; Cortini, M.; Giudice, G.F.; Zappalà, S.; Toscano, F. Safeguarding Nurses’ Mental Health: The Critical Role of Psychosocial Safety Climate in Mitigating Relational Stressors and Exhaustion. AIMS Public Health 2024, 11, 905–917. [Google Scholar] [CrossRef]
- Clark, A.; Moule, P.; Topping, A.; Serpell, M. Rescheduling Nursing Shifts: Scoping the Challenge and Examining the Potential of Mathematical Model Based Tools. J. Nurs. Manag. 2015, 23, 411–420. [Google Scholar] [CrossRef]
- Inchingolo, F.; Ballini, A.; Mura, S.; Farronato, D.; Cirulli, N.; Pettini, F.; Gheno, E.; Vermesan, D.; Pederzoli, P.; Resta, G.; et al. Use of Platelet Rich Fibrin and Bio-OSS/SINT-Oss for Implant-Prosthetic Rehabilitation in Maxillary Atrophy with Sinus Pathology: A 48-Month Follow-Up. Eur. J. Inflamm. 2015, 13, 58–65. [Google Scholar] [CrossRef]
- de Cordova, P.B.; Phibbs, C.S.; Stone, P.W. Perceptions and Observations of Off-Shift Nursing. J. Nurs. Manag. 2013, 21, 283–292. [Google Scholar] [CrossRef]
- Weng, P.-W.; Chang, W.-P. Relationship between Shift Type and Sleep Quality in Rotating-Shift Nurses with Chronotype as a Moderator Variable. Int. Nurs. Rev. 2025, 72, e13010. [Google Scholar] [CrossRef]
- Salah, R.A.; Malak, M.Z.; Bani Salameh, A.K. Relationship between Shift-Work and Life-Style Behaviors among Emergency Department Nurses in Jordan. Arch. Environ. Occup. Health 2022, 77, 27–34. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Rotenberg, L.; Griep, R.H.; Fischer, F.M. Relationship between Sleeping on the Night Shift and Recovery from Work among Nursing Workers—The Influence of Domestic Work. J. Adv. Nurs. 2011, 67, 972–981. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Pacifici, A.; Gargari, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G.; Marrelli, M.; Abenavoli, F.M.; Pacifici, L. Use of Dermal-Fat Grafts in the Post-Oncological Reconstructive Surgery of Atrophies in the Zygomatic Region: Clinical Evaluations in the Patients Undergone to Previous Radiation Therapy. Head Face Med. 2012, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Corelli, R.; Inchingolo, A.M.; Dipalma, G. Upper Eyelid Reconstruction: A Short Report of an Eyelid Defect Following a Thermal Burn. Head Face Med. 2009, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Malcangi, G.; Costa, S.; Fatone, M.C.; Avantario, P.; Campanelli, M.; Piras, F.; Patano, A.; Ferrara, I.; Di Pede, C.; et al. Tooth Complications after Orthodontic Miniscrews Insertion. Int. J. Environ. Res. Public Health 2023, 20, 1562. [Google Scholar] [CrossRef]
- Niu, S.-F.; Chung, M.-H.; Chu, H.; Tsai, J.-C.; Lin, C.-C.; Liao, Y.-M.; Ou, K.-L.; O’Brien, A.P.; Chou, K.-R. Differences in Cortisol Profiles and Circadian Adjustment Time between Nurses Working Night Shifts and Regular Day Shifts: A Prospective Longitudinal Study. Int. J. Nurs. Stud. 2015, 52, 1193–1201. [Google Scholar] [CrossRef]
- Shiffer, D.; Minonzio, M.; Dipaola, F.; Bertola, M.; Zamuner, A.R.; Dalla Vecchia, L.A.; Solbiati, M.; Costantino, G.; Furlan, R.; Barbic, F. Effects of Clockwise and Counterclockwise Job Shift Work Rotation on Sleep and Work-Life Balance on Hospital Nurses. Int. J. Environ. Res. Public Health 2018, 15, 2038. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Griffiths, P.; Emmanuel, T.; Rafferty, A.M.; Ewings, S. The RN4CAST Consortium 12-hr Shifts in Nursing: Do They Remove Unproductive Time and Information Loss or Do They Reduce Education and Discussion Opportunities for Nurses? A Cross-sectional Study in 12 European Countries. J. Clin. Nurs. 2020, 29, 53–59. [Google Scholar] [CrossRef]
- Inoue, M.; Takano, M.; Ueno, C.; Mori, M.; Morimatsu, Y.; Matsumoto, Y.; Kushino, N.; Ishitake, T. Advantages of the Variable Shift System, and Effective Use of Break Time to Better Support the Work Engagement of Nurses on Extended Day Shifts. Kurume Med. J. 2020, 65, 155–168. [Google Scholar] [CrossRef]
- Waage, S.; Pallesen, S.; Moen, B.E.; Vedaa, Ø.; Thun, E.; Vikanes Buchvold, H.; Blytt, K.M.; Harris, A.; Bjorvatn, B. Changes in Work Schedule Affect the Prevalence of Shift Work Disorder among Norwegian Nurses—A Two Year Follow-up Study. Chronobiol. Int. 2021, 38, 924–932. [Google Scholar] [CrossRef]
- Kubo, T.; Matsumoto, S.; Izawa, S.; Ikeda, H.; Nishimura, Y.; Kawakami, S.; Tamaki, M.; Masuda, S. Shift-Work Schedule Intervention for Extending Restart Breaks after Consecutive Night Shifts: A Non-Randomized Controlled Cross-Over Study. Int. J. Environ. Res. Public Health 2022, 19, 15042. [Google Scholar] [CrossRef]
- Jung, H.-S.; Lee, B. Contributors to Shift Work Tolerance in South Korean Nurses Working Rotating Shift. Appl. Nurs. Res. 2015, 28, 150–155. [Google Scholar] [CrossRef]
- Pahlevanzadeh, M.J.; Jolai, F.; Goodarzian, F.; Ghasemi, P. A New Two-Stage Nurse Scheduling Approach Based on Occupational Justice Considering Assurance Attendance in Works Shifts by Using Z-Number Method: A Real Case Study. RAIRO-Oper. Res. 2021, 55, 3317–3338. [Google Scholar] [CrossRef]
- Bülbül, E.; ÇeliK, S.; Özkan, A.; Akbaş, G. Assessment of the Chronotypes of Nurses Working in Shifts and the Quality of Their Lives. Clin. Exp. Health Sci. 2023, 13, 491–496. [Google Scholar] [CrossRef]
- Li, J.-N.; Chen, X.-Q.; Jiang, X.-M.; Zheng, Q.-X.; Pan, Y.-Q.; Zhu, Y.; Huang, L.; Liu, R.-L. Exploring the Associations between Chronotype, Night Shift Work Schedule, Quality of Work Life, and Sleep Quality among Maternal and Child Health Nurses: A Multicentre Cross-Sectional Study. J. Nurs. Manag. 2023, 2023, 1811732. [Google Scholar] [CrossRef]
- De Bruijn, L.; Berentzen, N.E.; Vermeulen, R.C.H.; Vlaanderen, J.J.; Kromhout, H.; Van Leeuwen, F.E.; Schaapveld, M. Chronotype in Relation to Shift Work: A Cohort Study among 37,731 Female Nurses. J. Sleep Res. 2024, 34, e14308. [Google Scholar] [CrossRef]
- Dehring, T.; Von Treuer, K.; Redley, B. The Impact of Shift Work and Organisational Climate on Nurse Health: A Cross-Sectional Study. BMC Health Serv. Res. 2018, 18, 586. [Google Scholar] [CrossRef]
- Abed Al Ahad, M.; Elbejjani, M.; Simon, M.; Ausserhofer, D.; Abu-Saad Huijer, H.; Dhaini, S.R. Variability, Shift-specific Workloads and Rationed Care Predictors of Work Satisfaction among Registered Nurses Providing Acute Care: A Longitudinal Study. Nurs. Open 2022, 9, 1190–1199. [Google Scholar] [CrossRef]
- Lee, J.; Jeong, I.S. Compliance with Recommendations on Work Schedule for Shift Nurses in South Korea. Saf. Health Work 2021, 12, 255–260. [Google Scholar] [CrossRef]
- Booker, L.A.; Mills, J.; Bish, M.; Spong, J.; Deacon-Crouch, M.; Skinner, T.C. Nurse Rostering: Understanding the Current Shift Work Scheduling Processes, Benefits, Limitations, and Potential Fatigue Risks. BMC Nurs. 2024, 23, 295. [Google Scholar] [CrossRef]
- Shin, S.-H.; Lee, E.-H. Development and Validation of a Quality of Healthy Work Environment Instrument for Shift Nurses. BMC Nurs. 2024, 23, 37. [Google Scholar] [CrossRef]
- Griepentrog, J.E.; Labiner, H.E.; Gunn, S.R.; Rosengart, M.R. Bright Environmental Light Improves the Sleepiness of Nightshift ICU Nurses. Crit. Care 2018, 22, 295. [Google Scholar] [CrossRef]
- Bjorvatn, B.; Pallesen, S.; Waage, S.; Thun, E.; Blytt, K.M. The Effects of Bright Light Treatment on Subjective and Objective Sleepiness during Three Consecutive Night Shifts among Hospital Nurses—A Counter-Balanced Placebo-Controlled Crossover Study. Scand. J. Work Environ. Health 2021, 47, 145–153. [Google Scholar] [CrossRef]
- Hoshi, H.; Iwasa, H.; Goto, A.; Yasumura, S. Effects of Working Environments with Minimum Night Lighting on Night-Shift Nurses’ Fatigue and Sleep, and Patient Safety. BMJ Open Qual. 2022, 11, e001638. [Google Scholar] [CrossRef]
- Kim, J.H.; Song, Y. The Effects of Indoor Ambient Temperature at Work on Physiological Adaptation in Night Shift Nurses. J. Nurs. Manag. 2020, 28, 1098–1103. [Google Scholar] [CrossRef]
- Sadeghniiat-Haghighi, K.; Bahrami, H.; Aminian, O.; Meysami, A.; Khajeh-Mehrizi, A. Melatonin Therapy in Shift Workers with Difficulty Falling Asleep: A Randomized, Double-Blind, Placebo-Controlled Crossover Field Study. Work 2016, 55, 225–230. [Google Scholar] [CrossRef]
- Gholipour Baradari, A.; Alipour, A.; Mahdavi, A.; Sharifi, H.; Nouraei, S.M.; Emami Zeydi, A. The Effect of Zinc Supplementation on Sleep Quality of ICU Nurses: A Double Blinded Randomized Controlled Trial. Workplace Health Saf. 2018, 66, 191–200. [Google Scholar] [CrossRef]
- Suyoto, P.S.; de Rijk, M.G.; de Vries, J.H.; Feskens, E.J. The Effect of Meal Glycemic Index and Meal Frequency on Glycemic Control and Variability in Female Nurses Working Night Shifts: A Two-Arm Randomized Cross-Over Trial. J. Nutr. 2024, 154, 69–78. [Google Scholar] [CrossRef]
- Leedo, E.; Beck, A.M.; Astrup, A.; Lassen, A.D. The Effectiveness of Healthy Meals at Work on Reaction Time, Mood and Dietary Intake: A Randomised Cross-over Study in Daytime and Shift Workers at an University Hospital. Br. J. Nutr. 2017, 118, 121–129. [Google Scholar] [CrossRef]
- Matsugaki, R.; Kuhara, S.; Saeki, S.; Jiang, Y.; Michishita, R.; Ohta, M.; Yamato, H. Effectiveness of Workplace Exercise Supervised by a Physical Therapist among Nurses Conducting Shift Work: A Randomized Controlled Trial. J. Occup. Health 2017, 59, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Baek, Y.; Han, K.; Kim, J.; Yoo, H.Y. Smartphone-Based Home Workout Program for Shift-Work Nurses Working during the COVID-19 Pandemic. Nurs. Health Sci. 2022, 24, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, Y. Restorative Yoga for Occupational Stress among Japanese Female Nurses Working Night Shift: Randomized Crossover Trial. J. Occup. Health 2019, 61, 508–516. [Google Scholar] [CrossRef]
- Baek, G.; Cha, C. AI-Assisted Tailored Intervention for Nurse Burnout: A Three-Group Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2025, 22, e70003. [Google Scholar] [CrossRef]
- Ell, J.; Brückner, H.A.; Johann, A.F.; Steinmetz, L.; Güth, L.J.; Feige, B.; Järnefelt, H.; Vallières, A.; Frase, L.; Domschke, K.; et al. Digital Cognitive Behavioural Therapy for Insomnia Reduces Insomnia in Nurses Suffering from Shift Work Disorder: A Randomised-Controlled Pilot Trial. J. Sleep. Res. 2024, 33, e14193. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Q.; Zheng, D.; Mei, J.; Lu, J.; Chen, G.; Wang, W.; Ding, F. The Effects of a Complex Interactive Multimodal Intervention on Personalized Stress Management Among Health Care Workers in China: Nonrandomized Controlled Study. J. Med. Internet Res. 2024, 26, e45422. [Google Scholar] [CrossRef]
- Lu, C.; Sun, Y.; Wang, C.; Chen, T.; Tang, Y. The Effects of Confiding on Shift Work Nurses’ Emotion Regulation and Self-Perceived Well-Being: An Online Randomized Controlled Trial. Behav. Sci. 2025, 15, 9. [Google Scholar] [CrossRef]
- Watanabe, K.; Sugimura, N.; Shishido, I.; Konya, I.; Yamaguchi, S.; Yano, R. Effects of 90 Min Napping on Fatigue and Associated Environmental Factors among Nurses Working Long Night Shifts: A Longitudinal Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 9429. [Google Scholar] [CrossRef]
- Watanabe, K.; Shishido, I.; Ito, Y.M.; Yano, R. Quantity and quality of napping to mitigate fatigue and sleepiness among nurses working long night shifts: A prospective observational study. J. Physiol. Anthropol. 2025, 44, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Booker, L.A.; Sletten, T.L.; Barnes, M.; Alvaro, P.; Collins, A.; Chai-Coetzer, C.L.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M.W.; Howard, M.E. The Effectiveness of an Individualized Sleep and Shift Work Education and Coaching Program to Manage Shift Work Disorder in Nurses: A Randomized Controlled Trial. J. Clin. Sleep Med. 2022, 18, 1035–1045. [Google Scholar] [CrossRef]
- Albakri, U.; Smeets, N.; Kant, I.; Meertens, R. Strategies That Nurses Working Irregular Night Shifts Use to Improve Sleep Quality: A Qualitative Study among Good and Poor Sleepers. J. Adv. Nurs. 2024, 80, 2038–2050. [Google Scholar] [CrossRef]
- Oriyama, S.; Miyakoshi, Y.; Rahman, M.M. The Effects of a 120-Minute Nap on Sleepiness, Fatigue, and Performance during 16-Hour Night Shifts: A Pilot Study. J. Occup. Health 2019, 61, 368–377. [Google Scholar] [CrossRef]
- Comparative Effects of Music Therapy and Aromatherapy on Stress, Quality of Life, and Happiness Among Shift Nurses in Korea: A Randomized Controlled Trial. Available online: https://jkbns.org/journal/view.php?number=657 (accessed on 29 March 2025).
- Wang, X.; Feng, T.; Liu, S.; Ruan, J. Application of Music Therapy in Improving the Sleep Quality and Mental Health of Nurses with Circadian Rhythm Sleep Disorders Caused by Work Shifts. Noise Health 2024, 26, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Zamanifar, S.; Bagheri-Saveh, M.I.; Nezakati, A.; Mohammadi, R.; Seidi, J. The Effect of Music Therapy and Aromatherapy with Chamomile-Lavender Essential Oil on the Anxiety of Clinical Nurses: A Randomized and Double-Blind Clinical Trial. J. Med. Life 2020, 13, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Molzof, H.E.; Wirth, M.D.; Burch, J.B.; Shivappa, N.; Hebert, J.R.; Johnson, R.L.; Gamble, K.L. The Impact of Meal Timing on Cardiometabolic Syndrome Indicators in Shift Workers. Chronobiol. Int. 2017, 34, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, A.; Boroomand, M.M. The Effect of Rosemary Essential Oil Inhalation on Sleepiness and Alertness of Shift-Working Nurses: A Randomized, Controlled Field Trial. Complement. Ther. Clin. Pract. 2021, 43, 101326. [Google Scholar] [CrossRef]

| Article Screening Strategy | Keywords: A: “shift work”; B: “nurses” |
| Boolean Indicators: “A” AND “B” | |
| Timespan: from 1 January 2015 to 3 March 2025 | |
| Electronic Databases: PubMed, Scopus, Web of Science, and Cochrane |
| Intervention on Category | No. of Studies | Study Designs (RCT/Obs./Other) | Main Targeted Outcomes | No. Studies Reporting Improvement |
|---|---|---|---|---|
| Shift planning and individual factors | 12 | 3 RCT, 9 Obs. | Sleep quality, fatigue, work engagement, absenteeism | 10 |
| Satisfaction questionnaires | 5 | 0 RCT, 5 Obs. | Job satisfaction, workload, compliance with ergonomic guidelines | 4 |
| Light and temperature modulation | 4 | 2 RCT, 2 Obs. | Sleepiness, fatigue, performance, thermal comfort | 3 |
| Supplementation | 2 | 2 RCT | Sleep efficiency, latency, micronutrient status | 2 |
| Meal management | 3 | 2 RCT, 1 Obs. | Glycemic control, mood, metabolic parameters | 3 |
| Physical activity, relaxation, yoga | 3 | 2 RCT, 1 Exp. | Aerobic capacity, depression, sleep quality | 3 |
| Psychotherapy | 4 | 3 RCT, 1 Non-RCT | Burnout, stress, insomnia | 4 |
| Sleep education | 6 | 2 RCT, 4 Obs. | Fatigue, sleep quality, anxiety | 5 |
| Music and aromatherapy | 4 | 3 RCT, 1 Retrospective | Sleep quality, anxiety, stress, alertness | 4 |
| Total | 43 | — | — | — |
| Study | Bias Due to Confounding | Selection Bias | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of Reported Results | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Niu S.F. et al. (2015) [77] |  |  |  |  |  |  |  |  |
| Schiffer D. et al. (2018) [78] |  |  |  |  |  |  |  |  |
| Dall’Ora C. et al. (2020) [79] |  |  |  |  |  |  |  |  |
| Inoue M. et al. (2020) [80] |  |  |  |  |  |  |  |  |
| Waage S. et al. (2021) [81] |  |  |  |  |  |  |  |  |
| Kubo T. et al. (2022) [82] |  |  |  |  |  |  |  |  |
| Jung H.S et al. (2015) [83] |  |  |  |  |  |  |  |  |
| Pahlevanzadeh M.J. et al. (2021) [84] |  |  |  |  |  |  |  |  |
| Bülbül E. et al. (2023) [85] |  |  |  |  |  |  |  |  |
| Li J.N et al. (2023) [86] |  |  |  |  |  |  |  |  |
| de Bruijn L. et al. (2024) [87] |  |  |  |  |  |  |  |  |
| Dehring T. et al. (2018) [88] |  |  |  |  |  |  |  |  |
| Abed Al Ahad M. et al. (2021) [89] |  |  |  |  |  |  |  |  |
| Lee J. et al. (2021) [90] |  |  |  |  |  |  |  |  |
| Booker L.A. et al. (2024) [91] |  |  |  |  |  |  |  |  |
| Shin S.H. et al. (2024) [92] |  |  |  |  |  |  |  |  |
| Griepentrog J.E. et al. (2018) [93] |  |  |  |  |  |  |  |  |
| Bjorvatn B. et al. (2021) [94] |  |  |  |  |  |  |  |  |
| Hoshi H. et al. (2022) [95] |  |  |  |  |  |  |  |  |
| Kim J.H. et al. (2020) [96] |  |  |  |  |  |  |  |  |
| Sadeghniiat-Haghighi et al. (2016) [97] |  |  |  |  |  |  |  |  |
| Gholipour Baradari A. et al. (2017) [98] |  |  |  |  |  |  |  |  |
| Suyoto et al. (2024) [99] |  |  |  |  |  |  |  |  |
| Leedo E. (2017) [100] |  |  |  |  |  |  |  |  |
| Matsugaki R. (2017) [101] |  |  |  |  |  |  |  |  |
| Baek Y. (2022) [102] |  |  |  |  |  |  |  |  |
| Yoko M. (2019) [103] |  |  |  |  |  |  |  |  |
| Baek G. et al. (2025) [104] |  |  |  |  |  |  |  |  |
| Eli et al. (2024) [105] |  |  |  |  |  |  |  |  |
| Wenhua Lu et al. (2024) [106] |  |  |  |  |  |  |  |  |
| Cui Lu et al. (2025) [107] |  |  |  |  |  |  |  |  |
| Elif B. et al. (2023) [85] |  |  |  |  |  |  |  |  |
| Watanabe K. et al. (2022) [108] |  |  |  |  |  |  |  |  |
| Watanabe K. et al. (2025) [109] |  |  |  |  |  |  |  |  |
| Oriyama S. et al. (2019) [110] |  |  |  |  |  |  |  |  |
| Albakri U. et al. (2023) [109] |  |  |  |  |  |  |  |  |
| Booker L.A. et al. (2022) [111] |  |  |  |  |  |  |  |  |
| Wang X. et al. (2024) [112] |  |  |  |  |  |  |  |  |
| Zamanifar et al. (2020) [113] |  |  |  |  |  |  |  |  |
| Lee Sh. et al. (2024) [114] |  |  |  |  |  |  |  |  |
| Nasiri A. et al. (2021) [115] |  |  |  |  |  |  |  |  |
| Molzof et al. (2017) [116] |  |  |  |  |  |  |  |  |
 low risk;
low risk;  moderate risk;
moderate risk;  high risk;
high risk;  missing data.
missing data.| Authors | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Niu S.F. et al. (2015) [77] | Prospective longitudinal, parallel group, comparative | 63 randomly assigned to night and day-shift groups | Salivary cortisol measurement to assess circadian secretion patterns | Observation over work shifts and recovery periods | Circadian cortisol levels, cortisol awakening response, SW impact | Night-shift nurses required at least 4 days to adjust their circadian rhythm; 2 days off were necessary to restore diurnal cortisol levels. Night shifts led to altered cortisol profiles, affecting adaptation and recovery. |
| Schiffer D. et al. (2018) [78] | Cross-sectional | 100 females in Northern Italy | Questionnaire and daily diary assessing sleep, work performance, and work–life balance. | None | Sleep quantity/quality, work performance, work–life balance | CW shift nurses had better sleep quality, fewer awakenings, and better work–life balance than CCW shift nurses. CCW rotation was linked to more sleep disturbances, attention deficits, and social/family life interference. |
| Dall’Ora C. et al. (2020) [79] | Cross-sectional survey | 31,627 from 487 hospitals in 12 European countries | Comparison of 12 h shifts vs. shorter shifts in relation to education, discussion opportunities, continuity of care, and information loss during handovers. | None | Participation in continuing education programs, time for discussion with colleagues, continuity of care, and loss of patient information during handovers | Long shifts were associated with reduced educational opportunities and fewer discussions on patient care. No significant association with continuity of care or information loss was found. |
| Inoue, M. et al. (2020) [80] | Survey-based observational | 805 in Japan | Evaluation of a variable shift system and break activities. | Self-reported survey data analysis | Work engagement, stress, fatigue, break activities | Variable shift system supports work engagement; workload correlates with stress; effective breaks improve engagement. |
| Waage S. et al. (2021) [81] | Longitudinal cohort | 1076 | Changes in work schedules, reduction/increase in night shifts, and quick returns. | 2 yrs. | SWDs prevalence, number of night shifts, number of quick returns | Stopping night shifts reduced SWD prevalence; increasing night shifts increased SWD prevalence. |
| Kubo T. et al. (2022) [82] | Non-randomized controlled cross-over | 30 females in Japan | Extended restart breaks from 31 h to 55 h after consecutive night shifts, subjective and objective fatigue, and sleep measurements | 5-mo. | Vital exhaustion, psychological distress, hair cortisol, salivary C-reactive protein, sleep patterns | Extended restart breaks moderately reduced fatigue and distress. No significant effect on objectively measured stress, sleep, or biomarkers |
| Authors | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Jung H.S. et al. (2015) [83] | Cross-sectional, correlational | 660 females in South Korea | Questionnaire on demographics, lifestyle, and work conditions | None | SWT, insomnia, fatigue, depression | SWT influenced by self-esteem, job stress, morningness, and physical activity. Job stress was the key factor. Physical activity reduced insomnia and fatigue, while alcohol increased fatigue. More depression in younger nurses |
| Pahlevanzadeh M.J. et al. (2021) [84] | Mathematical modeling, real case | Mathematical modeling, real case: 18 male nurses, 11 female nurses without a child, 7 female nurses with a child | Binary integer programming model for nurse scheduling using Z-number method for justice-based shift assignment | Performance assessed post-implementation | Nurse attendance, complaints, and satisfaction | 40% reduction in absences, 50% reduction in complaints, 30% increase in satisfaction |
| Bülbül E. et al. (2023) [85] | Descriptive | 267 females | MEQ, SF-36 | None | Chronotypes of nurses, quality of life, number of night shifts, sleep patterns | Evening-type nurses had lower quality of life; morning-type nurses were older and had more work experience; evening-type nurses had more night shifts and lower scores in physical and mental health |
| Li J.N. et al. (2023) [86] | Multicenter cross-sectional | 1426 female MCH in China | Demographic questionnaire, self-reported chronotype, PSQI, WRQOL-2 scale. | None | Sleep quality, chronotype, night shift schedule, quality of work life | 57.9% of nurses had poor sleep quality. Chronotype and work–life quality were major predictors. Night shift schedule had no significant effect on adjusted models. Poor sleep was linked to older age, caffeine intake, and irregular meals |
| de Bruijn L. et al. (2024) [87] | Cohort | 37,731 Dutch females | Self-reported assessments of SW history, shift type preference, chronotype classification, MOS-SPI-II | 6 yrs. | Chronotype stability, sleep timing in work-free periods, shift type preference, sleep problems related to SW | Evening types preferred night shifts, while morning types favored day shifts. Intermediate chronotypes had fewer sleep problems compared to morning or evening types. Chronotype remained stable over six years, with gradual shifts towards morningness. Extreme chronotypes experienced greater circadian disruption, affecting sleep quality and SWT |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Dehring T. et al. (2018) [88] | Cross-sectional | 108 registered nurses from two Melbourne health services. 98 females | Survey on demographic characteristics, organizational climate, and health outcomes | None | Organizational climate factors, health outcomes (general health, social dysfunction, stress) | Rotating shift nurses had higher coworker cohesion; night staff reported greater physical comfort. Supervisor support predicted better health outcomes. Task orientation reduced social dysfunction. Enhancing organizational climate could mitigate negative health effects of SW |
| Abed Al Ahad M. et al. (2021) [89] | Longitudinal | 90 female registered nurses, 1303 responses, Lebanese hospital | Daily surveys assessing work satisfaction, workload, patient-to-nurse ratio, and rationed care | day 91 | Shift-specific workload, job satisfaction, implicit rationing of care | Work satisfaction varied among individual nurses but not across units. Lower workload and less rationed care improved satisfaction. Objective workload (patient-to-nurse ratio) was not a strong predictor. Improving scheduling and teamwork may enhance satisfaction |
| Lee J. et al. (2021) [90] | Descriptive | 182 females working in three shifts for more than one year in superior general and general hospitals: | Self-administered questionnaire, 13-week work schedule tables analyzed based on 17 work schedule recommendations (WSRs), person-based and cycle-based compliance assessments | None | General nurse characteristics, compliance with 17 WSRs, factors affecting compliance (hospital type, workplace standards, nurses in school/pregnancy) | Compliance with WSRs averaged 11.77/17. No nurse fully adhered to “no work on weekends.” Factors like hospital type, institutional standards, and demographics influenced compliance. Frequent weekend work and consecutive night shifts led to inadequate rest. Two-day rest after night shifts was rarely followed. Hospitals with scheduling standards showed better compliance |
| Booker L.A. et al. (2024) [91] | Qualitative single case | 24 across 3 hospitals in Victoria, Australia | Semi-structured interviews, thematic analysis, grounded theory methods | None | Rostering process, training, fatigue risks, SW practices, cultural barriers | Rostering staff lacked formal training, self-rostering was common but led to fatigue concerns, cultural resistance to change, and the need for better education on safe shift scheduling |
| Shin S.H. et al. (2024) [92] | Methodological | 247 in Korea | Literature review, in-depth interviews, expert validation, questionnaire testing | None | QHWE, reliability, validity, job satisfaction | Developed a 23-item instrument measuring physical, psychological, social, and structural factors. High reliability and validity confirmed. Can assess and improve nurses’ work environment |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Griepentrog J.E. et al. (2018) [93] | Randomized, crossover | 43 matched pairs of ICU (31 subjects + 12 in both phases); 71% female | High illuminance light (1500–2000 lx) for 10 h during night shift Compared with standard hospital lighting (300 lx) | Each nurse completed both lighting exposures; primary assessments were performed at 5:00 h (end of exposure) | SSS PVT: errors, lapses, reaction time Salivary melatonin levels | Reduced sleepiness under bright light. Increased psychomotor errors. No significant changes in PVT lapses or reaction times. Melatonin suppressed more under bright light, but not statistically significant |
| Bjorvatn B. et al. (2021) [94] | RCT | 35 | Bright light (10,000 lx) vs. red dim light (100 lx) for 30 min at night (timed from 2:00 to 4:00 over 3 nights) Three-night shifts with each light condition | 9-day protocol: 3 days before, 3 night shifts, 3 days after; crossover with ≥3-we. washout | Subjective KSS. Accumulated Time with Sleepiness (heavy eyelids, reduced performance). Objective performance PVT. Mood, caffeine intake, general functioning. | Heavy eyelids reduced with bright light on nights 1 and 2. No significant effect on KSS or PVT. No difference in overall functioning after night shifts. Bright light did not impair readaptation to day rhythm |
| Hoshi H. et al. (2022) [95] | Non-randomized, open-label, quasi-experimental | 20 females (17 analyzed for dark; 10 for well-lit condition): | Comparison of dark lighting (110 lx) vs. bright lighting (410 lx) at nurse workstations during night shifts | Two lighting phases: Nov–Dec 2015 (dark); Jan–Feb 2016 (well-lit) | Subjective fatigue and sleepiness (instability, uneasiness, grogginess, lethargy, drowsiness). Sleep quality (sleepiness on waking, sleep induction/maintenance, dreaming, recovery from fatigue, sleep duration). Incident/accident reports. | Fatigue and sleepiness were higher under dark lighting (e.g., lethargy and drowsiness significantly increased) No significant difference in sleep quality No negative impact on work performance (incident/accident rates not significantly affected) |
| Kim J.H. et al. (2020) [96] | Crossover | 20 female (2 groups of 10) | Nurses worked in two temperature-controlled environments: 23 °C CTE 26 °C NTE Each nurse experienced both conditions for 2 consecutive night shifts. | 2-night shifts per condition, with 2-we. washout between | Thermal sensation Night work tolerance (fatigue, sleepiness, adaptation) Body temperature Urinary 6-sulphatoxymelatonin | 23 °C improved thermal comfort. Body temperature was lower at 23 °C. Melatonin significantly decreased on the 2nd night in 23 °C group. No significant difference in fatigue, sleepiness, or adaptation scores between conditions |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Sadeghniiat-Haghighi et al., (2016) [97] | RCT | 39 males with difficulty falling asleep (from 50 enrolled, out of 295 screened). | 3 mg melatonin vs. placebo taken 30 min. before sleep for 3 nights, with a 2 we. washout period | 3-night intervention periods for both melatonin and placebo | TST SE SOL WASO | SE increased with melatonin (82.2% → 85.5%) SOL decreased (0.27 h → 0.20 h) No significant change in TST and WASO No adverse effects reported. |
| Gholipour Baradari A. et al. (2017) [98] | RCT | 53 female ICU nurses (27 zinc group, 26 placebo group). | Zinc sulfate capsules (220 mg) every 72 h for 1 mo. vs. placebo | 1 mo. | Sleep Quality (PSQI: total and 7 components) Serum Zinc and Copper levels | Improved total sleep quality score with zinc. Significant improvement in subjective sleep quality and sleep latency. Serum zinc levels increased significantly in zinc group. No adverse effects reported. |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Suyoto et al. (2024) [99] | RCT | 49 | Comparison of night-shift meal strategies: no meal, 1 high-GI meal, 1 low-GI meal, 3 high-GI meals, 3 low-GI meals | 3 intervention periods: 3 days each with 2 we. of washout | CGM, AUCmin, PEAK, MEAN, CV, GVP, CONGA1h | 1 or 3 high-GI meals increased glycemic variability and peak glucose levels; 1 or 3 low-GI meals had no significant effect on glycemic control or variability vs. fasting; meal frequency had no independent effect; |
| Molzof et al. (2017) [116] | Observational, comparative | 17 | 9-day food intake recording, evaluation of inflammatory potential of diet (Dietary Inflammatory Index™), fasting metabolic panel on day off | 9 days + 1 fasting blood sample | Dietary intake by shift and time of day; CMS risk factors (lipids, HDL, etc.); inflammatory potential | Night-shift food intake (total grams) was positively associated with lipid levels; daytime intake was more pro-inflammatory for all nurses, regardless of shift |
| Leedo E. (2017) [100] | RCT | 60 | Healthy cold lunch, healthy snack, and water vs. usual diet (control) | Start point; end point | Reaction time (Go/No-Go test) Mood (POMS) Food intake (food diary 4 days) | No effect on reaction time. In shift workers: ↓ fatigue, ↑ vitality, ↓ mood disturbance ↑ intake of water, carbohydrates, fiber; ↓ fat |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Matsugaki, R. (2017) [101] | RCT | 30 SG: 15 VG: 15 | SG: Exercises under the supervision of a PT, twice a we. for 12 we, including aerobic and resistance training. VG: Exercises without supervision, with instruction only in the first session and encouragement by e-mail biweekly. | 12 we. | Aerobic capacity (VO2 max) Muscle strength Anthropometric data (BMI, muscle mass, fat mass) Biochemical parameters (total cholesterol, HDL, LDL, triglycerides, blood glucose, insulin, high molecular weight adiponectin, reactive oxygen metabolites) Mental health (depression levels, mood status with POMS) | Exercise supervised by a physical therapist has been shown to be more effective than voluntary exercise alone in improving aerobic capacity, muscle strength, and certain biochemical parameters |
| Baek Y. (2022) [102] | experimental study | 54 (I.G.: 25; C.G.: 24) | Smartphone-based home workout program; Text-message counseling; Environmental improvement | 18 we. | Sleep disturbance, fatigue, musculoskeletal problems, resilience, and nursing performance | The I.G. showed significant improvements |
| Yoko M. (2019) [103] | Randomized crossover trial | 20 | Restorative Yoga Program; Control Period; crossover | 9 we. | Psychological and physical stress Vital signs (blood pressure, heart rate). Body weight | Yoga significantly reduced psychological and physical stress reactions No significant changes in vital signs and body weight were observed. A reduction in stress after 4 weeks of home practice, with more pronounced effects than a single guided session |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Baek G. et al. (2025) [104] | RCT | 120 | E.G.: AI-assisted tailored intervention, selecting from four programs C.G.1: self-selected one of the four programs. C.G.2: online information on burnout reduction. | 4 we., with assessments at baseline, we. 2, and we. 4 | P. O.: client-related burnout, personal burnout, and work-related burnout. S.O.: job stress, stress responses, and coping strategies | E.G.: significant reductions in client-related burnout and personal burnout; Stress response reduction highest in C.G.1 N.S.D. for work-related burnout and job stress reduction |
| Eli et al. (2024) [105] | RCT | 120 | dCBT-I | 6 mo. | Insomnia severity index, sleep efficiency, daytime functioning, and psychological distress | dCBT-I group showed significant reductions in insomnia severity and psychological distress, with improvements in sleep efficiency and daytime functioning compared to the control group. |
| Wenhua Lu et al. (2024) [106] | Non-RCT | 245 | I.G.: CIMI, consisting of mobile stress management education, a web-based WeChat social network, personalized feedback, and support from a coach nurse. C.G.: self-guided stress management intervention. | 12 we. | Psychological indicators (perceived stress, mental distress, subjective happiness), physiological indicators (heart rate variability), and sleep-related measures (fatigue and sleepiness) | CIMI reduced perceived stress, depression, fatigue, and sleepiness while increasing subjective happiness. N.S.D. in physiological stress indicators were observed between the groups |
| Cui Lu et al. (2025) [107] | RCT | 66 I.G.: 34 C.G.: 32 | I.G.: online intervention focused on reflecting on social support obtained from confiding about work-related hassles C.G.: recorded confiding activities twice a week without reflecting on social support | 8 we. | IERQ, SRGHSQ and PHQ-9 | The confiding intervention enhanced interpersonal emotion regulation but had limited effects on intrapersonal emotion regulation and well-being |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Elif B. et al. (2023) [85] | Descriptive, cross-sectional | 267 | No clinical intervention; assessment through questionnaires: MEQ and SF-36 | None | Chronotype (morning, intermediate, evening via MEQ) Health-related quality of life (via SF-36) | 68.9% intermediate-type, 15.7% morning-type, 15.4% evening-type Evening-type nurses had more night shifts and significantly lower scores in physical, mental, and social domains of SF-36 |
| Watanabe K. et al. (2022) [108] | Longitudinal observational | 49 | No intervention; effects of natural 90 min napping during 16 h night shifts | 4-night shifts per nurse over 1 mo. | Total nap duration (TND) Environmental factors (noise, light, bedding, etc.) Fatigue levels Use of electronics, nap break duration, activity levels | Longer naps (≥90 min) are linked to less post-nap drowsiness and reduced fatigue at shift end Environmental factors (noise, screen time, nap time length) significantly influenced ability to nap ≥90 min More experienced nurses were more likely to achieve ≥90 min naps |
| Watanabe K. et al. (2025) [109] | Prospective observational | 32 | No clinical intervention; measured natural nap behaviors using activity monitors and surveys | 1 mo. (data collected from 120-night shifts; 105 included in nap-related analysis) | Nap quantity: TIB Nap quality: SE Fatigue Sleepiness Individual and environmental factors | TIB ≥ 120 min and SE ≥ 70% were optimal for reducing fatigue and sleepiness Low SE or short naps increased post-shift fatigue Factors influencing nap success: sleep reactivity, electronic device use, and prophylactic naps |
| Albakri U. et al. (2023) [109] | Qualitative descriptive study using semi-structured interviews | 34 (17 good sleepers, 17 poor sleepers) working irregular night shifts | No formal intervention: participants discussed strategies for sleep before, during, and after night shifts | None | Sleep quality Strategies used for sleep and alertness management Lifestyle and behavioral routines | Sleep quality Strategies used for sleep and alertness management Lifestyle and behavioral routines |
| Booker, L.A. et al. (2022) [111] | RCT | 149 | I.G.: 8-week individualized sleep and SW education + coaching program C.G.: Coaching on low glycemic index dietary habits | 6 mo. (pre- and post-intervention sick leave analysis + questionnaires at baseline/follow-up) | ISI SHI PHQ-9 GAD-7 FOSQ-1 0SWD risk | No significant difference in sick leave reduction Improvements in insomnia and depression in both groups Anxiety and sleep function improved significantly only in the intervention group |
| Oriyama, S. et al. (2019) [110] | Pilot crossover experimental | 14 | 120 min. naps at 3 different times: 22:00–00:00 (22-NAP) 00:00–02:00 (00-NAP) 02:00–04:00 (02-NAP) | 3 repeated lab experiments per participant, spaced 1 month apart | Sleep metrics: TST, SE, SOL, WASO Cognitive performance (mental arithmetic) VAS Sublingual temperature Heart rate variability | Sleep parameters are similar across all naps post-nap: ↑ sleepiness, fatigue, ↓ performance 00-NAP showed better early-morning outcomes 02-NAP showed highest fatigue immediately after nap |
| Authors (Year) | Study Design | Study Sample (N. Nurses) | Interventions/ Strategies | Follow-Up | Parameters Evaluated | Outcomes |
|---|---|---|---|---|---|---|
| Wang X. et al. (2024) [112] | Retrospective | 360 I.G.:180 C.G.: 180 | I.G.: MT2 treatment + music therapy C.G.: MT2 treatment. | Six treatment courses, with evaluations before and after. | SAS, SDS, PSQI, CE | I.G.: SAS, SDS, PSQI, and CE significantly improved |
| Lee Sh. et al. (2024) [114] | RCT | 78 | M.G.: Listened to music for at least 30 min, three times a day, for one week A.G.: Continuous inhalation of a blend of essential oils (lavender, ylang-ylang, and lemon) through an aroma necklace worn for one week. C.G.: no intervention | One we., with pre- and post-treatment evaluations. | LK, SI, QOL, OHQ | Music therapy and aromatherapy are effective in reducing stress and improving quality of life |
| Zamanifar et al. (2020) [113] | RCT | 120 | I.G.: (1) music therapy, (2) aromatherapy with chamomile-lavender oil, (3) both music therapy and aromatherapy C.G.: no intervention | After 3 consecutive work shifts | BAI | Significant reduction in anxiety in all three groups. Aromatherapy group had the lowest anxiety score post-intervention. |
| Nasiri A. et al. (2021) [115] | RCT | 80 I.G.:40 C.G.:40 | I.G.: inhalation of one drop of rosemary essential oil via mask C.G.: inhalation of distilled water during night shift for 2 h | Before and after intervention during the same shift | KSS, ESS | Rosemary oil significantly decreased sleepiness and increased alertness |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.D.; Inchingolo, A.M.; Fatone, M.C.; Ferrante, L.; Casamassima, L.; Trilli, I.; Inchingolo, F.; Palermo, A.; Marinelli, G.; Dipalma, G. Guidelines for Reducing the Adverse Effects of Shift Work on Nursing Staff: A Systematic Review. Healthcare 2025, 13, 2148. https://doi.org/10.3390/healthcare13172148
Inchingolo AD, Inchingolo AM, Fatone MC, Ferrante L, Casamassima L, Trilli I, Inchingolo F, Palermo A, Marinelli G, Dipalma G. Guidelines for Reducing the Adverse Effects of Shift Work on Nursing Staff: A Systematic Review. Healthcare. 2025; 13(17):2148. https://doi.org/10.3390/healthcare13172148
Chicago/Turabian StyleInchingolo, Alessio Danilo, Angelo Michele Inchingolo, Maria Celeste Fatone, Laura Ferrante, Lucia Casamassima, Irma Trilli, Francesco Inchingolo, Andrea Palermo, Grazia Marinelli, and Gianna Dipalma. 2025. "Guidelines for Reducing the Adverse Effects of Shift Work on Nursing Staff: A Systematic Review" Healthcare 13, no. 17: 2148. https://doi.org/10.3390/healthcare13172148
APA StyleInchingolo, A. D., Inchingolo, A. M., Fatone, M. C., Ferrante, L., Casamassima, L., Trilli, I., Inchingolo, F., Palermo, A., Marinelli, G., & Dipalma, G. (2025). Guidelines for Reducing the Adverse Effects of Shift Work on Nursing Staff: A Systematic Review. Healthcare, 13(17), 2148. https://doi.org/10.3390/healthcare13172148










