Knowledge, Confidence, and Comfort Regarding Sickle Cell Disease Among Medical Students: A Pilot Study in Two Universities
Abstract
1. Introduction
2. Materials and Methods
2.1. Development and Distribution
2.2. Statistical Analysis
2.3. Post-Hoc Power Assessment
3. Results
3.1. Demographic Characteristics
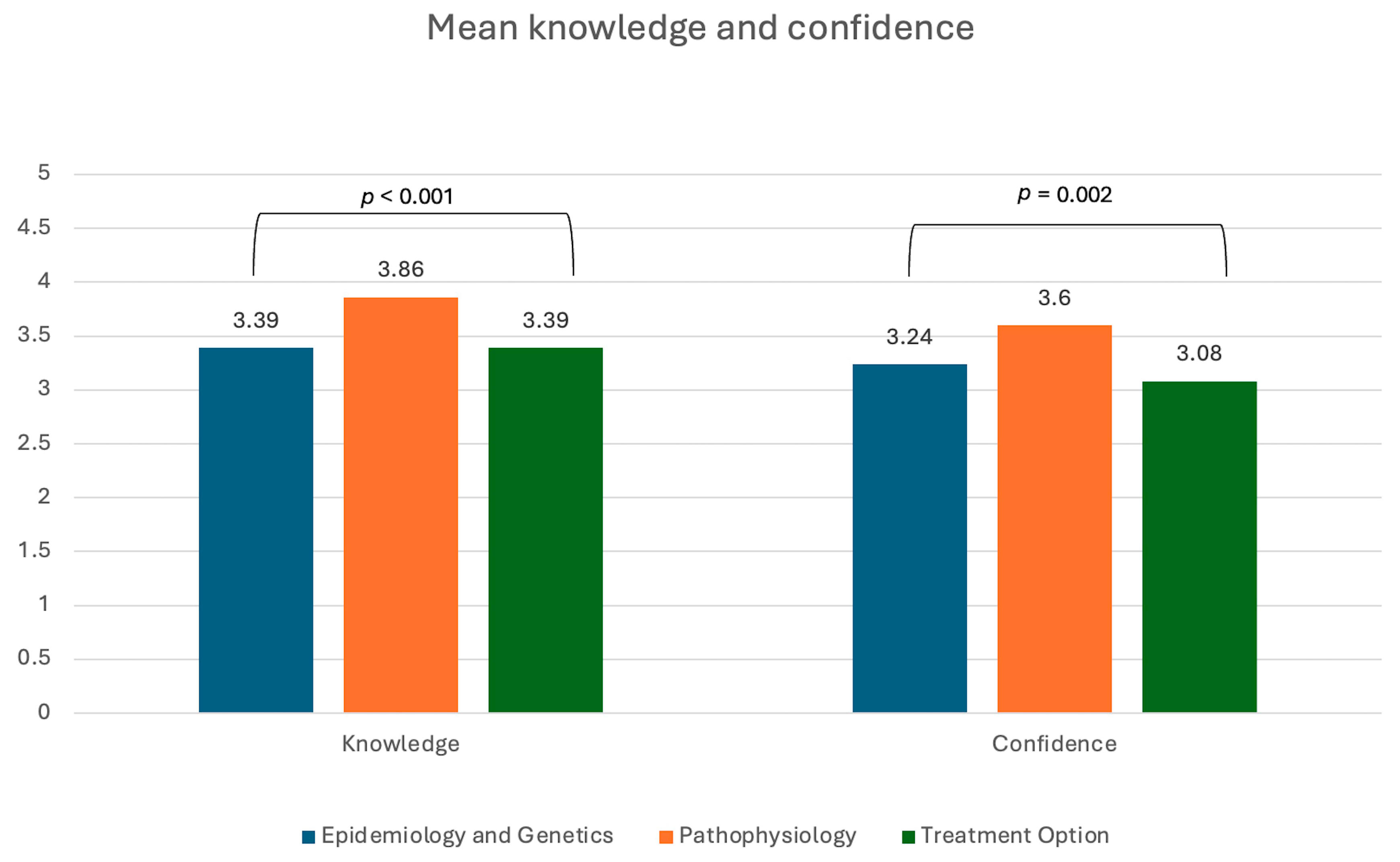
3.2. Overall Difference in Knowledge and Confidence
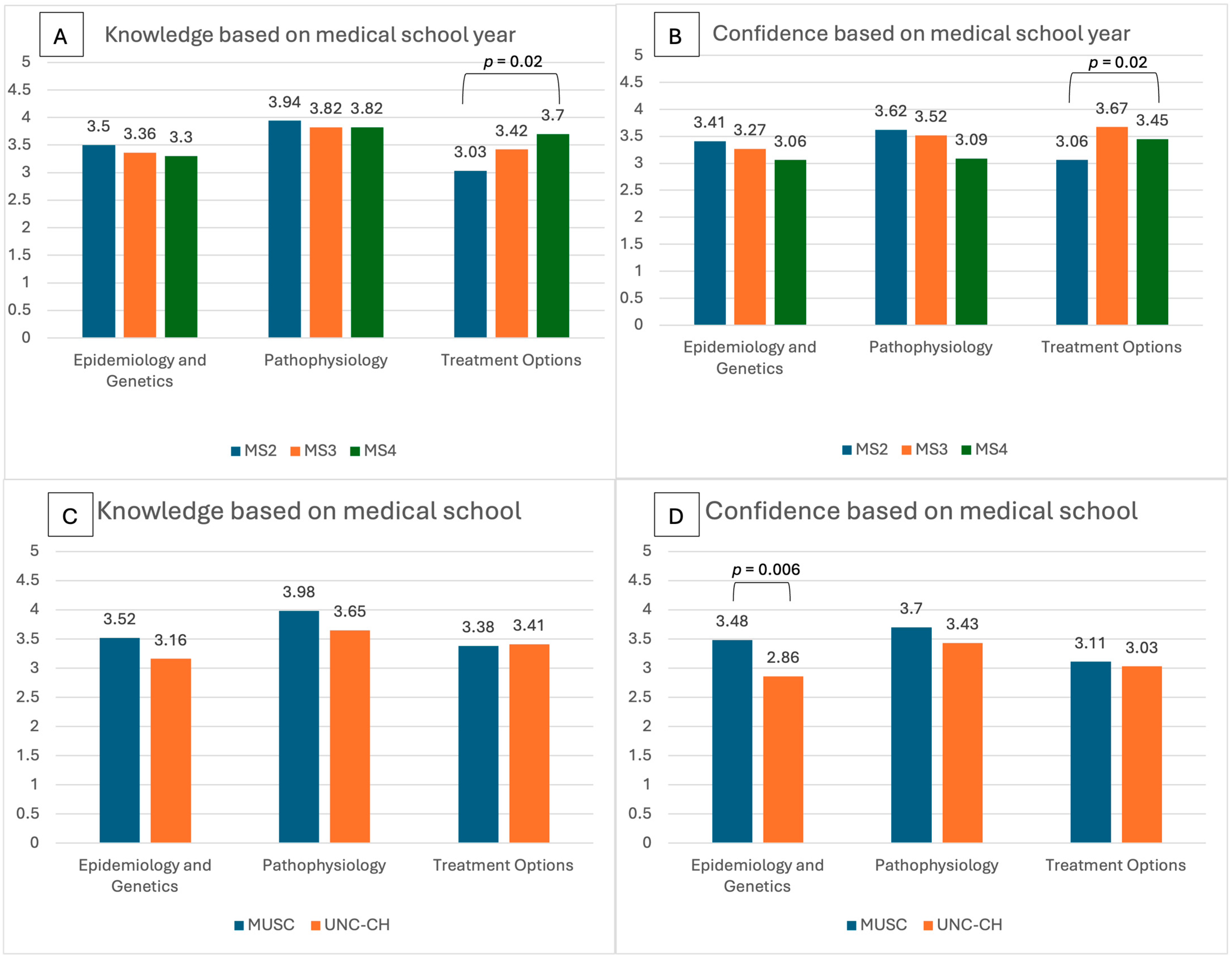
3.3. Self-Reported Knowledge and Confidence Based on Year of Medical School Training
3.4. Self-Reported Knowledge of and Comfort in Treatments of Various Complications
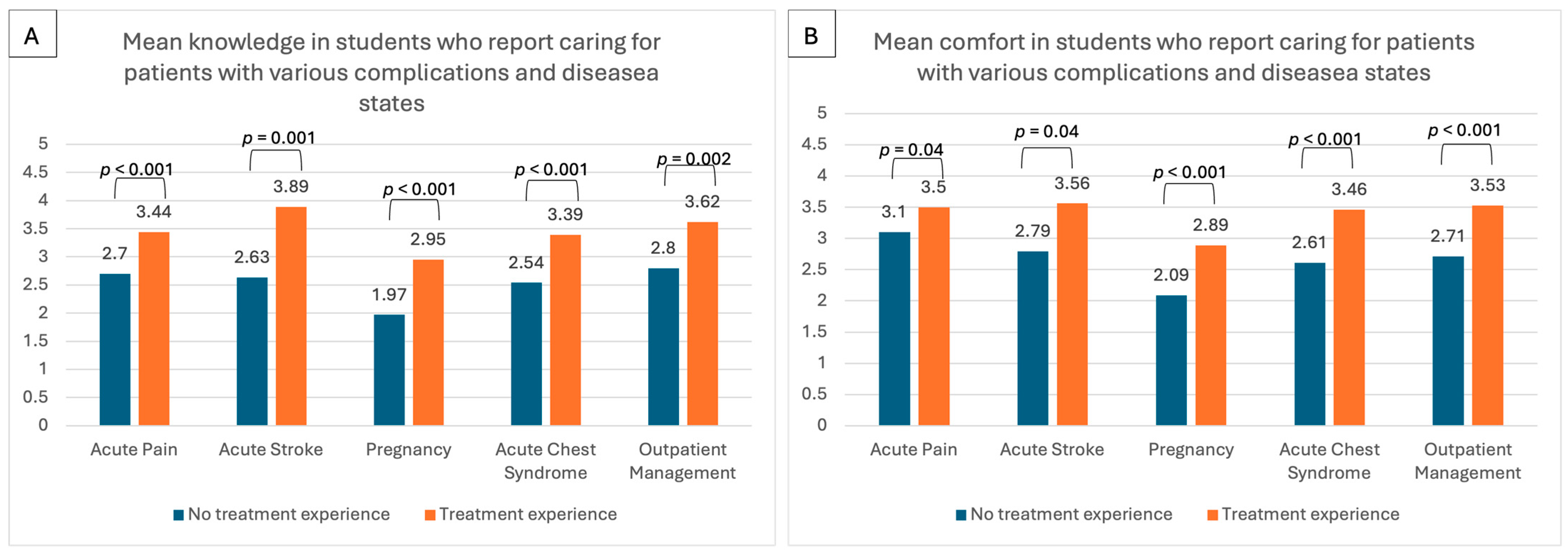
3.5. Caring for Patients with Various Complications
3.6. Examination of Student’s Knowledge Related to SCD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SCD | Sickle cell disease |
| RBC | Red blood cell |
| MUSC | Medical University of South Carolina |
| UNC-CH | University of North Carolina, Chapel Hill |
| REDCap | Research Electronic Data Capture |
| MS | Medical students |
| ED | Emergency department |
References
- GBD 2021 Sickle Cell Disease Collaborators. Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: A systematic analysis from the Global Burden of Disease Study 2021. Lancet Haematol. 2023, 10, e585–e599. [Google Scholar] [CrossRef]
- Data and Statistics on Sickle Cell Disease. Available online: https://www.cdc.gov/sickle-cell/data/ (accessed on 4 July 2024).
- Kato, G.J.; Piel, F.B.; Reid, C.D.; Gaston, M.H.; Ohene-Frempong, K.; Krishnamurti, L.; Smith, W.R.; Panepinto, J.A.; Weatherall, D.J.; Costa, F.F.; et al. Sickle cell disease. Nat. Rev. Dis. Primers 2018, 4, 18010. [Google Scholar] [CrossRef]
- Blinder, M.A.; Duh, M.S.; Sasane, M.; Trahey, A.; Paley, C.; Vekeman, F. Age-Related Emergency Department Reliance in Patients with Sickle Cell Disease. J. Emerg. Med. 2015, 49, 513–522.e1. [Google Scholar] [CrossRef] [PubMed]
- Moukalled, N.M.; Bou Fakhredin, R.; Taher, A.T. Pregnancy and sickle cell disease: An overview of complications and suggested perinatal care. Expert. Rev. Hematol. 2022, 15, 1055–1061. [Google Scholar] [CrossRef] [PubMed]
- Adam, S.; Jonassaint, J.; Kruger, H.; Kail, M.; Orringer, E.P.; Eckman, J.R.; Ashley-Koch, A.; Telen, M.J.; De Castro, L.M. Surgical and obstetric outcomes in adults with sickle cell disease. Am. J. Med. 2008, 121, 916–921. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fearon, A.; Marsh, A.; Kim, J.; Treadwell, M. Pediatric residents’ perceived barriers to opioid use in sickle cell disease pain management. Pediatr. Blood Cancer 2019, 66, e27535. [Google Scholar] [CrossRef] [PubMed]
- Van Doren, L.N.; Feder, K.J.; Calhoun, C.; Carroll, C.P.; Prince, E. Trainees’ Perspectives on Components of Sickle Cell Specific Education. Blood 2023, 142 (Suppl. 1), 791. [Google Scholar] [CrossRef]
- Anderson, D.; Hickey, E.; Syed, S.; Hines, J.; Abou Baker, N. Barriers and Resident Attitudes Surrounding Care of Patients with Sickle Cell Disease. Blood 2020, 136 (Suppl. 1), 21–22. [Google Scholar] [CrossRef]
- Burns, T.L.; DeBaun, M.R.; Boulet, J.R.; Murray, G.M.; Murray, D.J.; Fehr, J.J. Acute care of pediatric patients with sickle cell disease: A simulation performance assessment. Pediatr. Blood Cancer 2013, 60, 1492–1498. [Google Scholar] [CrossRef]
- Prince, E.J.; Feder, K.J.; Calhoun, C.; Lee, A.I.; Carroll, C.P.; Restrepo, V.; Van Doren, L. Trainees’ perspectives on sickle cell education: A qualitative needs assessment. BMC Med. Educ. 2024, 24, 715. [Google Scholar] [CrossRef] [PubMed]
- Whiteman, L.N.; Haywood, C., Jr.; Lanzkron, S.; Strouse, J.J.; Feldman, L.; Stewart, R.W. Primary Care Providers’ Comfort Levels in Caring for Patients with Sickle Cell Disease. South. Med. J. 2015, 108, 531–536. [Google Scholar] [CrossRef]
- Shook, L.M.; House, B.; Farrell, C.B.; Stewart, R.; Lanzkron, S.; King, A.A.; Varughese, T.; Strouse, J.J.; Treadwell, M.; Kanter, J. Challenges of Engaging Primary Care Providers in Specialized Telementoring Education About Sickle Cell Disease for Sickle Cell Specialists: Results from the Sickle Cell Disease Training and Mentoring Program for Primary Care Providers (STAMP) Project ECHO. AJPM Focus. 2025, 4, 100304. [Google Scholar] [CrossRef]
- Kanter, J.; Smith, W.R.; Desai, P.C.; Treadwell, M.; Andemariam, B.; Little, J.; Nugent, D.; Claster, S.; Manwani, D.G.; Baker, J.; et al. Building access to care in adult sickle cell disease: Defining models of care, essential components, and economic aspects. Blood Adv. 2020, 4, 3804–3813. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Wallace, N.; Levinsohn, E.A.; Marshall, A.L.; Kayoumi, K.; Madero, J.; Homer, M.; Reynolds, R.; Hafler, J.; Podoltsev, N.A.; et al. Trends and factors affecting the US adult hematology workforce: A mixed methods study. Blood Adv. 2019, 3, 3550–3561. [Google Scholar] [CrossRef] [PubMed]
- Hastings, C.; Borinstein, S.C.; Bergsagel, D.J.; Hagstrom, J.N.; Hooker, R.; Nugent, D.J.; Hudspeth, M. American Society of Pediatric Hematology Oncology Workforce Publication, W. The American Society of Pediatric Hematology Oncology workforce, productivity, and fellowship assessment: Current state of the workforce. Pediatr. Blood Cancer 2023, 70, e30221. [Google Scholar] [CrossRef]
- Hemker, B.G.; Brousseau, D.C.; Yan, K.; Hoffmann, R.G.; Panepinto, J.A. When children with sickle-cell disease become adults: Lack of outpatient care leads to increased use of the emergency department. Am. J. Hematol. 2011, 86, 863–865. [Google Scholar] [CrossRef]
- Lee, L.; Smith-Whitley, K.; Banks, S.; Puckrein, G. Reducing Health Care Disparities in Sickle Cell Disease: A Review. Public Health Rep. 2019, 134, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Druye, A.A.; Agyare, D.F.; Akoto-Buabeng, W.; Zutah, J.; Offei, F.O.; Nabe, B.; Ofori, G.O.; Alhassan, A.; Anumel, B.K.; Cobbinah, G.; et al. Healthcare Professionals’ Knowledge, Attitudes, and Practices in the Assessment, and Management of Sickle-Cell Disease: A Meta-Aggregative Review. Diseases 2024, 12, 156. [Google Scholar] [CrossRef]
- Azonobi, I.C.; Anderson, B.L.; Byams, V.R.; Grant, A.M.; Schulkin, J. Obstetrician-gynecologists’ knowledge of sickle cell disease screening and management. BMC Pregnancy Childbirth 2014, 14, 356. [Google Scholar] [CrossRef]
- Okumura, M.J.; Heisler, M.; Davis, M.M.; Cabana, M.D.; Demonner, S.; Kerr, E.A. Comfort of general internists and general pediatricians in providing care for young adults with chronic illnesses of childhood. J. Gen. Intern. Med. 2008, 23, 1621–1627. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute Blood Diseases; Disorders Education Program; CVS Health. Sickle Cell Disease Knowledge and Practices Among Healthcare Providers: Results of a National Survey; National Institutes of Health: Bethesda, MD, USA, 2025. [Google Scholar]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Martin, O.Y.; Thompson, S.M.; Carroll, A.E.; Jacob, S.A. Emergency Department Provider Survey Regarding Acute Sickle Cell Pain Management. J. Pediatr. Hematol. Oncol. 2020, 42, 375–380. [Google Scholar] [CrossRef]
- Robinson, K.; Esgro, R.A.; Cooper, S.; LoPresti, M.; Carson, B. Identifying and Addressing Knowledge and Confidence Gaps Regarding the Management of Patients with Sickle Cell Disease Via Engaging Continuing Medical Education. Blood 2023, 142 (Suppl. S1), 7228. [Google Scholar] [CrossRef]
- Aljuhani, O. Pain in sickle cell diseases; physicians’ knowledge, attitude, and barriers: A cross sectional study. J. Pak. Med. Assoc. 2022, 72, 2043–2047. [Google Scholar] [CrossRef]
- Ismail, A.S.; Aqel, A.; Abumuhfouz, M.I.; Safieh, M.; Arabyat, M.; Izham, M.; Singh, K.; Yassin, M.A. Knowledge, Attitude, and Practice Among Physicians Regarding Pain Management in Patients with SCD. Blood 2022, 140, 11159–11160. [Google Scholar] [CrossRef]
- Merz, L.E.; Osei, M.A.; Green, A.; Story, C.M.; Schuering, K.M.; Achebe, M.O. Development of a Hematology-General Medicine Hybrid Team to Improve Care of Patients With Sickle Cell Disease. Acad. Med. 2024, 99, 618–622. [Google Scholar] [CrossRef]
- Cramer-Bour, C.; Peterson, J.; Walsh, B.; Klings, E.S. Common Complications of Sickle Cell Disease: A Simulation-Based Curriculum. MedEdPORTAL 2021, 17, 11139. [Google Scholar] [CrossRef]
- Burgess, A.E.; Morrison, O.; Kent, P. Exposing Racial Bias to Confront Care Chasms: Innovations in the Sickle Cell Disease Curriculum at Rush Medical College. Acad. Med. 2022, 97, S119. [Google Scholar] [CrossRef]
- Oteng-Ntim, E.; Pavord, S.; Howard, R.; Robinson, S.; Oakley, L.; Mackillop, L.; Pancham, S.; Howard, J. British Society for Haematology, G. Management of sickle cell disease in pregnancy. A British Society for Haematology Guideline. Br. J. Haematol. 2021, 194, 980–995. [Google Scholar] [CrossRef]
- Sharma, D.; Kozanoglu, I.; Ataga, K.I.; Benachi, A.; Buyukkurt, S.; Lanzkron, S.; Ozdogu, H.; Pancham, S.; Pecker, L.H.; Robinson, S.E.; et al. Managing sickle cell disease and related complications in pregnancy: Results of an international Delphi panel. Blood Adv. 2024, 8, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- Society for Maternal-Fetal Medicine; Sinkey, R.G.; Ogunsile, F.J.; Kanter, J.; Bean, C.; Greenberg, M.; Society for Maternal-Fetal Medicine Publications Committee. Electronic address, p.s.o. Society for Maternal-Fetal Medicine Consult Series #68: Sickle cell disease in pregnancy. Am. J. Obstet. Gynecol. 2024, 230, B17–B40. [Google Scholar] [CrossRef]
- Alsuwaidi, L.; Kristensen, J.; Hk, A.; Al Heialy, S. Use of simulation in teaching haematological aspects to undergraduate medical students improves student’s knowledge related to the taught theoretical underpinnings. BMC Med. Educ. 2021, 21, 271. [Google Scholar] [CrossRef]
- Kanter, J.; Gibson, R.; Lawrence, R.H.; Smeltzer, M.P.; Pugh, N.L.; Glassberg, J.; Masese, R.V.; King, A.A.; Calhoun, C.; Hankins, J.S.; et al. Perceptions of US Adolescents and Adults With Sickle Cell Disease on Their Quality of Care. JAMA Netw. Open 2020, 3, e206016. [Google Scholar] [CrossRef]
- Lanzkron, S.; Carroll, C.P.; Haywood, C., Jr. The burden of emergency department use for sickle-cell disease: An analysis of the national emergency department sample database. Am. J. Hematol. 2010, 85, 797–799. [Google Scholar] [CrossRef]
- Sobota, A.; Neufeld, E.J.; Sprinz, P.; Heeney, M.M. Transition from pediatric to adult care for sickle cell disease: Results of a survey of pediatric providers. Am. J. Hematol. 2011, 86, 512–515. [Google Scholar] [CrossRef]
- Campbell, A.D.; Ross, P.T.; Kumagai, A.K.; Christner, J.G.; Lypson, M.L. Coming of age with sickle cell disease and the role of patient as teacher. J. Natl. Med. Assoc. 2010, 102, 1073–1078. [Google Scholar] [CrossRef]
- Bulgin, D.; Tanabe, P.; Jenerette, C. Stigma of Sickle Cell Disease: A Systematic Review. Issues Ment. Health Nurs. 2018, 39, 675–686. [Google Scholar] [CrossRef]
- Wakefield, E.O.; Pantaleao, A.; Popp, J.M.; Dale, L.P.; Santanelli, J.P.; Litt, M.D.; Zempsky, W.T. Describing Perceived Racial Bias Among Youth With Sickle Cell Disease. J. Pediatr. Psychol. 2018, 43, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Power-Hays, A.; McGann, P.T. When Actions Speak Louder Than Words-Racism and Sickle Cell Disease. N. Engl. J. Med. 2020, 383, 1902–1903. [Google Scholar] [CrossRef] [PubMed]
- Desai, P.; Little, J.; Kanter, J.; Bridges, K.; Andemariam, B.; Lanzkron, S. Kneeling Was the First Step for Sickle Cell Disease. Ann. Intern. Med. 2021, 174, 1004–1005. [Google Scholar] [CrossRef]
- Anderson, D.; Lien, K.; Agwu, C.; Ang, P.S.; Abou Baker, N. The Bias of Medicine in Sickle Cell Disease. J. Gen. Intern. Med. 2023, 38, 3247–3251. [Google Scholar] [CrossRef]
- Haywood, C., Jr.; Beach, M.C.; Lanzkron, S.; Strouse, J.J.; Wilson, R.; Park, H.; Witkop, C.; Bass, E.B.; Segal, J.B. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J. Natl. Med. Assoc. 2009, 101, 1022–1033. [Google Scholar] [CrossRef]
- Wickersham, K.E.; Dawson, R.M.; Becker, K.P.; Everhart, K.C.; Miles, H.S.; Schultz, B.E.; Tucker, C.M.; Wright, P.J.; Jenerette, C.M. Experiences of African Americans Living With Sickle Cell Disease. J. Transcult. Nurs. 2022, 33, 334–345. [Google Scholar] [CrossRef]
- Mulchan, S.S.; Theriault, C.B.; DiVietro, S.; Litt, M.D.; Sukhera, J.; Tanabe, P.; Thomas, H.R.; Zempsky, W.T.; Boruchov, D.; Hirsh, A.T. Provider Implicit Racial Bias in Pediatric Sickle Cell Disease. J. Racial Ethn. Health Disparities 2024, 12, 2743–2751. [Google Scholar] [CrossRef] [PubMed]
- Farooq, F.; Mogayzel, P.J.; Lanzkron, S.; Haywood, C.; Strouse, J.J. Comparison of US Federal and Foundation Funding of Research for Sickle Cell Disease and Cystic Fibrosis and Factors Associated With Research Productivity. JAMA Netw. Open 2020, 3, e201737. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; Boulware, L.E. Combating Racism Through Research, Training, Practice, and Public Health Policies. Prev. Chronic Dis. 2023, 20, E54. [Google Scholar] [CrossRef]
- Durham Walker, C.; McCray, G.G.; Wimes, A.; Levine, D.; Rivers, D. Training Medical Students to Recognize, Understand, and Mitigate the Impact of Racism in a Service-Learning Course. Prev. Chronic Dis. 2023, 20, E41. [Google Scholar] [CrossRef] [PubMed]
- Crump, A.; Al-Jorani, M.S.; Ahmed, S.; Abrol, E.; Jain, S. Implicit bias assessment by career stage in medical education training: A narrative review. BMC Med. Educ. 2025, 25, 137. [Google Scholar] [CrossRef]
- van Ryn, M.; Hardeman, R.; Phelan, S.M.; Burgess, D.J.; Dovidio, J.F.; Herrin, J.; Burke, S.E.; Nelson, D.B.; Perry, S.; Yeazel, M.; et al. Medical School Experiences Associated with Change in Implicit Racial Bias Among 3547 Students: A Medical Student CHANGES Study Report. J. Gen. Intern. Med. 2015, 30, 1748–1756. [Google Scholar] [CrossRef]
| Overall | MUSC | UNC | p-Value | |
|---|---|---|---|---|
| Number of Subjects | 98 | 61 | 37 | |
| Year | <0.001 | |||
| MS2 | 32 (33%) | 31 (51%) | 1 (3%) | |
| MS3 | 33 (34%) | 21 (34%) | 12 (32%) | |
| MS4 | 33 (34%) | 9 (15%) | 25 (68%) | |
| Gender | 1.000 | |||
| Female | 67 (68%) | 42 (69%) | 25 (68%) | |
| Male | 29 (30%) | 18 (30%) | 11 (30%) | |
| Other | 2 (2%) | 1 (2%) | 1 (3%) | |
| Race | 0.695 | |||
| White | 57 (61%) | 37 (64%) | 20 (56%) | |
| Black/AA | 12 (13%) | 8 (14%) | 4 (11%) | |
| White/AA | 2 (2%) | 1 (2%) | 1 (3%) | |
| Asian | 22 (23%) | 11 (19%) | 11 (31%) | |
| Other | 1 (1%) | 1 (2%) | 0 (0%) | |
| Ethnicity | 0.471 | |||
| Latinx/Hispanic | 8 (8%) | 4 (7%) | 4 (11%) | |
| Non-Hispanic | 90 (92%) | 57 (93%) | 33 (89%) | |
| Exposure to SCD | ||||
| Training/Workshop = Yes (%) | 23 (24%) | 20 (33%) | 3 (8%) | 0.006 |
| Personal Experience = Yes (%) | 5 (5.%) | 4 (7%) | 1 (3%) | 0.647 |
| Education Exposure, Readings, Lectures = Yes (%) | 97 (99%) | 60 (98%) | 37 (100%) | 1.000 |
| Media = Yes (%) | 34 (35%) | 20 (33%) | 14 (38%) | 0.665 |
| Other = Yes (%) | 5 (5%) | 3 (5%) | 2 (5%) | 1.000 |
| Career Goal | 0.652 | |||
| Primary Care | 48 (50%) | 28 (47%) | 20 (54%) | |
| Subspecialty Care | 20 (21%) | 12 (20%) | 8 (22%) | |
| Surgical | 29 (30%) | 20 (33%) | 9 (24%) |
| Overall: Mean (SD) | p-Value | |
|---|---|---|
| Knowledge of Treatment | ||
| Acute Pain | 3.06 (0.98) | <0.001 |
| Acute Stroke | 2.74 (1.07) | |
| Pregnancy | 2.16 (0.96) | |
| Acute Chest Syndrome | 2.79 (1.06) | |
| Outpatient Management | 2.94 (1.00) | |
| Comfort in Treatment | ||
| Acute Pain | 3.30 (0.91) | <0.001 |
| Acute Stroke | 2.86 (1.01) | |
| Pregnancy | 2.24 (0.92) | |
| Acute Chest Syndrome | 2.86 (0.99) | |
| Outpatient Management | 2.84 (0.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abrams, C.M.; Witherspoon, D.; Keller, E.; Picca, A.J.; Boucher, M. Knowledge, Confidence, and Comfort Regarding Sickle Cell Disease Among Medical Students: A Pilot Study in Two Universities. Healthcare 2025, 13, 1909. https://doi.org/10.3390/healthcare13151909
Abrams CM, Witherspoon D, Keller E, Picca AJ, Boucher M. Knowledge, Confidence, and Comfort Regarding Sickle Cell Disease Among Medical Students: A Pilot Study in Two Universities. Healthcare. 2025; 13(15):1909. https://doi.org/10.3390/healthcare13151909
Chicago/Turabian StyleAbrams, Christina M., DeAsia Witherspoon, Everette Keller, Andrew J. Picca, and Maria Boucher. 2025. "Knowledge, Confidence, and Comfort Regarding Sickle Cell Disease Among Medical Students: A Pilot Study in Two Universities" Healthcare 13, no. 15: 1909. https://doi.org/10.3390/healthcare13151909
APA StyleAbrams, C. M., Witherspoon, D., Keller, E., Picca, A. J., & Boucher, M. (2025). Knowledge, Confidence, and Comfort Regarding Sickle Cell Disease Among Medical Students: A Pilot Study in Two Universities. Healthcare, 13(15), 1909. https://doi.org/10.3390/healthcare13151909






