Effects of 12-Week Infant Shantala Massage Program on Maternal Emotional Well-Being Following First-Time Birth
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
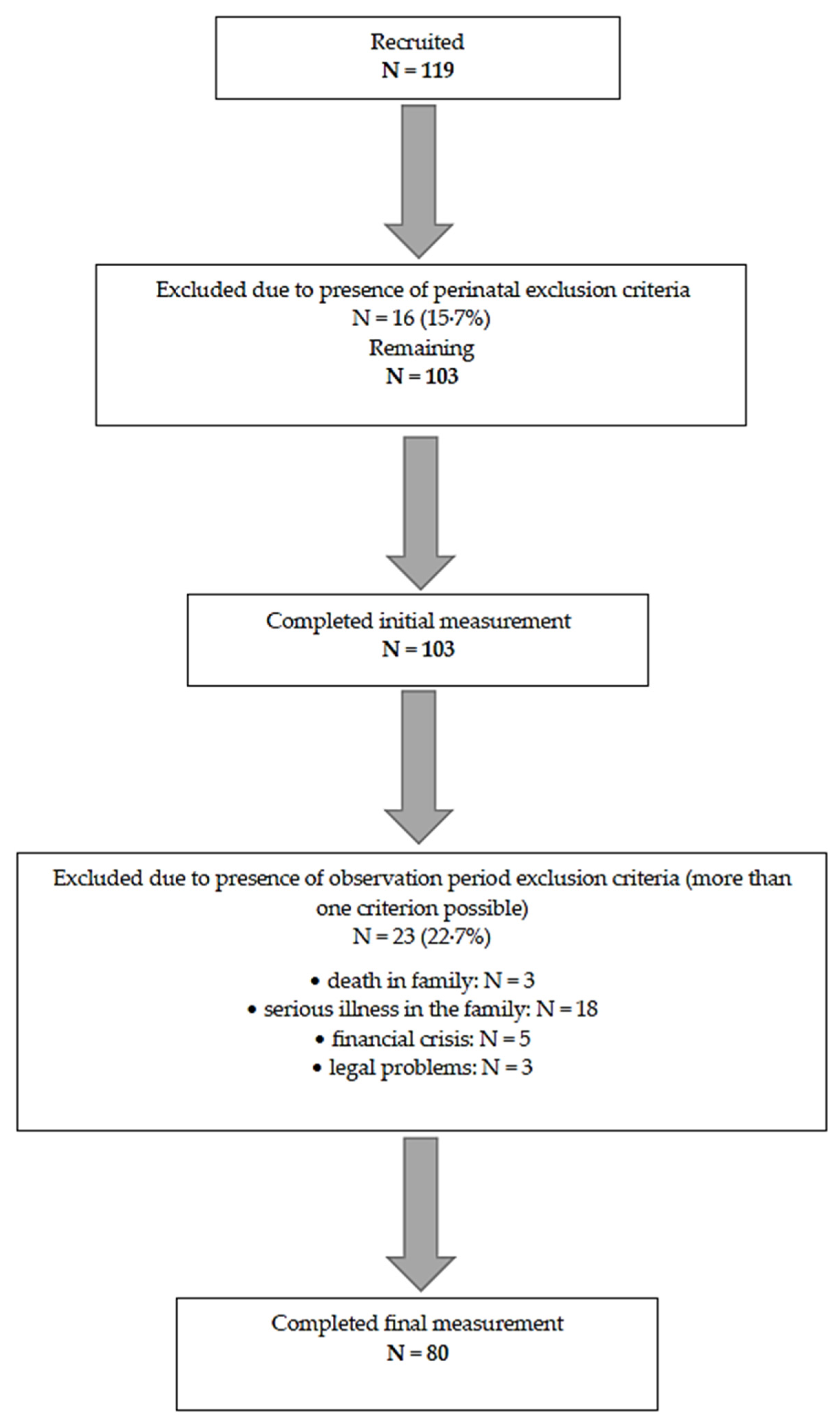
2.2. Participants
2.3. Measurements
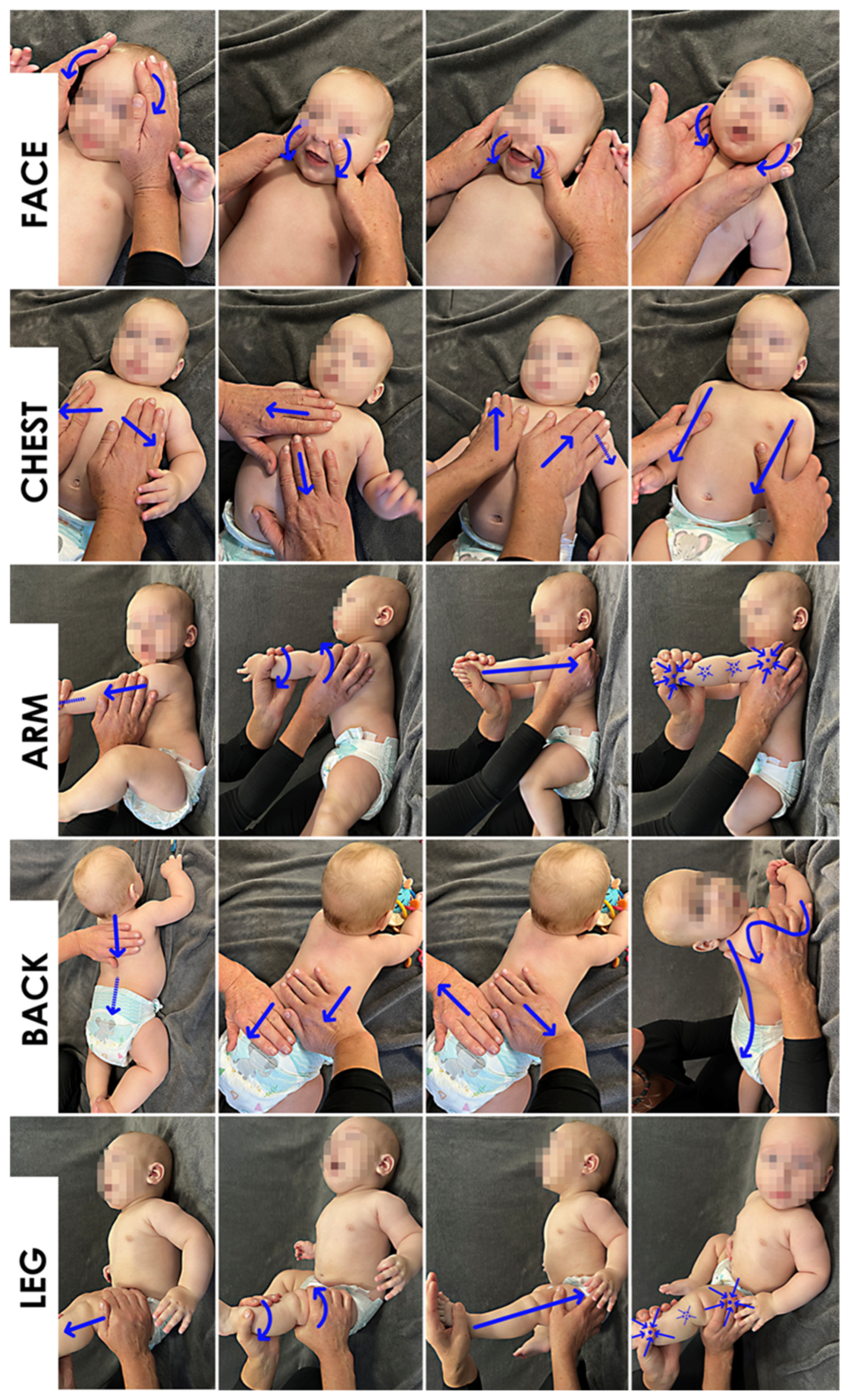
2.4. Procedure
2.5. Data Management
2.6. Statistical Analysis
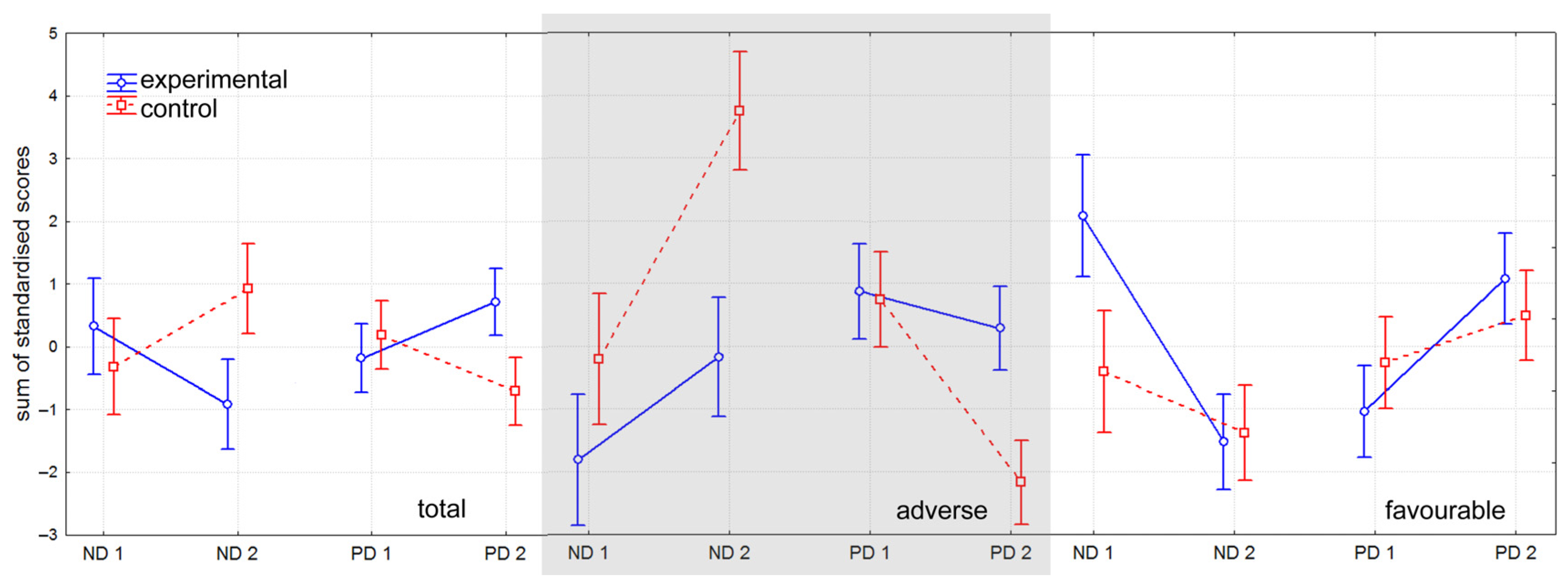
3. Results
3.1. Internal Consistency
3.2. Cluster Analysis
3.3. Control Group Selection
3.4. Descriptive Statistics and Analysis of Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PES | Postnatal emotional status |
| PPD | Postpartum depression |
| EPDS | Edinburgh Postnatal Depression Scale |
| HADS | Hospital Depression and Anxiety Scale |
| PANAS | Positive and Negative Affect Schedule |
| PSOC | Parenting Sense of Competence |
References
- Di Blasio, P.; Miragoli, S.; Camisasca, E.; Di Vita, A.M.; Pizzo, R.; Pipitone, L. Emotional distress following childbirth: An intervention to buffer depressive and PTSD symptoms. Eur. J. Psychol. 2015, 11, 214–232. [Google Scholar] [CrossRef]
- Stewart, D.E.; Vigod, S. Postpartum Depression. N. Engl. J. Med. 2016, 375, 2177–2186. [Google Scholar] [CrossRef]
- Adrianto, N.; Caesarlia, J.; Pajala, F. Depression in pregnant and postpartum women during COVID-19 pandemic: Systematic review and meta-analysis. Obs. Gynecol. Sci. 2022, 65, 287–302. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services. Available online: https://www.who.int/publications/i/item/9789240057142 (accessed on 21 December 2023).
- Burleson, M.; Quigley, K. Social interoception and social allostasis through touch: Legacy of the somatovisceral afference model of emotion. Soc. Neurosci. 2021, 16, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Suryawanshi, O.; Pajai, S. A comprehensive review on postpartum depression. Cureus 2022, 14, e32745. [Google Scholar] [CrossRef]
- Genova, F.; Tambell, R.; Marzilli, E. Parental postnatal depression in the time of the COVID-19 pandemic: A systematic review of its effects on the parent-child relationship and the child’s developmental outcomes. Int. J. Environ. Res. Public Health 2023, 20, 2018. [Google Scholar] [CrossRef]
- Friedman, S.H.; Reed, E.; Ross, N.E. Postpartum psychosis. Curr. Psychiatry Rep. 2023, 25, 65–72. [Google Scholar] [CrossRef]
- Watson, D.; Naragon-Gainey, K. On the specificity of positive emotional dysfunction in psychopathology: Evidence from the mood and anxiety disorders and schizophrenia/schizotypy. Clin. Psychol. Rev. 2010, 30, 839–848. [Google Scholar] [CrossRef]
- Pingeton, B.C.; Cochran, A.; Goodman, S.H.; Laurent, H.; Sbrilli, M.D.; Knight, B.; Newport, D.J.; Stowe, Z.N. Positive affect improves a transdiagnostic model of perinatal depression symptoms. J. Affect. Disord. 2023, 336, 112–119. [Google Scholar] [CrossRef]
- Chen, S.Y.; Zhao, W.W.; Cheng, Y.; Bian, C.; Yan, S.R.; Zhang, Y.H. Effects of positive psychological interventions on positive and negative emotions in depressed individuals: A systematic review and meta-analysis. J. Ment. Health 2025, 34, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Saboor, S.; Medina, A.; Marciano, L. Application of positive psychology in digital interventions for children, adolescents, and young adults: Systematic review and meta-analysis of controlled trials. JMIR Ment. Health 2024, 11, e56045. [Google Scholar] [CrossRef]
- Scroggins, J.; Ledbetter, L.; Jones-Hepler, B.; Brandon, D.; Reuter-Rice, K. Postpartum symptom clusters in birthing individuals: A systematic review. J. Clin. Nurs. 2023, 32, 4419–4440. [Google Scholar] [CrossRef]
- Buttner, M.; O’Hara, M.; Watson, D. The structure of women’s mood in the early postpartum. Assessment 2012, 19, 247–256. [Google Scholar] [CrossRef]
- Pritchett, R.V.; Daley, A.J.; Jolly, K. Does aerobic exercise reduce postpartum depressive symptoms?: A systematic review and meta-analysis. Br. J. Gen. Pract. 2017, 67, e684–e691. [Google Scholar] [CrossRef] [PubMed]
- Blamey, R.V.; Daley, A.J.; Jolly, K. Exercise for postnatal psychological outcomes: A systematic review and meta-analysis. Lancet 2012, 380, 25. [Google Scholar] [CrossRef]
- Kempler, L.; Sharpe, L.; Miller, C.B.; Bartlett, D.J. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Med. Rev. 2016, 29, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.V.E.; Wilson, C.A.; Ayre, K.; Robertson, L.; South, E.; Molyneaux, E.; Trevillion, K.; Howard, L.M.; Khalifeh, H. Antidepressant treatment for postnatal depression. Cochrane Database Syst. Rev. 2021, 2, CD013560. [Google Scholar] [CrossRef]
- Doren, F.M.; Raies, C.L.; Martínez, S.R. Significado de ser madre e hijo/a por medio del masaje. Rev. Esc. Enferm. 2014, 48, 415–422. [Google Scholar] [CrossRef]
- Dehkordi, Z.B.; Hosseini-Baharanchi, F.; Kazemian, A.; Madiseh, M.R.; Reisi, M.; Motaghi, B. The effects of infant massage on maternal postpartum depression: A randomized controlled trial. Nurs. Midwifery 2019, 8, 28–33. [Google Scholar] [CrossRef]
- O’Higgins, M.; Roberts, I.S.J.; Glover, V. Postnatal depression and mother and infant outcomes after infant massage. J. Affect. Disord. 2008, 109, 189–192. [Google Scholar] [CrossRef]
- Onozawa, K.; Glover, V.; Adams, D.; Modi, N.; Kumar, R.C. Infant massage improves mother-infant interaction for mothers with postnatal depression. J. Affect. Disord. 2001, 63, 201–207. [Google Scholar] [CrossRef]
- Moussa, S.; Fawaz, L.; Ibrahim, W.; Fathelbab, E.M.; Mostafa, A.M. Effect of infant massage on salivary oxytocin level of mothers and infants with normal and disordered bonding. J. Prim. Care Community Health 2021, 12, 21501327211012942. [Google Scholar] [CrossRef] [PubMed]
- Arifin, W.N. Sample Size Calculator. Available online: http://wnarifin.github.io (accessed on 10 May 2024).
- Gnat, R.; Gogola, A.; Matyja, M. Two opposite directions of emotional transformation are present in women after first physiological delivery. Ment. Health Rev. J. 2025, 30, 102–116. [Google Scholar] [CrossRef]
- Lanes, A.; Kuk, J.L.; Tamim, H. Prevalence and characteristics of postpartum depression symptomatology among Canadian women: A cross-sectional study. BMC Public Health 2011, 11, 302. [Google Scholar] [CrossRef]
- Kossakowska, K. Edynburska skala depresji poporodowej: Właściwości psychometryczne i charakterystyka. Acta Univ. Lodz. Folia Psychol. 2013, 17, 39–50. [Google Scholar] [CrossRef]
- Majkowicz, M. Praktyczna ocena efektywności opieki paliatywnej—Wybrane techniki badawcze. In Ocena JakośCi Opieki Paliatywnej w Teorii i Praktyce; de Walden-Gałuszko, K., Majkowicz, M., Eds.; Wydawnictwo Akademii Medycznej w Gdańsku: Gdańsk, Poland, 2000; pp. 6–34. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Fajkowska, M.; Marszał-Wiśniewska, M. Właściwości psychometryczne Skali Pozytywnego i Negatywnego Afektu wersja rozszerzona (PANAS-X). Wstępne wyniki badań w polskiej próbie. Przegląd Psychol. 2009, 4, 355–387. [Google Scholar]
- Gibaud-Wallston, J.; Wandersman, L.P. Parental sense of competence scale. In Handbook of Family Measurement Techniques; Touliatos, J., Perlmutter, B.F., Straus, A.S., Eds.; Sage: Thousand Oaks, CA, USA, 2001; p. 315. [Google Scholar]
- Kossakowska, K. Charakterystyka i ocena właściwości psychometrycznych polskiej adaptacji Skali Poczucia Kompetencji Rodzicielskich (Parenting Sense of Competence Scale—PSOC-PL) w wersji dla matek. Acta Univ. Lodz. Folia Psychol. 2017, 21, 79–95. [Google Scholar] [CrossRef]
- Windhorst, D.A.; Klein Velderman, M.; van der Pal, S.; de Weerth, C. The effects and process of the intervention “Individual Shantala Infant Massage” in preventive child healthcare to improve parent-child interaction: Study protocol for a quasi-experimental study. BMC Complement. Med. Ther. 2023, 23, 231. [Google Scholar] [CrossRef]
- Howard, L.; Khalifeh, H. Perinatal mental health: A review of progress and challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Education: Hoboken, NJ, USA, 2009. [Google Scholar]
- Liu, S.; Yan, Y.; Gao, X.; Xiang, S.; Sha, T.; Zeng, G.; He, Q. Risk factors for postpartum depression among Chinese women: Path model analysis. BMC Pregnancy Childbirth 2017, 17, 133. [Google Scholar] [CrossRef]
- Ghaedrahmati, M.; Kazemi, A.; Kheirabadi, G.; Ebrahimi, A.; Bahrami, M. Postpartum depression risk factors: A narrative review. J. Educ. Health Promot. 2017, 6, 60. [Google Scholar] [CrossRef]
- Skrundz, M.; Bolten, M.; Nast, I.; Hellhammer, D.H.; Meinlschmidt, G. Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression. Neuropsychopharmacology 2011, 36, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Brummelte, S.; Galea, L. Postpartum depression: Etiology, treatment and consequences for maternal care. Horm. Behav. 2016, 77, 153–166. [Google Scholar] [CrossRef]
- Khazanov, G.; Ruscio, A. Is low positive emotionality a specific risk factor for depression? A meta-analysis of longitudinal studies. Psychol. Bull. 2016, 142, 991–1015. [Google Scholar] [CrossRef]
- Pepino, V.C.; Mezzacappa, M.A. Application of tactile/kinesthetic stimulation in preterm infants: A systematic review. J. Pediatr. 2015, 91, 213–233. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gnazzo, A.; Guerriero, V.; Di Folco, S.; Zavattini, G.C.; De Campora, G. Skin to skin interactions. Does the infant massage improve the couple functioning? Front. Psychol. 2015, 6, 1468. [Google Scholar] [CrossRef] [PubMed]
- Mrljak, R.; Danielsson, A.A.; Hedov, G.; Garmy, P. Effects of infant massage: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 6378. [Google Scholar] [CrossRef]

| Mean ± SD (Min–Max) or Number (%) | |
|---|---|
| age (years) | 30.95 ± 4.58 (20.00–40.00) |
| body height (m) | 1.67 ± 0.06 (1.55–1.80) |
| body mass index (kg/m2) | 27.51 ± 2.48 (22.86–33.46) |
| secondary: 14 (17.50) | |
| education level | high: 66 (82.50) |
| yes: 14 (17.50) | |
| pregnancy planning | no: 66 (82.50) |
| Subscale | Maximal Score (Points) | Interpretation | Polish Adaptation Validity Metrics | |
|---|---|---|---|---|
| The Edinburgh Postnatal Depression Scale [26] | none | 30 | ≥13 = risk of depression | Cronbach’s alpha 0.91 sensitivity 96% specificity 93% [27] |
| The Hospital Anxiety | depression | 21 | ≥11 = severe disorder | Cronbach’s alpha 0.85 [28] |
| and Depression Scale [29] | anxiety | 21 | ≥11 = severe disorder | Cronbach’s alpha 0.81 [28] |
| Positive and | negative affect | 50 | ≥20 = strong affect | |
| Negative Affect Schedule [30] | positive affect | 50 | ≥30 = strong affect | Cronbach’s alpha 0.86 [31] |
| Parenting Sense | satisfaction | 54 | ≥35 = high satisfaction | Cronbach’s alpha 0.84 [33] |
| of Competence [32] | effectiveness | 48 | ≥31 = high effectiveness |
| Adverse PES | Favorable PES | ||
|---|---|---|---|
| Mean ± SD (Min–Max) | Mean ± SD (Min–Max) | p Adverse | |
| or Number (%) | or Number (%) | vs. Favorable | |
| number | 36 | 44 | .. |
| age (years) | 30.83 ± 4.42 (23.00–39.00) | 31.04 ± 4.75 (20.00–40.00) | 0.83 ! |
| body height (m) | 1.66 ± 0.05 (1.57–1.80) | 1.68 ± 0.06 (1.55–1.80) | 0.16 ! |
| body mass index (kg/m2) | 27.35 ± 2.39 (23.03–32.83) | 27.63 ± 2.57 (22.86–33.46) | 0.61 ! |
| secondary: 8 (22.22) | secondary: 6 (13.64) | ||
| education level | high: 28 (77.78) | high: 38 (86.36) | 0.32 † |
| yes: 6 (16.67) | yes: 8 (18.18) | ||
| pregnancy planning | no: 30 (83.33) | no: 36 (81.82) | 0.86 † |
| Experimental | Control | ||
|---|---|---|---|
| Mean ± SD (Min–Max) | Mean ± SD (Min–Max) | p Experimental | |
| or Number (%) | or Number (%) | vs. Control | |
| number | 80 (100) | 80 (100) | .. |
| age (years) | 30.95 ± 4.58 (20.00–40.00) | 29.99 ± 4.24 (19.00–40.00) | 0.17 ! |
| body height (m) | 1.67 ± 0.06 (1.55–1.80) | 1.67 ± 0.05 (1.52–1.78) | 0.61 ! |
| body mass index (kg/m2) | 27.51 ± 2.48 (22.86–33.46) | 27.04 ± 3.91(20.41–37.10) | 0.36 ! |
| postnatal emotional | adverse: 36 (45) | adverse: 36 (45) | |
| status changes | favorable: 44 (55) | favorable: 36 (55) | .. |
| vocational: 0 (0.00) | 2 (2.50) | ||
| secondary: 14 (17.50) | secondary: 14 (17.50) | ||
| education level | high: 66 (82.50) | high: 64 (80.00) | 0.25 † |
| yes: 14 (17.50) | yes: 16 (17.50) | ||
| pregnancy planning | no: 66 (82.50) | no: 64 (82.50) | 0.68 † |
| p | p | p Experimental | ||||
|---|---|---|---|---|---|---|
| Experimental | 1 vs. 2 | Control | 1 vs. 2 | vs. Control | ||
| 1 | 8.75 ± 4.99 [0–28] | 9.21 ± 4.02 [0–18] | 0.15 † | |||
| 2 | 7.11 ± 4.25 [0–18] | 0.01 ^* | 9.03 ± 4.64 [0–22] | 0.73 ! | 0.01 †* | |
| EPDS | Δ | −1.64 (−2.80–−0.47) | −0.19 (−1.25–0.88) | 0.07 † | ||
| 1 | 6.40 ± 4.06 [0–15] | 5.20 ± 3.16 [0–12] | 0.12 † | |||
| 2 | 4.30 ± 3.04 [0–15] | <0.01 ^* | 5.35 ± 3.23 [0–13] | 0.76 ^ | 0.03 †* | |
| HADS (dep) | Δ | −2.10 (−3.01–−1.19) | 0.15 (−0.52–0.82) | <0.01 †* | ||
| 1 | 4.69 ± 3.15 [0–12] | 3.76 ± 3.14 [0–12] | 0.06 † | |||
| 2 | 2.59 ± 2.48 [0–8] | <0.01 ^* | 4.72 ± 3.27 [0–14] | 0.02 ^* | <0.01 †* | |
| HADS (anx) | Δ | −2.10 (−2.83–−1.37) | 0.96 (0.22–1.71) | <0.01 !* | ||
| 1 | 23.44 ± 6.79 [13–49] | 22.55 ± 7.30 [10–39] | 0.47 † | |||
| 2 | 19.35 ± 5.98 [7–38] | <0.01 ^* | 22.07 ± 7.34 [8–38] | 0.76 ^ | 0.02 †* | |
| PANAS (neg) | Δ | −4.09 (−5.85–−2.32) | −0.47 (−2.16–1.21) | <0.01 †* | ||
| 1 | 37.45 ± 5.72 [22–49] | 36.80 ± 6.42 [22–48] | 0.50 ! | |||
| 2 | 41.50 ± 4.94 [30–50] | <0.01 ^* | 37.58 ± 6.02 [21–49] | 0.29 ! | <0.01 †* | |
| PANAS (pos) | Δ | 4.05 (2.82–5.28) | 0.78 (−0.66–2.21) | <0.01 !* | ||
| 1 | 34.90 ± 5.58 [22–46] | 35.26 ± 6.85 [16–48] | 0.55! | |||
| 2 | 38.04 ± 6.26 [21–49] | <0.01 ^* | 35.21 ± 5.66 [24–48] | 0.99 ^ | <0,01 †* | |
| PSOC (sat) | Δ | 3.14 (1.42–4.85) | −0.05 (−1.38–1.28) | <0.01 !* | ||
| 1 | 25.63 ± 4.74 [17–38] | 27.71 ± 5.07 [16–41] | 0.01 †* | |||
| 2 | 29.53 ± 5.62 [19–43] | <0.01 ^* | 27.86 ± 5.75 [18–40] | 0.94 ^ | 0.03 †* | |
| PSOC (effect) | Δ | 3.90 (2.81–4.99) | 0.15 (−1.28–1.58) | <0.01 !* |
| p | p | p Experimental | ||||
|---|---|---|---|---|---|---|
| Experimental | 1 vs. 2 | Control | 1 vs. 2 | vs. Control | ||
| 1 | 6.28 ± 2.80 [0–12] | 9.42 ± 4.37 [0–18] | <0.01 !* | |||
| 2 | 7.69 ± 4.41 [1–18] | 0.04 !* | 12.28 ± 3.44 [6–22] | <0.01 ^* | <0.01 †* | |
| EPDS | Δ | 1.42 (0.01–2.82) | 2.86 (1.34–4.39) | 0.14 † | ||
| 1 | 4.11 ± 3.27 [0–13] | 5.42 ± 3.50 [0–11] | 0.10 † | |||
| 2 | 4.89 ± 3.33 [1–15] | 0.06 ^ | 7.03 ± 3.12 [2–13] | <0.01 ^* | 0.01 †* | |
| HADS (dep) | Δ | 0.78 (−0.26–1.82) | 1.61 (0.68–2.54) | 0.35 † | ||
| 1 | 2.64 ± 2.36 [0–10] | 3.69 ± 3.24 [0–11] | 0.26 † | |||
| 2 | 2.89 ± 2.63 [0–8] | 0.38 ^ | 6.94 ± 2.80 [1–14] | <0.01 ^* | <0.01 †* | |
| HADS (anx) | Δ | 0.25 (−0.73–1.23) | 3.25 (2.23–4.27) | <0.01 †* | ||
| 1 | 21.17 ± 4.61 [13–29] | 22.75 ± 7.74 [10–36] | 0.51 † | |||
| 2 | 21.61 ± 6.46 [12–38] | 0.71 ! | 27.92 ± 5.87 [16–38] | <0.01 ^* | <0.01 !* | |
| PANAS (neg) | Δ | 0.44 (−1.99–2.88) | 5.17 (3.57–6.76) | <0.01 !* | ||
| 1 | 40.17 ± 4.66 [30–49] | 38.06 ± 7.17 [22–48] | 0.14 ! | |||
| 2 | 42.06 ± 5.12 [30–50] | 0.02 !* | 34.50 ± 4.99 [21–42] | <0.01 !* | <0.01 !* | |
| PANAS (pos) | Δ | 1.89 (0.27–3.50) | −3.56 (−5.19–−1.92) | <0.01 !* | ||
| 1 | 37.72 ± 4.21 [27–45] | 36.36 ± 5.74 [27–47] | 0.39 † | |||
| 2 | 36.14 ± 6.79 [21–45] | 0.19 ^ | 32.58 ± 3.64 [24–40] | <0.01 ^* | 0.01 †* | |
| PSOC (sat) | Δ | −1.58 (−3.56–0.39) | −3.78 (−5.20–−2.36) | 0.07 † | ||
| 1 | 26.39 ± 4.24 [18–36] | 28.57 ± 5.10 [16–41] | 0.05 ! | |||
| 2 | 28.28 ± 5.11 [20–38] | 0.01 !* | 24.97 ± 2.87 [20–32] | <0.01 ^* | <0.01 !* | |
| PSOC (effect) | Δ | 1.89 (0.41–3.37) | −3.58 (−5.24–−1.93) | <0.01 !* |
| p | p | p Experimental | ||||
|---|---|---|---|---|---|---|
| Experimental | 1 vs. 2 | Control | 1 vs. 2 | vs. Control | ||
| 1 | 10.77 ± 5.49 [3–28] | 9.05 ± 3.75 [1–17] | 0.23 † | |||
| 2 | 6.64 ± 4.11 [0–15] | <0.01 ^* | 6.36 ± 3.72 [0–15] | <0.01 ^* | 0.88 † | |
| EPDS | Δ | −4.14 (−5.56–−2.71) | −2.68 (−3.71–−1.65) | 0.10 ! | ||
| 1 | 8.27 ± 3.69 [2–15] | 5.02 ± 2.89 [0–12] | <0.01 !* | |||
| 2 | 3.82 ± 2.73 [0–10] | <0.01 ^* | 3.98 ± 2.63 [0–11] | 0.01!* | 0.74 † | |
| HADS (dep) | Δ | −4.45 (−5.44–−3.47) | −1.05 (−1.87–−0.22) | <0.01 †* | ||
| 1 | 6.36 ± 2.71 [1–12] | 3.82 ± 3.09 [0–12] | <0.01 †* | |||
| 2 | 2.34 ± 2.36 [0–8] | <0.01 ^* | 2.91 ± 2.41 [0–9] | 0.01 ^* | 0.19 † | |
| HADS (anx) | Δ | −4.02 (−4.67–−3.37) | −0.91 (−1.61- −0.21) | <0.01 †* | ||
| 1 | 25.30 ± 7.71 [15–49] | 22.39 ± 7.01 [10–39] | 0.10 † | |||
| 2 | 17.50 ± 4.90 [7–27] | <0.01 ^* | 17.30 ± 4.3 [58–26] | <0.01!* | 0.84 ! | |
| PANAS (neg) | Δ | −7.80 (−9.76–−5.83) | −5.09 (−6.99–−3.19) | <0.01 †* | ||
| 1 | 35.23 ± 5.59 [22–47] | 35.77 ± 5.61 [25–48] | 0.65 ! | |||
| 2 | 41.05 ± 4.80 [31–49] | <0.01!* | 40.09 ± 5.65 [27–49] | <0.01 ^* | 0.55 † | |
| PANAS (pos) | Δ | 5.82 (4.14–7.50) | 4.32 (2.67–5.96) | 0.20 ! | ||
| 1 | 32.59 ± 5.53 [22–46] | 34.36 ± 7.59 [16–48] | 0.21 ! | |||
| 2 | 39.59 ± 5.38 [24–49] | <0.01 ^* | 37.36 ± 6.13 [25–48] | <0.01!* | 0.07 ! | |
| PSOC (sat) | Δ | 7.00 (4.90–9.10) | 3.00 (1.32–4.68) | <0.01 !* | ||
| 1 | 25.00 ± 5.08 [17–38] | 27.02 ± 5.01 [17–38] | 0.04 †* | |||
| 2 | 30.55 ± 5.86 [19–43] | <0.01 ^* | 30.23 ± 6.42 [18–40] | <0.01 ^* | 0.03 †* | |
| PSOC (effect) | Δ | 5.55 (4.10–6.99) | 3.20 (1.39–5.02) | 0.04 !* |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gogola, A.; Gnat, R. Effects of 12-Week Infant Shantala Massage Program on Maternal Emotional Well-Being Following First-Time Birth. Healthcare 2025, 13, 1895. https://doi.org/10.3390/healthcare13151895
Gogola A, Gnat R. Effects of 12-Week Infant Shantala Massage Program on Maternal Emotional Well-Being Following First-Time Birth. Healthcare. 2025; 13(15):1895. https://doi.org/10.3390/healthcare13151895
Chicago/Turabian StyleGogola, Anna, and Rafał Gnat. 2025. "Effects of 12-Week Infant Shantala Massage Program on Maternal Emotional Well-Being Following First-Time Birth" Healthcare 13, no. 15: 1895. https://doi.org/10.3390/healthcare13151895
APA StyleGogola, A., & Gnat, R. (2025). Effects of 12-Week Infant Shantala Massage Program on Maternal Emotional Well-Being Following First-Time Birth. Healthcare, 13(15), 1895. https://doi.org/10.3390/healthcare13151895






