The Impact of Perceived Quality on Patients’ Adoption and Usage of Online Health Consultations: An Empirical Study Based on Trust Theory
Abstract
1. Introduction
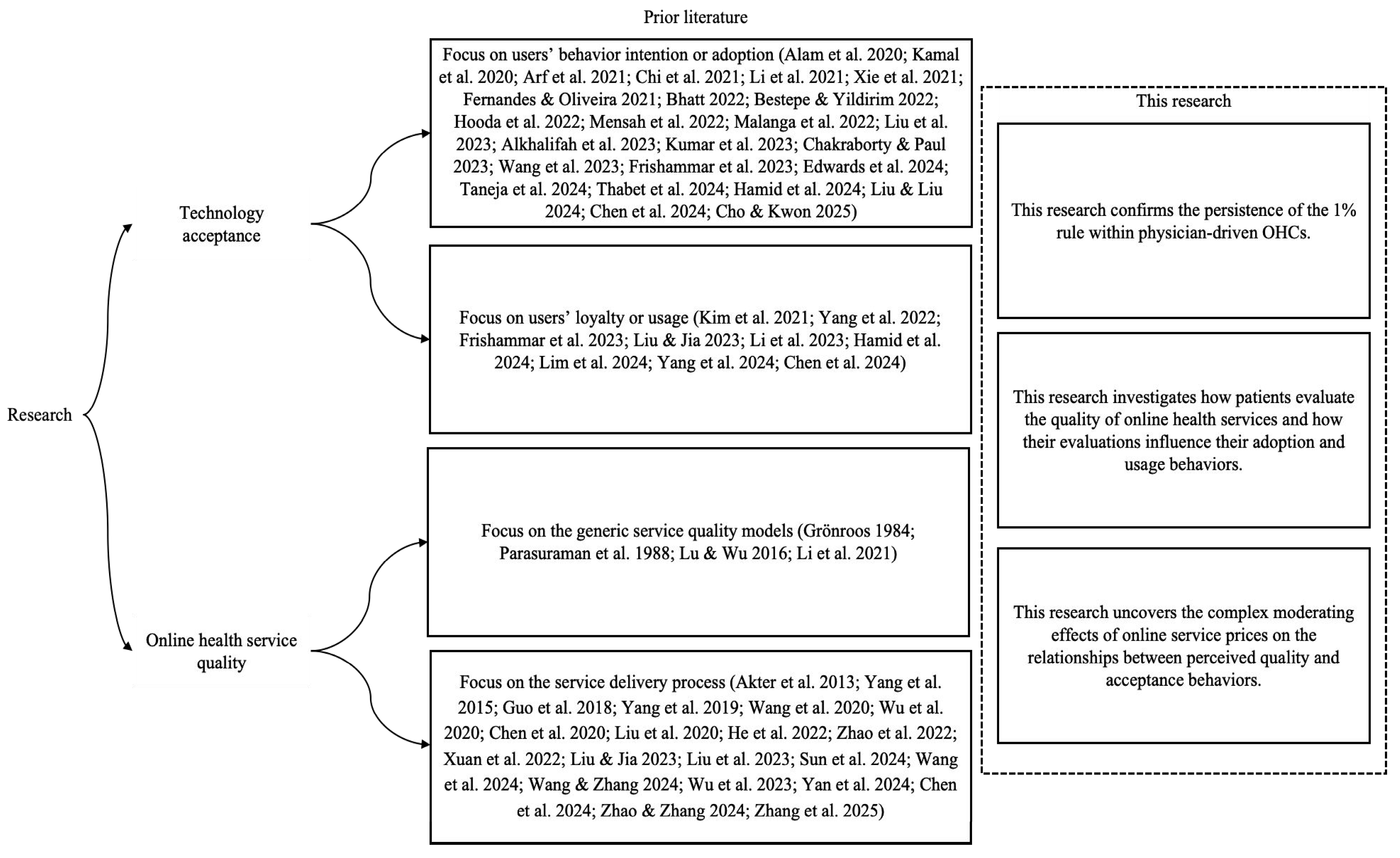
2. Literature Review and Theoretical Background
2.1. Online Health Service Quality
2.2. Technology Acceptance Behaviors and Motivations
2.3. Trust Theory
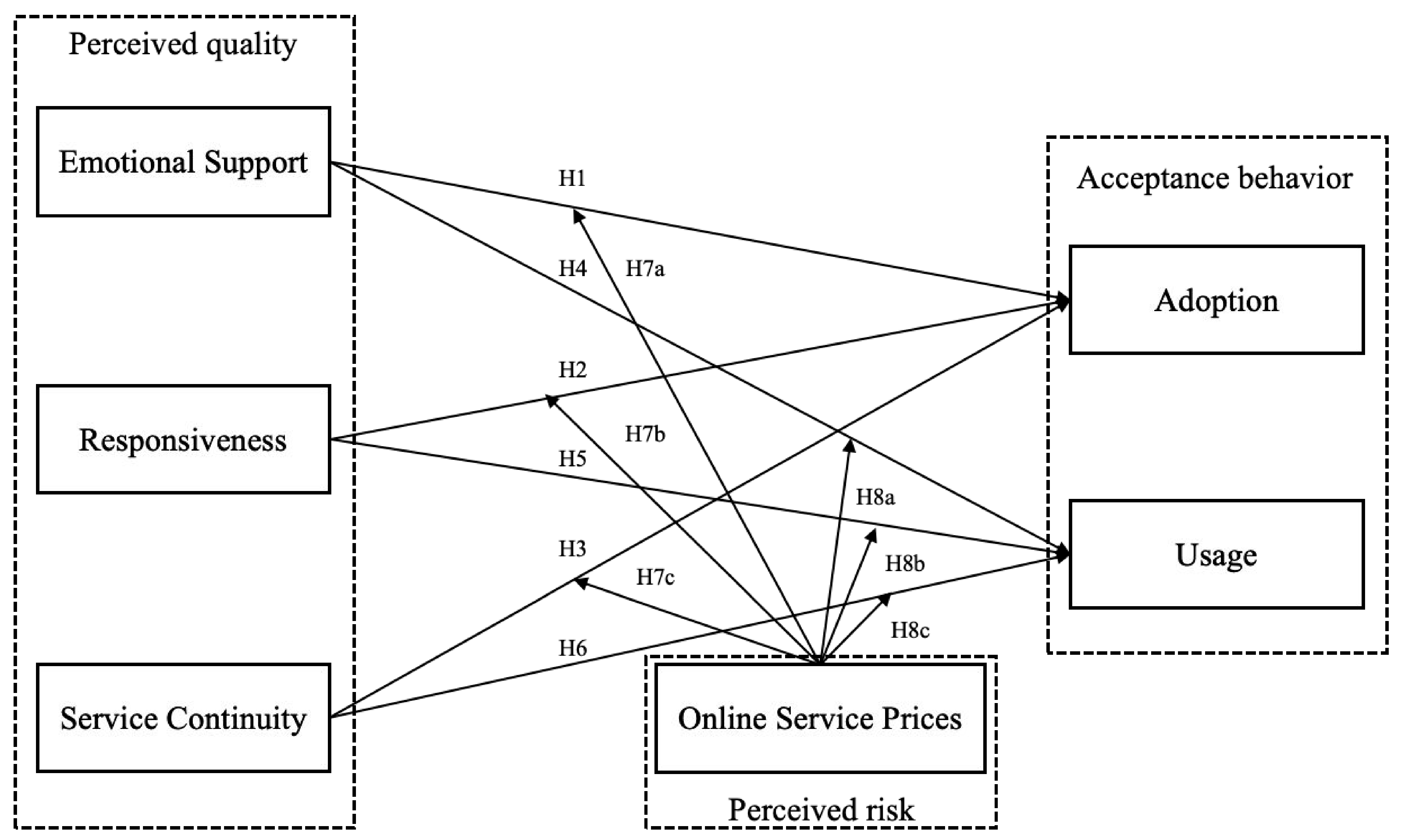
3. Hypothesis Development
3.1. The Effects of Physicians’ Perceived Quality on Patients’ Adoption of Online Health Consultations
3.2. The Effects of Physicians’ Perceived Quality on Patients’ Usage of Online Health Consultations
3.3. The Moderating Effects of Online Service Prices on the Relationships Between Perceived Quality and Acceptance Behaviors
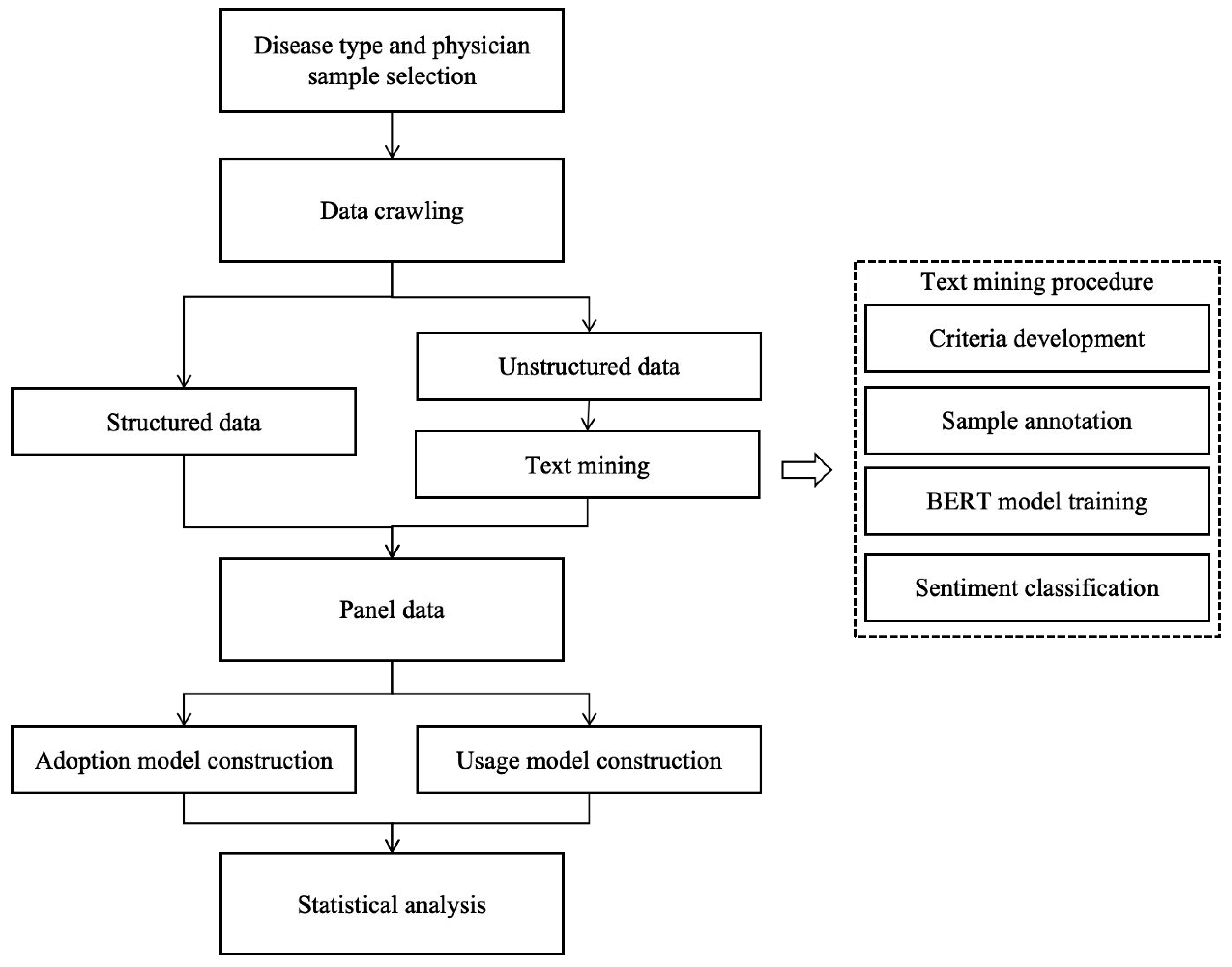
4. Research Methodology
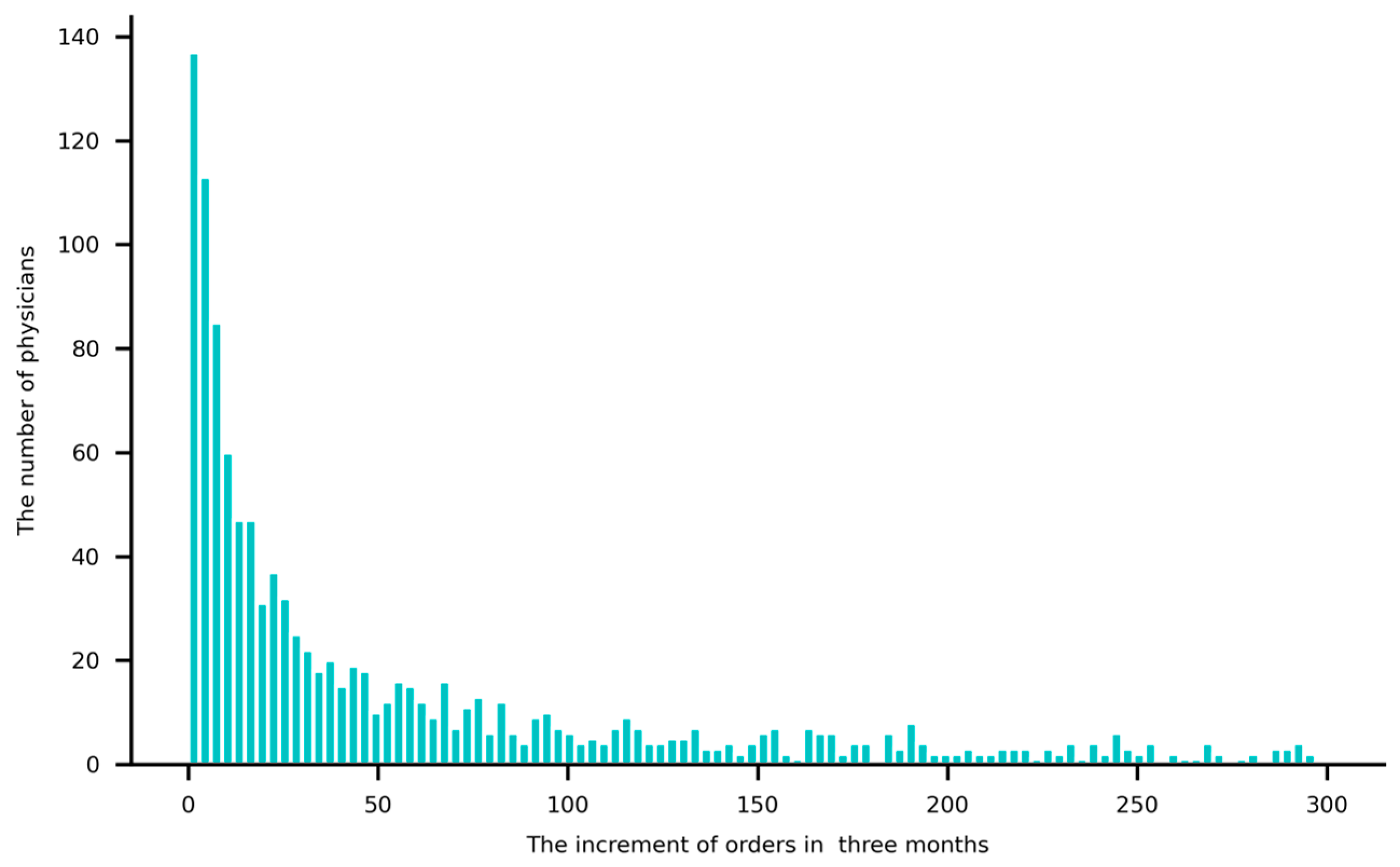
4.1. Research Context and Data Collection
4.2. Variable Measurement
4.2.1. Dependent Variables
4.2.2. Independent Variables
4.2.3. Moderator Variable
4.2.4. Control Variables
4.3. The Procedure of Text Mining
4.4. Model Construction
5. Result
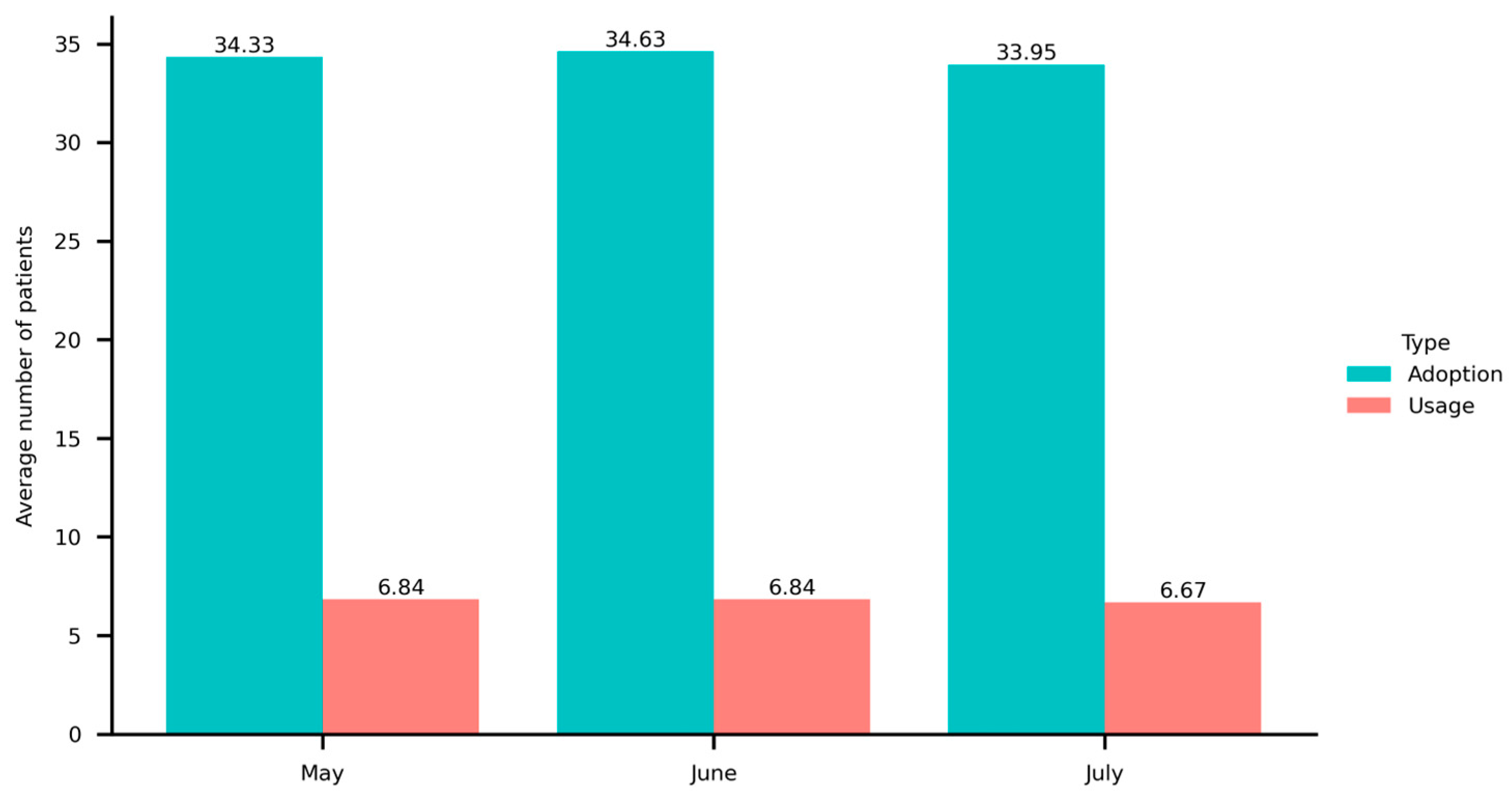
5.1. Descriptive Statistics and Correlations
5.2. Empirical Results
5.3. Robustness Check
6. Discussion and Implications
6.1. Discussion
6.2. Theoretical Implications
6.3. Practical Implications
6.4. Limitations and Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Criterion | Examples |
|---|---|
| Daily greetings | “Hello! Welcome to my online clinic.” “How’s it going these days?” |
| Positive comments on recovery outcomes | “Your situation has quite a bit of improvement” “You’re recovering well.” |
| Reassurance and encouragement | “Don’t worry!” “We’ll work together!” |
| Clarifications aimed at alleviating uncertainty regarding treatment modalities and recovery processes | “The success rate of this surgery is quite high” “It will improve over time.” |
Appendix B
| Variable | Min | Max | Mean | Std.Dev. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adoption | 0 | 2600 | 34.302 | 90.806 | 1 | ||||||||
| 2. Usage | 0 | 254 | 6.785 | 17.675 | 0.649 *** | 1 | |||||||
| 3. Emotional Support | 0 | 13.333 | 0.714 | 0.808 | 0.375 *** | 0.326 *** | 1 | ||||||
| 4. Responsiveness | 1 | 3 | 2.600 | 0.684 | 0.474 *** | 0.355 *** | 0.442 *** | 1 | |||||
| 5. Service Continuity | 0 | 1 | 0.408 | 0.401 | 0.494 *** | 0.286 *** | 0.073 *** | 0.231 *** | 1 | ||||
| 6. Price | 0 | 3000 | 138.560 | 194.704 | 0.249 *** | 0.135 *** | 0.133 *** | 0.164 *** | −0.025 | 1 | |||
| 7. Recommendation | 0 | 5 | 3.974 | 0.461 | 0.679 *** | 0.468 *** | 0.192 *** | 0.249 *** | 0.379 *** | 0.292 *** | 1 | ||
| 8. Article | 0 | 155 | 0.479 | 5.163 | 0.196 *** | 0.132 *** | 0.081 *** | 0.091 *** | 0.098 *** | 0.078 *** | 0.199 *** | 1 | |
| 9. Gift | 0 | 151 | 1.152 | 4.218 | 0.611 *** | 0.517 *** | 0.234 *** | 0.246 *** | 0.219 *** | 0.218 *** | 0.530 *** | 0.299 *** | 1 |
References
- Facts & Factors. Digital Health Market Size, Share, Industry Demand, Forecast Report 2032. Available online: https://www.fnfresearch.com/digital-health-market-report (accessed on 14 March 2025).
- Liu, X.; Liu, Q.B. Superior Medical Resources or Geographic Proximity? The Joint Effects of Regional Medical Resource Disparity, Geographic Distance, and Cultural Differences on Online Medical Consultation. Soc. Sci. Med. 2024, 350, 116911. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Deng, Z.; Wang, B.; Wu, T. Online Service Qualities in the Multistage Process and Patients’ Compliments: A Transaction Cycle Perspective. Inf. Manag. 2020, 57, 103230. [Google Scholar] [CrossRef]
- Qiu, C.; Zhang, Y.; Wang, X.; Gu, D. Trust-Based Research: Influencing Factors of Patients’ Medical Choice Behavior in the Online Medical Community. Healthcare 2022, 10, 938. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, X. Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective. Healthcare 2024, 12, 1113. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.-B.; Lu, Z.-Z.; Mu, L. Factors Influencing Proxy Online Health Information Seeking among the Elderly: A Study from the Perspective of the Elderly with Chronic Illnesses. THC 2024, 32, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Xi, N.; Gu, D.; Liang, C.; Li, H.; Tang, H.; Hamari, J. Medical Practice in Gamified Online Communities: Longitudinal Effects of Gamification on Doctor Engagement. Inf. Manag. 2024, 61, 103906. [Google Scholar] [CrossRef]
- Wang, B.; Asan, O.; Mansouri, M. Systems Approach in Telemedicine Adoption During and After COVID-19: Roles, Factors, and Challenges. IEEE Open J. Syst. Eng. 2023, 1, 38–49. [Google Scholar] [CrossRef]
- Hamid, S.; Roslan, M.H.H.; Norman, A.A.; Ghani, N.A. Acceptance and Use Behaviour of Emerging Technology for Middle-Aged Healthy Lifestyle. THC 2024, 32, 1535–1554. [Google Scholar] [CrossRef] [PubMed]
- Frishammar, J.; Essén, A.; Bergström, F.; Ekman, T. Digital Health Platforms for the Elderly? Key Adoption and Usage Barriers and Ways to Address Them. Technol. Forecast. Soc. Change 2023, 189, 122319. [Google Scholar] [CrossRef]
- Liu, J.Y.W.; Sorwar, G.; Rahman, M.S.; Hoque, M.R. The Role of Trust and Habit in the Adoption of mHealth by Older Adults in Hong Kong: A Healthcare Technology Service Acceptance (HTSA) Model. BMC Geriatr. 2023, 23, 73. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.Z.; Hoque, M.R.; Hu, W.; Barua, Z. Factors Influencing the Adoption of mHealth Services in a Developing Country: A Patient-Centric Study. Int. J. Inf. Manag. 2020, 50, 128–143. [Google Scholar] [CrossRef]
- Lim, X.-J.; Chang, J.Y.-S.; Cheah, J.-H.; Lim, W.M.; Kraus, S.; Dabic, M. Out of the Way, Human! Understanding Post-Adoption of Last-Mile Delivery Robots. Technol. Forecast. Soc. Change 2024, 201, 123242. [Google Scholar] [CrossRef]
- Cho, Y.; Kwon, G.H. Understanding Service Robot Adoption and Resistance from a Service Provider Perspective. Technol. Forecast. Soc. Change 2025, 210, 123885. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. Service Provision, Pricing, and Patient Satisfaction in Online Health Communities. Int. J. Med. Inform. 2018, 110, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Wang, Q.; Roh, T. Do Information and Service Quality Affect Perceived Privacy Protection, Satisfaction, and Loyalty? Evidence from a Chinese O2O-Based Mobile Shopping Application. Telemat. Inform. 2021, 56, 101483. [Google Scholar] [CrossRef]
- Liu, X.; Jia, X. Exploration of the Nonlinear Relationship between Social Support and the Establishment of Long-Term Doctor–Patient Relationships: An Empirical Analysis Based on Virtual Doctor Teams. Int. J. Med. Inform. 2023, 178, 105198. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.; Wu, H. Exploring the Impact of Word-of-Mouth about Physicians’ Service Quality on Patient Choice Based on Online Health Communities. BMC Med. Inf. Decis. Mak. 2016, 16, 151. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Jiang, J.; Kiang, M.; Yuan, F. Re-Examining the Impact of Multidimensional Trust on Patients’ Online Medical Consultation Service Continuance Decision. Inf. Syst. Front. 2022, 24, 983–1007. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Liu, Y.; Zhu, Z.; Hu, J.; Chen, X. Online Selection of a Physician by Patients: Empirical Study from Elaboration Likelihood Perspective. Comput. Hum. Behav. 2017, 73, 403–412. [Google Scholar] [CrossRef]
- Fan, H.; Lederman, R. Online Health Communities: How Do Community Members Build the Trust Required to Adopt Information and Form Close Relationships? Eur. J. Inf. Syst. 2018, 27, 62–89. [Google Scholar] [CrossRef]
- Wu, D.C.; Zhao, X.; Wu, J. Online Physician-Patient Interaction and Patient Satisfaction: Empirical Study of the Internet Hospital Service. J. Med. Internet Res. 2023, 25, e39089. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Deng, Z.; Li, X.; Fan, G. A Real Bargain: Understanding the Impacts of Short-Term Price Discounts on Physicians’ Health Service Sales on Online Health Platforms. Inf. Manag. 2025, 62, 104142. [Google Scholar] [CrossRef]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An Integrative Model of Organizational Trust. AMR 1995, 20, 709–734. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating Acceptance of Telemedicine Services through an Extended Technology Acceptance Model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Yang, X.; Gu, D.; Li, H.; Liang, C.; Jain, H.K.; Li, P. Mobile Health Community Loyalty Development Process in China: An Empirical Study from Information Seeking Perspective|Emerald Insight. Inf. Technol. People 2024, 37, 635–661. [Google Scholar] [CrossRef]
- Sun, W.; Guo, X.; Kwok, R.C.-W. Emotion or Information? Differences and Relationships between Two Types of Professional Support in Online Health Communities. Inf. Manag. 2024, 61, 103944. [Google Scholar] [CrossRef]
- Chen, Q.; Jin, J.; Yan, X. Impact of Online Physician Service Quality on Patients’ Adoption Behavior across Different Stages: An Elaboration Likelihood Perspective. Decis. Support Syst. 2024, 176, 114048. [Google Scholar] [CrossRef]
- Yan, J.; Liang, C.; Zhou, P. Physician’s Service Quality and Patient’s Review Behavior: Managing Online Review to Attract More Patients. Internet Res. 2024. ahead-of-print. [Google Scholar] [CrossRef]
- Wang, H.; Liu, S.; Gao, B.; Aziz, A. How Do Recommendations Influence Patient Satisfaction? Evidence from an Online Health Community. Inf. Technol. People 2024. ahead-of-print. [Google Scholar] [CrossRef]
- Liu, S.; Wang, H.; Gao, B.; Deng, Z. Doctors’ Provision of Online Health Consultation Service and Patient Review Valence: Evidence from a Quasi-Experiment. Inf. Manag. 2022, 59, 103360. [Google Scholar] [CrossRef]
- Zhang, Y.; Sun, F.; Zhang, X.; Ma, X. Are Multiple Information Sources Better? The Effect of Multiple Physicians in Online Medical Teams on Patient Satisfaction. Inf. Process. Manag. 2025, 62, 103889. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhu, L.; Wu, C.; Huang, S.; Wang, Q. Do the Rich Grow Richer? An Empirical Analysis of the Matthew Effect in an Online Healthcare Community. Electron. Commer. Res. Appl. 2022, 52, 101125. [Google Scholar] [CrossRef]
- Guo, S.; Guo, X.; Zhang, X.; Vogel, D. Doctor–Patient Relationship Strength’s Impact in an Online Healthcare Community. Inf. Technol. Dev. 2018, 24, 279–300. [Google Scholar] [CrossRef]
- Yang, Y.; Guo, X.; Wu, T.; Vogel, D. The Effects of Social Media Use and Consumer Engagement on Physician Online Return: Evidence from Weibo. Internet Res. 2024, 34, 371–397. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, H.; Xia, C.; Lu, N. Impact of the Price of Gifts From Patients on Physicians’ Service Quality in Online Consultations: Empirical Study Based on Social Exchange Theory. J. Med. Internet Res. 2020, 22, e15685. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Liu, Q.B.; Guo, X.; Wu, T.; Kumar, S. Quid pro Quo in Online Medical Consultation? Investigating the Effects of Small Monetary Gifts from Patients. Prod. Oper. Manag. 2022, 31, 1698–1718. [Google Scholar] [CrossRef]
- Wang, Q.; Qiu, L.; Xu, W. Informal Payments and Doctor Engagement in an Online Health Community: An Empirical Investigation Using Generalized Synthetic Control. Inf. Syst. Res. 2024, 35, 706–726. [Google Scholar] [CrossRef]
- Li, C.-R.; Zhang, E.; Han, J.-T. Adoption of Online Follow-up Service by Patients: An Empirical Study Based on the Elaboration Likelihood Model. Comput. Hum. Behav. 2021, 114, 106581. [Google Scholar] [CrossRef]
- Grönroos, C. A Service Quality Model and Its Marketing Implications. Eur. J. Mark. 1984, 18, 36–44. [Google Scholar] [CrossRef]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. Servqual: A Multiple-Item Scale For Measuring Consumer Perc. J. Retail. 1988, 64, 12. [Google Scholar]
- Akter, S.; D’Ambra, J.; Ray, P. Development and Validation of an Instrument to Measure User Perceived Service Quality of mHealth. Inf. Manag. 2013, 50, 181–195. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, L. Getting Better? Examining the Effects of Social Support in OHCs on Users’ Emotional Improvement. Inf. Process. Manag. 2024, 61, 103754. [Google Scholar] [CrossRef]
- Chen, S.; Guo, X.; Wu, T.; Ju, X. Exploring the Online Doctor-Patient Interaction on Patient Satisfaction Based on Text Mining and Empirical Analysis. Inf. Process. Manag. 2020, 57, 102253. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, M.; Gao, B. Physician Voice Characteristics and Patient Satisfaction in Online Health Consultation. Inf. Manag. 2020, 57, 103233. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, X.; Liu, L.; Lai, K. Does Voice Matter? Investigating Patient Satisfaction on Mobile Health Consultation. Inf. Process. Manag. 2023, 60, 103362. [Google Scholar] [CrossRef]
- Yang, H.; Guo, X.; Wu, T. Exploring the Influence of the Online Physician Service Delivery Process on Patient Satisfaction. Decis. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, X.; Lee, P.K.C. Improving the Effectiveness of Online Healthcare Platforms: An Empirical Study with Multi-Period Patient-Doctor Consultation Data. Int. J. Prod. Econ. 2019, 207, 70–80. [Google Scholar] [CrossRef]
- Xuan, Y.; Guo, C.; Lu, W. The Effects of Information Continuity and Interpersonal Continuity on Physician Services Online: Cross-Sectional Study. JMIR Med. Inform. 2022, 10, e35830. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Wong, S.F.; Wang, S.; Chang, Y. Continue Staying in Online Health Platforms or Not: The Moderating Role of Threat Appraisal | Emerald Insight. Ind. Manag. Data Syst. 2023, 124, 361–385. [Google Scholar] [CrossRef]
- Mensah, I.K.; Adams, S.; Adjei, J.K.; Mwakapesa, D.S. Drivers of Egovernment Adoption amidst COVID-19 Pandemic: The Information Adoption Model (IAM) Approach. Inf. Dev. 2022, 38, 494–509. [Google Scholar] [CrossRef]
- Chakraborty, D.; Paul, J. Healthcare Apps’ Purchase Intention: A Consumption Values Perspective. Technovation 2023, 120, 102481. [Google Scholar] [CrossRef]
- Fernandes, T.; Oliveira, E. Understanding Consumers’ Acceptance of Automated Technologies in Service Encounters: Drivers of Digital Voice Assistants Adoption. J. Bus. Res. 2021, 122, 180–191. [Google Scholar] [CrossRef]
- Bhatt, K. Adoption of Online Streaming Services: Moderating Role of Personality Traits | Emerald Insight. Int. J. Retail Distrib. Manag. 2022, 50, 437–457. [Google Scholar] [CrossRef]
- Thabet, Z.; Albashtawi, S.; Ansari, H.; Al-Emran, M.; Al-Sharafi, M.A.; AlQudah, A.A. Exploring the Factors Affecting Telemedicine Adoption by Integrating UTAUT2 and IS Success Model: A Hybrid SEM–ANN Approach. IEEE Trans. Eng. Manag. 2024, 71, 8938–8950. [Google Scholar] [CrossRef]
- Edwards, D.; Subramanian, N.; Chaudhuri, A.; Morlacchi, P.; Zeng, W. Use of Delivery Drones for Humanitarian Operations: Analysis of Adoption Barriers among Logistics Service Providers from the Technology Acceptance Model Perspective. Ann. Oper. Res. 2024, 335, 1645–1667. [Google Scholar] [CrossRef] [PubMed]
- Arf, W.B.; Nasr, I.B.; Kondrateva, G.; Hikkerova, L. The Role of Trust in Intention to Use the IoT in eHealth: Application of the Modified UTAUT in a Consumer Context. Technol. Forecast. Soc. Change 2021, 167, 120688. [Google Scholar] [CrossRef]
- Malanga, A.C.M.; Bernardes, R.C.; Borini, F.M.; Pereira, R.M.; Rossetto, D.E. Towards Integrating Quality in Theoretical Models of Acceptance: An Extended Proposed Model Applied to e-Learning Services. Br. J. Educ. Technol. 2022, 53, 8–22. [Google Scholar] [CrossRef]
- Alkhalifah, K.; Alzahrani, S.; Alhomod, A.S. Assessment of The Healthcare Providers’ Acceptance of Telemedicine: Case of Endocrinology Teleclinics. In Proceedings of the 2023 IEEE International Conference on Technology Management, Operations and Decisions (ICTMOD), Rabat, Morocco, 22–24 November 2023; pp. 1–6. [Google Scholar]
- Bestepe, F.; Yildirim, S.O. Acceptance of IoT-Based and Sustainability-Oriented Smart City Services: A Mixed Methods Study. Sustain. Cities Soc. 2022, 80, 103794. [Google Scholar] [CrossRef]
- Xie, J.; Ye, L.; Huang, W.; Ye, M. Understanding FinTech Platform Adoption: Impacts of Perceived Value and Perceived Risk. J. Theor. Appl. Electron. Commer. Res. 2021, 16, 1893–1911. [Google Scholar] [CrossRef]
- Kumar, R.; Singh, R.; Kumar, K.; Khan, S.; Corvello, V. How Does Perceived Risk and Trust Affect Mobile Banking Adoption? Empirical Evidence from India. Sustainability 2023, 15, 4053. [Google Scholar] [CrossRef]
- Taneja, S.; Ali, L.; Siraj, A.; Ferasso, M.; Luthra, S.; Kumar, A. Leveraging Digital Payment Adoption Experience to Advance the Development of Digital-Only (Neo) Banks: Role of Trust, Risk, Security, and Green Concern. IEEE Trans. Eng. Manag. 2024, 71, 10862–10873. [Google Scholar] [CrossRef]
- Hooda, A.; Gupta, P.; Jeyaraj, A.; Giannakis, M.; Dwivedi, Y.K. The Effects of Trust on Behavioral Intention and Use Behavior within E-Government Contexts. Int. J. Inf. Manag. 2022, 67, 102553. [Google Scholar] [CrossRef]
- Tucker, J.L.; Adams, S.R. Incorporating Patients’ Assessments of Satisfaction and Quality: An Integrative Model of Patients’ Evaluations of Their Care. Manag. Serv. Qual. Int. J. 2001, 11, 272–287. [Google Scholar] [CrossRef]
- He, Y.; Guo, X.; Wu, T.; Vogel, D. The Effect of Interactive Factors on Online Health Consultation Review Deviation: An Empirical Investigation. Int. J. Med. Inform. 2022, 163, 104781. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Wang, H.; Xia, Q.; Zheng, L.; Shi, Y. Factors That Determine a Patient’s Willingness to Physician Selection in Online Healthcare Communities: A Trust Theory Perspective. Technol. Soc. 2021, 64, 101510. [Google Scholar] [CrossRef] [PubMed]
- McAllister, D.J. Affect- and Cognition-Based Trust as Foundations for Interpersonal Cooperation in Organizations. Acad. Manag. J. 1995, 38, 24–59. [Google Scholar] [CrossRef]
- Huang, Z.; Duan, C.; Yang, Y.; Khanal, R. Online Selection of a Physician by Patients: The Impression Formation Perspective. BMC Med. Inf. Decis. Mak. 2022, 22, 193. [Google Scholar] [CrossRef] [PubMed]
- Chi, O.H.; Jia, S.; Li, Y.; Gursoy, D. Developing a Formative Scale to Measure Consumers’ Trust toward Interaction with Artificially Intelligent (AI) Social Robots in Service Delivery. Comput. Hum. Behav. 2021, 118, 106700. [Google Scholar] [CrossRef]
- Lu, J.; Bai, J.; Zhao, H.; Zhang, X. The Effect of “Offline-to-Online” Trust Transfer on the Utilization of Online Medical Consultation Among Chinese Rural Residents: Experimental Study. J. Med. Internet Res. 2023, 25, e43430. [Google Scholar] [CrossRef] [PubMed]
- Sevick, M.A.; Trauth, J.M.; Ling, B.S.; Anderson, R.T.; Piatt, G.A.; Kilbourne, A.M.; Goodman, R.M. Patients with Complex Chronic Diseases: Perspectives on Supporting Self-Management. J. Gen. Intern. Med. 2007, 22, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Yan, X.; Wang, W.Y.C.; Chen, Q. Unveiling Physicians’ Personal Branding Strategies in Online Healthcare Service Platforms. Technol. Forecast. Soc. Change 2021, 171, 120964. [Google Scholar] [CrossRef]
- Wu, P.; Zhang, R. Exploring the Effects of Health Information Seeking on E-Satisfaction in Online Health Communities: An Empirical Investigation. BMC Med. Inf. Decis. Mak. 2022, 22, 332. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. 2022 China Health Statistics Yearbook. Available online: https://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/202305/49beded3bd984669bfe9089c6f231cf5.shtml (accessed on 17 May 2023).
- Yan, Z.; Kuang, L.; Qiu, L. Prosocial Behaviors and Economic Performance: Evidence from an Online Mental Healthcare Platform. Prod. Oper. Manag. 2022, 31, 3859–3876. [Google Scholar] [CrossRef]
- van Mierlo, T. The 1% Rule in Four Digital Health Social Networks: An Observational Study. J. Med. Internet Res. 2014, 16, e2966. [Google Scholar] [CrossRef] [PubMed]
- Miles, O.; West, R.; Nadarzynski, T. Health Chatbots Acceptability Moderated by Perceived Stigma and Severity: A Cross-Sectional Survey. Digit. Health 2021, 7, 20552076211063012. [Google Scholar] [CrossRef] [PubMed]
- Sestino, A.; D’Angelo, A. My Doctor Is an Avatar! The Effect of Anthropomorphism and Emotional Receptivity on Individuals’ Intention to Use Digital-Based Healthcare Services. Technol. Forecast. Soc. Change 2023, 191, 122505. [Google Scholar] [CrossRef]

| Variable | Description | Measurement | |
|---|---|---|---|
| Dependent variable | The behavior of consulting with a chosen physician for the first time. | The increase in patients of physician i in month t. | |
| The behavior of consulting with the same physician continuously and repeatedly. | The difference between the increase in orders and the increase in patients for physician i in month t. | ||
| Independent variable | The positive emotional reinforcement provided by physicians during their interactions with patients. | The ratio of the number of sentences containing emotional support to the number of valid physician–patient interactions of physician i in month t. | |
| The ability of providers to address patients’ needs promptly. | The average response time, as rated by Good Doctor Online, of physician i in month t. | ||
| The extent to which physicians encourage patients to engage with online follow-up services after offline treatments. | The ratio of the increase in online follow-up patients to the increase in total patients of physician i in month t. | ||
| Moderator variable | The prices of online health services set by physicians. | The price of written consultations of physician i in month t. | |
| Control variable | The recommendation heat displayed on physician portals. | The recommendation heat of physician i in month t. | |
| The articles written by physicians and posted on portals. | The increase in articles of physician i in month t. | ||
| A voluntary behavior that patients engage in after interactions with physicians. | The increase in gifts of physician i in month t. |
| Variable | Adoption | Usage | ||
|---|---|---|---|---|
| VIF | 1/VIF | VIF | 1/VIF | |
| Emotional Support | 1.26 | 0.7920 | 1.28 | 0.7841 |
| Responsiveness | 1.34 | 0.7471 | 1.34 | 0.7447 |
| Service Continuity | 1.24 | 0.8079 | 1.10 | 0.9062 |
| Price | 1.14 | 0.8782 | 1.08 | 0.9288 |
| Recommendation | 1.37 | 0.7286 | ||
| Article | 1.05 | 0.9568 | ||
| Gift | 1.17 | 0.8573 | ||
| Mean VIF | 1.23 | 1.19 | ||
| Variable | (1) | (2) | (3) |
|---|---|---|---|
| Constant | 1.166 *** | 0.651 *** | 0.380 |
| (4.82) | (2.96) | (1.63) | |
| Recommendation | 0.029 | 0.036 | 0.038 |
| (0.68) | (0.93) | (0.97) | |
| Article | 0.072 ** | 0.074 ** | 0.073 ** |
| (2.07) | (2.34) | (2.31) | |
| Price | −0.139 | −0.116 | 0.036 |
| (−1.55) | (−1.43) | (0.39) | |
| Emotional Support | 0.239 *** | 0.488 *** | |
| (6.78) | (3.44) | ||
| Responsiveness | 0.111 *** | 0.201 *** | |
| (14.14) | (6.45) | ||
| Service Continuity | 0.269 *** | 0.244 *** | |
| (13.90) | (3.26) | ||
| Price × Emotional Support | −0.132 * | ||
| (−1.80) | |||
| Price × Responsiveness | −0.051 *** | ||
| (−3.02) | |||
| Price × Service Continuity | 0.013 | ||
| (0.31) | |||
| Physician-fixed effects | Yes | Yes | Yes |
| Month-fixed effects | Yes | Yes | Yes |
| Observations | 3765 | 3765 | 3765 |
| F | 2.59 | 96.31 | 66.27 |
| Prob > F | 0.052 | 0.000 | 0.000 |
| R-squared | 0.950 | 0.959 | 0.959 |
| Adjusted R-squared | 0.924 | 0.938 | 0.939 |
| Variable | (1) | (2) | (3) |
|---|---|---|---|
| Constant | 1.004 ** | −0.298 | −0.626 |
| (2.33) | (−0.65) | (−0.98) | |
| Gift | 0.141 *** | 0.123 *** | 0.124 *** |
| (4.86) | (4.26) | (4.28) | |
| Price | −0.630 *** | −0.613 *** | −0.436 |
| (−2.87) | (−2.77) | (−1.34) | |
| Emotional Support | 0.389 *** | 1.888 *** | |
| (2.88) | (3.44) | ||
| Responsiveness | 0.372 *** | 0.463 *** | |
| (9.00) | (3.11) | ||
| Service Continuity | 0.216 *** | −0.268 | |
| (3.61) | (−1.25) | ||
| Price × Emotional Support | −0.786 *** | ||
| (−2.82) | |||
| Price × Responsiveness | −0.048 | ||
| (−0.65) | |||
| Price × Service Continuity | 0.261 ** | ||
| (2.29) | |||
| Physician-fixed effects | Yes | Yes | Yes |
| Month-fixed effects | Yes | Yes | Yes |
| Observations | 2955 | 2955 | 2955 |
| Log pseudolikelihood | −2182.692 | −2176.316 | −2175.778 |
| Wald chi2 | 34.15 | 137.96 | 147.27 |
| Prob > chi2 | 0.000 | 0.000 | 0.000 |
| Pseudo R2 | 0.195 | 0.197 | 0.197 |
| Variable | Removing Outliers | Subsample Regression | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Constant | 1.063 *** | 0.551 ** | 0.279 | 1.227 *** | 0.683 *** | 0.380 |
| (4.47) | (2.55) | (1.22) | (4.83) | (2.96) | (1.55) | |
| Recommendation | 0.027 | 0.034 | 0.035 | 0.021 | 0.031 | 0.032 |
| (0.63) | (0.88) | (0.92) | (0.49) | (0.80) | (0.82) | |
| Article | 0.072 ** | 0.074 ** | 0.073 ** | 0.039 | 0.046 | 0.044 |
| (2.11) | (2.38) | (2.35) | (1.02) | (1.31) | (1.28) | |
| Price | −0.094 | −0.071 | 0.082 | −0.154 | −0.127 | 0.048 |
| (−1.06) | (−0.89) | (0.90) | (−1.58) | (−1.45) | (0.47) | |
| Emotional Support | 0.239 *** | 0.492 *** | 0.264 *** | 0.580 *** | ||
| (6.90) | (3.53) | (6.82) | (3.77) | |||
| Responsiveness | 0.110 *** | 0.199 *** | 0.113 *** | 0.214 *** | ||
| (14.38) | (6.50) | (13.19) | (6.24) | |||
| Service Continuity | 0.262 *** | 0.256 *** | 0.266 *** | 0.216 ** | ||
| (13.78) | (3.48) | (12.29) | (2.53) | |||
| Price × Emotional Support | −0.134 * | −0.169 ** | ||||
| (−1.86) | (−2.11) | |||||
| Price × Responsiveness | −0.050 *** | −0.058 *** | ||||
| (−3.01) | (−3.08) | |||||
| Price × Service Continuity | 0.002 | 0.026 | ||||
| (0.05) | (0.54) | |||||
| Physician-fixed effects | Yes | Yes | Yes | Yes | Yes | Yes |
| Month-fixed effects | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 3765 | 3765 | 3765 | 3299 | 3299 | 3299 |
| F | 2.13 | 97.40 | 67.07 | 1.35 | 80.42 | 55.87 |
| Prob > F | 0.094 | 0.000 | 0.000 | 0.255 | 0.000 | 0.000 |
| R-squared | 0.944 | 0.955 | 0.955 | 0.952 | 0.961 | 0.962 |
| Adjusted R-squared | 0.916 | 0.932 | 0.932 | 0.925 | 0.939 | 0.939 |
| Variable | Standardized Usage Variable | Poisson Fixed-Effects Model | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Constant | −1.186 ** | −2.454 *** | −3.004 *** | 4.226 *** | 3.098 *** | 2.537 *** |
| (−2.29) | (−4.39) | (−3.63) | (8.26) | (5.81) | (3.46) | |
| Gift | 0.224 *** | 0.220 *** | 0.228 *** | 0.224 *** | 0.220 *** | 0.228 *** |
| (4.22) | (4.42) | (4.54) | (6.64) | (6.49) | (6.69) | |
| Price | −0.630 ** | −0.630 ** | −0.358 | −0.630 *** | −0.630 *** | −0.358 |
| (−2.46) | (−2.44) | (−0.92) | (−2.78) | (−2.77) | (−1.03) | |
| Emotional Support | 0.660 *** | 2.527 *** | 0.660 ** | 2.527 *** | ||
| (3.01) | (2.97) | (4.04) | (3.63) | |||
| Responsiveness | 0.295 *** | 0.464 ** | 0.295 *** | 0.464 ** | ||
| (5.42) | (2.19) | (6.19) | (2.52) | |||
| Service Continuity | 0.386 *** | −0.363 | 0.386 *** | −0.363 | ||
| (3.73) | (−1.15) | (5.21) | (−1.30) | |||
| Price × Emotional Support | −0.949 ** | −0.949 *** | ||||
| (−2.31) | (−2.73) | |||||
| Price × Responsiveness | −0.083 | −0.083 | ||||
| (−0.87) | (−0.92) | |||||
| Price × Service Continuity | 0.390 ** | 0.390 *** | ||||
| (2.45) | (2.72) | |||||
| Physician-fixed effects | Yes | Yes | Yes | Yes | Yes | Yes |
| Month-fixed effects | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 2955 | 2955 | 2955 | 3765 | 3765 | 3765 |
| Log likelihood | −291.290 | * −291.108 | −291.080 | −5828.442 | −5782.355 | −5775.260 |
| Wald (LR) chi2 | 25.11 | 64.15 | 76.36 | 65,999.54 | 66,091.72 | 66,105.91 |
| Prob > chi2 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Pseudo R2 | 0.266 | 0.266 | 0.267 | 0.850 | 0.851 | 0.851 |
| Variable | (1) | (2) | (3) |
|---|---|---|---|
| Constant | 1.143 *** | 0.632 *** | 0.356 |
| (4.72) | (2.87) | (1.53) | |
| Recommendation | 0.043 | 0.046 | 0.047 |
| (1.01) | (1.18) | (1.21) | |
| Article | 0.077 ** | 0.077 ** | 0.075 ** |
| (2.19) | (2.43) | (2.40) | |
| Price | −0.157 * | −0.128 | 0.027 |
| (−1.75) | (−1.58) | (0.29) | |
| Emotional Support | 0.241 *** | 0.486 *** | |
| (6.84) | (3.42) | ||
| Responsiveness | 0.111 *** | 0.204 *** | |
| (14.27) | (6.54) | ||
| Service Continuity | 0.270 *** | 0.248 *** | |
| (13.94) | (3.30) | ||
| Price × Emotional Support | −0.129 * | ||
| (−1.76) | |||
| Price × Responsiveness | −0.052 *** | ||
| (−3.08) | |||
| Price × Service Continuity | 0.011 | ||
| (0.27) | |||
| Physician-fixed effects | Yes | Yes | Yes |
| Disease-fixed effects | Yes | Yes | Yes |
| Observations | 3765 | 3765 | 3765 |
| F | 3.22 | 98.11 | 67.51 |
| Prob > F | 0.022 | 0.000 | 0.000 |
| R-squared | 0.949 | 0.959 | 0.959 |
| Adjusted R-squared | 0.924 | 0.938 | 0.938 |
| Variables | (1) | (2) | (3) |
|---|---|---|---|
| Constant | 1.076 ** | −0.247 | −0.607 |
| (2.47) | (−0.53) | (−0.94) | |
| Gift | 0.149 *** | 0.129 *** | 0.130 *** |
| (5.10) | (4.48) | (4.51) | |
| Price | −0.669 *** | −0.642 *** | −0.448 |
| (−3.01) | (−2.87) | (−1.37) | |
| Emotional Support | 0.397 *** | 1.849 *** | |
| (2.94) | (3.39) | ||
| Responsiveness | 0.373 *** | 0.478 *** | |
| (9.01) | (3.22) | ||
| Service Continuity | 0.215 *** | −0.247 | |
| (3.59) | (−1.15) | ||
| Price × Emotional Support | −0.761 *** | ||
| (−2.75) | |||
| Price × Responsiveness | −0.056 | ||
| (−0.75) | |||
| Price × Service Continuity | 0.249 ** | ||
| (2.18) | |||
| Physician-fixed effects | Yes | Yes | Yes |
| Disease-fixed effects | Yes | Yes | Yes |
| Observations | 2955 | 2955 | 2955 |
| Log pseudolikelihood | −2183.014 | −2176.576 | −2176.067 |
| Wald chi2 | 37.98 | 142.76 | 150.87 |
| Prob > chi2 | 0.000 | 0.000 | 0.000 |
| Pseudo R2 | 0.195 | 0.197 | 0.197 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, S.; Zhou, J.; Xu, N. The Impact of Perceived Quality on Patients’ Adoption and Usage of Online Health Consultations: An Empirical Study Based on Trust Theory. Healthcare 2025, 13, 1753. https://doi.org/10.3390/healthcare13141753
Zhu S, Zhou J, Xu N. The Impact of Perceived Quality on Patients’ Adoption and Usage of Online Health Consultations: An Empirical Study Based on Trust Theory. Healthcare. 2025; 13(14):1753. https://doi.org/10.3390/healthcare13141753
Chicago/Turabian StyleZhu, Shuwan, Jiahao Zhou, and Nini Xu. 2025. "The Impact of Perceived Quality on Patients’ Adoption and Usage of Online Health Consultations: An Empirical Study Based on Trust Theory" Healthcare 13, no. 14: 1753. https://doi.org/10.3390/healthcare13141753
APA StyleZhu, S., Zhou, J., & Xu, N. (2025). The Impact of Perceived Quality on Patients’ Adoption and Usage of Online Health Consultations: An Empirical Study Based on Trust Theory. Healthcare, 13(14), 1753. https://doi.org/10.3390/healthcare13141753






