1. Introduction
Bertolotti syndrome was first described in 1917 by Bertolotti [
1] and is a frequently overlooked pathology characterized by a symptomatic lumbosacral transitional vertebra (LSTV). This congenital anatomic anomaly consists of an enlarged lateral process of the caudal lumbar vertebra (L5), which forms a pseudoarticulation or fusion with the ilium or sacrum [
2]. While the radiological presence of LSTV is relatively common and found in 4–30% of the general population [
3], only few of these cases manifest clinically as Bertolotti syndrome with significant pain and disability. LSTV is classified according to Castellvi, distinguishing type I to IV, depending on the extent of the pseudoarticulation and fusion. Castellvi type I is the most common (42%) anomaly [
2].
Leading symptoms are chronic lower back pain (LBP) and/or (pseudo-)radicular symptoms resulting from mechanical stress, degeneration of the pseudoarticulation, and/or irritation of the exiting L4 nerve root [
2,
4]. Bertolotti syndrome remains a diagnostic challenge, frequently overlooked in favor of more common causes of back pain. In 2006, Quinlan et al. [
5] indicated a higher prevalence in younger patients, making it less likely to be considered a differential diagnosis in middle-aged and older patients. A delay of up to seven years in diagnosis and treatment leads to prolonged patient suffering [
6].
First-line treatment of Bertolotti syndrome includes conservative treatment with physiotherapy, infiltration, and radiofrequency ablation [
2,
7]. When conservative treatment fails, surgical resection of the enlarged transverse process (“processectomy”) or spinal fusion are performed [
4,
6,
8]. There are no large-scale studies investigating the failure rate of conservative treatment nor any guidelines recommending the switch from conservative to surgical treatment based on concrete parameters.
We present a 48-year-old, highly active patient and emphasize that Bertolotti syndrome can occur in middle-aged, very athletic and active patients. For such patients in particular, the reduction in quality of life due to pain, often inadequately treated, is very significant. Future studies should include patients from all age groups. The discussion includes diagnostic challenges, limitations of conservative treatment, and outcomes of surgical treatment. This case follows the CARE reporting guidelines.
2. Case Presentation
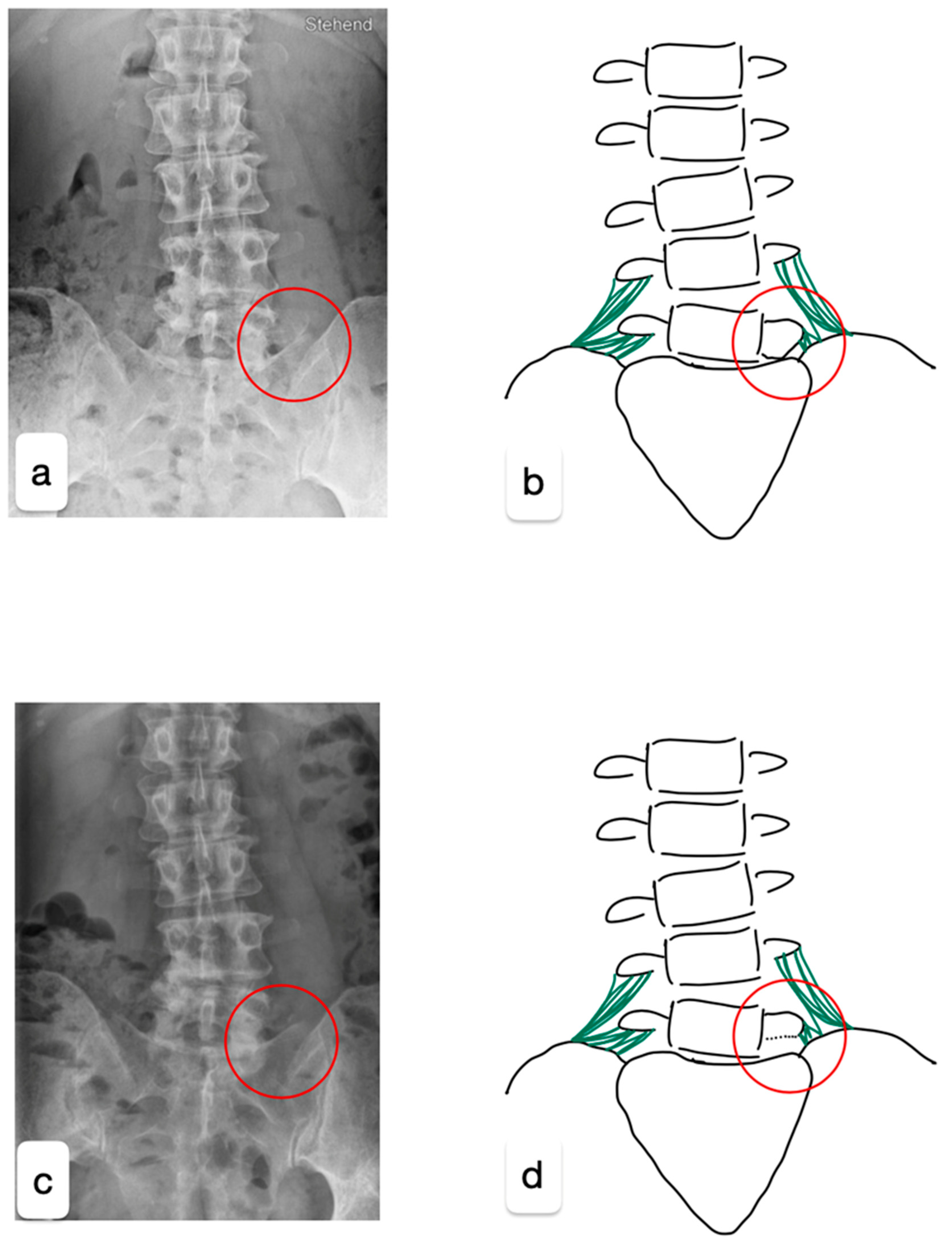
A 48-year-old healthy female triathlete presented to our outpatient clinic with pain in the left gluteal region persisting for two years, especially during sporting activities. No relevant past medical history. Neurological examination of the patient was unremarkable, showing normal flexibility and mild tenderness over the left sacroiliac joint. Magnetic resonance imaging and computed tomography revealed multisegmental degenerative changes with a right convex scoliosis, multisegmental disc extrusion without relevant stenosis, osteochondrosis L2/3, L4/5, and L5/S1, facet joint arthrosis L3/4, and left-sided LSTV (Castellvi type 1a) (
Figure 1a,b).
Prior to our consultation, the conservative treatment consisted of diagnostic–therapeutic infiltration of the L4-S1 levels and the sacroiliac joint, providing only temporary relief. Pathologies of the spinal canal, facet joints, and sacroiliac joints therefore appeared less likely as a differential source of pain. Repeated infiltrations of the L5/S1 pseudoarticulation later confirmed the diagnosis of Bertolotti syndrome but failed to achieve pain relief lasting for more than three weeks. Additional conservative treatments, including physiotherapy, manual therapy, chiropractic interventions, thermocoagulation, and radiofrequency ablation of the pseudoarticulation, were also ineffective in the long term. The patient continued to experience significant pain during physical activities such as running and swimming, resulting in a major impact on her quality of life.
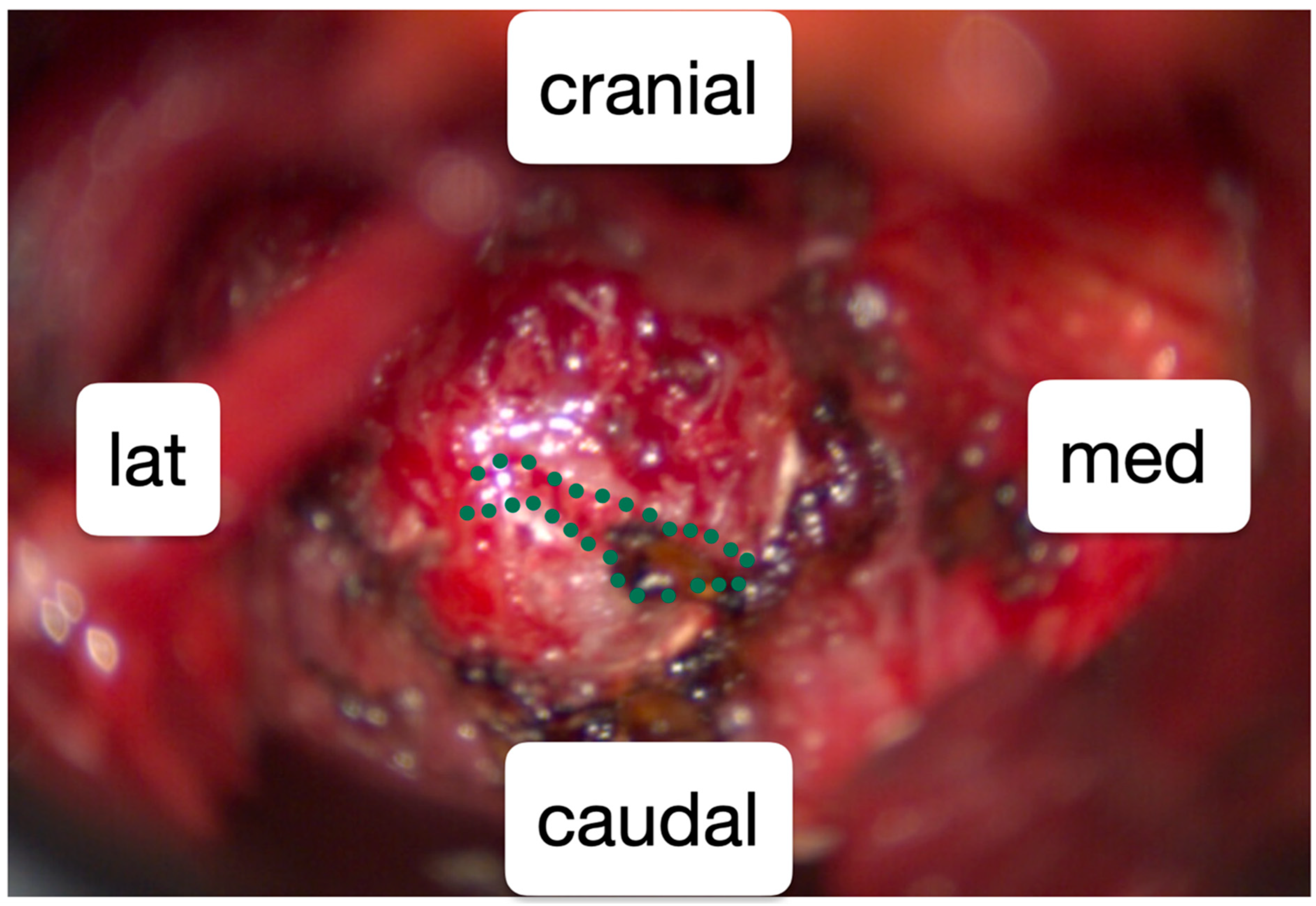
As the conservative treatment was exhausted, surgical reduction of the left L5 transverse process was performed. For the surgery with general anesthesia, the patient was positioned in a prone position on a Wilson frame. The L5/S1 neoarticulation was visualized using X-ray control (anterior–posterior and lateral beam path). Following a paramedian skin incision on the left L5/S1 level and dissection of the fascia and paravertebral musculature, a Caspar retractor was inserted. The caudal part of the transverse process L5 was reduced microsurgically using a 6 mm diamond drill and bone punch (
Figure 1 and
Figure 2). Strong adhesions to the pelvis were exposed and the L4 nerve root could be visualized.
Following a three-night stay, the patient was discharged home without any peri- or postoperative complications. Postoperative follow-up visits up to six months showed a satisfactory resolution of her chronic gluteal pain, allowing her to resume marathon training. At the most recent consultation, a year after surgery, the patient reported a pain reduction of at least 70% compared to before the surgery. This case highlights the effectiveness of surgical intervention for refractory Bertolotti syndrome, especially in active patients with significant functional impairment.
3. Discussion
Bertolotti syndrome describes a symptomatic LSTV in which the congenital enlarged lateral process of the caudal lumbar vertebra (L5) forms a pseudoarticulation with the ilium or sacrum [
2]. First described by Bertolotti in 1917 [
1], this condition is often overlooked or misinterpreted as a mere radiological anomaly rather than as a clinically significant source of pain. Uni- and bilateral radiological anomalies of the L5 transverse process are classified according to Castellvi [
9]. LSTV Castellvi type I is the most common anomaly [
2], as was found in the presented case. Bertolotti syndrome commonly presents as uni- or bilateral LBP, sometimes accompanied by (pseudo-)radicular pain. These symptoms result from L4 nerve compression (radicular symptoms) or degeneration of the pseudoarticulation (pseudoradicular symptoms) [
2,
4]. The L4 nerve root, located near the hypertrophic L5 transverse process, is particularly vulnerable to irritation [
4]. Altered biomechanics from LSTV may predispose individuals to earlier degenerative spinal changes [
10], possibly due to asymmetry between the lumbar vertebrae and sacrum [
7]. Bertolotti syndrome is the clinical correlate of the congenital, usually asymptomatic, LSTV.
The age at diagnosis of Bertolotti syndrome varies significantly across different published studies. Quinlan et al. [
5] reported a mean age of 32.7 years for patients with radiologically and clinically confirmed Bertolotti syndrome. In contrast, the presented patient is unique due to the relatively late onset of symptoms associated with congenital LSTV (Bertolotti syndrome). Perhaps her sporting activities delayed pain until later in life. Studies on protective factors such as physical constitution and sporting activities are needed to evaluate which and why patients with congenital LSTV develop Bertolotti syndrome. In contrast, Il Ju et al. [
4] reported a mean age of 55.9 years for patients with Bertolotti syndrome requiring surgery, and Ravikanth et al. [
11] found no statistically significant difference in age distribution between patients with radiologically confirmed Bertolotti syndrome and those with unspecific LBP, highlighting the variability in presentation.
Patients with Bertolotti syndrome often endure LBP with or without radicular symptoms for several years before receiving a diagnosis; Santarvirta et al. [
6] reported an average of seven years from onset of LBP to surgical intervention. This time is marked, besides severe pain and reduced quality of life, by many (potentially invasive) examinations, painful procedures, and, depending on the country, healthcare expenses and lost income. Treatment of Bertolotti syndrome ranges from conservative first-line treatment with physiotherapy, injections, and radiofrequency ablation to surgical intervention including resection of the enlarged transverse process (“processectomy”) or spinal fusion in refractory cases [
2,
7].
Holm et al. [
8] reviewed 79 cases treated with either infiltrations or surgery, of which 33 patients underwent transverse process resection, 8 had spinal fusion, and 7 had laminectomy. Santarvirta et al. [
6] compared surgical and conservative treatments, finding that surgery resulted in slightly lower pain scores (1.9 vs. 2.5). However, they noted that only four out of six patients with a positive preoperative infiltration response achieved significant postoperative improvement. This emphasizes the importance of a reliable preoperative diagnosis. In our case, particularly with a highly active patient, we opted for the less invasive surgical therapy and thus for a sole reduction of the transverse process instead of spinal fusion with potential long-term complications such as adjacent segment disease.
In the end, Bertolotti syndrome is a complex clinical picture that requires a personalized interdisciplinary conservative and surgical treatment. If conservative treatment fails, even in active patients, surgical treatment should be evaluated in an interdisciplinary setting and recommended if deemed appropriate.
This case report has limited generalizability as it describes only a single highly active middle-aged patient. Further studies are needed to investigate the prevalence and adequate treatment in (active) middle-aged and older patients.
4. Conclusions
We presented a single case of a highly active middle-aged patient suffering from therapy-refractory Bertolotti syndrome with extensive conservative therapy.
Bertolotti syndrome is a significant yet often overlooked cause of chronic lower back and gluteal pain in patients with LSTV. This case highlights the importance of considering Bertolotti syndrome in the differential diagnosis of chronic LBP in patients of all ages. Though traditionally associated with younger demographics [
5], symptomatic cases have been reported in patients as old as 65 years [
12]. The prolonged diagnostic delays seen in many patients, including this case, underscore the importance of imaging studies and targeted infiltrations for accurate diagnosis. First-line conservative treatment may fail in highly active patients, making surgical intervention necessary. As this is a single case report, larger-scale studies are needed to investigate the value of surgical treatment in active and/or elderly patients.
For this patient, microsurgical reduction of the caudal part of the hypertrophic transverse process after exhaustion of conservative treatment proved to be the definitive treatment. This case illustrates the need for tailored treatment and considering surgery in case of therapy-refractory Bertolotti syndrome. Further research focusing on long-term outcomes and the development of standardized diagnostic and treatment guidelines would improve patient care for this often unrecognized condition.
Author Contributions
Writing, reviewing and editing J.M., supervision A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The authors have completed the CARE reporting checklist. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this case report.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We thank Alexander Mattmann for his support in the finalization of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| LBP | lower back pain |
| LSTV | lumbosacral transitional vertebra |
References
- Bertolotti, M. Contributo alla conoscenza dei vizi differenzazione regionale del rachide con speciale riguardo all assimilazione sacrale della V. lombare. Radiol. Med. 1917, 4, 113–144. [Google Scholar]
- Crane, J.; Cragon, R.; O’nEill, J.; Berger, A.A.; Kassem, H.; Sherman, W.F.; Paladini, A.; Varrassi, G.; Odisho, A.S.; Miriyala, S.; et al. A Comprehensive Update of the Treatment and Management of Bertolotti’s Syndrome: A Best Practices Review. Orthop. Rev. 2021, 13, 24980. [Google Scholar] [CrossRef] [PubMed]
- Jat, S.K.; Srivastava, A.; Malhotra, R.; Chadha, M.; Tandon, A.; Jain, A.K. Prevalence of lumbosacral transitional vertebra in patients with chronic low back pain: A descriptive cross-sectional study. Am. J. Neurodegener. Dis. 2023, 12, 89–96. [Google Scholar] [PubMed]
- Lee, S.M.; Shin, H.; Lee, H.Y.; Kim, J.G.; Kim, S.W.; Ju, C.I. Retrospective Study Decompressive L5 Transverse Processectomy for Bertolotti’s Syndrome: A Preliminary Study Chang il. 2017. Available online: https://www.painphysicianjournal.com/linkout?issn=&vol=20&page=E923 (accessed on 14 December 2024).
- Quinlan, J.F.; Duke, D.; Eustace, S.; Frcsi, A.F. Bertolotti’s syndrome: A cause of back pain in young people. J. Bone Jt. Surg. 2006, 88, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Santavirta, S.; Tallroth, K.; Ylinen, P.; Suoranta, H. Orthopaedic Trauma Surgery Surgical treatment of Bertolotti’s syndrome Follow-up of 16 patients. Arch. Orthop. Trauma Surg. 1993, 112, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Almeida, D.B.D.; Mattei, T.A.; Sória, M.G.; Prandini, M.N.; Leal, A.G.; Milano, J.B.; Ramina, R. Transitional lumbosacral vertebrae and low back pain Diagnostic pitfalls and management of Bertolotti’s syndrome. Arq. Neuro-Psiquiatr. 2009, 67, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Holm, E.K.; Bünger, C.; Foldager, C.B. Symptomatic lumbosacral transitional vertebra: A review of the current literature and clinical outcomes following steroid injection or surgical intervention. SICOT-J 2017, 3, 71. [Google Scholar] [CrossRef] [PubMed]
- Castellvi Antonio, E.; Goldstein Louis, A.; Chan Donald, P.K. Lumbosacral Transitional Vertebrae and Their Relationship with Lumbar Extradural Defects. Spine 1984, 9, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; McGrath, K.; Rao, E.M.; Thompson, N.R.; Schmidt, E.; Lee, J.; Statsevych, V.; Steinmetz, M.P. Examining degenerative disease adjacent to lumbosacral transitional vertebrae: A retrospective cohort study. J. Neurosurg. Spine 2023, 38, 688–695. [Google Scholar] [CrossRef] [PubMed]
- Ravikanth, R.; Majumdar, P. Bertolotti’s syndrome in low-backache population: Classification and imaging findings. Tzu Chi Med. J. 2019, 31, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Barkhane, Z.; Belaaroussi, S.; Foudail, M. Bilateral Bertolotti’s Syndrome: A Case Report of an Uncommon Presentation of Chronic Low Back Pain in an Elder Patient. Cureus 2022, 14, e26569. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).