Evidence-Based Weight Management for Fertility Preservation in Endometrial Cancer Patients: Developing a Complex Intervention Based on the Medical Research Council Framework
Abstract
1. Introduction
2. Materials and Methods
2.1. Stage 1: Establishing the Intervention Development Group
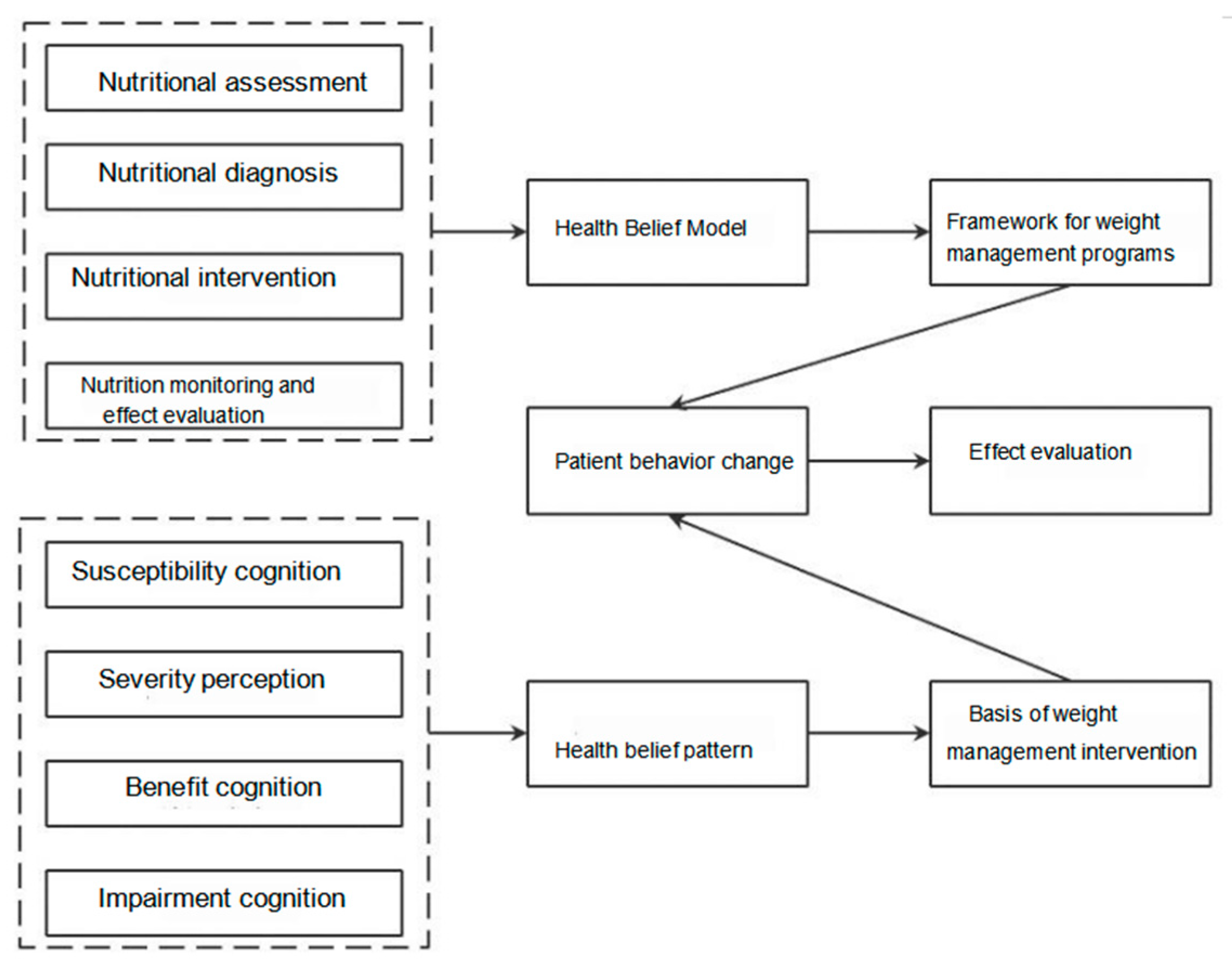
2.2. Stage 2: Identifying Theoretical Basis and Forming the Content Framework of the Weight Management Program
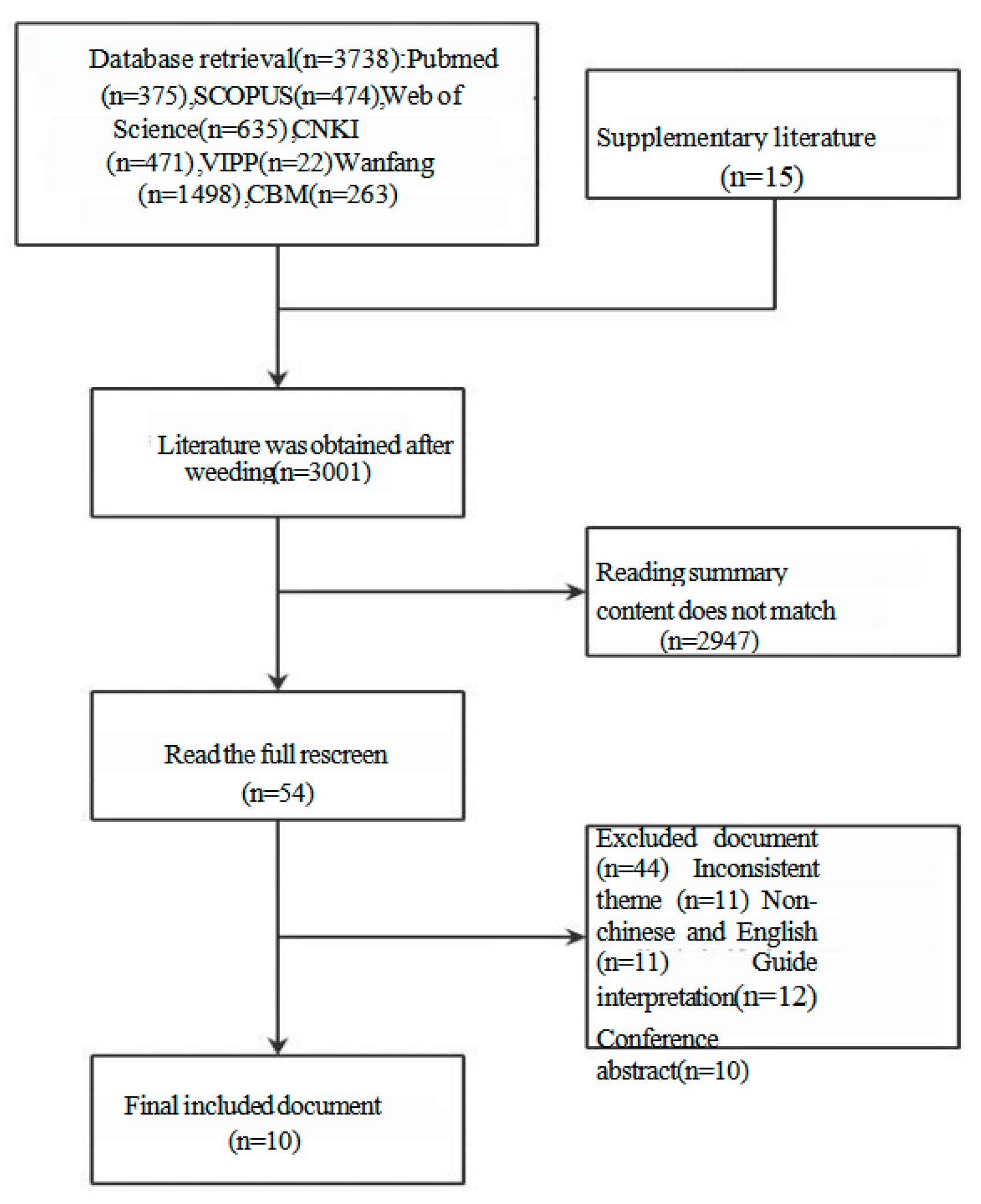
2.3. Stage 3: Evidence Retrieval and Synthesis
2.3.1. Inclusion and Exclusion Criteria
2.3.2. Search Strategy
2.3.3. Data Analysis
2.4. Stage 4: Refining and Modeling the Practice Program
2.4.1. Expert Consultation
2.4.2. Improvement Process
2.5. Ethical Considerations
3. Results
3.1. Stage 1: Establishing the Intervention Development Group
3.2. Stage 2: Identifying Theoretical Basis and Forming a Content Framework
3.3. Stage 3: Evidence Retrieval and Synthesis
3.4. Stage 4: Refining and Modeling the Practice Program
3.4.1. Expert Consultation
3.4.2. Improve the Process Results
4. Discussion
4.1. Literature Review Content Analysis
4.2. Scientific and Feasibility Analysis of the Weight Management Program for EC Patients with Fertility Preservation
4.3. Limitations and Outlook
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| First-Level Entry | Second-Level Entry | Three-Level Entry |
| 1. Establishing the intervention development group | 1.1 Membership composition | 1.1.1 To establish a multidisciplinary weight management team for overweight/obese patients with EC treated with fertility preservation, with key members including gynecologists, endocrinologists, nutritionists, rehabilitation physicians, nurses, etc. |
| 1.2 Define responsibilities | 1.2.1 Gynecologists are responsible for the treatment of patients with fertility preservation function, assessment of patients’ weight loss needs, and management of adverse reactions related to nursing therapy and nutritional interventions. | |
| 1.2.2 Endocrinologists are responsible for the assessment of patients’ endocrine metabolism, such as thyroid and islet cell function, and the formulation of endocrine drug therapy to improve blood sugar and insulin resistance. | ||
| 1.2.3 Nutrition physicians are responsible for the nutritional assessment of patients, the formulation and adjustment of nutritional intervention programs, regular nutritional monitoring and effect evaluation. | ||
| 1.2.4 Rehabilitation physicians are responsible for the exercise assessment of patients, the formulation and adjustment of exercise intervention programs, regular exercise monitoring and effect evaluation. | ||
| 1.2.5 Nurses are responsible for overweight/obesity risk screening of patients, assessing patients’ willingness to lose weight, and establishing weight management files for patients; Assist gynecologists, endocrinologists, nutritionists and rehabilitation physicians in the evaluation and weight management program formulation, monitoring and effect evaluation; Follow up regularly, carry out health education, provide information and psychological support for patients, and participate in the whole process of weight management and guidance. | ||
| 2. Screening evaluation | 2.1 Screening | 2.1.1 Timing: When it is clear that patients with EC have the intention of fertility preservation treatment, screening should be completed at the time of outpatient visit or admission. |
| 2.1.2 Contents: The patient’s height, weight, waist circumference and hip circumference were measured and BMI was calculated. BMI ≥ 24 kg/m2. Judged to be overweight; BMI ≥ 28 kg/m2 is considered obese, waist circumference ≥ 85 cm is considered central obesity. | ||
| 2.2 Evaluate | 2.2.1 Basic information: age, marital status, living status, education level, family income, occupation and previous weight loss experience. | |
| 2.2.2 Medical history: Family history, drug use history, smoking history, obesity-related comorbidities (type 2 diabetes, dyslipidemia, hypertension, coronary atherosclerotic heart disease, nonalcoholic fatty liver disease, sleep apnea syndrome, polycystic ovary syndrome, osteoarthritis, gout, etc.). | ||
| 2.2.3 Treatment of endometrial carcinoma or endometrial atypical hyperplasia. | ||
| 2.2.4 Willingness to lose weight. | ||
| 2.2.5 Body composition analysis, biochemical and metabolic indicators: triglyceride, total cholesterol, high density lipoprotein, low density lipoprotein, fasting blood glucose, fasting insulin, glycated hemoglobin, thyroid stimulating hormone, alanine transferase, blood creatinine, urea nitrogen, etc. | ||
| 2.2.6 Diet, exercise, lifestyle: Dietary nutrition Assessment questionnaire, physical activity assessment questionnaire, health promotion lifestyle scale were assessed. | ||
| 2.2.7 Health beliefs, self-efficacy, quality of life: The Health Belief Scale, self-efficacy scale, and General Quality of Life scale for cancer patients were evaluated. | ||
| 2.3 Judgment | 2.3.1 Stage 1: Overweight with one or more overweight/obesity-related diseases; Or obese, without or with one or more overweight/obesity-related preconditions. | |
| 2.3.2 Stage 2: Overweight/obesity with one or more overweight/obesity-related diseases. | ||
| 2.3.3 Stage 3: Overweight/obese with severe complications from one or more overweight/obesity-related diseases. | ||
| 3. Make a plan | 3.1 Set weight management goals | 3.1.1 Those with normal weight at the first screening maintained their original weight. |
| 3.1.2 Weight loss of at least 5% within 3 to 6 months of initial screening. | ||
| 3.1.3 Those who were first screened for obesity lost at least 10% of their body weight within 3 to 6 months. | ||
| 3.2 Create personalized meal recipes | 3.2.1 Dietary principles: less salt and less oil, control sugar and limit wine, reasonable collocation, balanced diet. | |
| 3.2.2 Dietary structure: Overweight and obese people adopt a balanced diet with limited energy, that is, the daily distribution of the three major nutrients is carbohydrates accounted for 50% to 55%, protein accounted for 10% to 20%, fat accounted for 25% to 30%, and the total amount is reduced by 500 kcal on the basis of the target intake; Normal weight patients were instructed to eat a balanced diet and improve bad eating habits. | ||
| 3.2.3 Recipe formulation: The food exchange portion method was used as a guide, that is, each 90 Kcal calorie of food was taken as one portion, the ideal weight was calculated, the total daily intake of calories was calculated according to the activity intensity, the number of six food exchange portions and the distribution of three meals were determined according to the total calories and diet structure, and the specific recipes were formulated according to the tastes and preferences of patients combined with the equivalent food exchange table to ensure that patients could accept and implement them. | ||
| 3.3 Develop an individualized exercise prescription | 3.3.1 Exercise principle: Take steps gradually, avoid sitting, and ensure at least 6000 steps a day. | |
| 3.3.2 Total exercise: Overweight and obese people are recommended to consume 90 kcal calories as one exercise unit, daily exercise consumption of 3 to 4 exercise units; People of normal weight can be guided to develop their exercise habits. | ||
| 3.3.3 Type of exercise: such as dancing, aerobics, brisk walking and other light aerobic exercise, about 90 kcal every 20 min; Moderate aerobic exercise, such as climbing, jogging and badminton, consumes about 90 kcal every 10 min; Jumping rope, swimming, basketball and other heavy aerobic exercise consumes about 90 kcal every 5 min; Resistance exercises such as sit-ups, squats, dumbbell heel raises, etc. | ||
| 3.3.4 Exercise intensity: exercise 3~5 days a week, can exercise every day or every other day; During exercise, the heart rate ranges from 64% to 76%, and the maximum heart rate or exercise intensity is 3–6 exercise equivalent; Increase the intensity by 5% for every 6 sessions until you reach 65% of your maximum load. | ||
| 3.3.5 Formulation of prescription: According to the patient’s health status and personal preference, individual exercise prescription including exercise type, exercise intensity, exercise time, exercise frequency and other contents shall be formulated. | ||
| 3.4 Develop a health education plan | 3.4.1 Time, form and frequency: Health education knowledge is promoted to patients through the online platform every two weeks, each time lasting 30 to 60 min, a total of 6 times. | |
| 3.4.2 Contents: Adverse effects of overweight/obesity on treatment outcomes of fertility preservation; The benefits of diet and exercise for weight control; Difficulties and problems that may be encountered in weight control, and give solutions; Popularizing nutrition knowledge such as caloric estimation method and common nutrition misunderstanding; Sports knowledge popularization, such as sports precautions and sports methods; Peer experience sharing, etc. | ||
| 4. Implementation plan | 4.1 Put into administration | 4.1.1 Add the patient to the WeChat group and keep timely communication and feedback. |
| 4.1.2 Establish a weight management profile for patients. | ||
| 4.2 Dietary program guidance | 4.2.1 Time: The first time to communicate with the patient to develop a personalized diet plan. | |
| 4.2.2 Contents: Use method and precautions of diet program. | ||
| 4.3 Exercise program guidance | 4.3.1 Time: The first time to communicate with the patient to formulate an individualized exercise program. | |
| 4.3.2 Content: Use method and precautions of exercise program. | ||
| 4.4 Health education and training | 4.4.1 Time: After the patient started the diet and exercise program. | |
| 4.4.2 Content: Same as health education program content. | ||
| 4.5 Timely information support and psychological support | 4.5.1 Timely answer patients’ questions about diet, exercise, treatment and other aspects. | |
| 4.5.2 Every day to the patient’s efforts to give affirmation, to the patient’s psychological dilemma to give resolution. | ||
| 4.5.3 Encourage patients to share diet and exercise records daily to promote peer support. | ||
| 5. Supervision and evaluation | 5.1 Weekly supervision | 5.1.1 Supervise patients to make daily diet, exercise and weight records. |
| 5.2 Evaluation once every 3 months, at least 2 consecutive times | 5.2.1 At 3 months, whether the weight management goal was achieved. | |
| 5.2.2 Body mass index, waist circumference, body composition analysis, glycolipid metabolism index, etc. | ||
| 5.2.3 Remission of EC or endometrial atypical hyperplasia after treatment. | ||
| 5.2.4 Lifestyle, health beliefs, self-efficacy, quality of life, etc. | ||
| 6. Analysis and adjustment | 6.1 Analyze the reasons that hinder weight management | 6.1.1 The diet and exercise program was adhered to well, but the weight control was not ideal: side effects of hormone therapy, insensitive diet and exercise program, etc. |
| 6.1.2 Diet and exercise program cannot be adhered to: Due to personal reasons such as changes in work and living environment or restrictions, the existing program cannot be adhered to. | ||
| 6.1.3 Other reasons. | ||
| 6.2 Adjust for cause | 6.2.1 Change of endometrial treatment plan: Adjust to other treatment plan according to the pathological results of patients and drug side effects. | |
| 6.2.2 Change of diet and exercise regimen: Consider the application of other diet or exercise regimen such as high-protein diet, intermittent energy restriction, ketogenic diet, etc. | ||
| 6.2.3 According to the patient’s personal situation, make the appropriate diet and exercise program fine-tuning. |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Koh, W.J.; Abu-Rustum, N.R.; Bean, S.; Bradley, K.; Campos, S.M.; Cho, K.R.; Chon, H.S.; Chu, C.; Cohn, D.; Crispens, M.A.; et al. Uterine Neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Com. Cancer Netw. 2018, 16, 170–199. [Google Scholar] [CrossRef]
- Minig, L.; Franchi, D.; de Bernabé, J.V.; Sideri, M. Controversies of the hormonal conservative treatment of endometrial cancer. Gynecol. Obstet. Investig. 2013, 75, 145–151. [Google Scholar] [CrossRef]
- Qin, Z.; Zhang, D.; Cao, G.; Li, H. Progestin-based pharmacotherapy in fertility preservation in early endometrial cancer. Front. Oncol. 2024, 14, 1487008. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-Y.; Seong, S.J.; Kim, T.-J.; Kim, J.W.; Bae, D.-S.; Nam, J.-H. Significance of body weight change during fertility-sparing progestin therapy in young women with early endometrial cancer. Gynecol. Oncol. 2017, 146, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Barr, C.E.; Ryan, N.A.J.; Derbyshire, A.E.; Wan, Y.L.; MacKintosh, M.L.; McVey, R.J.; Bolton, J.; Fitzgerald, C.; Awad, D.; Slade, R.J.; et al. Weight Loss During Intrauterine Progestin Treatment for Obesity-associated Atypical Hyperplasia and Early-Stage Cancer of The Endometrium. Cancer Prev. Res. 2021, 14, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cao, D.; Yang, J.; Yu, M.; Zhou, H.; Cheng, N.; Wang, J.; Zhang, Y.; Peng, P.; Shen, K. Fertility-Sparing Treatment for Endometrial Cancer or Atypical Endometrial Hyperplasia Patients with Obesity. Front. Oncol. 2022, 12, 812346. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, D.; Yan, Q.; Song, X.; Tian, W.; Wang, Y.; Teng, F.; Wei, L.; Wang, J.; Zhang, H.; et al. Weight Loss Improves Pregnancy and Livebirth Outcomes in Young Women with Early-Stage Endometrial Cancer and Atypical Hyperplasia. Cancer Manag. Res. 2021, 13, 5711–5722. [Google Scholar] [CrossRef]
- Li, X.; Chen, Y.; Li, X.; Yang, X.; Zhou, L.; Cheng, Y.; Hou, H.; Yang, D.; Gong, Y.; Xiao, H.; et al. Weight Management for Fertility-Preservation Therapy in Endometrial Cancer: Opportunities and Challenges. Curr. Oncol. Rep. 2025, 27, 195–210. [Google Scholar] [CrossRef]
- Yamagami, W.; Mikami, M.; Nagase, S.; Tabata, T.; Kobayashi, Y.; Kaneuchi, M.; Kobayashi, H.; Yamada, H.; Hasegawa, K.; Fujiwara, H.; et al. Japan Society of Gynecologic Oncology 2018 guidelines for treatment of uterine body neoplasms. J. Gynecol. Oncol. 2020, 31, e18. [Google Scholar] [CrossRef]
- Lee, S.W.; Lee, T.S.; Hong, D.G.; No, J.H.; Park, D.C.; Bae, J.M.; Seong, S.J.; Shin, S.J.; Ju, W.; Lee, K.H.; et al. Practice guidelines for management of uterine corpus cancer in Korea: A Korean Society of Gynecologic Oncology Consensus Statement. J. Gynecol. Oncol. 2017, 28, e12. [Google Scholar] [CrossRef] [PubMed]
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; González-Martín, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.R.; et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, Treatment and Follow-up. Int. J. Gynecol. Cancer 2016, 26, 2–30. [Google Scholar] [CrossRef]
- Coelho, F.; Furtado, L.; Tavares, M.; Sousa, J.P. A Complex Intervention to Minimize Medication Error by Nurses in Intensive Care: A Case Study. Healthcare 2025, 13, 66. [Google Scholar] [CrossRef] [PubMed]
- Hammond, M.I.; Myers, E.F.; Trostler, N. Nutrition care process and model: An academic and practice odyssey. J. Acad. Nutr. Diet. 2014, 114, 1879–1894. [Google Scholar] [CrossRef] [PubMed]
- Nutrition and Metabolic Management Branch of China International Exchange and Promotive Association for Medical and Health Care; Clinical Nutrition Branch of Chinese Nutrition Society; Chinese Diabetes Society; Chinese Society for Parenteral and Enteral Nutrition; Chinese Clinical Nutritionist Center of Chinese Medical Doctor Association. Guidelines for the Medical Nutrition Treatment of Overweight/Obesity in China (2021). Chin. J. Front. Med. Sci. 2021, 31, 450–482. [Google Scholar]
- Garvey, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R.; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pract. 2016, 22 (Suppl. 3), 1–203. [Google Scholar]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014, 129 (Suppl. S2), S102–S138. [Google Scholar] [CrossRef]
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. European Guidelines for Obesity Management in Adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef]
- NICE. Obesity: Identification, Assessment and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2014. [Google Scholar]
- Chinese Society of Health Management; Clinical Nutrition Branch of Chinese Nutrition Society; Medical Nutrition Industry Branch of the National Association of Health Industry and Enterprise Management; the Editorial Board of Chinese Journal of Health Management. Expert consensus on the procedure of body weight management among patients with overweight or obesity (2021). Chin. J. Health Manag. 2021, 15, 317–322. [Google Scholar]
- Chinese Society of Endocrinology (CSE); Diabetes Society of China Association of Chinese Medicine (DSCACM); Chinese Society for Metabolic and Bariatric Surgery (CSMBS); Chinese Association of Research Hospitals (CSDBS). Multidisciplinary clinical consensus on diagnosis and treatment of obesity (2021 edition). Chin. J. Endocrinol. Metab. 2021, 7, 211–246. [Google Scholar]
- Chinses Society of Nutritional Oncology. Expert consensus on nutritional therapy for patients with endometrial cancer. Electron. J. Metab. Nutr. Cancer 2020, 7, 415–417. [Google Scholar]
- Chinese Experts Consensus Group on the Body Quality Management Approach and Process for Overweight/Obese Infertility Patients. Expert consensus on the weight management of overweight/obese infertility patients in China. Chin. Soc. Nutr. Oncol. 2020, 15, 317–322. [Google Scholar]
- Chinese Society of Health Management Chinese Nutrition Society Reproductive Medicine Branch of China International Exchange; Promotion Association for Medicine; Healthcare China Health Promotion Foundation Zhejiang Provincial Clinical Nutrition Center. Expert consensus & standard on weight management for overweight or obese people. Chin. J. Health Manag. 2018, 12, 200–207. [Google Scholar]

| Serial Number | Literature Name | Time | Issuing Authority | Literature Type |
|---|---|---|---|---|
| Guide1 | Guidelines for medical nutrition treatment of overweight/obesity in China (2021) [15] | 2021 | Nutrition and Metabolic Management Branch of China International Exchange and Promotive Association for Medical and Health Care, Clinical Nutrition Branch of Chinese Nutrition Society, Chinese Diabetes Society, Chinese Society for Parenteral and Enteral Nutrition, Chinese Clinical Nutritionist Center of Chinese Medical Doctor Association | Evidence-based guidelines |
| Guide2 | American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity-Executive Summary [16] | 2016 | American Association of Clinical Endocrinologists | Evidence-based guidelines |
| Guide3 | 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults [17] | 2014 | ACC/AHA/TOS | Evidence-based guidelines |
| Guide4 | European Guidelines for Obesity Management in Adults [18] | 2015 | EASO | Evidence-based guidelines |
| Guide5 | Obesity: identification, assessment and management [19] | 2014 | NICE | Evidence-based guidelines |
| consensus1 | Expert consensus on the procedure of body weight management among patients with overweight or obesity (2021) [20] | 2021 | Chinese Society of Health Management, Clinical Nutrition Branch of Chinese Nutrition Society, Medical Nutrition Industry Branch of the National Association of Health Industry and Enterprise Management, the Editorial Board of Chinese Journal of Health Management | Expert consensus |
| consensus2 | Multidisciplinary Clinical Consensus on Obesity (2021) [21] | 2021 | Chinese Society of Endocrinology (CSE), Diabetes Society of China Association of Chinese Medicine (DSCACM), Chinese Society for Metabolic and Bariatric Surgery (CSMBS), Chinese Association of Research Hospitals (CSDBS) | Expert consensus |
| consensus3 | Expert consensus on nutritional therapy for patients with EC [22] | 2020 | Chinses Society of Nutritional Oncology | Expert consensus |
| consensus4 | Expert consensus on the weight management of overweight/obese infertility patients in China [23] | 2020 | Chinese Experts Consensus Group on the Body Quality Management Approach and Process for Overweight/Obese Infertility Patients. | Expert consensus |
| consensus5 | Expert consensus & standard on weight management for overweight or obese people [24] | 2018 | Chinese Society of Health Management Chinese Nutrition Society Reproductive Medicine Branch of China International Exchange and Promotion Association for Medicine and Healthcare China Health Promotion Foundation Zhejiang Provincial Clinical Nutrition Center | Expert consensus |
| Item | Frequency | Content |
|---|---|---|
| 1. Establishing the intervention development group | 6 | Establish a multidisciplinary diagnosis and treatment team for obesity management [16,17,18,19,20,21] |
| 2. Screening and evaluation | 10 | (1) Overweight and obese based on BMI [15,16,17,18,19,20,21,22,23,24] (2) Staging or classification of overweight and obesity based on BMI and comorbidities [20,23,24] (3) Patients’ history of overweight and obesity, complications and comorbidities, routine laboratory and instrument examination, energy intake and expenditure [15,16,18,20,24], lifestyle and behavioral ability assessment, psychological and quality of life assessment [15,18,19,21,24] |
| 3. Make a plan | 10 | (1) Set weight loss goals [18,20,22,24], 3 to 6 months of weight loss of 5% to 15% [18,20,24] (2) Develop an individualized diet and exercise program [16,17,18,19,20,21,23,24] (3) Develop a health education plan [20] |
| 4. Implementation plan | 7 | (1) Create a weight management profile [20] (2) Diet and exercise guidance [17,18,19,20,21,23,24] (3) Health education training [20,23,24] (4) Timely information support and psychological support [17,19,20,21,24] |
| 5. Supervision and evaluation | 5 | (1) Periodic follow-up monitoring [15,18,19,20,24] (2) Evaluation every 3 to 6 months [20] |
| 6. Adjust | 1 | Analyze the cause and adjust the cause [20] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, J.; Chen, Y.; Wang, Y.; Gong, Y.; Yang, D.; Li, X. Evidence-Based Weight Management for Fertility Preservation in Endometrial Cancer Patients: Developing a Complex Intervention Based on the Medical Research Council Framework. Healthcare 2025, 13, 1623. https://doi.org/10.3390/healthcare13131623
Gong J, Chen Y, Wang Y, Gong Y, Yang D, Li X. Evidence-Based Weight Management for Fertility Preservation in Endometrial Cancer Patients: Developing a Complex Intervention Based on the Medical Research Council Framework. Healthcare. 2025; 13(13):1623. https://doi.org/10.3390/healthcare13131623
Chicago/Turabian StyleGong, Jingjing, Yiqian Chen, Yongli Wang, Yuanyuan Gong, Dandan Yang, and Xiaodan Li. 2025. "Evidence-Based Weight Management for Fertility Preservation in Endometrial Cancer Patients: Developing a Complex Intervention Based on the Medical Research Council Framework" Healthcare 13, no. 13: 1623. https://doi.org/10.3390/healthcare13131623
APA StyleGong, J., Chen, Y., Wang, Y., Gong, Y., Yang, D., & Li, X. (2025). Evidence-Based Weight Management for Fertility Preservation in Endometrial Cancer Patients: Developing a Complex Intervention Based on the Medical Research Council Framework. Healthcare, 13(13), 1623. https://doi.org/10.3390/healthcare13131623







