From Perception to Action: Air Pollution Awareness and Behavioral Adjustments in Pregnant Women in Serbia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Ethical Considerations
2.4. Pregnancy-Related Data
2.5. Questionnaire
- Section 1: Demographic, Lifestyle, Residential, and Socioeconomic Characteristics
- Section 2: Perception of Air Quality and Information Engagement
- Section 3: Behavioral Adjustments and Recommendations
- Section 4: Perceived Health Effects and Psycho-Emotional Distress
2.6. Geospatial Assessment of Proximity to Land Use Attributes
2.7. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data
3.2. Lifestyle, Residential, and Socioeconomic Characteristics
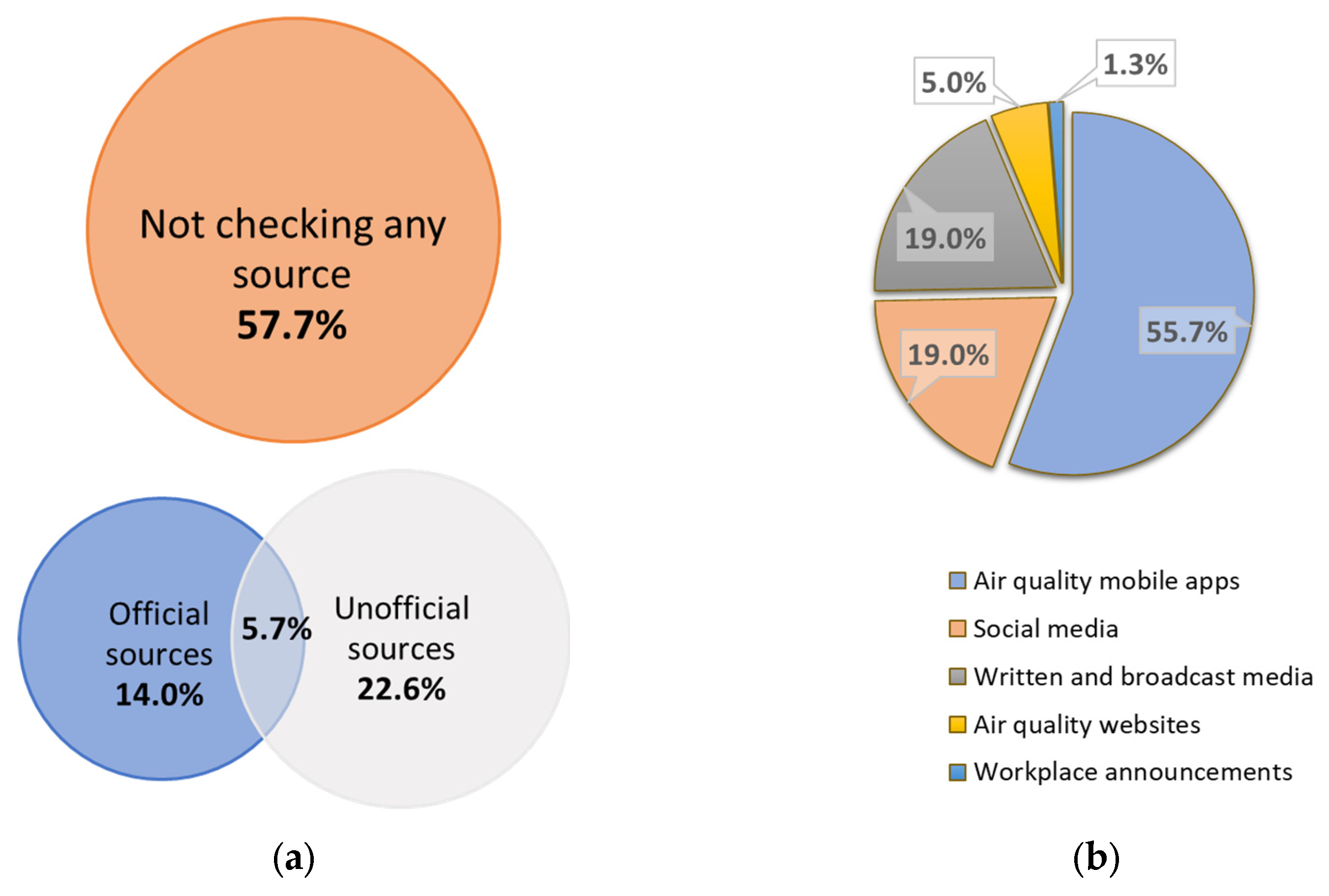
3.3. Perception of Air Quality and Information Engagement
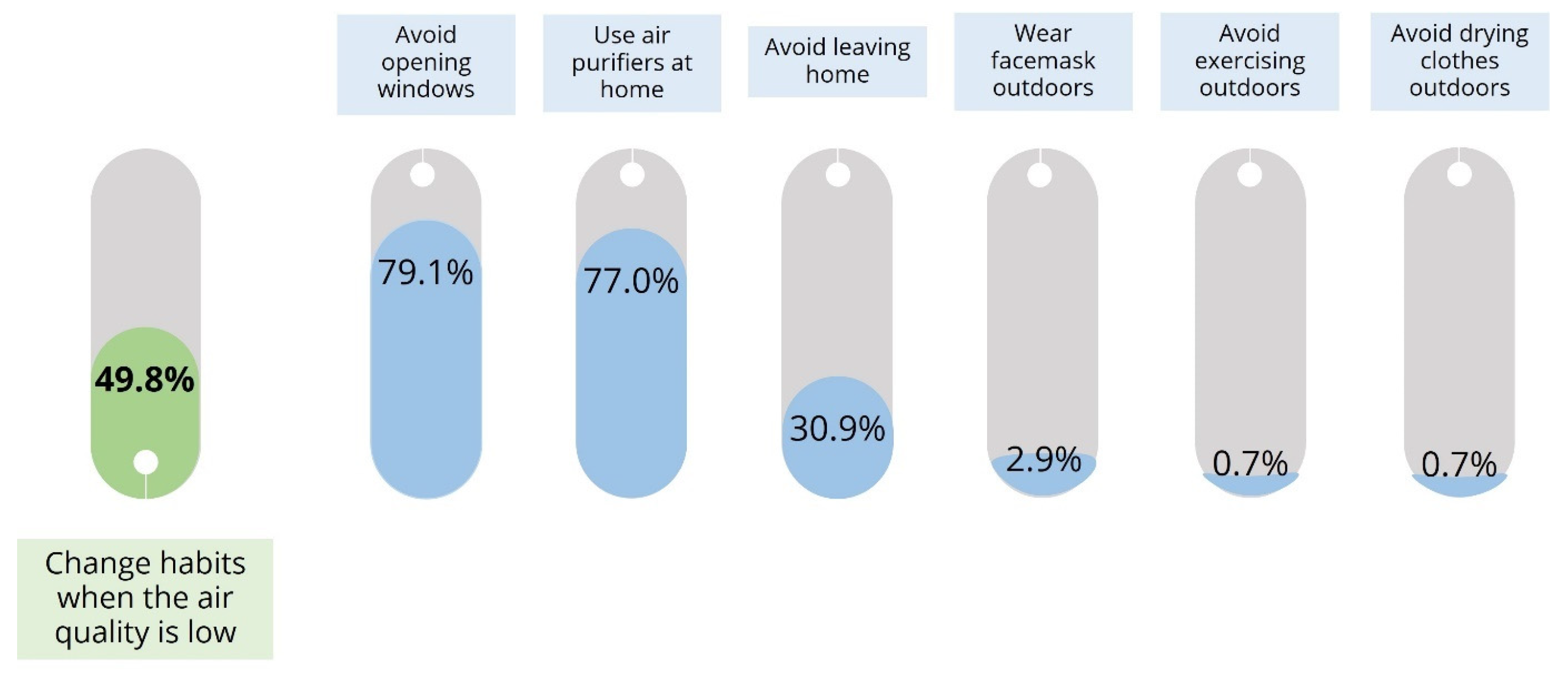
3.4. Behavioral Adjustments and Recommendations
3.5. Perceived Health Effects and Psycho-Emotional Distress
3.6. Geospatial Assessment of Proximity to Land Use Attributes
3.7. Regression Analysis of Behavioral Adjustments
4. Discussion
4.1. Perceptions in Light of Current Air Quality in Serbia
4.2. Understanding the Relationship Between Informational Accessibility, Perception, and Behavioral Responses Using Psychological Models
4.3. Limitations and Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, J.; Liu, F.; Liang, F.; Yang, Y.; Lu, X.; Gu, D. Air pollution exposure and vascular endothelial function: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2023, 30, 28525–28549. [Google Scholar] [CrossRef] [PubMed]
- Renzi, M.; Scortichini, M.; Forastiere, F.; De’ Donato, F.; Michelozzi, P.; Davoli, M.; Gariazzo, C.; Viegi, G.; Stafoggia, M.; BEEP Collaborative Group; et al. A nationwide study of air pollution from particulate matter and daily hospitalizations for respiratory diseases in Italy. Sci. Total Environ. 2022, 807, 151034. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Yang, X.; Hu, S.; Wang, Y.; Liu, J. Association between short-term exposure to air pollution and respiratory diseases among children in China: A systematic review and meta-analysis. Int. J. Environ. Health Res. 2022, 32, 2512–2532. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Oftedal, B.; Chen, J.; Rodopoulou, S.; Renzi, M.; Atkinson, R.W.; Bauwelinck, M.; Klompmaker, J.O.; Mehta, A.; Vienneau, D.; et al. Long-term exposure to low ambient air pollution concentrations and mortality among 28 million people: Results from seven large European cohorts within the ELAPSE project. Lancet Planet. Health 2022, 6, e9–e18. [Google Scholar] [CrossRef]
- GBD 2019 Diabetes and Air Pollution Collaborators. Estimates, trends, and drivers of the global burden of type 2 diabetes attributable to PM2·5 air pollution, 1990–2019: An analysis of data from the Global Burden of Disease Study 2019. Lancet Planet. Health 2022, 6, e586–e600. [Google Scholar] [CrossRef]
- Ha, S. Air pollution and neurological development in children. Dev. Med. Child. Neurol. 2021, 63, 374–381. [Google Scholar] [CrossRef]
- Roy, R.; D’Angiulli, A. Air pollution and neurological diseases, current state highlights. Front. Neurosci. 2024, 18, 1351721. [Google Scholar] [CrossRef]
- Jiang, F.; Zhao, J.; Sun, J.; Chen, W.; Zhao, Y.; Zhou, S.; Yuan, S.; Timofeeva, M.; Law, P.J.; Larsson, S.C.; et al. Impact of ambient air pollution on colorectal cancer risk and survival: Insights from a prospective cohort and epigenetic Mendelian randomization study. EBioMedicine 2024, 103, 105126. [Google Scholar] [CrossRef]
- Zare Sakhvidi, M.J.; Lequy, E.; Goldberg, M.; Jacquemin, B. Air pollution exposure and bladder, kidney and urinary tract cancer risk: A systematic review. Environ. Pollut. 2020, 267, 115328. [Google Scholar] [CrossRef]
- Bai, W.; Li, Y.; Niu, Y.; Ding, Y.; Yu, X.; Zhu, B.; Duan, R.; Duan, H.; Kou, C.; Li, Y.; et al. Association between ambient air pollution and pregnancy complications: A systematic review and meta-analysis of cohort studies. Environ. Res. 2020, 185, 109471. [Google Scholar] [CrossRef]
- Nyadanu, S.D.; Dunne, J.; Tessema, G.A.; Mullins, B.; Kumi-Boateng, B.; Lee Bell, M.; Duko, B.; Pereira, G. Prenatal exposure to ambient air pollution and adverse birth outcomes: An umbrella review of 36 systematic reviews and meta-analyses. Environ. Pollut. 2022, 306, 119465. [Google Scholar] [CrossRef] [PubMed]
- Chandra, M.; Paray, A.A. Natural Physiological Changes During Pregnancy. Yale J. Biol. Med. 2024, 97, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Liu, Q.; Hou, H.; Guo, G.; Zhang, T.; Fan, S.; Wang, L. Association of Ambient air Pollution with risk of preeclampsia during pregnancy: A retrospective cohort study. BMC Public Health 2020, 20, 1663. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Zhu, H.; Xu, J.; Zhao, Z.; Zhou, L.; Zhu, Q.; Cai, J.; Ji, L. Ambient air pollution and gestational diabetes mellitus: An updated systematic review and meta-analysis. Ecotoxicol. Environ. Saf. 2023, 255, 114802. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, C.; Liu, D.; Ha, S.; Kim, S.S.; Pollack, A.; Mendola, P. Ambient Air Pollution and Risk of Gestational Hypertension. Am. J. Epidemiol. 2017, 186, 334–343. [Google Scholar] [CrossRef]
- Hackley, B.; Feinstein, A.; Dixon, J. Air pollution: Impact on maternal and perinatal health. J. Midwifery Womens Health 2007, 52, 435–443. [Google Scholar] [CrossRef]
- Salavati, N.; Strak, M.; Burgerhof, J.G.M.; de Walle, H.E.K.; Erwich, J.J.H.M.; Bakker, M.K. The association of air pollution with congenital anomalies: An exploratory study in the northern Netherlands. Int. J. Hyg. Environ. Health 2018, 221, 1061–1067. [Google Scholar] [CrossRef]
- Marchetti, D.; Carrozzino, D.; Fraticelli, F.; Fulcheri, M.; Vitacolonna, E. Quality of Life in Women with Gestational Diabetes Mellitus: A Systematic Review. J. Diabetes Res. 2017, 2017, 7058082. [Google Scholar] [CrossRef]
- Zakour Khadari, M.; Zainal, H.; Athirah Daud, N.A.; Sha’aban, A. Health-Related Quality of Life in Pregnant Women with Gestational Hypertension: A Systematic Review. Cureus 2024, 16, e61340. [Google Scholar] [CrossRef]
- Llop, S.; Ballester, F.; Estarlich, M.; Esplugues, A.; Fernández-Patier, R.; Ramón, R.; Marco, A.; Aguirre, A.; Sunyer, J.; Iñiguez, C. Ambient air pollution and annoyance responses from pregnant women. Atmos. Environ. 2008, 42, 2982–2992. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Personal-Level Actions to Reduce Air Pollution Exposure in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2024; Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2024-9115-48887-72806 (accessed on 27 January 2025).
- Fournis, Y.; Fortin, M.J. From social ‘acceptance’ to social ‘acceptability’ of wind energy projects: Towards a territorial perspective. J. Environ. Plan. Manag. 2017, 60, 1–21. [Google Scholar] [CrossRef]
- Huang, Y.J.; Lee, P.H.; Hsieh, S.H.; Chiu, Y.C.; Chan, T.C. Understanding factors influencing adoption of air pollution protective measures using the knowledge-attitude-behavior model. Sci. Rep. 2024, 14, 28414. [Google Scholar] [CrossRef] [PubMed]
- Lou, B.; Barbieri, D.M.; Passavanti, M.; Hui, C.; Gupta, A.; Hoff, I.; Lessa, D.A.; Sikka, G.; Chang, K.; Fang, K.; et al. Air pollution perception in ten countries during the COVID-19 pandemic. Ambio 2022, 51, 531–545. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Kwan, M.P.; Huang, J. Assessment of air pollution and air quality perception mismatch using mobility-based real-time exposure. PLoS ONE 2024, 19, e0294605. [Google Scholar] [CrossRef]
- Cardinali, M.; Beenackers, M.A.; Timmeren, A.V.; Pottgiesser, U. Urban green spaces, self-rated air pollution and health: A sensitivity analysis of green space characteristics and proximity in four European cities. Health Place 2024, 89, 103300. [Google Scholar] [CrossRef]
- Alyafei, A.; Easton-Carr, R. The Health Belief Model of Behavior Change. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2025. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- McCarron, A.; Semple, S.; Swanson, V.; Braban, C.F.; Gillespie, C.; Price, H.D. “I have to stay inside …”: Experiences of air pollution for people with asthma. Health Place 2024, 85, 103150. [Google Scholar] [CrossRef]
- EEA. Europe’s Air Quality Status 2024. Available online: https://www.eea.europa.eu//publications/europes-air-quality-status-2024 (accessed on 27 January 2025).
- Environmental Protection Agency. Annual Report on the State of Air Quality in the Republic of Serbia for 2023; Environmental Protection Agency: Belgrade, Serbia, 2024. Available online: https://sepa.gov.rs/wp-content/uploads/2024/10/Vazduh2023.pdf (accessed on 15 January 2025). (In Serbian)
- Olander, E.K.; Smith, D.M.; Darwin, Z. Health behaviour and pregnancy: A time for change. J. Reprod. Infant. Psychol. 2018, 36, 1–3. [Google Scholar] [CrossRef]
- OECD. Applying the Degree of Urbanisation: A Methodological Manual to Define Cities, Towns and Rural Areas for International Comparisons; Paris/European Union; OECD Regional Development Studies, OECD Publishing: Brussels, Belgium, 2021; Available online: https://www.oecd.org/en/publications/applying-the-degree-of-urbanisation_4bc1c502-en.html (accessed on 31 January 2025).
- Statute of the City of Belgrade. Official Gazette of the City of Belgrade, Nos. 39/08, 6/10, 23/13, 60/19. 2008. Available online: https://www.sllistbeograd.rs/documents/statut_grada_lat.pdf (accessed on 31 January 2025). (In Serbian).
- Regulation on Monitoring Conditions and Air Quality Requirements. Official Gazette of the Republic of Serbia, Nos. 11/2010, 75/2010, 63/2013. 2010. Available online: https://pravno-informacioni-sistem.rs/eli/rep/sgrs/vlada/uredba/2010/11/9/reg (accessed on 27 January 2025). (In Serbian).
- Environmental Protection Agency. Annual Report on the State of Air Quality in the Republic of Serbia for 2010; Environmental Protection Agency: Belgrade, Serbia, 2011. Available online: https://sepa.gov.rs/wp-content/uploads/2024/10/Vazduh2010.pdf (accessed on 15 January 2025). (In Serbian)
- Republic of Serbia. Air Quality Programme of the Republic of Serbia for the Period 2022–2030 with an Action Plan; Ministry of Environmental Protection: Belgrade, Serbia, 2022. Available online: https://www.ekologija.gov.rs/sites/default/files/2023-03/en_aq_programme_adopted_version.pdf (accessed on 1 June 2025).
- Chiarini, B.; D’Agostino, A.; Marzano, E.; Regoli, A. The perception of air pollution and noise in urban environments: A subjective indicator across European countries. J. Environ. Manag. 2020, 263, 110272. [Google Scholar] [CrossRef]
- Piracha, A.; Chaudhary, M.T. Urban Air Pollution, Urban Heat Island and Human Health: A Review of the Literature. Sustainability 2022, 14, 9234. [Google Scholar] [CrossRef]
- Kim, D.; Song, S.-K. The Multifunctional Benefits of Green Infrastructure in Community Development: An Analytical Review Based on 447 Cases. Sustainability 2019, 11, 3917. [Google Scholar] [CrossRef]
- Berglund, E.; Westerling, R.; Lytsy, P. Housing Type and Neighbourhood Safety Behaviour Predicts Self-rated Health, Psychological Well-being and Frequency of Recent Unhealthy Days: A Comparative Cross-sectional Study of the General Population in Sweden. Plan Pract. Res. 2017, 32, 444–465. [Google Scholar] [CrossRef]
- Yu, X.; Fan, Y.; Kim, J.S.; Chung, H.; Lord, A.; Dunning, R. Is ignorance bliss? Evaluating information awareness and life satisfaction through the lens of perceived air pollution: The case of Beijing, China. J. Environ. Manag. 2024, 371, 123087. [Google Scholar] [CrossRef] [PubMed]
- Zielonka, T.M. Awareness of Polish physicians regarding the impact of air pollution on health. Arch. Environ. Occup. Health 2022, 77, 478–485. [Google Scholar] [CrossRef]
- Mirabelli, M.C.; Damon, S.A.; Beavers, S.F.; Sircar, K.D. Patient–Provider Discussions About Strategies to Limit Air Pollution Exposures. Am. J. Prev. Med. 2018, 55, e49–e52. [Google Scholar] [CrossRef]
- Boso, À.; Oltra, C.; Álvarez, B.; Garrido, J.; Hofflinger, Á.; Gálvez-García, G. Why do we misperceive air pollution? A scoping review of key judgmental biases. Air Qual. Atmos. Health 2025, 18, 447–460. [Google Scholar] [CrossRef]
- Bullinger, M. Psychological effects of air pollution on healthy residents—A time-series approach. J. Environ. Psychol. 1989, 9, 103–118. [Google Scholar] [CrossRef]
- Sun, Y.; Headon, K.S.; Jiao, A.; Slezak, J.M.; Avila, C.C.; Chiu, V.Y.; Sacks, D.A.; Molitor, J.; Benmarhnia, T.; Chen, J.C.; et al. Association of Antepartum and Postpartum Air Pollution Exposure with Postpartum Depression in Southern California. JAMA Netw. Open 2023, 6, e2338315. [Google Scholar] [CrossRef]
- Tan, J.; Chen, N.; Bai, J.; Yan, P.; Ma, X.; Ren, M.; Maitland, E.; Nicholas, S.; Cheng, W.; Leng, X.; et al. Ambient air pollution and the health-related quality of life of older adults: Evidence from Shandong China. J. Environ. Manag. 2023, 336, 117619. [Google Scholar] [CrossRef]
- Stone, A.A.; Bachrach, C.A.; Jobe, J.B.; Kurtzman, H.S.; Cain, V.S. (Eds.) The Science of Self-Report: Implications for Research and Practice; Psychology Press: New York, NY, USA, 1999; 392p. [Google Scholar]
- Tatit, P.; Adhinugraha, K.; Taniar, D. Navigating the Maps: Euclidean vs. Road Network Distances in Spatial Queries. Algorithms 2024, 17, 29. [Google Scholar] [CrossRef]
- Davies, G.; Whyatt, J.D. A network-based approach for estimating pedestrian journey-time exposure to air pollution. Sci. Total Environ. 2014, 485–486, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Azmi, W.N.F.W.; Pillai, T.R.; Latif, M.T.; Koshy, S.; Shaharudin, R. Application of land use regression model to assess outdoor air pollution exposure: A review. Environ. Adv. 2023, 11, 100353. [Google Scholar] [CrossRef]
- Shukla, K.; Kumar, P.; Mann, G.S.; Khare, M. Mapping spatial distribution of particulate matter using Kriging and Inverse Distance Weighting at supersites of megacity Delhi. Sustain. Cities Soc. 2020, 54, 101997. [Google Scholar] [CrossRef]


| Characteristics | Mean/N | SD/% |
|---|---|---|
| Age (years) (mean/SD) | 31.8 | 4.9 |
| Weight gain during pregnancy (kg) (mean/SD) | 14.3 | 7.4 |
| Body Mass Index at delivery (kg/m2) (mean/SD) | 28.4 | 4.3 |
| Total number of deliveries (mean/SD) | 1.5 | 0.7 |
| Gestational weeks at the time of delivery (mean/SD) | 38.9 | 1.3 |
| Type of delivery (N/%) | ||
| Vaginal delivery | 190 | 68.1 |
| Cesarean section | 89 | 31.9 |
| Characteristics | Number of Participants (N) | Percentage of Participants (%) |
|---|---|---|
| Lifestyle | ||
| Smoking status | ||
| No | 200 | 71.7 |
| Yes | 29 | 10.4 |
| Former smokers | 50 | 17.9 |
| Smoking in households | ||
| No | 143 | 51.2 |
| Yes | 78 | 28.0 |
| Yes, but not in the vicinity/room | 58 | 20.8 |
| Residence | ||
| Type of residence | ||
| House | 113 | 40.5 |
| Apartment building | 166 | 59.5 |
| Residential floor level | ||
| Ground to 2nd | 195 | 69.9 |
| 3rd to 5th | 73 | 26.2 |
| 6th and higher | 11 | 3.9 |
| Window orientation | ||
| Overlooking the street | 95 | 34.1 |
| Overlooking the yard | 94 | 33.7 |
| Both | 90 | 32.2 |
| Socioeconomic indicators | ||
| Employment status | ||
| Employed | 227 | 81.4 |
| Unemployed | 52 | 18.6 |
| Level of formal education | ||
| Elementary/middle/high school | 86 | 30.9 |
| Bachelor’s degree | 150 | 53.8 |
| Postgraduate education | 43 | 15.4 |
| Perceived family income | ||
| Good | 133 | 47.7 |
| Fair/poor | 146 | 52.3 |
| β * | p Value * | OR * | 95% CI * | |
|---|---|---|---|---|
| Residential characteristics | ||||
| Urban–rural typology | −0.429 | 0.210 | 0.651 | 0.333–1.274 |
| Type of residence | 0.398 | 0.239 | 1.489 | 0.768–2.886 |
| Window orientation (ref: overlooking the street) | ||||
| Overlooking the yard | −0.111 | 0.750 | 0.895 | 0.453–1.768 |
| Both | 0.230 | 0.348 | 0.711 | 0.348–1.445 |
| Sociodemographic characteristics | ||||
| Employment status | 0.071 | 0.800 | 1.074 | 0.518–2.226 |
| Level of formal education (ref: elementary/middle/high school) | ||||
| Bachelor’s degree | 0.248 | 0.469 | 1.281 | 0.655–2.506 |
| Postgraduate education | −0.122 | 0.800 | 0.885 | 0.344–2.275 |
| Perceived family income | −0.754 | 0.016 | 0.470 | 0.255–0.876 |
| Euclidian Distance from Participants’ Residential Addresses (m) | ||
|---|---|---|
| Land Use Attribute | Median | IQR |
| Urban green area | 335.4 | 628.5 |
| Forests | 1150.0 | 1217.4 |
| Water | 2607.7 | 3103.7 |
| Continuous Urban Fabric | 194.2 | 1120.4 |
| Perception of Air Quality N (%) | ||||
|---|---|---|---|---|
| Land use attribute | Good | Fair | Poor | Spearman’s correlation |
| Urban green areas | ||||
| Q1 ≤ 180.3 m | 1 (1.6) | 18 (28.1) | 45 (70.3) | ρ = −0.170 ** |
| Q2 = 180.4–335.3 m | 0 (0.0) | 14 (18.4) | 62 (81.6) | |
| Q3 = 335.5–807.8 m | 3 (4.3) | 18 (26.1) | 48 (69.6) | |
| Q4 ≥ 807.9 m | 5 (7.1) | 28 (40.0) | 37 (52.9) | |
| Forests | ||||
| Q1 ≤ 626.5 m | 5 (7.0) | 32 (45.1) | 34 (47.9) | ρ = 0.206 ** |
| Q2 = 626.6–1150.0 m | 3 (4.4) | 13 (19.1) | 52 (76.5) | |
| Q3 = 1150.1–1843.9 m | 1 (1.4) | 15 (21.4) | 54 (77.2) | |
| Q4 ≥ 1844.0 m | 0 (0.0) | 18 (25.7) | 52 (74.3) | |
| Water | ||||
| Q1 ≤ 1141.3 m | 0 (0.0) | 12 (17.4) | 57 (82.6) | ρ = −0.242 *** |
| Q2 = 1141.4–2607.7 m | 1 (1.4) | 19 (26.8) | 51 (71.8) | |
| Q3 = 2607.8–4245.0 m | 2 (2.9) | 19 (27.5) | 48 (69.6) | |
| Q4 ≥ 4245.1 m | 6 (8.6) | 28 (40.4) | 36 (51.4) | |
| Continuous urban fabric | ||||
| Q1 ≤ 30.0 m, | 0 (0.0) | 8 (11.4) | 62 (88.6) | ρ = −0.328 *** |
| Q2 = 30.1–194.2 m | 0 (0.0) | 20 (29.0) | 49 (71.0) | |
| Q3 = 194.3–1150 m | 1 (1.4) | 20 (28.6) | 49 (70.0) | |
| Q4 ≥ 1150.5 m | 8 (11.4) | 30 (42.9) | 32 (45.7) | |
| Land Use Attributes | β * | p Value * | OR * | 95% CI * |
|---|---|---|---|---|
| Urban green areas (ref: Q1) | ||||
| Q2 | 0.557 | 0.210 | 1.747 | 0.730–4.179 |
| Q3 | 0.416 | 0.329 | 1.516 | 0.657–3.500 |
| Q4 | 0.301 | 0.537 | 1.351 | 0.520–3.512 |
| Forests (ref: Q1) | ||||
| Q2 | 1.054 | 0.009 | 2.868 | 1.294–6.355 |
| Q3 | 0.950 | 0.021 | 2.585 | 1.152–5.800 |
| Q4 | 1.078 | 0.008 | 2.938 | 1.323–6.525 |
| Water (ref: Q1) | ||||
| Q2 | −0.702 | 0.112 | 0.495 | 0.208–1.117 |
| Q3 | −0.830 | 0.064 | 0.436 | 0.181–1.049 |
| Q4 | −1.183 | 0.008 | 0.306 | 0.127–0.738 |
| Continuous urban fabric (ref: Q1) | ||||
| Q2 | −1.023 | 0.034 | 0.360 | 0.139–0.928 |
| Q3 | −0.896 | 0.069 | 0.408 | 0.155–1.072 |
| Q4 | −1.714 | 0.003 | 0.180 | 0.059–0.558 |
| Characteristics | Model 1 (Perception Unadjusted) | Model 2 (Perception + Sociodemographic + Residential Characteristics) | Model 3 (Perception + Proximity to Land Use Attributes) | Model 4 (Fully Combined) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Air quality perception | 1.563 (1.050–2.936) | 0.032 | 1.333 (0.759–2.343) | 0.317 | 1.626 (0.906–2.920) | 0.103 | 1.500 (0.801–2.809) | 0.205 |
| Urban–rural typology | — | — | 0.694 (0.352–1.368) | 0.291 | — | — | 0.379 (0.142–1.010) | 0.052 |
| Type of residence | — | — | 2.626 (1.397–4.937) | 0.003 | — | — | 3.265 (1.627–6.552) | 0.001 |
| Window orientation (ref: overlooking the street) | ||||||||
| Overlooking the yard | — | — | 1.104 (0.600–2.032) | 0.751 | — | — | 1.091 (0.576–2.069) | 0.567 |
| Both | — | — | 1.330 (0.673–2.629) | 0.413 | — | — | 1.388 (0.672–2.865) | 0.672 |
| Employment status | — | — | 0.670 (0.332–1.355) | 0.265 | — | — | 0.677 (0.325–1.409) | 0.297 |
| Level of formal education (ref: elementary/middle/high school) | ||||||||
| Bachelor’s degree | — | — | 1.027 (0.544–1.940) | 0.934 | — | — | 1.122 (0.570–2.206) | 0.740 |
| Postgraduate education | — | — | 1.557 (0.658–3.781) | 0.307 | — | — | 1.578 (0.620–4.062) | 0.336 |
| Perceived family income | — | — | 0.611 (0.347–1.079) | 0.090 | — | — | 0.549 (0.301–1.003) | 0.051 |
| Urban green areas (ref: Q1) | ||||||||
| Q2 | — | — | — | — | 0.440 (0.214–0.904) | 0.025 | 0.517 (0.241–1.111) | 0.091 |
| Q3 | — | — | — | — | 0.868 (0.416–1.813) | 0.707 | 1.074 (0.495–2.333) | 0.856 |
| Q4 | — | — | — | — | 0.366 (0.153–0.869) | 0.024 | 0.712 (0.271–1.871) | 0.491 |
| Forests (ref: Q1) | ||||||||
| Q2 | — | — | — | — | 1.311 (0.636–2.704) | 0.463 | 1.198 (0.556–2.579) | 0.645 |
| Q3 | — | — | — | — | 1.611 (0.773–3.355) | 0.203 | 1.382 (0.630–3.031) | 0.419 |
| Q4 | — | — | — | — | 1.002 (0.482–2.084) | 0.995 | 1.234 (0.564–2.702) | 0.599 |
| Water (ref: Q1) | ||||||||
| Q2 | — | — | — | — | 0.517 (0.255–1.050) | 0.068 | 0.499 (0.236–1.054) | 0.068 |
| Q3 | — | — | — | — | 1.296 (0.636–2.642) | 0.476 | 1.276 (0.591–2.755) | 0.535 |
| Q4 | — | — | — | — | 0.984 (0.466–2.077) | 0.966 | 0.939 (0.425–2.076) | 0.877 |
| Continuous urban fabric (ref: Q1) | ||||||||
| Q2 | — | — | — | — | 0.725 (0.351–1.509) | 0.393 | 0.732 (0.339–1.584) | 0.428 |
| Q3 | — | — | — | — | 0.861 (0.408–1.817) | 0.695 | 0.987 (0.447–2.178) | 0.974 |
| Q4 | — | — | — | — | 0.942 (0.362–2.450) | 0.903 | 2.836 (0.843–9.555) | 0.092 |
| Nagelkerke R2 | 0.022 | 0.140 | 0.103 | 0.213 | ||||
| −2 Log likelihood | 383.1 | 355.9 | 364.3 | 338.3 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Susa, A.; Zekovic, M.; Davidovic, D.; Paunovic, K.; Kujundzic, V.; Mihajlovic, S.; Bogdanovic, L. From Perception to Action: Air Pollution Awareness and Behavioral Adjustments in Pregnant Women in Serbia. Healthcare 2025, 13, 1475. https://doi.org/10.3390/healthcare13121475
Susa A, Zekovic M, Davidovic D, Paunovic K, Kujundzic V, Mihajlovic S, Bogdanovic L. From Perception to Action: Air Pollution Awareness and Behavioral Adjustments in Pregnant Women in Serbia. Healthcare. 2025; 13(12):1475. https://doi.org/10.3390/healthcare13121475
Chicago/Turabian StyleSusa, Ana, Milica Zekovic, Dragana Davidovic, Katarina Paunovic, Vera Kujundzic, Sladjana Mihajlovic, and Ljiljana Bogdanovic. 2025. "From Perception to Action: Air Pollution Awareness and Behavioral Adjustments in Pregnant Women in Serbia" Healthcare 13, no. 12: 1475. https://doi.org/10.3390/healthcare13121475
APA StyleSusa, A., Zekovic, M., Davidovic, D., Paunovic, K., Kujundzic, V., Mihajlovic, S., & Bogdanovic, L. (2025). From Perception to Action: Air Pollution Awareness and Behavioral Adjustments in Pregnant Women in Serbia. Healthcare, 13(12), 1475. https://doi.org/10.3390/healthcare13121475


_MD__MPH_PhD.png)






