Associations of Body Mass Index and Lifestyle Factors with Suicidal Ideation, Planning, and Attempts Among Korean Adolescents: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
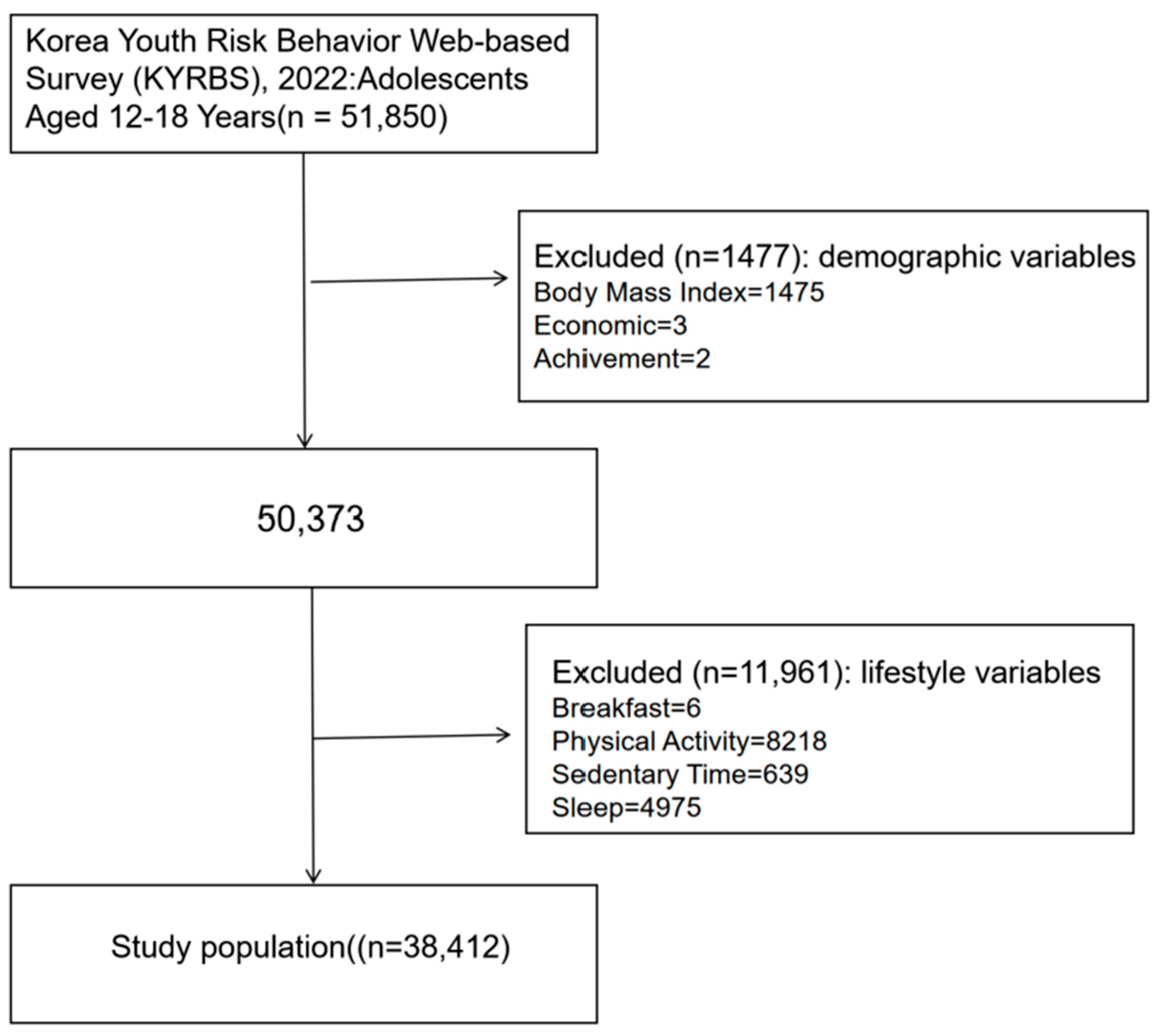
2.1. Data Sources and Study Design
2.2. Dependent Variable
2.3. Independent Variables
2.3.1. Sleep Time
2.3.2. Dietary Health
2.3.3. Physical Activity
2.3.4. Sedentary Time
2.3.5. Smoking
2.3.6. Hazardous Drinking
2.4. Covariates
2.5. BMI
2.6. Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Association Between Lifestyle Factors and Adolescent Suicide Risk
3.3. Subgroup Analysis of Adolescents
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fonseca-Pedrero, E.; Al-Halabí, S.; Pérez-Albéniz, A.; Debbané, M. Risk and Protective Factors in Adolescent Suicidal Behaviour: A Network Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1784. [Google Scholar] [CrossRef] [PubMed]
- Obesity—Our World in Data. Available online: https://ourworldindata.org/obesity (accessed on 7 November 2023).
- Glenn, C.R.; Kleiman, E.M.; Kellerman, J.; Pollak, O.; Cha, C.B.; Esposito, E.C.; Porter, A.C.; Wyman, P.A.; Boatman, A.E. Annual Research Review: A Meta-Analytic Review of Worldwide Suicide Rates in Adolescents. J. Child Psychol. Psychiatry 2020, 61, 294–308. [Google Scholar] [CrossRef] [PubMed]
- KDCA KDCA. Available online: https://www.kdca.go.kr (accessed on 3 May 2024).
- Li, Y.; Li, P.; Yuan, M.; Li, Y.; Zhang, X.; Chen, J.; Wang, G.; Su, P. Social-Ecological Perspective on the Suicidal Behaviour Factors of Early Adolescents in China: A Network Analysis. Gen. Psychiatry 2024, 37, e101317. [Google Scholar] [CrossRef] [PubMed]
- Kelly-Irving, M.; Vineis, P. Life-course approach: From socioeconomic determinants to biological embodiment. In Reducing Social Inequalities in Cancer: Evidence and Priorities for Research; International Agency for Research on Cancer: Lyon, France, 2019. [Google Scholar]
- Zhang, M.; Tang, R.; Rao, W.; Wang, M.; Liu, M.-W.; Yu, H.; He, Q. Body Mass Index and the Risk of Suicidal Ideation and Suicide Attempt among Youth in 45 Low-and Middle-Income Countries. J. Affect. Disord. 2022, 298, 357–363. [Google Scholar] [CrossRef]
- Liu, J.; Jia, F.; Li, C.; Yuan, H.; Yang, H.; Yang, R.; Yue, Y.; Zhang, G.; Zhang, X.; Ye, G.; et al. Association between Body Mass Index and Suicide Attempts in Chinese Patients of a Hospital in Shanxi District with First-Episode Drug-Naïve Major Depressive Disorder. J. Affect. Disord. 2023, 339, 377–383. [Google Scholar] [CrossRef]
- Liu, J.; Li, Z.; Jia, F.; Yuan, H.; Zhou, Y.; Xia, X.; Yang, R.; Wu, Y.; Zhang, X.; Ye, G.; et al. Gender Differences in the Association between Body Mass Index and Recent Suicide Attempts in Chinese Patients with First-Episode Drug-Naïve Major Depressive Disorder. Sci. Rep. 2023, 13, 16033. [Google Scholar] [CrossRef]
- Hochgraf, A.K.; Berge, J.M.; Lanza, S.T. Age-Varying Associations between Attempts to Change Weight and Suicidal Ideation among Adolescents in the United States. Prev. Med. 2024, 182, 107946. [Google Scholar] [CrossRef]
- Ninla-aesong, P.; Puangsri, P.; Kietdumrongwong, P.; Jongkrijak, H.; Noipha, K. Being Overweight and Obese Increases Suicide Risk, the Severity of Depression, and the Inflammatory Response in Adolescents with Major Depressive Disorders. Front. Immunol. 2023, 14, 1197775. [Google Scholar] [CrossRef]
- Elia, C.; Karamanos, A.; Dregan, A.; O’Keeffe, M.; Wolfe, I.; Sandall, J.; Morgan, C.; Cruickshank, J.K.; Gobin, R.; Wilks, R.; et al. Association of Macro-Level Determinants with Adolescent Overweight and Suicidal Ideation with Planning: A Cross-Sectional Study of 21 Latin American and Caribbean Countries. PLoS Med. 2020, 17, e1003443. [Google Scholar] [CrossRef]
- Graham, C.E.; Frisco, M.L. The Mental “Weight” of Discrimination: The Relationship between Perceived Interpersonal Weight Discrimination and Suicidality in the United States. J. Health Soc. Behav. 2023, 64, 610–625. [Google Scholar] [CrossRef]
- Iwatate, E.; Atem, F.D.; Jones, E.C.; Hughes, J.L.; Yokoo, T.; Messiah, S.E. Trends in the Relationship between Suicide Behaviors and Obesity among Adolescents in the United States from 1999 to 2019. Eur. Child Adolesc. Psychiatry 2024, 33, 725–737. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; He, X.; Tang, Y.; Tang, J.; Yang, J. Unveiling the Links between Physical Activity, Self-Identity, Social Anxiety, and Emotional Eating among Overweight and Obese Young Adults. Front. Psychol. 2024, 14, 1255548. [Google Scholar] [CrossRef] [PubMed]
- Iwatate, E.; Atem, F.D.; Jones, E.C.; Hughes, J.L.; Yokoo, T.; Messiah, S.E. Association of Obesity, Suicide Behaviors, and Psychosocial Wellness Among Adolescents in the United States. J. Adolesc. Health 2023, 72, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Solmi, F.; Sharpe, H.; Gage, S.H.; Maddock, J.; Lewis, G.; Patalay, P. Changes in the Prevalence and Correlates of Weight-Control Behaviors and Weight Perception in Adolescents in the UK, 1986–2015. JAMA Pediatr. 2021, 175, 267. [Google Scholar] [CrossRef]
- Li, X.; Chi, G.; Taylor, A.; Chen, S.-T.; Memon, A.R.; Zhang, Y.; Song, Y.; Li, J.; Luo, X.; Zou, L. Lifestyle Behaviors and Suicide-Related Behaviors in Adolescents: Cross-Sectional Study Using the 2019 YRBS Data. Front. Public Health 2021, 9, 766972. [Google Scholar] [CrossRef]
- Glenn, C.R.; Kleiman, E.M.; Kearns, J.C.; Boatman, A.E.; Conwell, Y.; Alpert-Gillis, L.J.; Pigeon, W. Sleep Problems Predict Next-Day Suicidal Thinking among Adolescents: A Multimodal Real-Time Monitoring Study Following Discharge from Acute Psychiatric Care. Dev. Psychopathol. 2021, 33, 1701–1721. [Google Scholar] [CrossRef]
- Michael, S.L.; Lowry, R.; Merlo, C.; Cooper, A.C.; Hyde, E.T.; McKeon, R. Physical Activity, Sedentary, and Dietary Behaviors Associated with Indicators of Mental Health and Suicide Risk. Prev. Med. Rep. 2020, 19, 101153. [Google Scholar] [CrossRef]
- Silva, A.F.D.; Júnior, C.A.S.A.; Hinnig, P.D.F.; Lima, L.R.A.D.; Silva, D.A.S. Suicidal Behaviors and Sedentary Lifestyles among Adolescents: A Cross-Sectional Epidemiological Study in Latin American and Caribbean Countries. Clinics 2020, 75, e2015. [Google Scholar] [CrossRef]
- Fabiano, N.; Gupta, A.; Fiedorowicz, J.G.; Firth, J.; Stubbs, B.; Vancampfort, D.; Schuch, F.B.; Carr, L.J.; Solmi, M. The Effect of Exercise on Suicidal Ideation and Behaviors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Affect. Disord. 2023, 330, 355–366. [Google Scholar] [CrossRef]
- Pakalska-Korcala, A.; Suligowska, K.; Wolańczyk, T.; Zdrojewski, T. Depression and Smoking—Widespread Health Problems among 14-Year-Old Adolescents in Poland. The Results of the SOPKARD-Junior Survey. Psychiatr. Pol. 2021, 55, 113–125. [Google Scholar] [CrossRef]
- Song, Y.; Liu, J.; Zhao, Y.; Gong, L.; Chen, Q.; Jiang, X.; Zhang, J.; Hao, Y.; Zhou, H.; Lou, X.; et al. Unhealthy Lifestyles and Clusters Status among 3637 Adolescents Aged 11–23 Years: A School-Based Cross-Sectional Study in China. BMC Public Health 2023, 23, 1279. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Nam, J.Y. Do Lifestyle Risk Behaviors Affect Anxiety, Depressive Symptoms, and Suicidal Ideation among Adolescents? Psychiatry Res. 2022, 318, 114942. [Google Scholar] [CrossRef] [PubMed]
- Healthy Lifestyle: From Pediatrics to Geriatrics; Kelishadi, R., Ed.; Integrated Science; Springer International Publishing: Cham, Switzerland, 2022; Volume 3, ISBN 978-3-030-85356-3. [Google Scholar]
- Main, K.; Whatman, S. Health and Well-Being in the Middle Grades: Research for Effective Middle Level Education; IAP: Charlotte, NC, USA, 2023; ISBN 9798887302034. [Google Scholar]
- Ortiz, C.; López-Cuadrado, T.; Rodríguez-Blázquez, C.; Simón, L.; Perez-Vicente, R.; Merlo, J.; Galán, I. Physical and Social Environmental Factors Related to Co-Occurrence of Unhealthy Lifestyle Behaviors. Health Place 2022, 75, 102804. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Shin, D.; Ahn, Y.M. Association between the Number of Hours of Sleep during Weekdays and Suicidality among Korean Adolescents: Mediating Role of Depressive and Anxiety Symptoms. J. Affect. Disord. 2023, 320, 74–80. [Google Scholar] [CrossRef]
- Lee, S.-H.; Lee, J.-H. Analysis on the Relationship between Eating Behavior, Physical Activities and Youth Obesity: Based on the Korea Youth Risk Behavior Survey for High School Students in 2016~2018. Information 2020, 11, 169. [Google Scholar] [CrossRef]
- Kim, J.-S.; Seo, Y. Breakfast Habits, Sedentary Behavior, and Suicide among Korean Adolescents: A Cross-Sectional National Study. PLoS ONE 2023, 18, e0285312. [Google Scholar] [CrossRef]
- Park, H.; Lee, K. Association Between Breakfast Consumption and Suicidal Attempts in Adolescents. Psychol. Res. Behav. Manag. 2022, 15, 2529–2541. [Google Scholar] [CrossRef]
- Cho, J.A.; Kim, S.; Shin, H.; Kim, H.; Park, E.-C. The Association between High-Caffeine Drink Consumption and Anxiety in Korean Adolescents. Nutrients 2024, 16, 794. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guzmán, V.; Lissner, L.; Arvidsson, L.; Hebestreit, A.; Solea, A.; Lauria, F.; Kaprio, J.; Reisch, L.A.; Moreno, L.; Felső, R.; et al. Associations of Sleep Duration and Screen Time with Incidence of Overweight in European Children: The IDEFICS/I.Family Cohort. Obes. Facts 2022, 15, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.M.S.; Mendes, C.G.; Sen Bressani, G.Y.; De Alcantara Ventura, S.; De Almeida Nogueira, Y.J.; De Miranda, D.M.; Romano-Silva, M.A. The Associations between Screen Time and Mental Health in Adolescents: A Systematic Review. BMC Psychol. 2023, 11, 127. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.; Brown, J.; McQuire, C.; de Vocht, F.; Beard, E.; West, R.; Shahab, L. Association between Cigarette Smoking Status and Voting Intentions: Cross Sectional Surveys in England 2015–2020. BMC Public Health 2021, 21, 2254. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, J.; Kim, J.S. Current Status of Korean Alcohol Drinking in Accordance with the Korean Alcohol Guidelines for Moderate Drinking Based on Facial Flushing. Korean J. Fam. Med. 2023, 44, 129–142. [Google Scholar] [CrossRef]
- Sarkkola, C.; Viljakainen, J.; Saari, A.; Lommi, S.; Engberg, E.; Viljakainen, H. Prevalence of Thinness, Overweight, Obesity, and Central Obesity in Finnish School-Aged Children: A Comparison of National and International Reference Values. Obes. Facts 2022, 15, 240–247. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended International (IOTF) Body Mass Index Cut-offs for Thinness, Overweight and Obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Baiden, P.; Tadeo, S.K.; Tonui, B.C.; Seastrunk, J.D.; Boateng, G.O. Association between Insufficient Sleep and Suicidal Ideation among Adolescents. Psychiatry Res. 2020, 287, 112579. [Google Scholar] [CrossRef]
- Joseph, V.A.; Kreski, N.T.; Keyes, K.M. Sleep Deprivation and Suicide Risk among Minoritized US Adolescents. BMC Psychiatry 2023, 23, 638. [Google Scholar] [CrossRef]
- Chang, C.-S.; Chang, L.-Y.; Wu, C.-C.; Chang, H.-Y. Associations between Social Jetlag Trajectories and Body Mass Index among Young Adults. Sleep 2024, 47, zsad270. [Google Scholar] [CrossRef]
- Kim, B.; Kim, H.-S.; Park, S.; Kwon, J.A. BMI and Perceived Weight on Suicide Attempts in Korean Adolescents: Findings from the Korea Youth Risk Behavior Survey (KYRBS) 2020 to 2021. BMC Public Health 2023, 23, 1107. [Google Scholar] [CrossRef]
- Golubnitschaja, O.; Liskova, A.; Koklesova, L.; Samec, M.; Biringer, K.; Büsselberg, D.; Podbielska, H.; Kunin, A.A.; Evsevyeva, M.E.; Shapira, N.; et al. Caution, “Normal” BMI: Health Risks Associated with Potentially Masked Individual Underweight—EPMA Position Paper 2021. EPMA J. 2021, 12, 243–264. [Google Scholar] [CrossRef] [PubMed]
- Cappelletti, S.; Piacentino, D.; Ciallella, C. A Systematic Review of Caffeine-Related Suicides and an Analysis of the Controversial Role of Caffeine Consumption in Suicidal Risk. Riv. Psichiatr. 2021, 56, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Echeverria, I.; Cotaina, M.; Jovani, A.; Mora, R.; Haro, G.; Benito, A. Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6103. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.; Munafò, M.R.; Davey Smith, G.; Wootton, R.E. Examining the Effect of Smoking on Suicidal Ideation and Attempts: Triangulation of Epidemiological Approaches. Br. J. Psychiatry 2020, 217, 701–707. [Google Scholar] [CrossRef]
- Basiru, T.; Adereti, I.; Umudi, O.; Ezeokoli, A.; Nwoye, I.; Hardy, O.J. Do Cigarette Smoking and Amphetamine Use Predict Suicide Behaviors Among Adolescents in Liberia? Findings from a National Cross-Sectional Survey. Int. J. Ment. Health Addict. 2024, 22, 199–215. [Google Scholar] [CrossRef]
- De Gregorio, D.; Dean Conway, J.; Canul, M.-L.; Posa, L.; Bambico, F.R.; Gobbi, G. Effects of Chronic Exposure to Low-Dose Delta-9-Tetrahydrocannabinol in Adolescence and Adulthood on Serotonin/Norepinephrine Neurotransmission and Emotional Behavior. Int. J. Neuropsychopharmacol. 2020, 23, 751–761. [Google Scholar] [CrossRef]
- Berlin, I.; Hakes, J.K.; Hu, M.-C.; Covey, L.S. Tobacco Use and Suicide Attempt: Longitudinal Analysis with Retrospective Reports. PLoS ONE 2015, 10, e0122607. [Google Scholar] [CrossRef]
- Sharma, V.K.; Sharma, A.; Verma, K.K.; Gaur, P.K.; Kaushik, R.; Abdali, B. A comprehensive review on pharmacological potentials of caffeine. J. Appl. Pharm. Sci. Res. 2023, 6, 16–26. [Google Scholar] [CrossRef]
- Soni, S.; Verma, L. Nicotine and Neurotransmitters an Update. Res. J. Pharm. Technol. 2024, 17, 2605–2612. [Google Scholar] [CrossRef]
- Shima, C.; Lee, R.; Coccaro, E.F. Associations of Agression and Use of Caffeine, Alcohol and Nicotine in Healthy and Aggressive Individuals. J. Psychiatr. Res. 2022, 146, 21–27. [Google Scholar] [CrossRef]
- Sevarino, K.A.; Farrell, M. Disorders Due to Substance Use: Stimulants. In Tasman’s Psychiatry; Tasman, A., Riba, M.B., Alarcón, R.D., Alfonso, C.A., Kanba, S., Lecic-Tosevski, D., Ndetei, D.M., Ng, C.H., Schulze, T.G., Eds.; Springer International Publishing: Cham, Swizerland, 2020; pp. 1–90. ISBN 978-3-030-42825-9. [Google Scholar]
- Stefanovics, E.A.; Potenza, M.N.; Pietrzak, R.H. Smoking, Obesity, and Their Co-Occurrence in the U.S. Military Veterans: Results from the National Health and Resilience in Veterans Study. J. Affect. Disord. 2020, 274, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Yunus, F.M.; Standage, C.; Walsh, C.; Lockhart, P.; Thompson, K.; Keough, M.; Krank, M.; Hadwin, A.; Conrod, P.J.; Stewart, S.H. High Peak Drinking Levels Mediate the Relation between Impulsive Personality and Injury Risk in Emerging Adults. Inj. Epidemiol. 2024, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Levola, J.; Sarala, M.; Mustonen, A.; Rose, R.J.; Miettunen, J.; Niemelä, A.-E.; Niemelä, S. Frequent Alcohol Intoxication and High Alcohol Tolerance During Adolescence as Predictors of Mortality: A Birth Cohort Study. J. Adolesc. Health 2020, 67, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Tetteh-Quarshie, S.; Risher, M.-L. Adolescent Brain Maturation and the Neuropathological Effects of Binge Drinking: A Critical Review. Front. Neurosci. 2023, 16, 1040049. [Google Scholar] [CrossRef]
- Alkattan, A.; Alsalameen, E.; Ahmed, A. Central Nervous System Depressant Drugs: Updated Review; Unpublished manuscript; Ministry of Health: Riyadh, Saudi Arabia, 2021; Available online: https://www.preprints.org/frontend/manuscript/7326564312d904f93ec8bca2e14af119/download_pub (accessed on 15 January 2025).
- Yang, W.; Singla, R.; Maheshwari, O.; Fontaine, C.J.; Gil-Mohapel, J. Alcohol Use Disorder: Neurobiology and Therapeutics. Biomedicines 2022, 10, 1192. [Google Scholar] [CrossRef]
- Lovinger, D.M.; Roberto, M. Synaptic Effects Induced by Alcohol. In Current Topics in Behavioral Neurosciences; Springer: Berlin/Heidelberg, Germany, 2023. [Google Scholar]
- Maharjan, S.; Amjad, Z.; Abaza, A.; Vasavada, A.M.; Sadhu, A.; Valencia, C.; Fatima, H.; Nwankwo, I.; Anam, M.; Mohammed, L. Executive Dysfunction in Patients With Alcohol Use Disorder: A Systematic Review. Cureus 2022, 14, e29207. [Google Scholar] [CrossRef]
- Skrzynski, C.J.; Chen, M.Y.; Bryan, A.D. More Frequent Solitary Alcohol Consumption Is Associated With Poorer Diet Quality, Worse Sleep, Higher Body Mass Index, and More Problematic Alcohol Use. Ann. Behav. Med. 2024, 58, 763–767. [Google Scholar] [CrossRef]
- Agarwal, K.; Demiral, S.B.; Manza, P.; Volkow, N.D.; Joseph, P.V. Relationship between BMI and Alcohol Consumption Levels in Decision Making. Int. J. Obes. 2021, 45, 2455–2463. [Google Scholar] [CrossRef]
- Girela-Serrano, B.M.; Guerrero-Jiménez, M.; Spiers, A.D.V.; Gutiérrez-Rojas, L. Obesity and Overweight among Children and Adolescents with Bipolar Disorder from the General Population: A Review of the Scientific Literature and a Meta-Analysis. Early Interv. Psychiatry 2022, 16, 113–125. [Google Scholar] [CrossRef]
- Patte, K.A.; Livermore, M.; Qian, W.; Leatherdale, S.T. Do Weight Perception and Bullying Victimization Account for Links between Weight Status and Mental Health among Adolescents? BMC Public Health 2021, 21, 1062. [Google Scholar] [CrossRef]
- Thörel, N.; Thörel, E.; Tuschen-Caffier, B. Differential Stigmatization in the Context of Eating Disorders: Less Blame Might Come at the Price of Greater Social Rejection. Stigma Health 2021, 6, 100–112. [Google Scholar] [CrossRef]
- Wang, H.; Xu, S.; Aku, Y.; Ren, Z.; Chen, R. Physical Activity, Psychopathologies, and Self-Injurious Behaviors in Youths: Which Type and How Much Is Sufficient? Unpublished Manuscript; Tsinghua University: Beijing, China, 2024; Available online: https://www.researchsquare.com/article/rs-4127644/v1 (accessed on 12 January 2025).
- Grasdalsmoen, M.; Clarsen, B.; Sivertsen, B. Mental Health in Elite Student Athletes: Exploring the Link Between Training Volume and Mental Health Problems in Norwegian College and University Students. Front. Sports Act. Living 2022, 4, 817757. [Google Scholar] [CrossRef] [PubMed]
- Stults-Kolehmainen, M.A.; Gilson, T.A.; SantaBarbara, N.; McKee, P.C.; Sinha, R.; Bartholomew, J.B.; Boullosa, D.; Budnick, C.J.; Bueno, F.A.; Haughton, A.; et al. Qualitative and Quantitative Evidence of Motivation States for Physical Activity, Exercise and Being Sedentary from University Student Focus Groups. Front. Sports Act. Living 2023, 5, 1033619. [Google Scholar] [CrossRef] [PubMed]
- Haddock, A.; Ward, N.; Yu, R.; O’Dea, N. Positive Effects of Digital Technology Use by Adolescents: A Scoping Review of the Literature. Int. J. Environ. Res. Public. Health 2022, 19, 14009. [Google Scholar] [CrossRef]
| Variables | Categories | Total (%) |
|---|---|---|
| Gender | Male | 19,946 (51.9) |
| Female | 18,466 (48.1) | |
| Grade | Middle School | 21,442 (55.8) |
| High School | 16,970 (44.2) | |
| Economic | Low Level | 3978 (10.4) |
| Middle Level | 17,806 (46.4) | |
| High Level | 16,628 (43.3) | |
| Subjective health assessment | Low Level | 13,014 (33.9) |
| High Level | 25,398 (66.1) | |
| Achievement | Low Level | 11,210 (29.2) |
| Middle Level | 11,584 (30.2) | |
| High Level | 15,618 (40.7) | |
| Violent victimization | No | 37,651 (98) |
| Yes | 761 (2) | |
| Healthy diet | ||
| Breakfast | Unhealthy | 27,706 (72.1) |
| Healthy | 10,706 (27.9) | |
| Coffee | Frequent | 7998 (20.8) |
| Infrequent | 30,414 (79.2) | |
| Physical activity | Inadequate | 5455 (14.2) |
| Adequate | 32,957 (85.8) | |
| Sedentary time | Low Level | 524 (1.4) |
| Middle Level | 1765 (4.6) | |
| High Level | 36,123 (94) | |
| Sleep | <5 h | 3115 (8.1) |
| 5–7 h | 18,381 (47.9) | |
| 7–9 h | 14,334 (37.3) | |
| ≥9 h | 2582 (6.7) | |
| Health risk behaviors | ||
| Cigarettes | No | 34,801 (90.6) |
| Yes | 3111 (9.4) | |
| Hazardous drinking | Yes | 1942 (5.1) |
| No | 2836 (7.4) | |
| Suicidal ideation | No | 33,296 (86.7) |
| Yes | 5116 (13.3) | |
| Suicide planning | No | 36,867 (96) |
| Yes | 1545 (4) | |
| Suicide attempt | No | 37,549 (97.8) |
| Yes | 863 (2.2) | |
| Body Mass Index | Underweight | 9029 (23.5) |
| Normal weight | 18,283 (47.5) | |
| Overweight | 7729 (20.2) | |
| Obesity | 3371 (8.8) |
| Suicidal Ideation | Suicide Planning | Suicide Attempt | ||||
|---|---|---|---|---|---|---|
| Crude | Adjusted a | Crude | Adjusted a | Crude | Adjusted a | |
| Odds Ratio (95% Confidence Intervals) | ||||||
| Healthy diet | ||||||
| Breakfast | ||||||
| Unhealthy | 1.323 (1.088–1.610) ** | 1.067 (0.868–1.312) | 1.060 (0.789–1.424) | 0.889 (0.654–1.209) | 1.249 (0.853–1.828) | 0.964 (0.647–1.436) |
| Healthy | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Coffee | ||||||
| Frequent | 1.381 (1.191–1.602) *** | 1.347 (1.153–1.573) *** | 1.563 (1.247–1.960) *** | 1.492 (1.183–1.882) ** | 1.733 (1.316–2.283) *** | 1.706 (1.282–2.271) *** |
| Infrequent | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Physical Activity | ||||||
| Inadequate | 1.012 (0.802–1.277) | 1.032 (0.809–1.316) | 0.685 (0.450–1.044) | 0.714 (0.465–1.096) | 0.700 (0.416–1.179) | 0.737 (0.432–1.257) |
| Adequate | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sedentary Time | ||||||
| Low Level | 1.048 (0.638–1.720) | 1.045 (0.613–1.779) | 1.100 (0.525–2.305) | 1.002 (0.457–2.194) | 1.012 (0.403–2.540) | 0.875 (0.317–2.415) |
| Middle Level | 0.822 (0.575–1.175) | 0.858 (0.592–1.245) | 1.175 (0.720–1.917) | 1.206 (0.728–1.997) | 1.306 (0.741–2.302) | 1.473 (0.815–2.662) |
| High Level | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sleep | ||||||
| <5 h | 1.736 (1.163–2.592) ** | 2.129 (1.391–3.259) ** | 1.890 (0.967–3.694) | 2.305 (1.152–4.611) ** | 2.000 (0.878–4.556) * | 2.415 (1.025–5.690) * |
| 5–7 h | 0.876 (0.607–1.264) | 1.202 (0.816–1.772) | 1.106 (0.589–2.079) | 1.569 (0.819–3.005) | 1.008 (0.461–2.208) | 1.527 (0.678–3.437) |
| 7–9 h | 0.784 (0.535–1.148) | 1.002 (0.671–1.494) | 1.022 (0.532–1.963) | 1.334 (0.684–2.604) | 1.148 (0.513–2.565) | 1.619 (0.706–3.711) |
| ≥9 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Health Risk Behaviors | ||||||
| Cigarettes | ||||||
| No | 0.737 (0.631–0.861) *** | 0.672 (0.567–0.796) *** | 0.712 (0.561–0.904) ** | 0.722 (0.559–0.932) ** | 0.583 (0.436–0.780) *** | 0.552 (0.402–0.757) *** |
| Yes | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Hazardous Drinking | ||||||
| Yes | 0.973 (0.833–1.137) | 0.975 (0.825–1.152) | 1.290 (1.017–1.637) * | 1.300 (1.010–1.673) * | 1.269 (0.948–1.699) | 1.171 (0.857–1.600) |
| No | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| R2 | 0.231 | 0.453 | 0.058 | 0.125 | 0.034 | 0.116 |
| Suicidal Ideation | Suicide Planning | Suicide Attempt | ||||
|---|---|---|---|---|---|---|
| Crude | Adjusted a | Crude | Adjusted a | Crude | Adjusted a | |
| Odds Ratio (95% Confidence Intervals) | ||||||
| Healthy Diet | ||||||
| Breakfast | ||||||
| Unhealthy | 1.488 (0.934–2.372) | 1.383 (0.848–2.255) | 1.000 (0.499–2.005) | 1.000 (0.499–2.005) | 1.107 (0.473–2.588) | 0.992 (0.403–2.441) |
| Healthy | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Coffee | ||||||
| Frequent | 1.499 (1.065–2.109) * | 1.419 (0.987–2.040) | 1.695 (1.003–2.867) * | 1.695 (1.003–2.867) * | 2.167 (1.180–3.982) * | 2.216 (1.153–4.258) * |
| Infrequent | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Physical Activity | ||||||
| Inadequate | 0.750 (0.435–1.292) | 0.785 (0.445–1.384) | 0.367 (0.110–1.220) | 0.367 (0.110–1.220) | 0.596 (0.177–2.010) | 0.609 (0.165–2.243) |
| Adequate | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sedentary Time | ||||||
| Low Level | 1.296 (0.308–5.453) | 1.000 (0.228–4.393) | 1.415 (0.163–12.291) | 1.415 (0.163–12.291) | 1.873 (0.212–16.550) | 1.820 (0.156–21.215) |
| Middle Level | 0.896 (0.410–1.959) | 0.996 (0.441–2.246) | 0.916 (0.261–3.213) | 0.916 (0.261–3.213) | 0.954 (0.214–4.250) | 1.134 (0.241–5.346) |
| High Level | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sleep | ||||||
| <5 h | 2.391 (1.035–5.525) * | 3.416 (1.403–8.317) ** | 2.179 (0.534–8.890) | 2.179 (0.534–8.890) | 2.825 (0.582–13.711) | 3.093 (0.590–16.215) |
| 5–7 h | 1.193 (0.565–2.517) | 1.718 (0.783–3.772) | 1.786 (0.503–6.344) | 1.786 (0.503–6.344) | 1.008 (0.222–4.574) | 1.268 (0.270–5.953) |
| 7–9 h | 0.900 (0.413–1.961) | 1.215 (0.539–2.738) | 1.250 (0.334–4.683) | 1.250 (0.334–4.683) | 0.878 (0.182–4.234) | 1.113 (0.222–5.566) |
| ≥9 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Health Risk Behaviors | ||||||
| Cigarettes | ||||||
| No | 0.699 (0.488–1.003) | 0.771 (0.522–1.136) | 0.982 (0.542–1.781) | 0.982 (0.542–1.781) | 0.451 (0.236–0.864) * | 0.490 (0.237–1.014) |
| Yes | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Hazardous Drinking | ||||||
| Yes | 0.843 (0.586–1.214) | 0.841 (0.569–1.243) | 0.836 (0.461–1.518) | 0.836 (0.461–1.518) | 0.760 (0.387–1.493) | 0.657 (0.308–1.401) |
| No | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| R2 | 0.257 | 0.296 | 0.076 | 0.160 | 0.067 | 0.201 |
| Suicidal Ideation | Suicide Planning | Suicide Attempt | ||||
|---|---|---|---|---|---|---|
| Crude | Adjusted a | Crude | Adjusted a | Crude | Adjusted a | |
| Odds Ratio (95% Confidence Intervals) | ||||||
| Healthy Diet | ||||||
| Breakfast | ||||||
| Unhealthy | 0.989 (0.670–1.459) | 0.768 (0.508–1.164) | 0.693 (0.393–1.222) | 0.534 (0.290–0.983) | 0.451 (0.226–0.901) | 0.307 (0.140–0.672) |
| Healthy | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Coffee | ||||||
| Frequent | 1.198 (0.871–1.646) | 1.259 (0.900–1.759) | 1.850 (1.133–3.020) * | 1.939 (1.163–3.233) * | 1.958 (1.024–3.742) * | 2.406 (1.211–4.783) ** |
| Infrequent | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Physical Activity | ||||||
| Inadequate | 1.440 (0.903–2.298) | 1.391 (0.845–2.290) | 1.007 (0.444–2.286) | 0.925 (0.385–2.220) | 0.506 (0.119–2.157) | 0.550 (0.124–2.447) |
| Adequate | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sedentary Time | ||||||
| Low Level | 1.234 (0.478–3.185) | 1.113 (0.373–3.319) | 1.787 (0.506–6.309) | 1.434 (0.325–6.324) | ------------------- | ------------------ |
| Middle Level | 0.919 (0.437–1.931) | 0.899 (0.417–1.940) | 2.201 (0.933–5.195) | 2.431 (0.982–6.019) | 2.317 (0.846–6.348) | 2.802 (0.958–8.196) |
| High Level | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sleep | ||||||
| <5 h | 2.397 (0.921–6.241) | 2.593 (0.937–7.172) | 4.487 (0.564–35.716) | 5.655 (0.649–49.248) | 0.282 (0.076–1.042) | 0.216 (0.040–1.162) |
| 5–7 h | 01.252 (0.513–3.055) | 1.822 (0.711–4.672) | 2.194 (0.290–16.585) | 4.129 (0.500–34.065) | 0.282 (0.076–1.042) | 0.355 (0.088–1.430) |
| 7–9 h | 1.121 (0.446–2.821) | 1.479 (0.561–3.902) | 2.853 (0.369–22.048) | 5.242 (0.618–44.432) | 0.595 (0.159–2.222) | 0.694 (0.171–2.820) |
| ≥9 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Health Risk Behaviors | ||||||
| Cigarettes | ||||||
| No | 0.706 (0.507–0.983) * | 0.566 (0.393–0.815) ** | 0.644 (0.384–1.079) | 0.528 (0.299–0.930) * | 0.840 (0.427–1.651) | 0.522 (0.239–1.138) |
| Yes | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Hazardous Drinking | ||||||
| Yes | 1.076 (0.772–1.500) | 1.045 (0.731–1.495) | 1.215 (0.721–2.047) | 1.138 (0.645–2.007) | 2.277 (1.132–4.580) * | 2.098 (0.974–4.518) |
| No | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| R2 | 0.183 | 0.638 | 0.030 | 0.093 | 0.098 | 1.156 |
| Suicidal Ideation | Suicide Planning | Suicide Attempt | ||||
|---|---|---|---|---|---|---|
| Crude | Adjusted a | Crude | Adjusted a | Crude | Adjusted a | |
| Odds Ratio (95% Confidence Intervals) | ||||||
| Healthy Diet | ||||||
| Breakfast | ||||||
| Unhealthy | 1.507 (0.793–2.864) | 1.254 (0.633–2.487) | 2.265 (0.783–6.551) | 1.843 (0.607–5.598) | 0.675 (0.273–1.670) | 0.477 (0.175–1.302) |
| Healthy | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Coffee | ||||||
| Frequent | 1.337 (0.827–2.161) | 1.348 (0.803–2.261) | 0.998 (0.502–1.983) | 0.898 (0.426–1.892) | 2.094 (0.948–4.629) | 2.492 (1.048–5.925) * |
| Infrequent | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Physical Activity | ||||||
| Inadequate | 1.348 (0.639–2.843) | 1.485 (0.655–3.367) | 0.783 (0.230–2.664) | 0.910 (0.245–3.377) | 0.361 (0.047–2.749) | 0.362 (0.042–3.119) |
| Adequate | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sedentary Time | ||||||
| Low Level | 1.620 (0.551–4.762) | 1.946 (0.614–6.166) | 1.193 (0.256–5.556) | 1.303 (0.236–7.182) | 2.874 (0.734–11.256) | 3.847 (0.831–17.813) |
| Middle Level | 0.510 (0.114–2.284) | 0.422 (0.089–2.006) | 1.108 (0.239–5.132) | 1.222 (0.246–6.073) | 0.855 (0.104–7.033) | 0.581 (0.059–5.765) |
| High Level | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Sleep | ||||||
| <5 h | 2.446 (0.482–12.413) | 3.242 (0.550–19.098) | ------------------ | ------------------ | ------------------ | ------------------ |
| 5–7 h | 1.256 (0.274–5.753) | 1.825 (0.347–9.613) | ------------------ | ------------------ | ------------------ | ------------------ |
| 7–9 h | 1.574 (0.333–7.445) | 1.912 (0.352–10.385) | ------------------ | ------------------ | ------------------ | ------------------ |
| ≥9 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Health Risk Behaviors | ||||||
| Cigarettes | ||||||
| No | 0.655 (0.400–1.071) | 0.514 (0.297–0.887) * | 0.893 (0.448–1.782) | 0.728 (0.337–1.573) | 0.797 (0.354–1.793) | 0.764 (0.302–1.932) |
| Yes | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| Hazardous Drinking | ||||||
| Yes | 0.762 (0.459–1.2660) | 0.731 (0.412–1.295) | 1.385 (0.687–2.793) | 1.102 (0.505–2.406) | 1.694 (0.730–3.929) | 1.686 (0.646–4.400) |
| No | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| R2 | 0.113 | 0.142 | 0.000 | 0.000 | 0.000 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Kim, K.-O. Associations of Body Mass Index and Lifestyle Factors with Suicidal Ideation, Planning, and Attempts Among Korean Adolescents: A Cross-Sectional Study. Healthcare 2025, 13, 1470. https://doi.org/10.3390/healthcare13121470
Wang H, Kim K-O. Associations of Body Mass Index and Lifestyle Factors with Suicidal Ideation, Planning, and Attempts Among Korean Adolescents: A Cross-Sectional Study. Healthcare. 2025; 13(12):1470. https://doi.org/10.3390/healthcare13121470
Chicago/Turabian StyleWang, Haitao, and Kyung-O Kim. 2025. "Associations of Body Mass Index and Lifestyle Factors with Suicidal Ideation, Planning, and Attempts Among Korean Adolescents: A Cross-Sectional Study" Healthcare 13, no. 12: 1470. https://doi.org/10.3390/healthcare13121470
APA StyleWang, H., & Kim, K.-O. (2025). Associations of Body Mass Index and Lifestyle Factors with Suicidal Ideation, Planning, and Attempts Among Korean Adolescents: A Cross-Sectional Study. Healthcare, 13(12), 1470. https://doi.org/10.3390/healthcare13121470







