Effect of Postural Stabilization Exercises in Combination with Cervical Stabilization Exercises on Craniovertebral Angle, Pain, Disability, and Quality of Life in Patients with Chronic Neck Pain: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
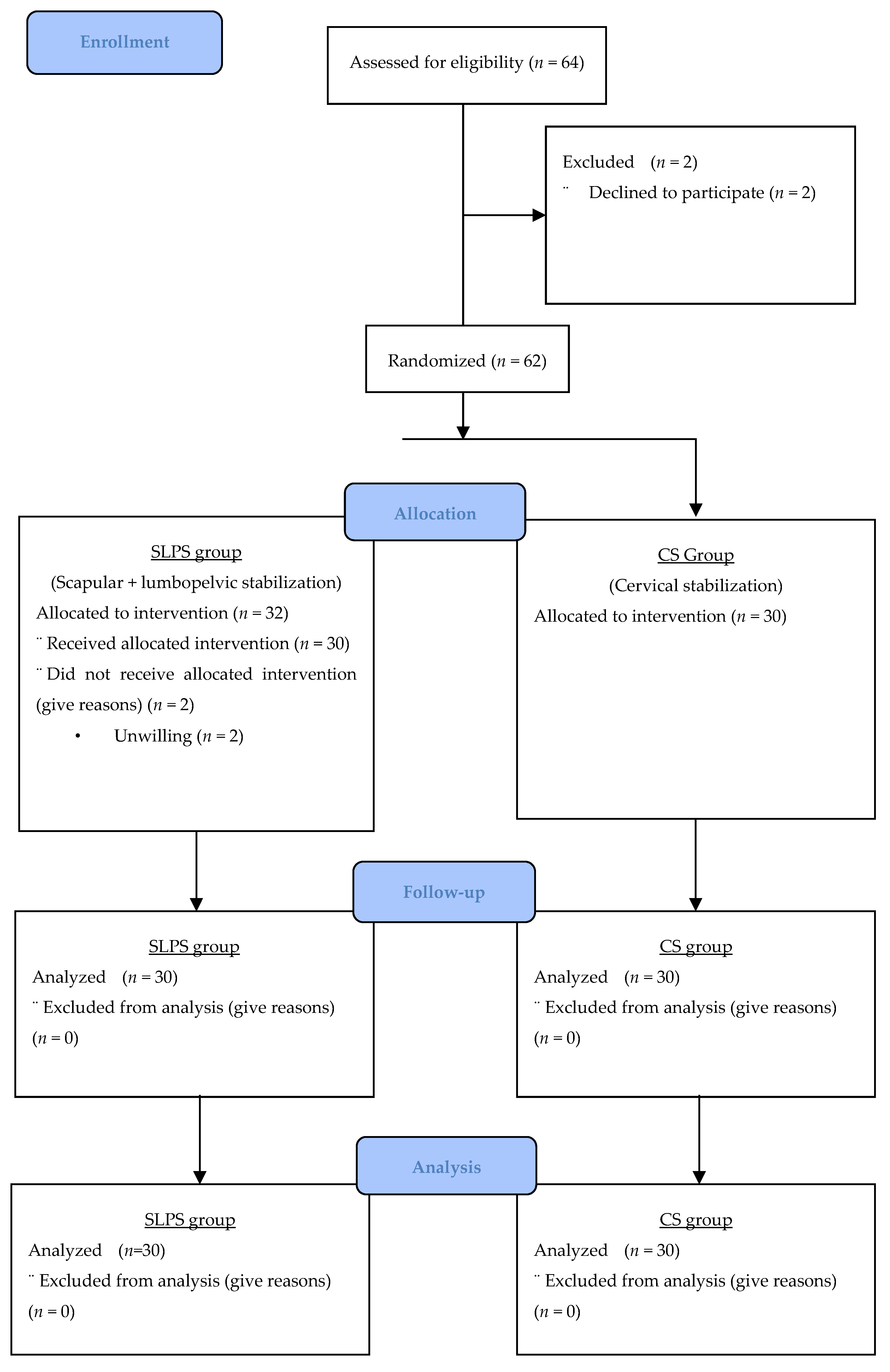
2.1. Study Design
2.2. Participants
Inclusion and Exclusion Criteria
2.3. Randomization
2.4. Interventions
2.4.1. Cervical Stabilization Exercises
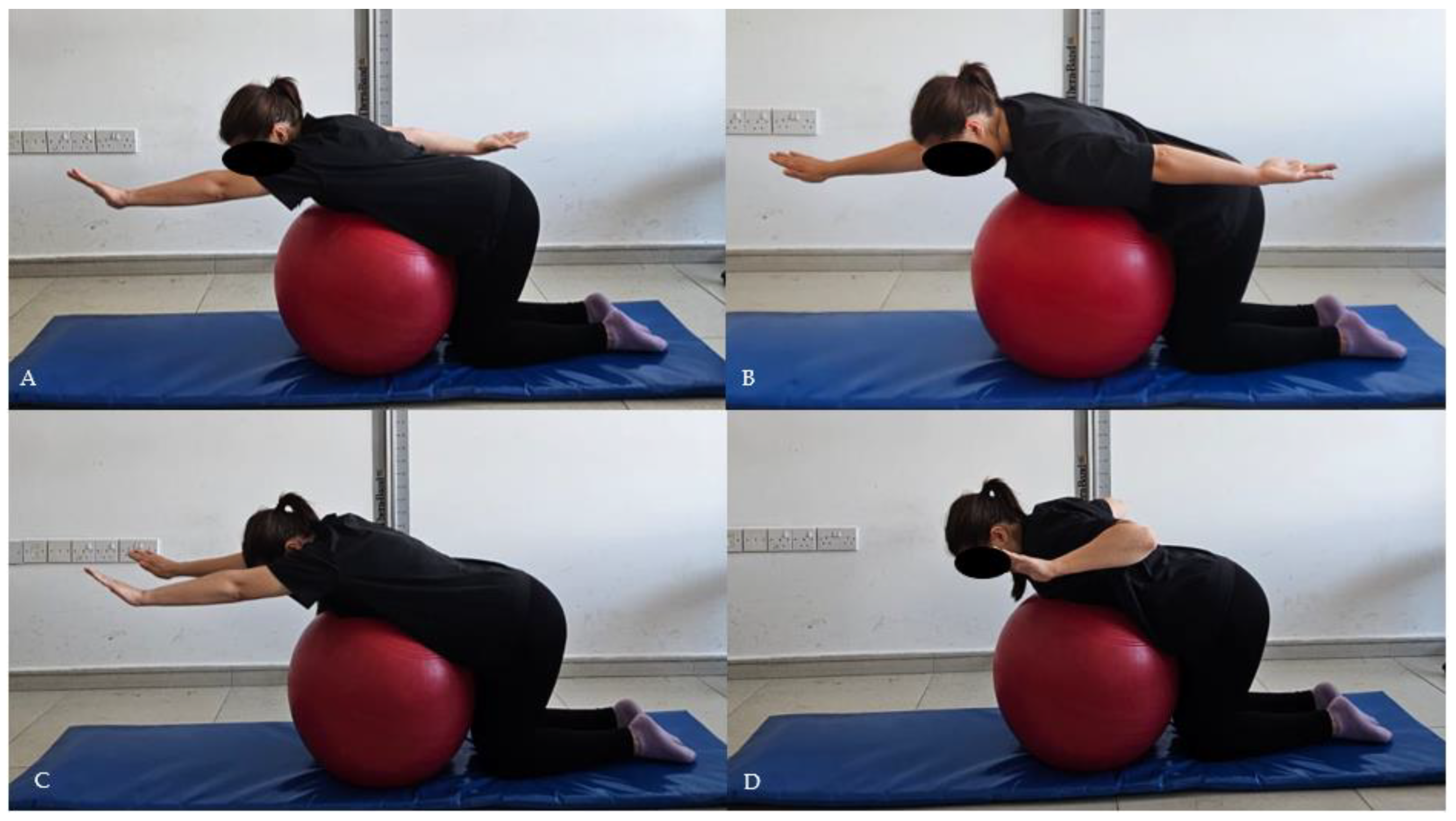
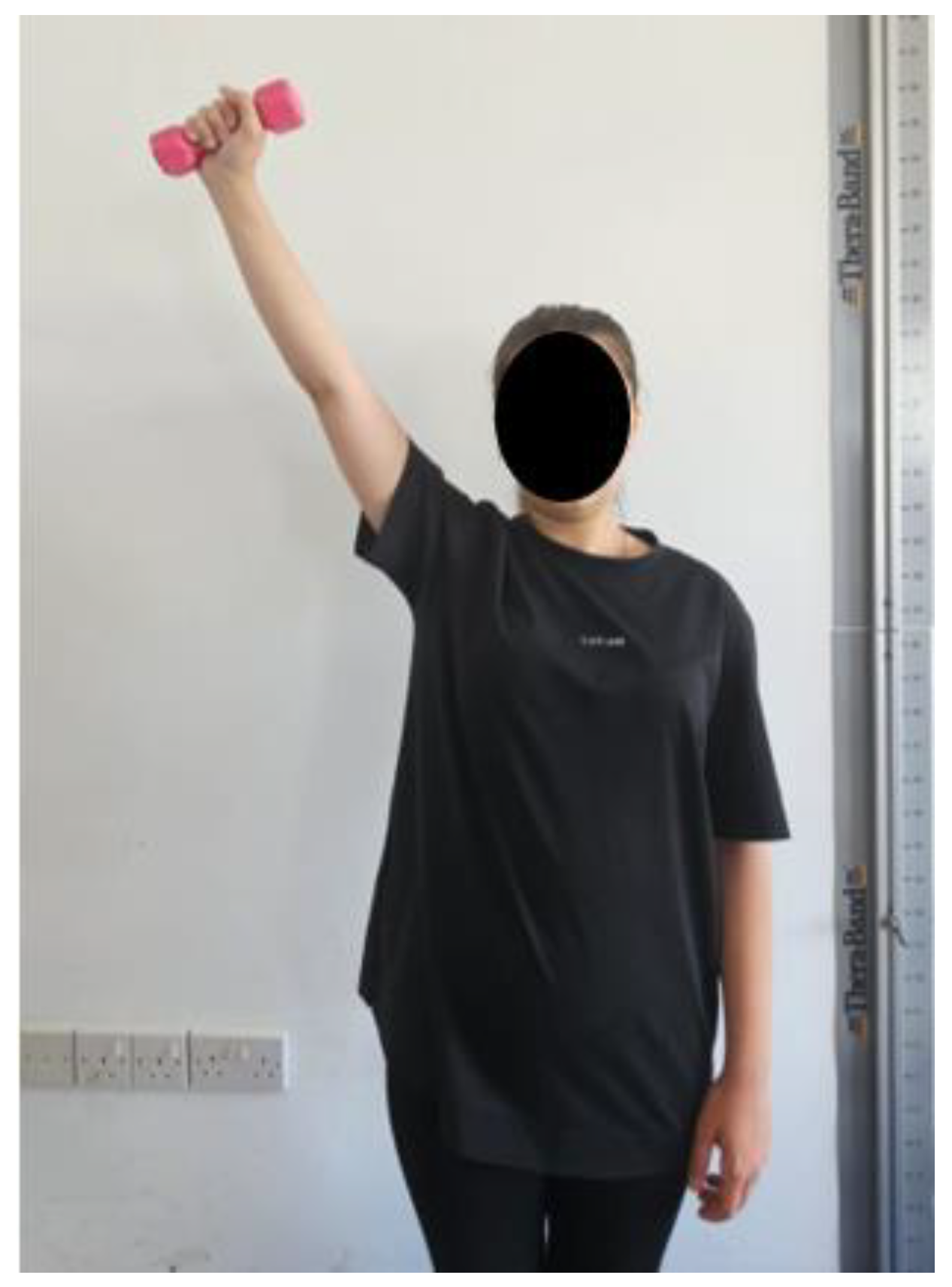
2.4.2. Scapular Stabilization Exercises
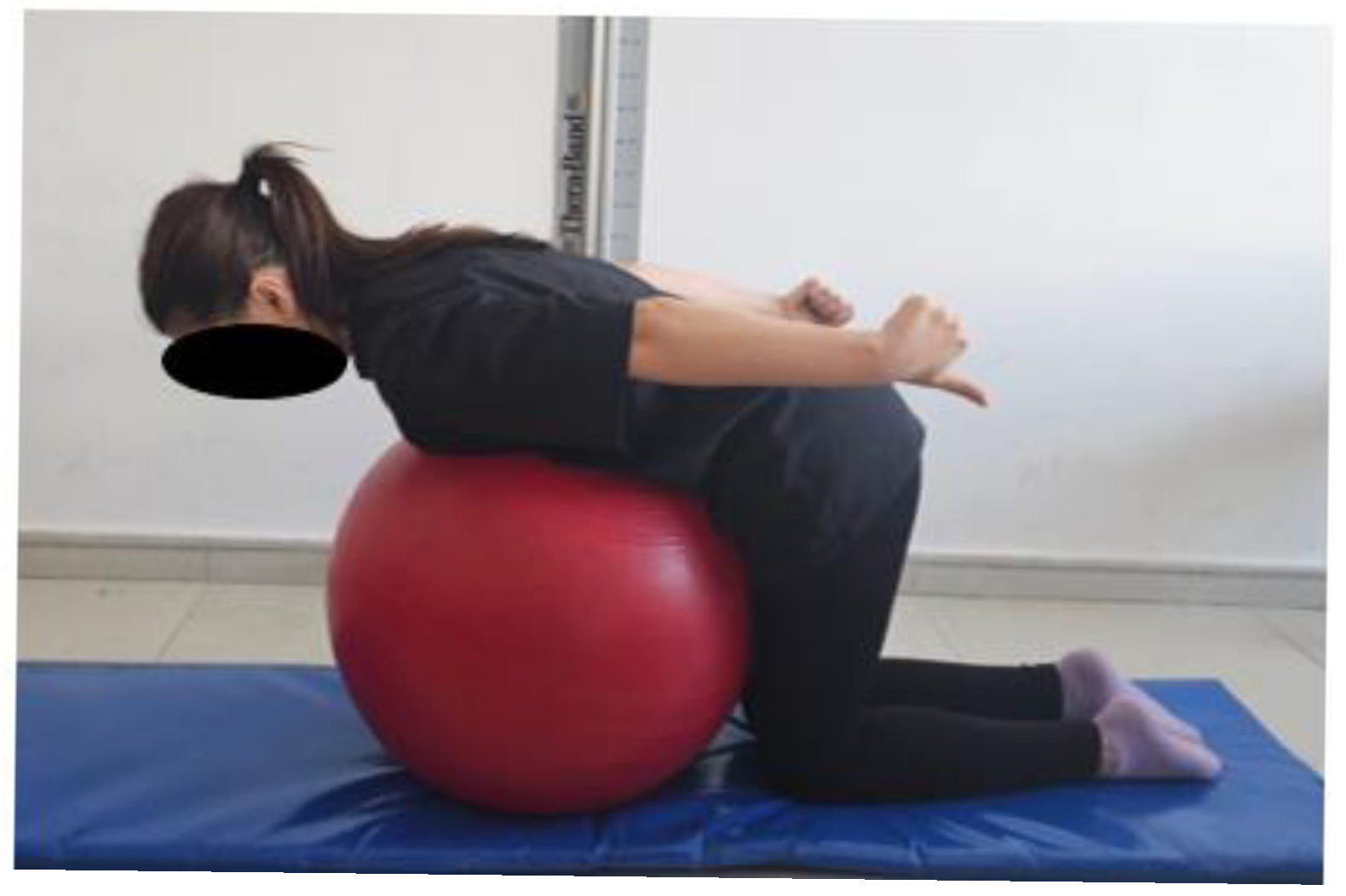
2.4.3. Postural Stabilization Exercises
2.5. Outcome Measures
2.5.1. Craniovertebral Angle Measurement
2.5.2. Pain Assessment
2.5.3. Neck Disability Index
2.5.4. Health-Related Quality of Life
2.6. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CS | Cervical stabilization group |
| CVA | Craniovertebral angle |
| EMG | Electromyography |
| NDI | Neck disability index |
| SF-36 | Short-Form Health Survey |
| SLPS | Scapular and lumbopelvic stabilization |
| VAS | Visual analog scale |
References
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.; Kolahi, A.-A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef] [PubMed]
- Fapojuwo, O.; Akodu, A.; Nwanne, C. Efficacy of neck stabilization and Pilates exercises on pain, sleep disturbance and kinesiophobia in patients with non-specific chronic neck pain: A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 26, 411–419. [Google Scholar] [CrossRef]
- Rosene, J.M.; Langford, D.; Gallo, C.A.; Desrochers, G.N.; Morris, G.J.; Rumney, C.D.; Sandell, S.J.; McDevitt, J.K. Sex differences in neck strength force and activation patterns in collegiate contact sport. J. Sports Sci. Med. 2022, 21, 68–73. [Google Scholar] [CrossRef]
- Barati, A.H.; Mozafaripour, E.; Javdaneh, N.; Ambroży, T.; Rydzik, Ł. Focus on the scapular region in the rehabilitation of chronic neck pain is effective in improving the symptoms: A randomized controlled trial. J. Clin. Med. 2021, 10, 3495. [Google Scholar] [CrossRef]
- Barati, A.H.; Shams, A.; Javdaneh, N.; Saeterbakken, A.H. Pain neuroscience education combined with therapeutic exercises provides added benefit in the treatment of chronic neck pain. Int. J. Environ. Res. Public Health 2021, 18, 8848. [Google Scholar] [CrossRef]
- Hirata, R.; Christensen, S.; Graven-Nielsen, T. Altered pain sensitivity and axioscapular muscle activity in neck pain patients compared with healthy controls. Eur. J. Pain 2017, 21, 1763–1771. [Google Scholar] [CrossRef]
- Cools, A.; Yildiz, T.I.; Duzgun, I. Alterations in the 3-dimensional scapular orientation in patients with non-specific neck pain. Clin. Biomech. 2019, 70, 97–106. [Google Scholar] [CrossRef]
- Kaya, B.K.; Gumuscu, B.H.; Kisa, E.P.; Muammer, R. Comparison of three different exercise trainings in patients with chronic neck pain: A randomized controlled study. Korean J. Pain 2023, 36, 242–252. [Google Scholar] [CrossRef]
- Cholewicki, J.; Stuart, M.; McGill, S. Mechanical stability of the in vivo lumbar spine: Implications for injury and chronic low back pain. Clin. Biomech. 1996, 11, 1–15. [Google Scholar] [CrossRef]
- Durall, C.J. Therapeutic exercise for athletes with nonspecific neck pain: A current concepts review. Sports Health 2012, 4, 293–301. [Google Scholar] [CrossRef]
- Patroncini, M. Impaired Trunk Muscle Function in Sub-acute Neck Pain: Etiologic in the Subsequent Development of Low Back Pain? Manuelletherapie 2005, 9, 187–188. [Google Scholar] [CrossRef]
- Thongprasert, C.; Kanlayanaphotporn, R. Abnormal performance of cervical stabilizer muscles in individuals with low back pain. J. Man. Manip. Ther. 2019, 27, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Park, W.H.; Seo, Y.G.; Kang, K.C.; Lee, S.M.; Bin Min, K.; Yoo, J.C. Is scapular stabilization exercise effective for managing nonspecific chronic neck pain?: A systematic review. Asian Spine J. 2020, 14, 122–129. [Google Scholar] [CrossRef]
- Duzgun, I.; Turgut, E.; Yildiz, T.I. Neck and scapula-focused exercise training on patients with nonspecific neck pain: A randomized controlled trial. J. Sport Rehabil. 2018, 27, 403–412. [Google Scholar] [CrossRef]
- Azadi, F.; Marioryad, H.; Amjad, R.N.; Alimohammadi, M.; Vazifehkhorani, A.K.; Poursadeghiyan, M. Effect of 12-week neck, core, and combined stabilization exercises on the pain and disability of elderly patients with chronic non-specific neck pain: A Clinical Trial. Iran. J. Ageing 2019, 13, 614–625. [Google Scholar] [CrossRef]
- Lee, K.-S. Effect of a Five-week scapular correction exercise in patients with chronic mechanical neck pain. J. Korean Phys. Ther. 2020, 32, 126–131. [Google Scholar] [CrossRef]
- Golub, R.M.; Thabane, L.; Boutron, I.; Schriger, D.L.; Moher, D.; White, I.R.; Aggarwal, R.; Collins, G.S.; E Lamb, S.; Hopewell, S.; et al. CONSORT 2025 statement: Updated guideline for reporting randomised trials. BMJ 2025, 389, e081123. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Iqbal, Z.A. Effect of deep cervical flexor muscle training using pressure biofeedback on pain and forward head posture in school teachers with neck pain: An observational study. BioMed Res. Int. 2021, 2021, 5588580. [Google Scholar] [CrossRef]
- Rajan, R.; Alghadir, A.H.; Khan, S.A.; Iqbal, Z.A. Effect of deep cervical flexor muscles training using pressure biofeedback on pain and disability of school teachers with neck pain. J. Phys. Ther. Sci. 2013, 25, 657–661. [Google Scholar] [CrossRef]
- Pink, M.; Tibone, J.; Moseley, J.B.; Jobe, F.W.; Perry, J. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am. J. Sports Med. 1992, 20, 128–134. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Donatelli, R.A.; Soderberg, G.L. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J. Orthop. Sports Phys. Ther. 2003, 33, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Kirupa, K.; Mary, S.D.; Nithyanisha, R.; Kumar, S.N. A study on the effectiveness of scapular retraction exercises on forward head posture. Indian J. Public Health Res. Dev. 2020, 11, 284–289. [Google Scholar]
- Hussain, M.E.; Veqar, Z.; Singla, D. Photogrammetric assessment of upper body posture using postural angles: A literature review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Intrarater and interrater reliability of photographic measurement of upper-body standing posture of adolescents. J. Manip. Physiol. Ther. 2015, 38, 74–80. [Google Scholar] [CrossRef]
- Van Niekerk, S.M.; Louw, Q.; Vaughan, C.; Grimmer-Somers, K.; Schreve, K. Photographic measurement of upper-body sitting posture of high school students: A reliability and validity study. BMC Musculoskelet. Disord. 2008, 9, 113. [Google Scholar] [CrossRef]
- Son, S.-M.; Kim, C.-J.; Kim, D.-H. Neck pain in adults with forward head posture: Effects of craniovertebral angle and cervical range of motion. Osong Public Health Res. Perspect. 2018, 9, 309–313. [Google Scholar] [CrossRef]
- Behtash, H.; Parnianpour, M.; Razmjoo, A.; Gohari, M.; Maroufi, N.; Ahmadi, A.; Salahzadeh, Z. Assessment of forward head posture in females: Observational and photogrammetry methods. J. Back Musculoskelet. Rehabil. 2014, 27, 131–139. [Google Scholar] [CrossRef]
- Deklerck, J.; Vanderhaeghen, J.; Dankaerts, W.; Brumagne, S.; Claeys, K. Sagittal evaluation of usual standing and sitting spinal posture. J. Bodyw. Mov. Ther. 2016, 20, 326–333. [Google Scholar] [CrossRef]
- Pareja, J.; Alonso-Blanco, C.; Fernández-De-Las-Peñas, C.; Cuadrado, M. Forward head posture and neck mobility in chronic tension-type headache. Cephalalgia 2006, 26, 314–319. [Google Scholar] [CrossRef]
- Hoving, J.L.; Pool, J.J.M.; de Vet, H.C.W.; Bouter, L.M.; Ostelo, R.W.J.G. Minimal Clinically Important Change of the Neck Disability Index and the Numerical Rating Scale for Patients with Neck Pain. Spine 2007, 32, 3047–3051. [Google Scholar] [CrossRef]
- Vernon, H.; Mior, S. The Neck Disability Index: A study of reliability and validity. J. Manip. Physiol. Ther. 1991, 14, 409–415. [Google Scholar]
- Aslan, E.; Karaduman, A.; Yakut, Y.; Aras, B.; Simsek, I.E.; Yaglý, N. The cultural adaptation, reliability, and validity of neck disability index in patients with neck pain: A Turkish version study. Spine 2009, 34, 1732–1735. [Google Scholar] [CrossRef] [PubMed]
- Kocyigit, H.; Aydemir, O.; Olmez, N.; Memis, A. Reliability and validity of the Turkish version of Short-Form-36 (SF-36). Turk. J. Drugs Therap. 1999, 12, 102–106. [Google Scholar]
- Gardiner, E.; Sharp, D.M.; McLean, S.M.; Klaber-Moffett, J.; May, S. Risk factors for the onset of non-specific neck pain: A systematic review. J. Epidemiol. Community Health 2010, 64, 565–572. [Google Scholar] [CrossRef]
- Guo, W.; Huang, G.; Sun, L.; Wu, H.; Han, F.; Li, Y.; Zou, C. Global burden of neck pain and its gender and regional inequalities from 1990–2021: A comprehensive analysis from the Global Burden of Disease Study 2021. BMC Musculoskelet. Disord. 2025, 26, 94. [Google Scholar] [CrossRef]
- Boucaut, R.; Uthaikhup, S.; Puntumetakul, R.; Suvarnnato, T. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: A randomized controlled trial. J. Pain Res. 2019, ume 12, 915–925. [Google Scholar] [CrossRef]
- Kang, N.-Y.; Kim, K. Effects of a combination of scapular stabilization and thoracic extension exercises on respiration, pain, craniovertebral angle and cervical range of motion in elementary school teachers with a forward head posture: A randomized controlled trial. J. Korean Soc. Phys. Med. 2022, 17, 29–40. [Google Scholar] [CrossRef]
- Kang, J.-I.; Jeong, D.-K.; Moon, Y.-J.; Park, J.-S.; Choi, H.-H. Effect of scapular stabilization exercise on neck alignment and muscle activity in patients with forward head posture. J. Phys. Ther. Sci. 2018, 30, 804–808. [Google Scholar] [CrossRef]
- Kim, B.; Kang, T. Cervical and scapula-focused resistance exercise program versus trapezius massage in patients with chronic neck pain: A randomized controlled trial. Medicine 2022, 101, e30887. [Google Scholar] [CrossRef]
- Hodges, P.W.; Tucker, K. Moving differently in pain: A new theory to explain the adaptation to pain. Pain 2011, 152, S90–S98. [Google Scholar] [CrossRef]
- Park, K.-N.; Kim, S.-H.; Jung, D.-Y. Trapezius and serratus anterior muscle strength in violinists with unilateral neck pain. J. Back Musculoskelet. Rehabil. 2020, 33, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Reinold, M.M.; Escamilla, R. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J. Orthop. Sports Phys. Ther. 2009, 39, 105–117. [Google Scholar] [CrossRef]
- Ganu, S.; Gor, U. Effects of abdominal control feedback and scapular stabilization exercise on chronic neck pain. Int. J. Health Sci. Res. 2021, 11, 318–325. [Google Scholar] [CrossRef]
- Gladin, A.; Khosrokiani, Z.; Letafatkar, A. Lumbar motor control training as a complementary treatment for chronic neck pain: A randomized controlled trial. Clin. Rehabil. 2022, 36, 99–112. [Google Scholar] [CrossRef]
- Chang, M.C.; Yi, Y.G.; Yang, S.; Boudier-Revéret, M.; Hong, K.Y. Treatment of Chronic Neck Pain in Patients with Forward Head Posture: A Systematic Narrative Review. Healthcare 2023, 11, 2604. [Google Scholar] [CrossRef]
- Mufraggi, N.; Royuela, A.; The Spanish Back Pain Research Network; Corcoll, J.; Alegre, L.; Tomás, M.; Cano, A.; Gestoso, M.; Mir, M.A.; Gil del Real, M.T.; et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet. Disord. 2008, 9, 43. [Google Scholar] [CrossRef]

| Variable | SLPS Group (n = 30) X ± SD | CS Group (n = 30) X ± SD | p-Value |
|---|---|---|---|
| Age (year) | 37.50 ± 13.14 | 38.16 ± 14.33 | 0.852 |
| Height (cm) | 163.6 ± 5.88 | 163.0 ± 5.75 | 0.691 |
| Weight (kg) | 67.16 ± 12.10 | 65.40 ± 13.77 | 0.600 |
| BMI (kg/m2) | 24.80 ± 3.70 | 24.70 ± 4.34 | 0.919 |
| Working time (year) | 12.06 ± 11.46 | 13.60 ± 12.09 | 0.616 |
| SLPS Group (n = 30) | CS Group (n = 30) | p2 | ||||
|---|---|---|---|---|---|---|
| ± SD | Median (IQR) | ± SD | Median (IQR) | |||
| VAS | Pre-treatment | 6.43 ± 1.81 | 6.50 (3.00) | 6.13 ± 2.00 | 5.00 (3.00) | 0.906 |
| Post-treatment | 0.93 ± 1.36 | 0.00 (2.00) | 4.60 ± 1.79 | 5.00 (3.00) | <0.001 | |
| Follow-Up | 2.60 ± 1.54 | 3.00 (3.00) | 6.27 ± 1.98 | 7.00 (3.00) | <0.001 | |
| p1 | a, b, c | a, c | ||||
| CVA (°) | Pre-treatment | 50.35 ± 4.76 | 50.33 (7.17) | 51.24 ± 4.47 | 51.89 (6.76) | 0.838 |
| Post-treatment | 58.00 ± 4.41 | 56.91 (7.54) | 53.00 ± 4.48 | 53.47 (5.66) | <0.001 | |
| Follow-Up | 56.50 ± 4.66 | 56.25 (7.65) | 51.59 ± 4.36 | 52.56 (4.97) | <0.001 | |
| p1 | a, b, c | a, c | ||||
| NDI | Pre-treatment | 18.00 ± 7.25 | 19.00 (9.00) | 16.17 ± 8.54 | 14.50 (11.00) | 0.755 |
| Post-treatment | 3.73 ± 2.21 | 3.00 (3.00) | 12.43 ± 7.61 | 11.00 (11.00) | <0.001 | |
| Follow-Up | 6.73 ± 2.83 | 7.00 (4.00) | 15.07 ± 8.23 | 13.00 (11.00) | <0.001 | |
| p1 | a, b, c | a, c | ||||
| SLPS Group (n = 30) | CS Group (n = 30) | p2 | ||||
|---|---|---|---|---|---|---|
| ± SD | Median (IQR) | ± SD | Median (IQR) | |||
| SF-36 Physical functioning | Pre-treatment | 72.33 ± 16.39 | 72.50 (20.00) | 69.17 ± 27.76 | 77.50 (45.00) | 0.933 |
| Post-treatment | 86.67 ± 10.69 | 90.00 (15.00) | 75.17 ± 21.27 | 80.00 (30.00) | 0.034 | |
| Follow-Up | 84.83 ± 12.07 | 87.50 (15.00) | 72.83 ± 23.37 | 80.00 (30.00) | 0.048 | |
| p1 | a, b, c | a | ||||
| SF-36 Role limitations due to physical health | Pre-treatment | 52.50 ± 39.03 | 50.00 (75.00) | 49.17 ± 40.73 | 50.00 (100.00) | 0.984 |
| Post-treatment | 89.17 ± 16.97 | 100.00 (25.00) | 60.00 ± 32.56 | 50.00 (50.00) | <0.001 | |
| Follow-Up | 75.83 ± 22.25 | 75.00 (50.00) | 50.83 ± 31.82 | 50.00 (50.00) | 0.003 | |
| p1 | a, b, c | c | ||||
| SF-36 Role limitations due to emotional problems | Pre-treatment | 51.12 ± 43.54 | 50.10 (100.00) | 47.78 ± 43.49 | 33.30 (100.00) | 0.987 |
| Post-treatment | 88.23 ± 18.16 | 100.00 (33.30) | 54.45 ± 37.64 | 66.70 (66.70) | <0.001 | |
| Follow-Up | 71.14 ± 22.69 | 66.70 (33.30) | 39.60 ± 41.82 | 33.30 (66.70) | 0.002 | |
| p1 | a, b, c | c | ||||
| SF-36 Energy/fatigue | Pre-treatment | 40.00 ± 21.24 | 40.00 (25.00) | 43.67 ± 24.81 | 42.50 (40.00) | 0.903 |
| Post-treatment | 67.00 ± 15.35 | 65.00 (15.00) | 51.00 ± 20.53 | 50.00 (20.00) | 0.004 | |
| Follow-Up | 64.67 ± 14.26 | 62.50 (15.00) | 47.50 ± 21.08 | 50.00 (30.00) | 0.002 | |
| p1 | a, b | a | ||||
| SF-36 Emotional well-being | Pre-treatment | 56.53 ± 16.16 | 54.00 (20.00) | 56.53 ± 24.13 | 60.00 (40.00) | >0.999 |
| Post-treatment | 71.53 ± 16.01 | 72.00 (12.00) | 58.33 ± 21.48 | 58.00 (36.00) | 0.028 | |
| Follow-Up | 66.60 ± 15.14 | 68.00 (12.00) | 56.67 ± 21.64 | 60.00 (24.00) | 0.127 | |
| p1 | a, b, c | - | ||||
| SF-36 Social functioning | Pre-treatment | 72.25 ± 20.09 | 75.00 (37.50) | 66.67 ± 30.68 | 75.00 (37.50) | 0.793 |
| Post-treatment | 90.87 ± 16.69 | 100.00 (12.50) | 70.98 ± 27.50 | 75.00 (50.00) | 0.004 | |
| Follow-Up | 82.27 ± 15.77 | 87.50 (12.50) | 62.25 ± 29.94 | 62.50 (37.50) | 0.007 | |
| p1 | a, c | c | ||||
| SF-36 Pain | Pre-treatment | 51.58 ± 19.49 | 46.25 (25.00) | 56.67 ± 23.06 | 57.50 (32.50) | 0.738 |
| Post-treatment | 87.58 ± 9.88 | 90.00 (20.00) | 61.23 ± 19.45 | 67.50 (30.00) | <0.001 | |
| Follow-Up | 75.42 ± 10.71 | 77.50 (12.50) | 54.17 ± 19.52 | 55.00 (22.50) | <0.001 | |
| p1 | a, b, c | c | ||||
| SF-36 General health | Pre-treatment | 50.17 ± 18.55 | 47.50 (20.00) | 57.17 ± 19.81 | 55.00 (30.00) | 0.414 |
| Post-treatment | 66.17 ± 19.15 | 62.50 (25.00) | 58.00 ± 22.38 | 55.00 (35.00) | 0.352 | |
| Follow-Up | 61.83 ± 16.99 | 60.00 (25.00) | 55.33 ± 20.04 | 50.00 (30.00) | 0.450 | |
| p1 | a, b, c | - | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mehmetoğlu, G.; Yüksel, İ. Effect of Postural Stabilization Exercises in Combination with Cervical Stabilization Exercises on Craniovertebral Angle, Pain, Disability, and Quality of Life in Patients with Chronic Neck Pain: A Randomized Controlled Trial. Healthcare 2025, 13, 1388. https://doi.org/10.3390/healthcare13121388
Mehmetoğlu G, Yüksel İ. Effect of Postural Stabilization Exercises in Combination with Cervical Stabilization Exercises on Craniovertebral Angle, Pain, Disability, and Quality of Life in Patients with Chronic Neck Pain: A Randomized Controlled Trial. Healthcare. 2025; 13(12):1388. https://doi.org/10.3390/healthcare13121388
Chicago/Turabian StyleMehmetoğlu, Gölgem, and İnci Yüksel. 2025. "Effect of Postural Stabilization Exercises in Combination with Cervical Stabilization Exercises on Craniovertebral Angle, Pain, Disability, and Quality of Life in Patients with Chronic Neck Pain: A Randomized Controlled Trial" Healthcare 13, no. 12: 1388. https://doi.org/10.3390/healthcare13121388
APA StyleMehmetoğlu, G., & Yüksel, İ. (2025). Effect of Postural Stabilization Exercises in Combination with Cervical Stabilization Exercises on Craniovertebral Angle, Pain, Disability, and Quality of Life in Patients with Chronic Neck Pain: A Randomized Controlled Trial. Healthcare, 13(12), 1388. https://doi.org/10.3390/healthcare13121388





