Effects of Core Stability Training on Balance, Standing, and Gait in Children with Mild Cerebral Palsy: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Design and Randomization
2.3. Outcome Measures
2.3.1. Pediatric Balance Scale (PBS)
2.3.2. Kinovea Motion Analysis Software
2.3.3. Gross Motor Function Measure (GMFM)
2.4. Treatment Procedures
2.5. Statistical Analysis
3. Results
3.1. General Characteristics
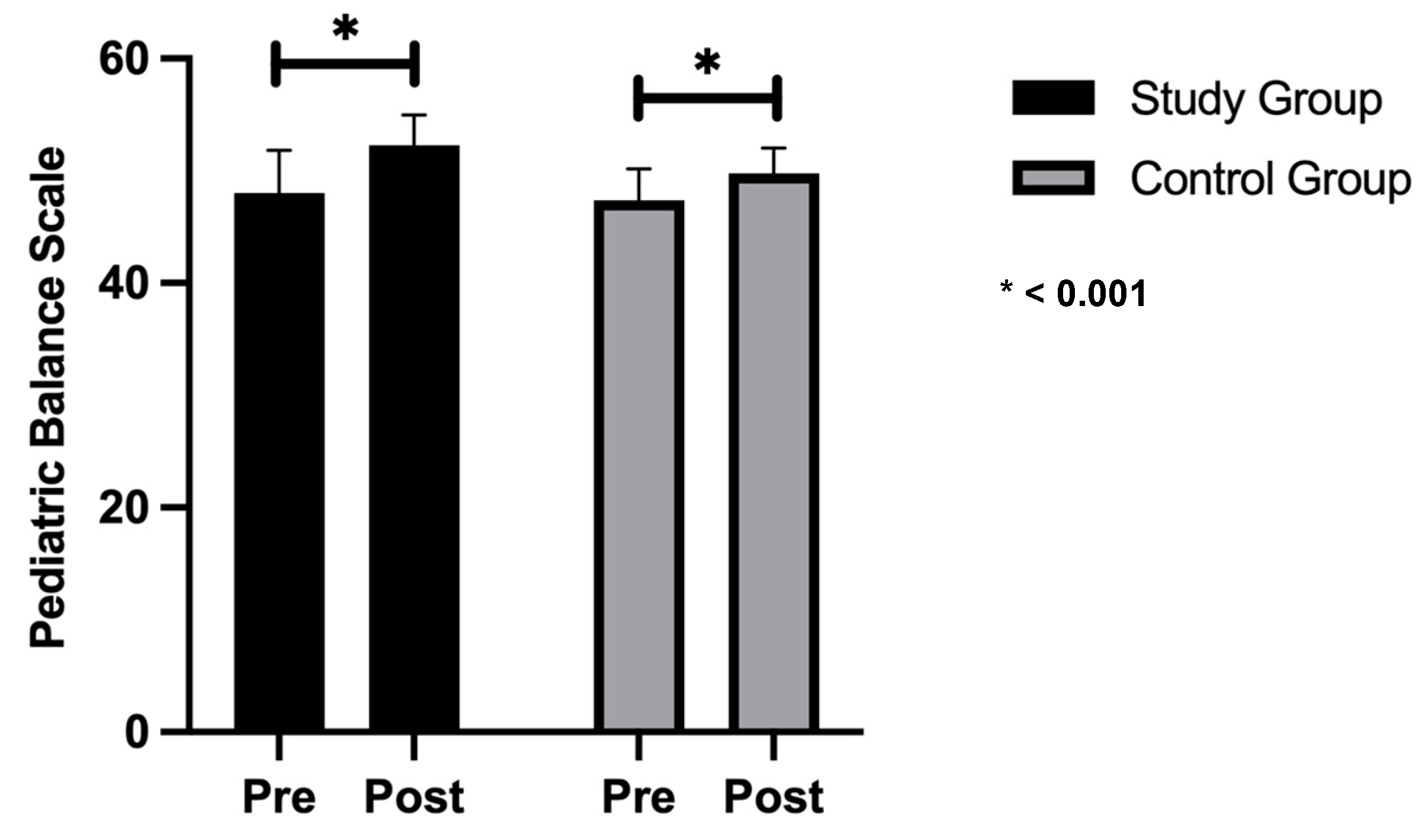
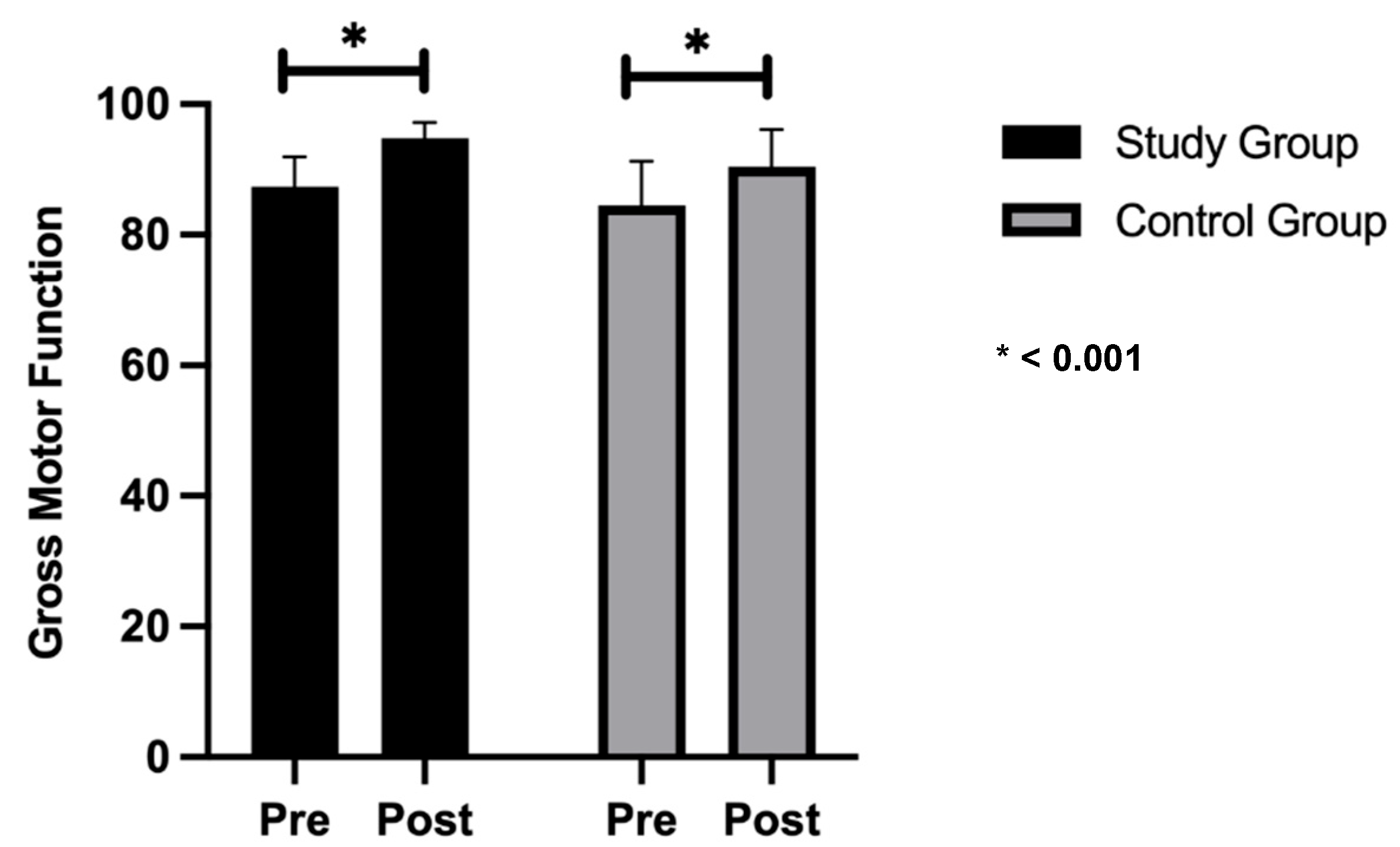
3.2. Gross Motor Function Measures and Pediatric Balance Scale
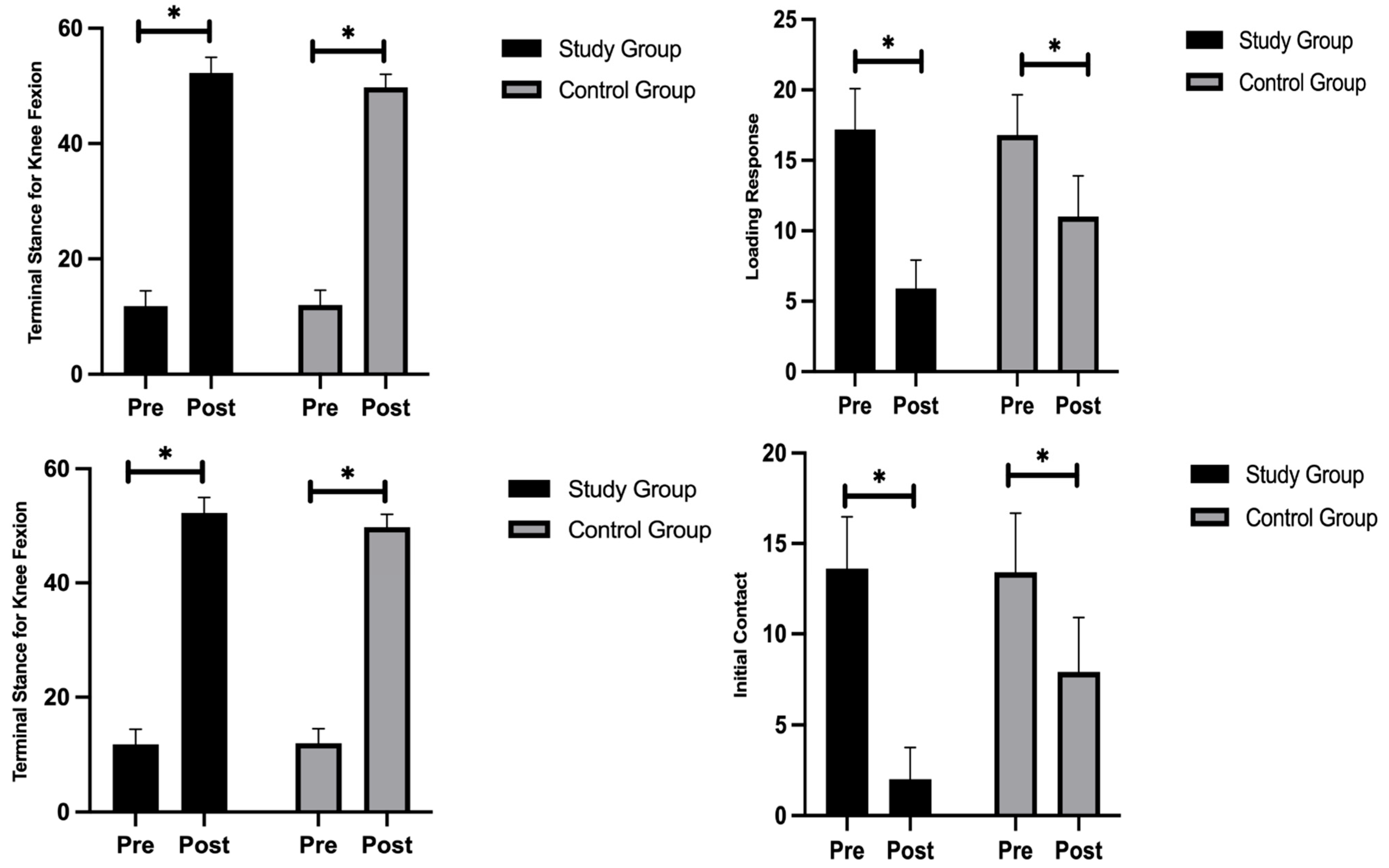
3.3. Knee Flexion During the Gait Cycle
3.4. Ankle Plantar Flexion and Dorsiflexion During the Gait Cycle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CP | Cerebral palsy |
| RCT | Randomized controlled trial |
| MAS | Modified Ashworth Scale |
| GMFCS | Gross Motor Function Classification System |
| PBS | Pediatric Balance Scale |
References
- Alenzy, M.F.S.; Araigah, M.S.A.A.; Al Marshoud, M.M.I.; Medhat, M.W.; Aldossari, A.M.B. An Overview on Cerebral Palsy; Horizon Books: Traverse City, MI, USA, 2021. [Google Scholar]
- Park, S.-H.; Son, S.-M.; Choi, J.-Y. Effect of Posture Control Training Using Virtual Reality Program on Sitting Balance and Trunk Stability in Children with Cerebral Palsy. NeuroRehabilitation 2021, 48, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Danto, A.; Pruzansky, M. 1001 Pediatric Treatment Activities: Creative Ideas for Therapy Sessions; Routledge: Abingdon, UK, 2024. [Google Scholar]
- Tucker, M.R.; Olivier, J.; Pagel, A.; Bleuler, H.; Bouri, M.; Lambercy, O.; Millán, J.D.R.; Riener, R.; Vallery, H.; Gassert, R. Control Strategies for Active Lower Extremity Prosthetics and Orthotics: A Review. J. Neuroeng. Rehabil. 2015, 12, 1. [Google Scholar] [CrossRef]
- Tang-Wai, R.; Webster, R.I.; Shevell, M.I. A Clinical and Etiologic Profile of Spastic Diplegia. Pediatr. Neurol. 2006, 34, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Pierret, J.; Caudron, S.; Paysant, J.; Beyaert, C. Impaired Postural Control of Axial Segments in Children with Cerebral Palsy. Gait Posture 2021, 86, 266–272. [Google Scholar] [CrossRef]
- Saranti, A.; Dragoumi, P.; Papavasiliou, A.; Zafeiriou, D. Current Approach to Cerebral Palsy. Eur. J. Paediatr. Neurol. 2024, 51, 49–57. [Google Scholar] [CrossRef]
- Cook, A.S.; Woollacott, M.H. Motor Control: Theory and Practical Applications; Lippincott Williams and Wilkins: Pennsylvania, PA, USA, 2001. [Google Scholar]
- Alashram, A.R.; Annino, G.; Raju, M.; Padua, E. Effects of Physical Therapy Interventions on Balance Ability in People with Traumatic Brain Injury: A Systematic Review. NeuroRehabilitation 2020, 46, 455–466. [Google Scholar] [CrossRef]
- Faries, M.D.; Greenwood, M. Core Training: Stabilizing the Confusion. Strength Cond. J. 2007, 29, 10–25. [Google Scholar] [CrossRef]
- Behm, D.G.; Drinkwater, E.J.; Willardson, J.M.; Cowley, P.M. The Use of Instability to Train the Core Musculature. Appl. Physiol. Nutr. Metab. 2010, 35, 91–108. [Google Scholar] [CrossRef]
- Huxel Bliven, K.C.; Anderson, B.E. Core Stability Training for Injury Prevention. Sports Health Multidiscip. Approach 2013, 5, 514–522. [Google Scholar] [CrossRef]
- Sasaki, S.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Kimura, Y.; Fujita, Y.; Ishibashi, Y. Core-Muscle Training and Neuromuscular Control of the Lower Limb and Trunk. J. Athl. Train. 2019, 54, 959–969. [Google Scholar] [CrossRef]
- Muir-Hunter, S.W.; Graham, L.; Montero Odasso, M. Reliability of the Berg Balance Scale as a Clinical Measure of Balance in Community-Dwelling Older Adults with Mild to Moderate Alzheimer Disease: A Pilot Study. Physiother. Can. 2015, 67, 255–262. [Google Scholar] [CrossRef]
- Zhou, J.; Zhong, Y.; Xu, W. Effects of Core Stability Exercises on Balance Ability of Children and Adolescents with Intellectual Disabilities: A Systematic Review and Meta-Analysis. PLoS ONE 2024, 19, e0314664. [Google Scholar] [CrossRef]
- Panjabi, M.M. The Stabilizing System of the Spine. Part I. Function, Dysfunction, Adaptation, and Enhancement. J. Spinal Disord. 1992, 5, 383. [Google Scholar] [CrossRef]
- Ozmen, T.; Aydogmus, M. Effect of Core Strength Training on Dynamic Balance and Agility in Adolescent Badminton Players. J. Bodyw. Mov. Ther. 2016, 20, 565–570. [Google Scholar] [CrossRef]
- Yiou, E.; Caderby, T.; Delafontaine, A.; Fourcade, P.; Honeine, J.-L. Balance Control during Gait Initiation: State-of-the-Art and Research Perspectives. World J. Orthop. 2017, 8, 815–828. [Google Scholar] [CrossRef]
- Cabanas-Valdés, R.; Bagur-Calafat, C.; Girabent-Farrés, M.; Caballero-Gómez, F.M.; Du Port De Pontcharra-Serra, H.; German-Romero, A.; Urrútia, G. Long-Term Follow-up of a Randomized Controlled Trial on Additional Core Stability Exercises Training for Improving Dynamic Sitting Balance and Trunk Control in Stroke Patients. Clin. Rehabil. 2017, 31, 1492–1499. [Google Scholar] [CrossRef]
- Daniel, W.W. Biostatistics: A Foundation for Analysis in the Health Sciences; Wiley: Hoboken, NJ, USA, 1978; Volume 129. [Google Scholar]
- Franjoine, M.R.; Gunther, J.S.; Taylor, M.J. Pediatric Balance Scale: A Modified Version of the Berg Balance Scale for the School-Age Child with Mild to Moderate Motor Impairment. Pediatr. Phys. Ther. 2003, 15, 114–128. [Google Scholar] [CrossRef]
- Kalantari, M.; Alimi, E.; Irani, A.; Nazeri, A.; Akbarzade Baghban, A. Content and Face Validity of Pediatric Balance Scale in Children with Spastic Cerebral Palsy. Sci. J. Rehabil. Med. 2016, 5, 104–110. [Google Scholar]
- Pellatt, L.; Dewar, A.; Philippides, A.; Roggen, D. Mapping Vicon Motion Tracking to 6-Axis IMU Data for Wearable Activity Recognition. In Activity and Behavior Computing; Ahad, M.A.R., Inoue, S., Roggen, D., Fujinami, K., Eds.; Smart Innovation, Systems and Technologies; Springer: Singapore, 2021; Volume 204, pp. 3–20. ISBN 9789811589430. [Google Scholar]
- Puig-Diví, A.; Escalona-Marfil, C.; Padullés-Riu, J.M.; Busquets, A.; Padullés-Chando, X.; Marcos-Ruiz, D. Validity and Reliability of the Kinovea Program in Obtaining Angles and Distances Using Coordinates in 4 Perspectives. PLoS ONE 2019, 14, e0216448. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.; Alghamdi, G.A.; Alghamdi, M.A.; Altowaijri, A.; Richardson, S. The Relationship of Lower Limb Muscle Strength and Knee Joint Hyperextension during the Stance Phase of Gait in Hemiparetic Stroke Patients. Physiother. Res. Int. 2012, 17, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Gait, V.P. Product Guide—Foundation Notes 2010. Available online: https://help.vicon.com/download/attachments/11378719/Plug-in%20Gait%20Reference%20Guide.pdf (accessed on 19 May 2023).
- Russell, D.J.; Rosenbaum, P.L.; Cadman, D.T.; Gowland, C.; Hardy, S.; Jarvis, S. The Gross Motor Function Measure: A Means to Evaluate the Effects of Physical Therapy. Dev. Med. Child Neurol. 1989, 31, 341–352. [Google Scholar] [CrossRef]
- Vuijk, P.J.; Hartman, E.; Scherder, E.; Visscher, C. Motor Performance of Children with Mild Intellectual Disability and Borderline Intellectual Functioning. J. Intellect. Disabil. Res. 2010, 54, 955–965. [Google Scholar] [CrossRef]
- Surbala, L.; Khuman, P.R.; Trivedi, P.; Devanshi, B.; Mital, V. Pilates versus Conventional Balance Training on Functional Balance and Quality of Life in Elderly Individuals: A Randomized Controlled Study. Sch. J. Appl. Med. Sci. 2014, 2, 221–226. [Google Scholar]
- Fry, A.C.; Irwin, C.C.; Nicoll, J.X.; Ferebee, D.E. Muscular Strength and Power in 3-to 7-Year-Old Children. Pediatr. Exerc. Sci. 2015, 27, 345–354. [Google Scholar] [CrossRef]
- Zadnikar, M.; Kastrin, A. Effects of Hippotherapy and Therapeutic Horseback Riding on Postural Control or Balance in Children with Cerebral Palsy: A Meta-Analysis: Review. Dev. Med. Child Neurol. 2011, 53, 684–691. [Google Scholar] [CrossRef]
- Uyanik, M.; Kayihan, H. Down Syndrome: Sensory Integration, Vestibular Stimulation and Neurodevelopmental Therapy Approaches for Children. Int. Encycl. Rehabil. 2010, 9, 1–22. [Google Scholar]
- Bahramizadeh, M.; Mousavi, M.E.; Rassafiani, M.; Aminian, G.; Ebrahimi, I.; Karimlou, M.; Toole, G.O. The Effect of Floor Reaction Ankle Foot Orthosis on Postural Control in Children with Spastic Cerebral Palsy. Prosthet. Orthot. Int. 2012, 36, 71–76. [Google Scholar] [CrossRef]
- Sahoo, J.; Halder, M.S.K.; Sethy, M.M.K. Effect of Standing to Improve Balance and Gait of Children with Cerebral Palsy. Int. J. Trend Sci. Res. Dev. 2020, 5, 398–404. [Google Scholar]
- Aksen-Cengizhan, P.; Onay, D.; Sever, O.; Doğan, A.A. A Comparison between Core Exercises with Theraband and Swiss Ball in Terms of Core Stabilization and Balance Performance. Isokinet. Exerc. Sci. 2018, 26, 183–191. [Google Scholar] [CrossRef]
- Chaudhari, A.M.; Van Horn, M.R.; Monfort, S.M.; Pan, X.; Oñate, J.A.; Best, T.M. Reducing Core Stability Influences Lower Extremity Biomechanics in Novice Runners. Med. Sci. Sports Exerc. 2020, 52, 1347–1353. [Google Scholar] [CrossRef]
- Alizamani, S.; Ghasemi, G.; Nejadian, S.L. Effects of Eight Week Core Stability Training on Stable-and Unstable-Surface on Ankle Muscular Strength, Proprioception, and Dorsiflexion in Athletes with Chronic Ankle Instability. J. Bodyw. Mov. Ther. 2023, 34, 6–12. [Google Scholar] [CrossRef]
- Zawadka, M.; Smołka, J.; Skublewska-Paszkowska, M.; Łukasik, E.; Zieliński, G.; Byś, A.; Gawda, P. Altered Squat Movement Pattern in Patients with Chronic Low Back Pain. Ann. Agric. Environ. Med. 2021, 28, 158–162. [Google Scholar] [CrossRef]

| Frequency & Duration | 3 sessions per week, 60 min per session |
| Session Structure |
|
| Conventional Physiotherapy (30 min) |
|
| Core Stability Training (30 min) | Progressive levels (3 levels) |
| Level 1 (Beginner) |
|
| Level 2 (Intermediate) |
|
| Level 3 (Advanced) |
|
| Rest Periods | 30–60 s between exercises |
| Repetition of Sequence | Full sequence repeated 3–5 times per session based on tolerance |
| Exercise | Description | Dosage | Progression |
|---|---|---|---|
| Walking on variable surfaces | Walking on soft mats, foam pads, and firm ground | 20 steps per surface × 3 sets | Increase surface difficulty and reduce support |
| Transitioning between kneeling and standing | Practicing transitions from kneeling to standing | 20 transitions × 3–5 sets | Increase repetitions or reduce assistive support |
| Step training (ascending and descending) | Using a 15 cm step platform to practice ascending and descending steps with support as needed | 10 ascents + 10 descents per set × 3–5 sets | Increase step height or reduce assistance |
| Dual-task standing and walking activities | Walking while performing cognitive tasks such as holding an object or counting aloud | 10 m of dual-task walking × 3 repetitions | Add more complex cognitive tasks or increase distance |
| Single-limb stance (eyes open and closed) | Balancing on one leg with eyes open or closed, near a stable support for safety | 10–20 s per leg × 3 repetitions | Increase duration or progress from eyes open to closed |
| Variable | Study Group | Control Group | t-Value | p-Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Age (years) | 6.2 ± 1.87 | 5.4 ± 0.97 | 1.2 | 0.246 |
| Height (cm) | 123.1 ± 6.67 | 121.9 ± 16.24 | 0.216 | 0.831 |
| Weight (kg) | 35.1 ± 7.13 | 28 ± 9.24 | 1.925 | 0.07 |
| Variables | Group | Mean Difference | p-Value Group × Time Interaction | ||
|---|---|---|---|---|---|
| Study | Control | ||||
| Mean ± SD | Mean ± SD | ||||
| Gross Motor Function Measure | Pre-test | 87.39 ± 4.59 | 84.56 ± 6.74 | 2.83 | 0.29 |
| Post-test | 94.82 ± 2.42 | 90.48 ± 5.67 | 4.34 | 0.3 | |
| p-value | <0.001 | <0.001 | |||
| Pediatric Balance Scale | Pre-test | 48 ± 3.83 | 47.4 ± 2.8 | 0.6 | 0.69 |
| Post-test | 52.3 ± 2.67 | 49.8 ± 2.2 | 2.5 | 0.04 | |
| p-value | <0.001 | <0.001 | |||
| Variables | Group | Mean Difference | p-Value Group × Time Interaction | ||
|---|---|---|---|---|---|
| Study | Control | ||||
| Mean ± SD | Mean ± SD | ||||
| Terminal Stance | Pre-test | 11.8 ± 2.66 | 12 ± 2.58 | 0.2 | 0.866 |
| Post-test | 2.3 ± 1.7 | 7.1 ± 2.6 | 4.8 | 0.0001 | |
| p-value | <0.001 | <0.001 | |||
| Loading Response | Pre-test | 17.2 ± 2.94 | 16.8 ± 2.86 | 0.4 | 0.76 |
| Post-test | 5.9 ± 2.02 | 11 ± 2.91 | 5.1 | 0.0002 | |
| p-value | <0.001 | <0.001 | |||
| Initial Contact | Pre-test | 13.6 ± 2.88 | 13.4 ± 3.27 | 0.2 | 0.88 |
| Post-test | 2 ± 1.76 | 7.9 ± 3 | 5.9 | <0.001 | |
| p-value | <0.001 | <0.001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamed, N.; Ibrahim, M.B.; El-Agamy, O.A.; Aldhahi, M.I.; Elsebahy, S.Y. Effects of Core Stability Training on Balance, Standing, and Gait in Children with Mild Cerebral Palsy: A Randomized Controlled Trial. Healthcare 2025, 13, 1296. https://doi.org/10.3390/healthcare13111296
Mohamed N, Ibrahim MB, El-Agamy OA, Aldhahi MI, Elsebahy SY. Effects of Core Stability Training on Balance, Standing, and Gait in Children with Mild Cerebral Palsy: A Randomized Controlled Trial. Healthcare. 2025; 13(11):1296. https://doi.org/10.3390/healthcare13111296
Chicago/Turabian StyleMohamed, Nancy, Mohamed B. Ibrahim, Osama A. El-Agamy, Monira I. Aldhahi, and Sara Y. Elsebahy. 2025. "Effects of Core Stability Training on Balance, Standing, and Gait in Children with Mild Cerebral Palsy: A Randomized Controlled Trial" Healthcare 13, no. 11: 1296. https://doi.org/10.3390/healthcare13111296
APA StyleMohamed, N., Ibrahim, M. B., El-Agamy, O. A., Aldhahi, M. I., & Elsebahy, S. Y. (2025). Effects of Core Stability Training on Balance, Standing, and Gait in Children with Mild Cerebral Palsy: A Randomized Controlled Trial. Healthcare, 13(11), 1296. https://doi.org/10.3390/healthcare13111296







