Development and Validation of the Patient-Centered Communication Competency Scale for Dental Hygienists
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Ethical Considerations
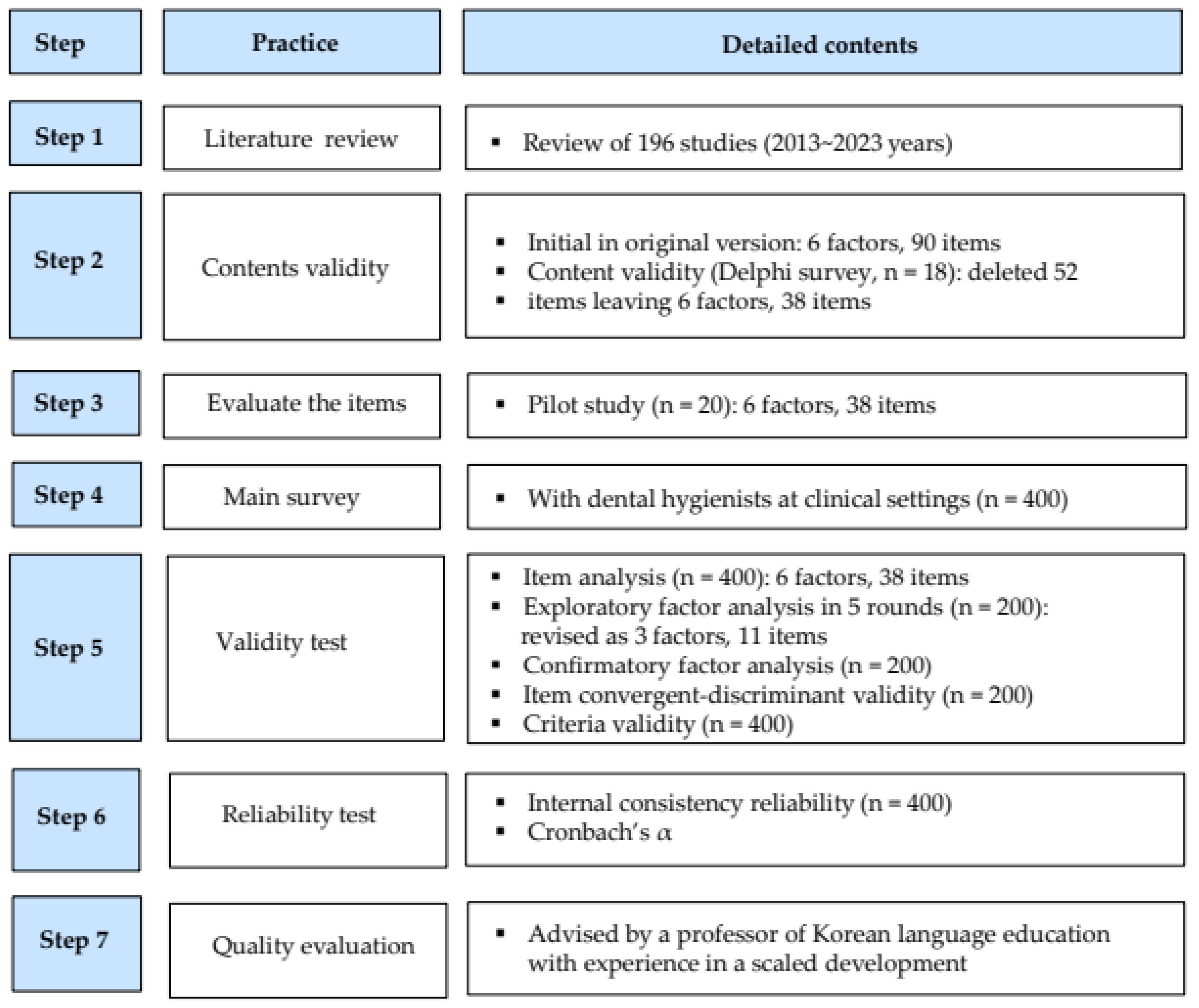
2.2. Scale Development
2.2.1. Conceptual Framework and Initial Item Generation
2.2.2. Content Validity
2.2.3. Preliminary Survey
2.3. Validity and Reliability
2.3.1. Participants
2.3.2. Measurement
2.3.3. Data Collection
2.3.4. Validity and Reliability Tests
2.4. Optimization of PCCS
3. Results
3.1. Demographic Characteristics of Study Participants
3.2. Item Analysis
3.3. Construct Validity
3.3.1. Exploratory Factor Analysis (EFA)
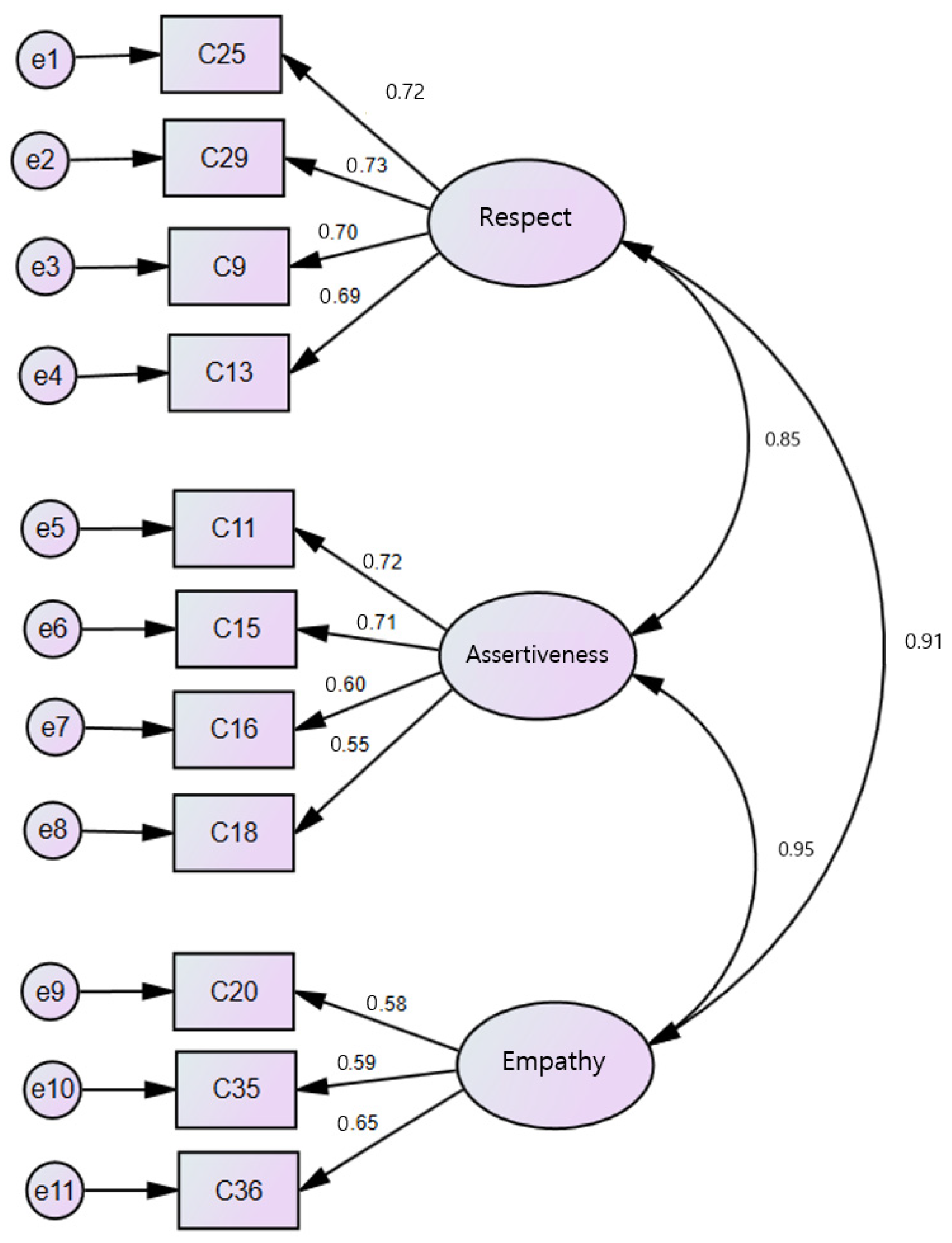
3.3.2. Confirmatory Factor Analysis for Validity (CFA)
3.4. Criteria Validity and Reliability of PCCS
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AVE | average variance extracted |
| CFA | confirmatory factor analysis |
| CFI | comparative fit index |
| CR | construct reliability |
| EFA | exploratory factor analysis |
| GFI | goodness-of-fit index |
| IFI | incremental fit index |
| NFI | normed fit index |
| PCCS | Patient-Centered Communication Competency Scale |
| RMR | root mean residual |
| RMSEA | root mean square error of approximation |
| TLI | Tucker–Lewis index |
References
- Lee, S.K.; Hwang, K.S.; Park, Y.D.; Beom, K.C. The relationship between factors influencing smooth communication among dental workers. J. Korean Acad. Oral Health 2011, 35, 85–92. [Google Scholar]
- Son, Y.H. An exploratory study for development of tools to measure university students’ communication competence. J. Speech Media Commun. Assoc. 2016, 15, 83–107. [Google Scholar]
- Heo, Y.J. Doctor’s competency and empowerment measures desired by the state and society. J. Korean Med. Assoc. 2014, 57, 121–127. [Google Scholar] [CrossRef][Green Version]
- Kim, A.; Cho, M. A comparison of dental hygienists’ legal duties among nations: Korea, USA and Canada. J. Korean Soc. Oral Health Sci. 2019, 7, 18–28. [Google Scholar] [CrossRef]
- Kim, H.J. Development and Validation of a Self-Assessment Tool for Communication Skills Needed in Nursing Assessment. Ph.D. Thesis, Eulji University, Daejeon, Republic of Korea, 2021. [Google Scholar]
- Kang, S.K.; Bae, K.H.; Lim, S.R. Analysis of communication of dental hygienist in oral hygiene instruction during scaling. J. Dent. Hyg. Sci. 2014, 14, 546–553. [Google Scholar] [CrossRef][Green Version]
- Howick, J.; Moscrop, A.; Mebius, A.; Fanshawe, T.R.; Lewith, G.; Bishop, F.L.; Mistiaen, P.; Roberts, N.W.; Dieninytė, E.; Hu, X.Y.; et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J. R. Soc. Med. 2018, 111, 240–252. [Google Scholar] [CrossRef]
- Haribhai-Thompson, J.; McBride-Henry, K.; Hales, C.; Rook, H. Understanding of empathetic communication in acute hospital settings: A scoping review. BMJ Open 2022, 12, e063375. [Google Scholar] [CrossRef]
- Kang, J.O.; Kim, J.H.; Hwang, J.M.; Kwon, H.J.; Seong, J.M.; Lee, S.K.; Kim, C.H.; Kim, H.Y.; Cho, Y.S.; Park, Y.D. Recognition about communication of dental personnel in dental clinics and hospitals in the capital. J. Korean Acad. Oral Health 2010, 34, 318–326. [Google Scholar]
- Moon, H.J.; Lee, S.Y.; Lim, S.R. Validity and reliability of the assessment tool for measuring communication skills of dental hygienist. J. Dent. Hyg. Sci. 2014, 14, 198–206. [Google Scholar]
- Gwon, A.R.; Han, S.J. Effect of communication competence on the organizational effectiveness in dental hygienists. J. Korean Soc. Dent. Hyg. 2015, 15, 1009–1017. [Google Scholar] [CrossRef]
- Jeong, M.A. The study on effect of communication ability of dental hygienist on job satisfaction and turnover intention. J. Korea Contents Assoc. 2022, 22, 579–586. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kang, Y.J. A study on factors affecting job satisfaction of dental hygienists. J. Korea Contents Assoc. 2019, 19, 478–488. [Google Scholar] [CrossRef]
- Choi, D.S.; Kim, S.H.; Kim, J.S. A comparative analysis of competencies in American dental education association and American dental hygiene schools. J. Korean Soc. Dent. Hyg. 2015, 15, 547–553. [Google Scholar] [CrossRef]
- Sasaki, N.; Pang, J.; Surdu, S.; Morrissey, R.W.; Vujicic, M.; Moore, J. Workplace factors associated with job satisfaction among dental hygienists and assistants in the United States. Health Aff. Sch. 2025, 3, qxae 147. [Google Scholar] [CrossRef]
- Loeffen, A.W.M.; Van Swaaij, B.W.M.; Saminsky, M.; Slot, D.E. Common practices of dental implant maintenance among dental hygienists working in the Netherlands—A survey. Int. J. Dent. Hyg. 2025, 23, 14–25. [Google Scholar] [CrossRef]
- Moon, H.J.; Lim, S.R. Development of a job competency model of a dental intermediary-manager using the Delphi method. J. Dent. Hyg. Sci. 2017, 17, 150–159. [Google Scholar] [CrossRef]
- Hur, G.H. Construction and validation of a global interpersonal communication competence scale. Korean Soc. J. Commun. Stud. 2003, 47, 380–408. [Google Scholar]
- Kim, H.J.; Oh, H.Y. The validity and reliability of Nursing Assessment Communication-Competence Scale for clinical nurses. J. Korean Acad. Fundam. Nurs. 2023, 30, 78–89. [Google Scholar] [CrossRef]
- Jeong, N.K.; Kim, J.H. The developing and validation of communication ability scale. Korean Soc. Creat. Educ. 2010, 10, 85–109. [Google Scholar]
- Kim, D.E.; Jang, J.H. Communication competency for dental hygienists in Korea: A scoping review. J. Korean Soc. Dent. Hyg. 2024, 12, 361–372. [Google Scholar] [CrossRef]
- DeVellis, R.F. Scale Development: Theory and Applications, 4th ed.; Sage: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Ho, J.C.Y.; Chai, H.H.; Lo, E.C.M.; Huang, M.Z.; Chu, C.H. Strategies for effective dentist-patient communication: A literature review. Patient Prefer. Adherence 2024, 18, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Hymes, D. Foundations in Sociolinguistics; University of Pennsylvania Press: Philadelphia, PA, USA, 1974. [Google Scholar]
- Lee, Y.H.; Lee, Y.M.; Park, Y.G. Patients’ expectations of a good dentist: The views of communication. Korean J. Health Commun. 2011, 6, 89–104. [Google Scholar] [CrossRef]
- Rogers, C.R. Client-Centered Therapy; Houghton-Mifflin: Boston, MA, USA, 1951; p. 560. [Google Scholar]
- Lee, H.; Chalmers, N.I.; Brow, A.; Boynes, S.; Monopoli, M.; Doherty, M.; Croom, O.; Engineer, L. Person-centered care model in dentistry. BMC Oral Health. 2018, 18, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Apelian, N.; Vergnes, J.N.; Hovey, R.; Bedos, C. How can we provide person-centred dental care? Br. Dent. J. 2017, 223, 419–424. [Google Scholar] [CrossRef]
- Ko, Y.J.; Hong, G.R. Development and evaluation of nursing work environment scale of clinical nurses. J. Korean Acad. Nurs. Adm. 2022, 28, 576–585. [Google Scholar] [CrossRef]
- Nunnally, J.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw Hill: New York, NY, USA, 1994. [Google Scholar]
- Hair, J.F., Jr.; Anderson, R.E.; Babin, B.J.; Black, W.C. Multivariate Data Analysis: A Global Perspective, 7th ed.; Pearson Education: Harlow, UK, 2010. [Google Scholar]
- Arrindell, W.A.; Van der Ende, J. An empirical test of the utility of the observations-to-variables ratio in factor and components analysis. Appl. Psychol. Meas. 1985, 9, 165–178. [Google Scholar] [CrossRef]
- Park, J.H. Development of Dental Hygienists Job Satisfaction Scale and Path Analysis of Psychological Ownership, Job Engagement, Job Performance. Ph.D. Thesis, Namseoul University, Chungcheongnam-do, Republic of Korea, 2020. [Google Scholar]
- Chen, G.; Gully, S.M.; Eden, D. Validation of a new general self-efficacy scale. Organ. Res. Methods 2001, 4, 62–83. [Google Scholar] [CrossRef]
- Cho, H.J. A Study of the Effects of Resilience Factor on Flight Attendants’ Job Performance and Organizational Effectiveness: Focused on the Mediating Effects of Self-Efficacy. Ph.D. Thesis, Kyonggi University, Seoul, Republic of Korea, 2016. [Google Scholar]
- Mishra, P.; Pandey, C.M.; Singh, U.; Gupta, A.; Sahu, C.; Keshri, A. Descriptive statistics and normality tests for statistical data. Ann. Card. Anaesth. 2019, 22, 67–72. [Google Scholar] [CrossRef]
- Lee, B.S.; Eo, Y.S.; Lee, M.A. Development of job satisfaction scale for clinical nurses. J. Korean Acad. Nurs. 2018, 48, 12–25. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics: And Sex and Drugs and Rock ‘n’ Roll, 4th ed.; Sage Publications: London, UK, 2013. [Google Scholar]
- Heo, M.L. Development of the Patient Caring Communication Scale. Ph.D. Thesis, Eulji University, Daejeon, Republic of Korea, 2018. [Google Scholar]
- Hong, S.H. The criteria for selecting appropriate fit indices in structural equation modeling and their rationales. Korean J. Cli. Psychol. 2020, 19, 161–177. [Google Scholar]
- Choi, C.H.; Yoo, Y.Y. The study on the comparative analysis of EFA and CFA. J. Digit. Converg. 2017, 15, 103–111. [Google Scholar] [CrossRef]
- Song, T.M.; Kim, G.S. Structural Equation Modeling for Health & Welfare Research: From Beginner to Advanced; Hannarae Academy: Seoul, Republic of Korea, 2012. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Oldham, G.R.; Hackman, J.R. Not what it was and not what it will be: The future of job design research. J. Organ. Behav. 2010, 31, 463–479. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy. In The Corsini Encyclopedia of Psychology; American Cancer Society: Atlanta, GA, USA, 2010; pp. 1–3. [Google Scholar]
- Lee, I.H. The sub-elements of communication competency as core competence reflected in the 2015 revised curriculum. J. Curric. Eval. 2019, 22, 1–29. [Google Scholar] [CrossRef]
- McCabe, C. Nurse-patient communication: An exploration of patients’ experiences. J. Clin. Nurs. 2004, 13, 41–49. [Google Scholar] [CrossRef]
- Felix Gomez, G.G.; Mao, J.M.; Thyvalikakath, T.P.; Li, S. Building bridges: Fostering collaborative education in training dental informaticians. Appl. Clin. Inform. 2025, 16, 205–214. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, J.M. A study on the relationship between patient’s medical communication, reliance, and satisfaction to dental hygienist. J. Korean Soc. Dent. Hyg. 2012, 12, 1017–1027. [Google Scholar] [CrossRef][Green Version]
- Ghahremani, L.; Khoramaki, Z.; Kaveh, M.H.; Karimi, M.; Nazari, M.; Orgambídez Ramos, A. Communication self-Efficacy and job satisfaction among nurses during the COVID-19 pandemic. J. Nur. Manag. 2024, 2024, 8869949. [Google Scholar] [CrossRef]
- Kim, B.J.; Lee, S.Y.; An, G.J.; Lee, G.A.; Yun, H.J. Influence of communication competency and nursing work environment on job satisfaction in hospital nurses. J. Health Inform. Stat. 2019, 44, 189–197. [Google Scholar] [CrossRef]
- Lee, A.K.; Yeo, J.Y.; Jung, S.W.; Byun, S.S. Relations on communication competence, job stress, and job satisfaction of clinical nurses. J. Korea Contents Assoc. 2013, 13, 299–308. [Google Scholar] [CrossRef]
- Ho, J.C.Y.; Chai, H.H.; Luo, B.W.; Lo, E.C.M.; Huang, M.Z.; Chu, C.H. An overview of dentist–patient communication in quality dental care. Dent. J. 2025, 13, 31. [Google Scholar] [CrossRef] [PubMed]

| Variables | Categories | Total (n = 400) | EFA (n = 200) | CFA (n = 200) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Sex | Male | 38 (9.5) | 18 (9.0) | 20 (10.0) |
| Female | 362 (90.5) | 182 (91.0) | 180 (90.0) | |
| Age (in years) | ≤29 | 147 (36.8) | 75 (37.5) | 72 (36.0) |
| 30–39 | 212 (53.0) | 103 (51.5) | 109 (54.5) | |
| ≥40 | 41 (10.3) | 22 (11.0) | 19 (9.5) | |
| Education | College | 222 (55.5) | 112 (56.0) | 110 (55.0) |
| University | 132 (33.0) | 67 (33.5) | 65 (32.5) | |
| ≥Master | 46 (11.5) | 21 (10.5) | 25 (12.5) | |
| Workplace | Dental clinic | 300 (75.0) | 143 (71.5) | 157 (78.5) |
| Dental hospital | 84 (21.0) | 48 (24.0) | 36 (18.0) | |
| Tertiary hospital | 13 (3.3) | 8 (4.0) | 5 (2.5) | |
| Others | 3 (0.8) | 1 (0.5) | 2 (1.0) | |
| Work experience (in years) | ≤3 | 70 (17.5) | 32 (16.0) | 38 (9.0) |
| ≥3–≤7 | 140 (35.0) | 69 (34.5) | 71 (35.5) | |
| ≥7 | 178 (44.5) | 94 (47.0) | 84 (42.0) | |
| Current position | Clinical dental hygienist | 257 (64.3) | 129 (64.5) | 128 (64.0) |
| Team leader | 53 (13.3) | 29 (14.5) | 24 (12.0) | |
| Counseling manager | 68 (17.0) | 31 (15.5) | 37 (18.5) | |
| Others | 22 (5.5) | 11 (5.5) | 11 (5.5) |
| No | Items | Item-Total Correlation | Factor Loading | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| 25 | Encourage patients to express their emotions freely | 0.612 | 0.743 | 0.093 | 0.226 |
| 29 | Present information by topic at a pace the patient can follow | 0.600 | 0.763 | 0.107 | 0.080 |
| 9 | Mirror the patient’s words or actions to demonstrate empathy | 0.587 | 0.692 | 0.272 | 0.185 |
| 13 | Repeat questions to clarify implied content and emotions | 0.502 | 0.661 | 0.198 | 0.157 |
| 11 | Communicate in a structured and proficient manner | 0.462 | 0.361 | 0.526 | 0.235 |
| 15 | Summarize key points throughout the conversation | 0.683 | 0.161 | 0.791 | 0.176 |
| 16 | Clearly signal transitions between topics or situations. | 0.628 | 0.103 | 0.695 | 0.367 |
| 18 | Redirect off-topic discussions back to the main topic | 0.553 | 0.164 | 0.725 | −0.011 |
| 20 | Clarify expectations regarding diagnosis, treatment, prognosis | 0.682 | 0.165 | 0.302 | 0.751 |
| 35 | Conclude communication with gratitude for cooperation | 0.675 | 0.151 | 0.104 | 0.801 |
| 36 | Ask if the patient has any additional questions or concerns | 0.672 | 0.256 | 0.118 | 0.770 |
| Eigenvalues | 2.360 | 2.160 | 21.453 | ||
| % of variance | 21.453 | 19.640 | 41.093 | ||
| % of cumulated variance | 21.453 | 19.413 | 60.508 | ||
| Kaiser–Meyer–Olkin (KMO) value: 0.84, Bartlett’s sphericity test value: 674.772 (p < 0.001) | |||||
| Concept | Factors | Item Number | Standardized Estimate (β) | SE | AVE | CR |
|---|---|---|---|---|---|---|
| Behavioral | Respect | 25 | 0.715 | 0.308 | 0.614 | 0.864 |
| 29 | 0.729 | 0.273 | ||||
| 9 | 0.703 | 0.339 | ||||
| 13 | 0.691 | 0.348 | ||||
| Cognitive | Assertiveness | 11 | 0.715 | 0.342 | 0.533 | 0.818 |
| 15 | 0.705 | 0.327 | ||||
| 16 | 0.598 | 0.318 | ||||
| 18 | 0.547 | 0.473 | ||||
| Affective | Empathy | 20 | 0.583 | 0.441 | 0.472 | 0.728 |
| 35 | 0.594 | 0.440 | ||||
| 36 | 0.646 | 0.362 | ||||
| Model fitness: χ2/df = 1.749, RMR = 0.027, RMSEA = 0.061, GFI = 0.941, NFI = 0.911, IFI = 0.960, CFI = 0.959, TLI = 0.949 | ||||||
| Factors | Respect | Assertiveness | Empathy |
|---|---|---|---|
| Respect | 0.783 | ||
| Assertiveness | 0.584 * | 0.730 | |
| Empathy | 0.551 * | 0.566 * | 0.687 |
| PCCS | Self-Efficacy | Job Satisfaction | Mean ± SD | Cronbach’s α |
|---|---|---|---|---|
| r | r | |||
| Total | 0.603 * | 0.624 * | 3.94 ± 0.52 | 0.862 |
| Respect | 0.441 * | 0.592 * | 3.94 ± 0.63 | 0.777 |
| Assertiveness | 0.526 * | 0.520 * | 3.95 ± 0.57 | 0.731 |
| Empathy | 0.548 * | 0.452 * | 3.93 ± 0.66 | 0.701 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.-E.; Jang, J.-H. Development and Validation of the Patient-Centered Communication Competency Scale for Dental Hygienists. Healthcare 2025, 13, 1241. https://doi.org/10.3390/healthcare13111241
Kim D-E, Jang J-H. Development and Validation of the Patient-Centered Communication Competency Scale for Dental Hygienists. Healthcare. 2025; 13(11):1241. https://doi.org/10.3390/healthcare13111241
Chicago/Turabian StyleKim, Da-Eun, and Jong-Hwa Jang. 2025. "Development and Validation of the Patient-Centered Communication Competency Scale for Dental Hygienists" Healthcare 13, no. 11: 1241. https://doi.org/10.3390/healthcare13111241
APA StyleKim, D.-E., & Jang, J.-H. (2025). Development and Validation of the Patient-Centered Communication Competency Scale for Dental Hygienists. Healthcare, 13(11), 1241. https://doi.org/10.3390/healthcare13111241






