Pregnancy Care in Times of Cannabis Legalization: Self-Rated Knowledge, Risk Perception and Communication Practices of Midwives in Germany
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Study Population and Recruitment
2.3. Questionnaire and Data Collection
2.4. Data Preparation and Analysis
2.5. Ethical and Data Protection Aspects
3. Results
3.1. Sociodemographic Characteristics of the Sample
3.2. Midwives’ Knowledge About Cannabis Use During Pregnancy
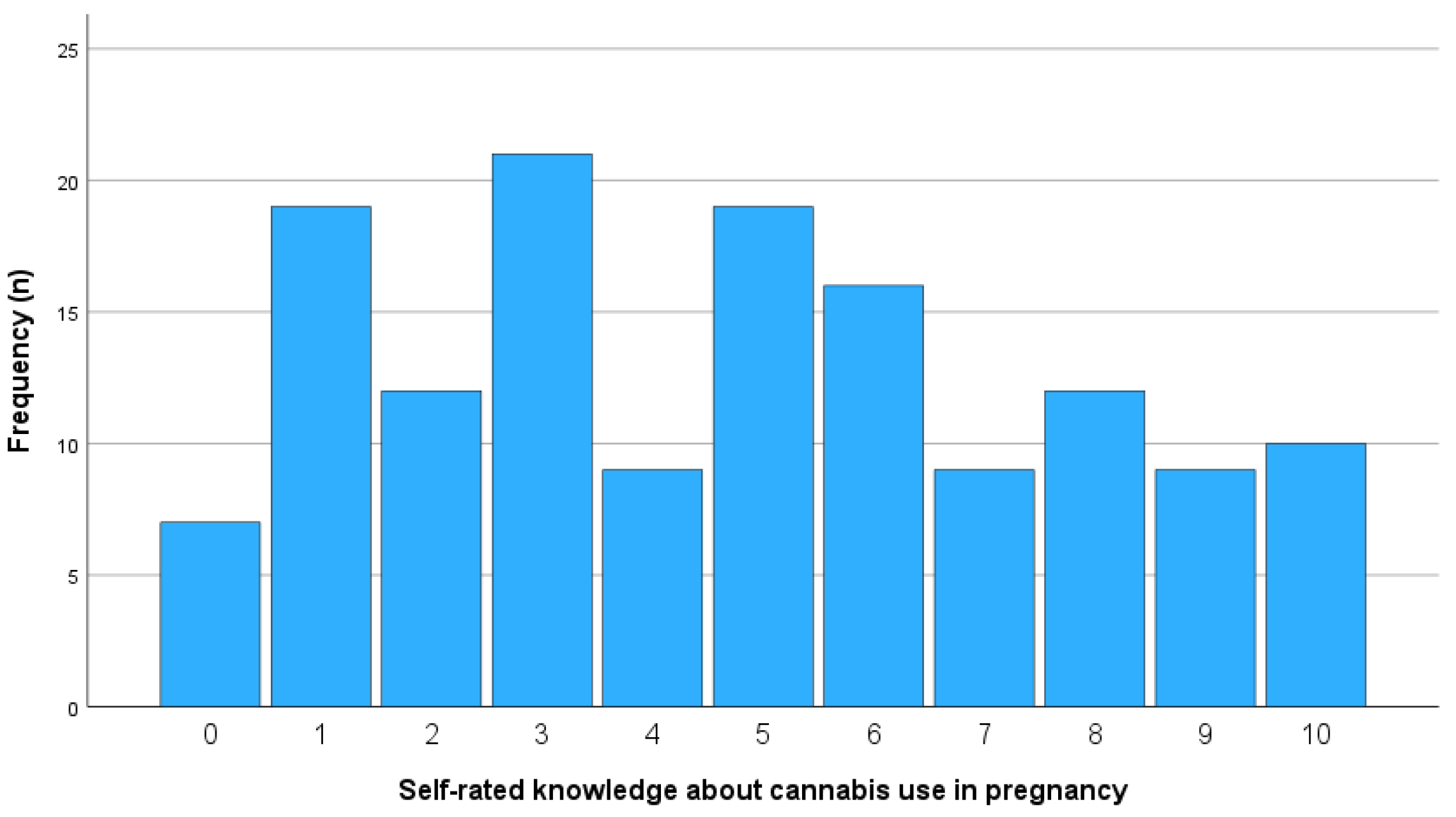
3.2.1. Self-Rated Knowledge Level
3.2.2. Education and Training
3.2.3. Influence of Age
3.3. Risk Perception of Cannabis Use During Pregnancy
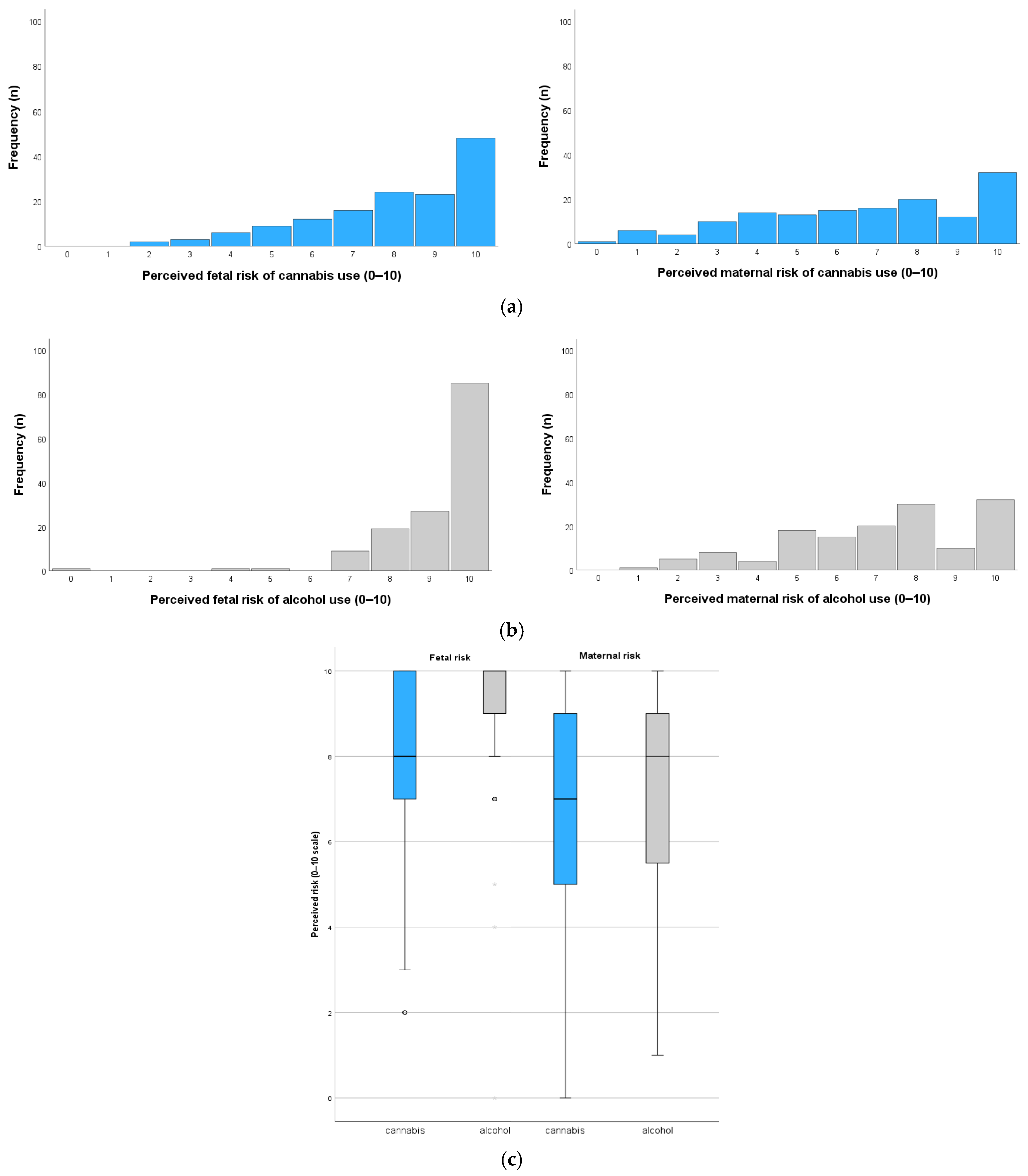
3.3.1. Perceived Risks of Cannabis Use for the Fetus and the Pregnant Person
3.3.2. Predictors of Risk Perception
3.4. Communication and Counseling Behavior Regarding Cannabis Use
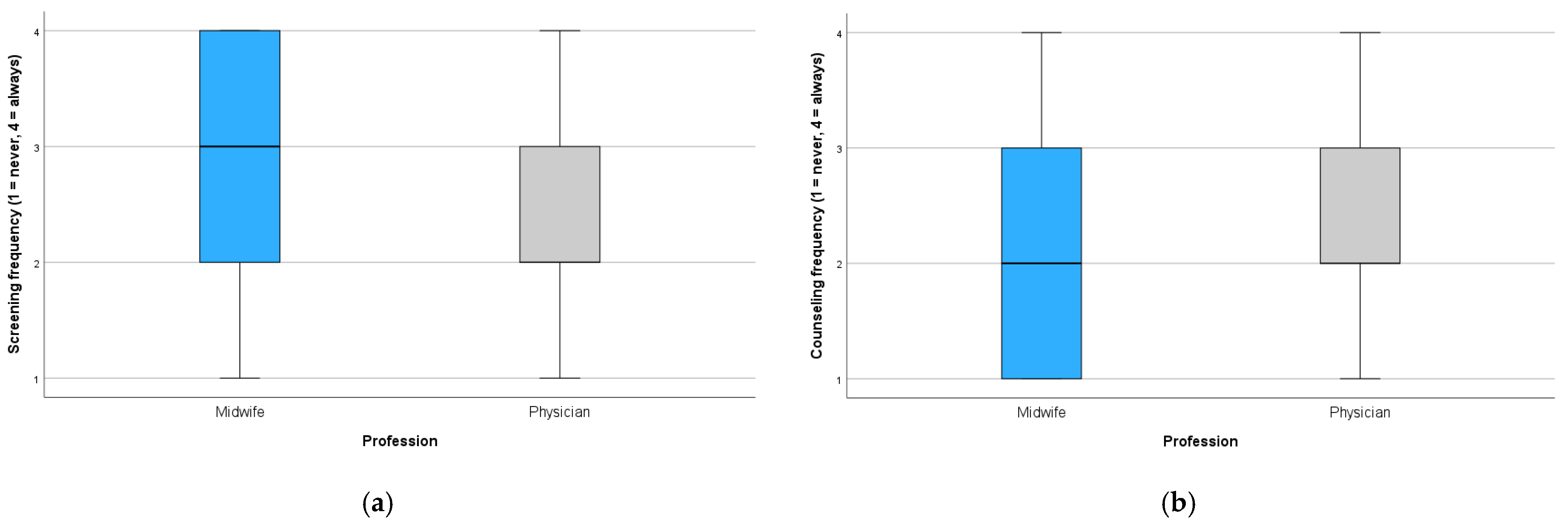
3.4.1. Frequency of Screening and Counseling on Cannabis Use
3.4.2. Influence of Profession
3.4.3. Influence of Age and Knowledge Level on Screening/Counseling Behavior
4. Discussion
4.1. Summary of Key Findings
4.2. Integration with Existing Literature
4.2.1. Knowledge
4.2.2. Risk Perception
4.2.3. Communication Practices
4.3. Strengths and Limitations
4.4. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BIÖG | Federal Institute for Public Health (Germany) |
| CB1 | cannabinoid receptor type 1 |
| d | D |
| EU GDPR | European Union General Data Protection Regulation |
| F | F-statistic (from ANOVA or regression) |
| IUGR | Intrauterine Growth Restriction |
| LBW | Low Birth Weight |
| M | Mean |
| p | p-Value |
| r | Pearson’s correlation coefficient |
| ρ | Spearman’s rank correlation coefficient |
| SD | Standard Deviation |
| SGA | Small for Gestational Age |
| THC | Tetrahydrocannabinol |
| X2 | Chi-squared statistic |
| Z | Z-statistic (e.g., from Wilcoxon test) |
| β | Standardized regression coefficient |
Appendix A. Summary of Statistical Results
| Outcome Variable | Predictor | Test(s) Used | Group Difference | t(df)/Z/χ2 | p-Value | Effect Size (Cohen’s d) | Correlation (ρ, p) | Regression (β, p) |
|---|---|---|---|---|---|---|---|---|
| Self-rated knowledge | Substance 1 | Paired t-test, correlation | Yes | t(142) = −9.09 | <0.001 *** | 0.76 | 0.31 (<0.001) | – |
| Profession 2 | t-test | No | t(274) = 1.54 | 0.125 | 0.18 | – | – | |
| Age | Spearman | – | – | – | – | 0.39 (<0.001) | – | |
| Initial training | t-test | No | t(141) = −0.85 | 0.399 | −0.17 | – | – | |
| Further training | t-test | Yes | t(106.6) = 2.77 | 0.007 ** | 0.48 | – | – | |
| Risk Perception (fetus) | Profession | t-test | No | t(280.3) = −1.77 | 0.078 | 0.21 | – | – |
| Age | Spearman, Regression | – | – | – | – | 0.20 (0.016) | 0.26 (0.005) | |
| Knowledge | Spearman, Regression | – | – | – | – | 0.20 (0.016) | 0.11 (0.225) | |
| Risk Perception (mother) | Profession | t-test | No | t(281.9) = −0.50 | 0.615 | 0.06 | – | – |
| Age | Spearman, Regression | – | – | 0.001 | – | 0.27 (0.001) | 0.20 (0.030) | |
| Knowledge | Spearman, Regression | – | – | 0.002 | – | 0.26 (0.002) | 0.20 (0.026) | |
| Screening frequency | Substance 1 | Wilcoxon signed rank test | Yes | Z = 4.65 | <0.001 *** | – | – | – |
| Profession | χ2 | Yes | χ2(3) = 14.40 | 0.002 ** | – | – | – | |
| Age | Spearman | – | – | – | – | 0.08 (0.369) | – | |
| Knowledge | Spearman | – | – | – | – | 0.25 (0.003) | – | |
| Counseling frequency | Profession | χ2 | Yes | χ2(3) = 9.58 | 0.023 * | – | – | – |
| Age | Spearman, Regression | – | – | – | – | 0.19 (0.030) | 0.03 (0.705) | |
| Knowledge | Spearman, Regression | – | – | – | – | 0.43 (<0.001) | 0.42 (<0.001) |
Appendix B. Questionnaire
- What is your biological sex?
- ☐ Male☐ Female☐ Diverse☐ No statement
- What is your social gender?
- ☐ Cis (Gender identity corresponds to the sex assigned at birth)☐ Trans (Gender identity does not correspond to the sex assigned at birth)☐ No statement
- What is your age?
- ________ years
- What is your profession?
- ☐ Doctor☐ Midwife☐ Social worker☐ Psychologist☐ Social educator☐ Other: ___________________
- How many years have you been working in this profession?
- ________ years
- In which federal state do you live?
- ☐ Baden-Württemberg☐ Bavaria☐ Berlin☐ Brandenburg☐ Bremen☐ Hamburg☐ Hesse☐ Mecklenburg- Western Pomerania☐ Niedersachsen☐ Nordrhein-Westfalen☐ Rhineland-Palatinate☐ Saarland☐ Saxony-Anhalt☐ Saxony☐ Schleswig-Holstein☐ Thuringia☐ Outside of Germany
- Do you work in direct contact with pregnant women?
- ☐ Yes☐ No
- Do you only care for pregnant women during childbirth?
- ☐ Yes☐ No
- How many years have you been working in direct contact with pregnant women?
- ________ years
- In which context do you work with pregnant women?
- ☐ University Hospital☐ Hospital☐ Doctors office☐ Midwifery practice/birth center☐ Advice center☐ Other: ___________________________
- You stated that you work in a doctor’s office or midwifery practice/birth center:
- Are you self-employed or employed?
- ☐ Self-employed☐ Employed☐ No statement
- Was the topic of addiction/substance use (alcohol, smoking, e-cigarettes, cannabis and illegal substances) part of your training/studies?
- ☐ Yes☐ No
- If yes, please indicate the format in the comments (e.g., presentation, lecture, seminar, course).
- Comment: ___________________________________________________________
- You have stated that the topic of addiction/substance use was part of your education/studies:
- Was the topic of substance use (alcohol, smoking, e-cigarettes, cannabis and illegal substances) during pregnancy also addressed?
- ☐ Yes☐ No
- Have you ever participated in training on addiction/substance use (alcohol, smoking, e-cigarettes, cannabis and illegal substances)?
- ☐ Yes☐ No
- If yes, please indicate the training in the comments.
- Comment: ___________________________________________________________
- You have stated that you have participated in training courses on addiction/substance use (alcohol, smoking, e-cigarettes, cannabis and illegal substances):
- Was the topic of substance use (alcohol, smoking, e-cigarettes, cannabis and illegal substances) during pregnancy also addressed?
- ☐ Yes☐ No
- How often do you talk to pregnant women about alcohol consumption during pregnancy or ask about alcohol consumption during pregnancy?
- ☐ Always☐ Most of the time☐ Rarely☐ Never
- How many pregnant women do you treat/advise/care for in an average working week?
- ________ (Number)
- How many of these pregnant women do you talk to about alcohol consumption during pregnancy?
- ________ (Number)
- (Questions 15, 16 and 17 only appear if the value in question 14 is > 0)
- How long does the discussion about alcohol consumption usually last (per pregnant woman)?
- ________ Minutes
- How much time would you like to spend discussing alcohol consumption (per pregnant woman)?
- ________ MinutesDo you ask how much alcohol is consumed?☐ Yes, always☐ Yes, most of the time☐ Yes, rarely☐ No, never
- Do you use a screening questionnaire to assess alcohol consumption in pregnant women?
- ☐ Yes, I use: ____________________☐ No
- Do you ask pregnant women about their consumption habits (alcohol) before pregnancy?
- ☐ Yes, always☐ Yes, most of the time☐ Yes, rarely☐ No, never
- Do you ask women who are not pregnant about their alcohol consumption?
- ☐ Yes, always☐ Yes, most of the time☐ Yes, rarely☐ No, never
- How do you rate your current knowledge of the possible risks and consequences of consuming alcohol during pregnancy?
- No knowledge Very high knowledge☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10
- How do you assess your need for further training on possible risks and consequences of alcohol consumption during pregnancy?
- ☐ Very high ☐ High ☐ Low ☐ Very low ☐ No need
- How would you generally rate your personal communication skills in a professional context?
- ☐ Very good ☐ Good ☐ Satisfactorily ☐ Sufficiently
- How confident do you feel talking to pregnant women about alcohol during pregnancy?
- ☐ Confident☐ Rather confident☐ Rather not confident☐ Not confident☐ I don’t talk about that issue
- How do you assess your need for further training on communication strategies regarding alcohol consumption during pregnancy?
- ☐ Very high ☐ High ☐ Low ☐ Very low
- What do you consider the biggest obstacles in communicating with pregnant women about alcohol consumption? (multiple answers are possible)
- ☐ No time (insufficient time resources)☐ Concern that pregnant women feel prejudged☐ Concern that pregnant women feel ashamed☐ Worry about endangering/straining the relationship with the pregnant woman☐ Uncertainty about what to do if pregnant women report alcohol consumption☐ Insufficient knowledge regarding the consequences of alcohol consumption during pregnancy☐ Lack of confidence in one’s own communication skills when dealing with difficult topics☐ Doubts about the pregnant woman’s honesty (I don’t expect an honest answer)☐ I do not see it as my responsibility to address the issue☐ I think it is unnecessary to discuss alcohol consumption during pregnancy because so few women drink☐ Insufficient incentive in the healthcare system (no/low remuneration)☐ I don’t see any obstaclesOther: __________________________________________________________
- When do you inform pregnant women about the risks of alcohol consumption during pregnancy? (multiple answers are possible)
- ☐ At first contact☐ At follow-up appointments☐ If there are signs of addiction☐ When pregnant women ask for it☐ When pregnant women talk about consumption on their own☐ I do not inform about that issue
- What media do you use to provide information about alcohol consumption during pregnancy (multiple answers are possible)?
- ☐ Oral counseling☐ Posters/placards☐ Information brochures/flyers☐ Reference to video material☐ Reference to websites☐ Reference to online interventions☐ None☐ Other: _____________________________
- If you work in a facility, clinic, or practice with multiple professionals:
- Are there guidelines or agreements on how alcohol consumption during pregnancy is recorded and documented?
- ☐ Not answerable—I work independently/not in an institution☐ Yes, there are guidelines/agreements. They are as follows: _____________________☐ There are no guidelines/agreements
- Please give your personal estimate: What percentage of pregnant women in Germany consume alcohol at least occasionally?
- ________%
- Based on the clientele of your clinic/practice/counseling center–please estimate what percentage of pregnant women consume alcohol at least occasionally?
- ________%
- What do you think are the three most common reasons why pregnant women consume alcohol? (3 answers are possible)
- ☐ Beliefs about the supposedly safe or even health-promoting effects of alcohol (e.g., a glass of sparkling wine won’t do any harm)☐ Lack of knowledge about potential risks☐ Regular consumption before pregnancy is detected (despite a general desire for abstinence during pregnancy)☐ Ambiguous communication about risks in the institutional/social community☐ Emotion regulation/coping with stressful life circumstances/events☐ Enjoyment☐ Consumption at social events (e.g., birthdays/New Year’s Eve are impossible without a toast)☐ Maintaining autonomy and control over decisions/self-determination☐ Social environment and the associated pressure to consume☐ Regular consumption at social events to avoid having to disclose the pregnancy☐ Alcohol dependence☐ Other: ____________________________________________________________________
- Please rate the following statements on a scale from “strongly disagree” to “strongly agree”
| Strongly Agree | Agree | Disagree | Strongly Disagree | |
| The pregnant woman is responsible for maintaining abstinence during pregnancy. | ☐ | ☐ | ☐ | ☐ |
| I feel responsible for ensuring that pregnant women maintain abstinence. | ☐ | ☐ | ☐ | ☐ |
| It should be a given for pregnant women to abstain from alcohol. | ☐ | ☐ | ☐ | ☐ |
| Policymakers should ensure that pregnant women maintain abstinence. | ☐ | ☐ | ☐ | ☐ |
| Women who consume alcohol during pregnancy are fundamentally irresponsible. | ☐ | ☐ | ☐ | ☐ |
| Only women with alcohol addiction fail to remain abstinent during pregnancy. | ☐ | ☐ | ☐ | ☐ |
| The social environment should support pregnant women in maintaining abstinence during pregnancy. | ☐ | ☐ | ☐ | ☐ |
| Women who cannot/do not want to abstain completely from alcohol should not have children. | ☐ | ☐ | ☐ | ☐ |
| It can be challenging for women to abstain from alcohol during pregnancy, even if they are not addicted. | ☐ | ☐ | ☐ | ☐ |
| I get angry when women continue to consume alcohol during pregnancy. | ☐ | ☐ | ☐ | ☐ |
| Women who have consumed alcohol during pregnancy cannot responsibly care for children. | ☐ | ☐ | ☐ | ☐ |
| I can tell when a pregnant woman is consuming alcohol during pregnancy. | ☐ | ☐ | ☐ | ☐ |
| I understand that it is difficult for some pregnant women to remain abstinent. | ☐ | ☐ | ☐ | ☐ |
- Other substances
- How high do you estimate the health risk for the unborn child when consuming the following substances during pregnancy?
- AlcoholNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10SmokingNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10E-CigarettesNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10CannabisNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Opioids (e.g., Heroin)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Amphetamines (e.g., Speed)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Methamphetamines (e.g., Crystal meth)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10SugarNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Over-the-counter pregnancy vitamins in usual dosesNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10
- How high do you estimate the health risk for pregnant women when consuming the following substances during pregnancy?
- AlcoholNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10SmokingNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10E-CigarettesNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10CannabisNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Opioids (e.g., Heroin)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Amphetamines (e.g., Speed)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Methamphetamines (e.g., Crystal meth)No risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10SugarNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10Over-the-counter pregnancy vitamins in usual dosesNo risk Very high risk☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10
- How do you rate your knowledge of the possible risks and consequences of consuming the following substances during pregnancy?
- CigarettesNo knowledge Very high knowledge☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10E-CigarettesNo knowledge Very high knowledge☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10CannabisNo knowledge Very high knowledge☐ 0 ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 ☐ 6 ☐ 7 ☐ 8 ☐ 9 ☐ 10
- How much do you estimate your need for further training on the possible risks and consequences of the following substances when consumed during pregnancy?
- Cigarettes☐ Very high ☐ High ☐ Rather low ☐ LowE-Cigarettes☐ Very high ☐ High ☐ Rather low ☐ LowCannabis☐ Very high ☐ High ☐ Rather low ☐ Low
- Do you ask pregnant women about the consumption of the following substances?
- Cigarettes☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverE-Cigarettes☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverCannabis☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, never
- Do you advise pregnant women about the risks and consequences of consuming the following substances during pregnancy?
- Cigarettes☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverE-Cigarettes☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverCannabis☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverE-Cigarettes☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, neverCannabis☐ Yes, always ☐ Yes, most of the time ☐ Yes, rarely ☐ No, never
- Personal consumption:
- One glass of alcohol is equivalent to:0.33 L of beer0.25 L of wine or sparkling wine0.02 L of spirits
- How often do you consume one alcoholic drink?
- ☐ Never☐ About once a month☐ About 2–4 times a month☐ About 2–3 times a week☐ 4 times or more per week☐ No statement
- If you drink alcohol, how many alcoholic drinks do you typically consume?
- ☐ 1–2 ☐ 3–4 ☐ 5–6 ☐ 7–9 ☐ 10 or more ☐ No statement
- How often have you consumed more than 6 alcoholic drinks in one day?
- ☐ Never☐ Less than once per month☐ Once per month☐ Once per week☐ Daily or almost daily☐ No statement
- Do you smoke Cigarettes?
- ☐ Yes☐ No☐ No statement
- Do you consume E-Cigarettes?
- ☐ Yes☐ No☐ No statement
- Do you consume Cannabis?
- ☐ Yes☐ No☐ No statement
References
- Law on the Handling of Consumer Cannabis. 2024. Available online: https://www.gesetze-im-internet.de/kcang/BJNR06D0B0024.html (accessed on 30 May 2024).
- Chanal, C.; Mazurier, E.; Doray, B. Use of Psychoactive Substances during the Perinatal Period: Guidelines for Interventions during the Perinatal Period from the French National College of Midwives. J. Midwifery Womens Health 2022, 67, S17–S37. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.A.; Fonseca, B.M.; Marques, F.; Teixeira, N.A.; Correia-da-Silva, G. The psychoactive compound of Cannabis sativa, Δ9-tetrahydrocannabinol (THC) inhibits the human trophoblast cell turnover. Toxicology 2015, 334, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Gesterling, L.; Bradford, H. Cannabis Use in Pregnancy: A State of the Science Review. J. Midwifery Womens Health 2022, 67, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, J.; Schleußner, E. Die Effekte von legalen und illegalen Drogen auf die Plazentafunktion. In Die Plazenta; Huppertz, B., Schleußner, E., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 119–133. [Google Scholar]
- Ayonrinde, O.T.; Ayonrinde, O.A.; Van Rooyen, D.; Tait, R.; Dunn, M.; Mehta, S.; White, S.; Ayonrinde, O.K. Association between gestational cannabis exposure and maternal, perinatal, placental, and childhood outcomes. J. Dev. Orig. Health Dis. 2021, 12, 694–703. [Google Scholar] [CrossRef]
- Bouquet, E.; Blouin, P.; Pérault-Pochat, M.-C.; Carlier-Guérin, C.; Millot, F.; Ricco, J.B.; De Keizer, J.; Pain, S.; Guétarni, F. Maternal, Fetal and Neonatal Outcomes Related to Recreational Cannabis Use during Pregnancy: Analysis of a Real-World Clinical Data Warehouse between 2010 and 2019. Int. J. Environ. Res. Public Health 2023, 20, 6686. [Google Scholar] [CrossRef]
- Gunn, J.K.L.; Rosales, C.B.; Center, K.E.; Nuñez, A.; Gibson, S.J.; Christ, C.; Ehiri, J.E. Prenatal exposure to cannabis and maternal and child health outcomes: A systematic review and meta-analysis. BMJ Open 2016, 6, e009986. [Google Scholar] [CrossRef]
- Ainiti, D.-F.; Lykeridou, A.; Nanou, C.; Deltsidou, A. Cannabis use during pregnancy and its effect on the fetus, newborn and later childhood: A systematic review. Eur. J. Midwifery 2023, 7, 19. [Google Scholar] [CrossRef]
- Gerede, A.; Stavros, S.; Chatzakis, C.; Vavoulidis, E.; Papasozomenou, P.; Domali, E.; Nikolettos, K.; Oikonomou, E.; Potiris, A.; Tsikouras, P.; et al. Cannabis Use during Pregnancy: An Update. Medicina 2024, 60, 1691. [Google Scholar] [CrossRef]
- Marroun, H.E.; Hudziak, J.J.; Tiemeier, H.; Creemers, H.; Steegers, E.A.; Jaddoe, V.W.; Hofman, A.; Verhulst, F.C.; van den Brink, W.; Huizink, A.C. Intrauterine cannabis exposure leads to more aggressive behavior and attention problems in 18-month-old girls. Drug Alcohol Depend. 2011, 118, 470–474. [Google Scholar] [CrossRef]
- Badowski, S.; Smith, G. Cannabis use during pregnancy and postpartum. Can. Fam. Physician 2020, 66, 98–103. [Google Scholar]
- Conner, S.N.; Bedell, V.; Lipsey, K.; Macones, G.A.; Cahill, A.G.; Tuuli, M.G. Maternal Marijuana Use and Adverse Neonatal Outcomes: A Systematic Review and Meta-analysis. Obstet. Gynecol. 2016, 128, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, T.M.; Feng, E.; Vahedi, F.; Ermolina, S.; Bellissimo, C.J.; De Jong, E.; Portillo, A.L.; Poznanski, S.M.; Chan, L.; Ettehadieh, S.M.; et al. The impact of oral cannabis consumption during pregnancy on maternal spiral artery remodelling, fetal growth and offspring behaviour in mice. eBioMedicine 2025, 114, 105572. [Google Scholar] [CrossRef] [PubMed]
- Metz, T.D.; Borgelt, L.M. Marijuana Use in Pregnancy and While Breastfeeding. Obstet. Gynecol. 2018, 132, 1198–1210. [Google Scholar] [CrossRef]
- Schauberger, C.W.; Newbury, E.J.; Colburn, J.M.; Al-Hamadani, M. Prevalence of illicit drug use in pregnant women in a Wisconsin private practice setting. Am. J. Obstet. Gynecol. 2014, 211, 255.e1–255.e4. [Google Scholar] [CrossRef] [PubMed]
- Warner, T.D.; Roussos-Ross, D.; Behnke, M. It’s Not Your Mother’s Marijuana: Effects on maternal-fetal health and the developing child. Clin. Perinatol. 2014, 41, 877–894. [Google Scholar] [CrossRef]
- Cinelli, H.; Lelong, N.; Le Ray, C. French National Perinatal Survey 2021: Births, 2-Month Follow-Up and Establishments. Situation and Trends since 2016; Inserm: Paris, France, 2022. [Google Scholar]
- Olderbak, S.; Möckl, J.; Manthey, J.; Lee, S.; Rehm, J.; Hoch, E.; Kraus, L. Trends and projection in the proportion of (heavy) cannabis use in Germany from 1995 to 2021. Addiction 2024, 119, 311–321. [Google Scholar] [CrossRef]
- Orth, B.; Merkel, C. Der Substanzkonsum Jugendlicher und Junger Erwachsener in Deutschland. Ergebnisse des Alkoholsurveys 2021 zu Alkohol, Rauchen, Cannabis und Trends; Bundeszentrale für Gesundheitliche Aufklärung: Köln, Germany, 2022. [Google Scholar]
- Mark, K.; Gryczynski, J.; Axenfeld, E.; Schwartz, R.P.; Terplan, M. Pregnant Women’s Current and Intended Cannabis Use in Relation to Their Views Toward Legalization and Knowledge of Potential Harm. J. Addict. Med. 2017, 11, 211–216. [Google Scholar] [CrossRef]
- Gould, E.E.; Ganesh, S.S.; Nguyen, R.M.; Breton, C.V.; Bastain, T.M.; Dunton, G.F.; Ceasar, R.C. The unseen patient: Competing priorities between patients and providers when cannabis is used in pregnancy, a qualitative study. Front. Glob. Womens Health 2024, 5, 1355375. [Google Scholar] [CrossRef]
- Vanstone, M.; Taneja, S.; Popoola, A.; Panday, J.; Greyson, D.; Lennox, R.; McDonald, S.D. Reasons for cannabis use during pregnancy and lactation: A qualitative study. Can. Med. Assoc. J. 2021, 193, E1906–E1914. [Google Scholar] [CrossRef]
- Young-Wolff, K.C.; Foti, T.R.; Green, A.; Altschuler, A.; Does, M.B.; Jackson-Morris, M.; Adams, S.R.; Ansley, D.; Conway, A.; Goler, N.; et al. Perceptions About Cannabis Following Legalization Among Pregnant Individuals with Prenatal Cannabis Use in California. JAMA Netw. Open 2022, 5, e2246912. [Google Scholar] [CrossRef]
- Lamy, S.; Thibaut, F. Psychoactive substance use during pregnancy: A review. Encephale 2010, 36, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Benoit, C.; Magnus, S.; Phillips, R.; Marcellus, L.; Charbonneau, S. Complicating the dominant morality discourse: Mothers and fathers’ constructions of substance use during pregnancy and early parenthood. Int. J. Equity Health 2015, 14, 72. [Google Scholar] [CrossRef] [PubMed]
- Gould, E.E.; Ganesh, S.S.; Ceasar, R.C. “I don’t need my kid to be high”: Prioritizing harm reduction when using cannabis during pregnancy. Harm Reduct. J. 2024, 21, 166. [Google Scholar] [CrossRef] [PubMed]
- Egelkraut, R.; Ensel, A.; Erdmann, D.; Friese-Berg, S.; Krauspenhaar, D.; Kruid, A.; Lange, U.; Lohmann, S.; Rauer-Sell, M.; Schäfers, R.; et al. Schwangerenvorsorge durch Hebammen, 4th ed.; Georg Thieme Verlag KG: Stuttgart, Germany, 2023. [Google Scholar]
- Gérardin, M.; Victorri-Vigneau, C.; Louvigné, C.; Rivoal, M.; Jolliet, P. Management of cannabis use during pregnancy: An assessment of healthcare professionals’ practices. Pharmacoepidemiol. Drug Saf. 2011, 20, 464–473. [Google Scholar] [CrossRef]
- Ceasar, R.C.; Gould, E.; Stal, J.; Laughter, J.; Tran, M.; Wang, S.D.; Granacki, J.; Ziltzer, R.S.; Santos, J.J. Legislation has Changed but Issues Remain: Provider Perceptions of Caring for People Who Use Cannabis During Pregnancy in Safety Net Health Settings, a Qualitative Pilot Study. Womens Health Rep. 2023, 4, 400–408. [Google Scholar] [CrossRef]
- Panday, J.; Taneja, S.; Popoola, A.; Pack, R.; Greyson, D.; McDonald, S.D.; Black, M.; Murray-Davis, B.; Darling, E.; Vanstone, M. Clinician responses to cannabis use during pregnancy and lactation: A systematic review and integrative mixed-methods research synthesis. Fam. Pract. 2022, 39, 504–514. [Google Scholar] [CrossRef]
- Forray, A. Substance use during pregnancy. F1000Res 2016, 5, 887. [Google Scholar] [CrossRef]
- Schendera, C.F. Datenqualität mit SPSS, 1st ed.; Oldenbourg Wissenschaftsverlag: München, Germany, 2007. [Google Scholar]
- Döring, N. Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften, 6th ed.; Springer: Berlin/Heidelberg, Germany, 2023. [Google Scholar]
- LimeSurvey GmbH. LimeSurvey: An Open-Source Survey Tool. 2024. Available online: https://www.limesurvey.org/de (accessed on 15 May 2025).
- Deutscher Hebammenverband. Wie Arbeiten Hebammen? Available online: https://hebammenverband.de/hebamme-werden-und-sein/wie-arbeiten-hebammen (accessed on 11 April 2025).
- Verbund Hebammenforschung. Neue Perspektiven Entwickeln—Hebammen Stellen Ihre Arbeit Dar. Ergebnisse einer Bestandsaufnahme der Versorgungsleistungen durch Hebammen in Niedersachsen im Jahr 2007; Verbund Hebammenforschung: Osnabrück, Germany, 2009; Available online: https://www.hebammenforschung.de/fileadmin/HSOS/Homepages/Hebammenforschung/Ergebnisse_Bestandsaufnahme.pdf (accessed on 15 May 2025).
- Richter-Kuhlmann, E. Tobias Richter: Männliche Hebamme wirbt für Diversität im Beruf. Dtsch. Arztebl. 2023, 120, 891. [Google Scholar]
| Variable | Type/Scale | Coding/Range | Statistical Tests Applied |
|---|---|---|---|
| Profession | Categorical (nominal) | Midwife, Physician | χ2-test, t-test |
| Age | Continuous (metric) | Years | Spearman correlation, regression |
| Years of professional experience | Continuous (metric) | Years | Not used (strongly correlated with age: ρ = 0.94, p < 0.001) |
| Addiction/substance use was part of the professional training | Categorical (nominal) | Yes, No | χ2-test, t-test, regression |
| Attended further training on addiction/substance | Categorical (nominal) | Yes, No | χ2-test, t-test, regression |
| Self-rated knowledge | Ordinal/ Interval | 0 = no knowledge to 10 = very high knowledge | t-test, Spearman correlation, regression |
| Risk perception (child) | Ordinal/ Interval | 0 = no risk to 10 = very high risk | t-test, Wilcoxon signed-rank, Spearman correlation, regression |
| Risk perception (pregnant person) | Ordinal/ Interval | 0 = no risk to 10 = very high risk | t-test, Wilcoxon signed-rank, Spearman correlation, regression |
| Screening frequency | Ordinal (4-point) | 1 = never, 4 = always | χ2-test, Wilcoxon signed-rank test, Spearman correlation, regression |
| Counseling frequency | Ordinal (4-point) | 1 = never, 4 = always | χ2-test, Spearman correlation, regression |
| Characteristic | Midwives (n = 143) | Physicians (n = 141) | Total (N = 284) |
|---|---|---|---|
| Age (years), M (SD) 1 | 38.8 (11.6) | 45.9 (10.3) | 42.3 (11.4) |
| Biological sex, n (%) | |||
| Male | 1 (0.7%) | 12 (8.5%) | 13 (4.6%) |
| Female | 142 (99.3%) | 129 (91.5%) | 271 (95.4%) |
| Divers | – | – | – |
| No statement | 7 (4.9%) | 3 (2.1%) | 10 (3.5%) |
| Social gender, n (%) | |||
| Cis | 136 (95.1%) | 138 (97.9%) | 274 (96.5%) |
| Trans | 2 (1.4%) | 2 (0.7%) | |
| No statement | 5 (3.5%) | 3 (2.1%) | 8 (2.8%) |
| Personal cannabis consumption | |||
| Yes | 9 (6.3%) | 4 (2.8%) | 13 (4.6%) |
| No | 133 (93.0%) | 137 (97.2%) | 270 (95.1%) |
| No statement | 1 (0.7%) | – | 1 (0.4%) |
| Work experience (years), M (SD) | 14.3 (11.8) | 18.5 (10.2) | 16.4 (11.1) |
| Work context | |||
| University hospital | 10 (7%) | 23 (16.3%) | 33 (11.6%) |
| Hospital | 43 (30.1%) | 20 (14.2%) | 63 (22.2%) |
| Doctor’s office | 5 (3.5%) | 92 (65.2%) | 97 (34.2%) |
| Midwifery practice/birth center/self-employed | 78 (54.5%) | – | 78 (27.5%) |
| Advice center | 1 (0.7%) | 2 (1.4%) | 3 (1.1%) |
| Other | 6 (4.2%) | 4 (2.8%) | 10 (3.5%) |
| Addiction/substance use was part of the professional training | |||
| Yes | 112 (78.3%) | 92 (65.2%) | 204 (71.8%) |
| No | 31 (21.7%) | 49 (34.8%) | 80 (28.2%) |
| Attended further training on addiction/substance | |||
| Yes | 51 (35.7%) | 49 (34.8%) | 100 (35.2%) |
| No | 92 (64.3%) | 92 (65.2%) | 184 (64.8%) |
| Frequency | Screening (%) | Counseling (%) |
|---|---|---|
| Never (1) | 30 (21.0%) | 50 (35.0%) |
| Rarely (2) | 30 (21.0%) | 38 (26.6%) |
| Mostly (3) | 26 (18.2%) | 24 (16.8%) |
| Always (4) | 57 (39.9%) | 31 (21.7%) |
| Mean (SD) | 2.77 (1.19) | 2.08 (1.15) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wollscheid, J.; Burke, M.; Kimmel, T.; Kaufmann, T.; Batra, A.; Binder, A. Pregnancy Care in Times of Cannabis Legalization: Self-Rated Knowledge, Risk Perception and Communication Practices of Midwives in Germany. Healthcare 2025, 13, 1228. https://doi.org/10.3390/healthcare13111228
Wollscheid J, Burke M, Kimmel T, Kaufmann T, Batra A, Binder A. Pregnancy Care in Times of Cannabis Legalization: Self-Rated Knowledge, Risk Perception and Communication Practices of Midwives in Germany. Healthcare. 2025; 13(11):1228. https://doi.org/10.3390/healthcare13111228
Chicago/Turabian StyleWollscheid, Julia, Matthias Burke, Theresa Kimmel, Tobias Kaufmann, Anil Batra, and Annette Binder. 2025. "Pregnancy Care in Times of Cannabis Legalization: Self-Rated Knowledge, Risk Perception and Communication Practices of Midwives in Germany" Healthcare 13, no. 11: 1228. https://doi.org/10.3390/healthcare13111228
APA StyleWollscheid, J., Burke, M., Kimmel, T., Kaufmann, T., Batra, A., & Binder, A. (2025). Pregnancy Care in Times of Cannabis Legalization: Self-Rated Knowledge, Risk Perception and Communication Practices of Midwives in Germany. Healthcare, 13(11), 1228. https://doi.org/10.3390/healthcare13111228







