Determinants of Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
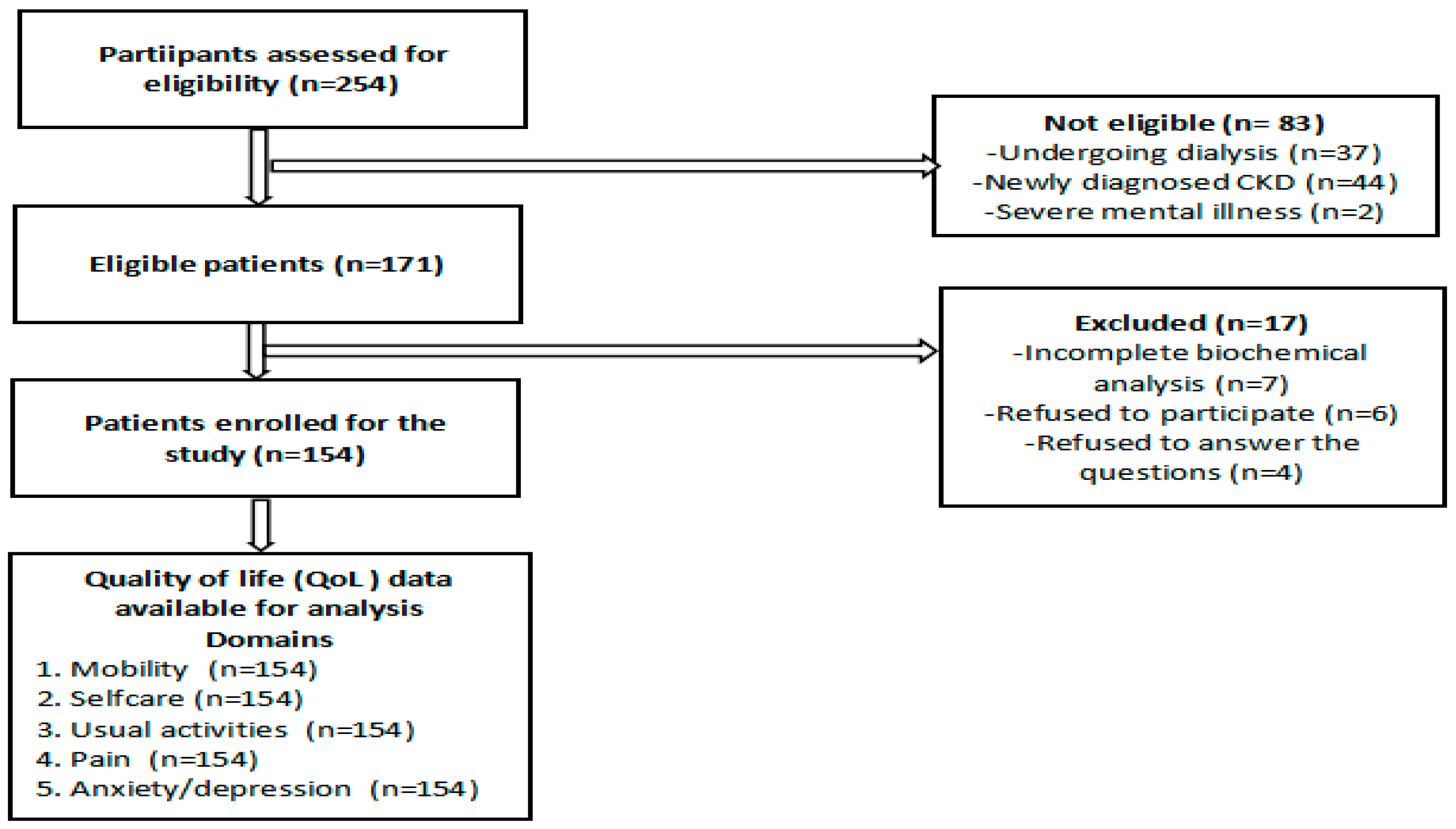
2.2. Population Size and Population Criteria
2.3. Data Collection Procedure
2.4. EQ-5D-3L
2.5. Ethical Approval
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2024, 105, S117–S314. [Google Scholar] [CrossRef] [PubMed]
- Stanifer, J.W.; Muiru, A.; Jafar, T.H.; Patel, U.D. Chronic kidney disease in low- and middle-income countries. Nephrol Dial. Transplant. 2016, 31, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Okoye, O.C.; Carnegie, E.; Mora, L. Air pollution-associated chronic kidney disease (APA-CKD): Evidence from a cross-sectional study of Niger Delta communities. BMJ Open 2025, 15, e096336. [Google Scholar] [CrossRef]
- Muiru, A.N.; Charlebois, E.D.; Balzer, L.B.; Kwarisiima, D.; Elly, A.; Black, D.; Okiror, S.; Kabami, J.; Atukunda, M.; Snyman, K.; et al. The epidemiology of chronic kidney disease (CKD) in rural East Africa: A population-based study. PLoS ONE 2020, 15, e0229649. [Google Scholar] [CrossRef]
- Singh, A.K.; Farag, Y.M.; Mittal, B.V.; Subramanian, K.K.; Reddy, S.R.K.; Acharya, V.N.; Almeida, A.F.; Channakeshavamurthy, A.; Ballal, H.S.; Gaccione, P.; et al. Epidemiology and risk factors of chronic kidney disease in India—Results from the SEEK (Screening and Early Evaluation of Kidney Disease) study. BMC Nephrol. 2013, 14, 114. [Google Scholar] [CrossRef]
- Whoqol Group. The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Trifirò, G.; Sultana, J.; Giorgianni, F.; Ingrasciotta, Y.; Buemi, M.; Muscianisi, M.; Tari, D.U.; Perrotta, M.; Canale, V.; Arcoraci, V.; et al. Chronic kidney disease requiring healthcare service: A new approach to evaluate epidemiology of renal disease. BioMed Res. Int. 2014, 2014, 268362. [Google Scholar] [CrossRef]
- Boudreau, J.E.; Dube, A. Quality of life in end stage renal disease: A concept analysis. CANNT J. 2014, 24, 12–20. [Google Scholar]
- Karimi, M.; Brazier, J. Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Hussien, H.; Apetrii, M.; Covic, A. Health-related quality of life in patients with chronic kidney disease. Expert Rev. Pharmacoeconomics Outcomes Res. 2020, 21, 43–54. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Unruh, M. Health related quality of life in patients with chronic kidney disease. Int. Urol. Nephrol. 2005, 37, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Kefale, B.; Alebachew, M.; Tadesse, Y.; Engidawork, E. Quality of life and its predictors among patients with chronic kidney disease: A hospital-based cross sectional study. PLoS ONE 2019, 14, e0212184. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Kumar, P.; Ansari, J.A.; Fatima, M.; Irrum, F. A prospective observational study on medication usage pattern in patients risk factors of chronic kidney disease. Asian J. Pharm. Clin. Res. 2021, 14, 144–148. [Google Scholar] [CrossRef]
- Ahlawat, R.; D’cruz, S.; Tiwari, P. Drug utilization pattern in chronic kidney disease patients at a tertiary care public teaching hospital: Evidence from a cross-sectional study. J. Pharm. Care Health Syst. 2015, 3, 1–5. [Google Scholar] [CrossRef]
- Sharma, S.; Kalra, D.; Rashid, I.; Mehta, S.; Maity, M.K.; Wazir, K.; Gupta, S.; Ansari, S.A.; Alruqi, O.S.; Khan, R.; et al. Assessment of Health-Related Quality of Life in Chronic Kidney Disease Patients: A Hospital-Based Cross-Sectional Study. Medicina 2023, 59, 1788. [Google Scholar] [CrossRef]
- Manju, L.; Joseph, J. Health-related quality of life among patients undergoing hemodialysis in a tertiary center in South Kerala. Clin. Epidemiol. Glob. Health 2023, 26, 101547. [Google Scholar] [CrossRef]
- Kharshid, A.M.; Sulaiman, S.A.S.; Saadh, M.J. Health-Related Quality of Life in Chronic Kidney Disease Patients: A Cross-Sectional Study. Syst. Rev. Pharm. 2020, 11, 188–192. [Google Scholar]
- EuroQol Group. EuroQol a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Kampmann, J.D.; Heaf, J.G.; Mogensen, C.B.; Mickley, H.; Wolff, D.L.; Brandt, F. Prevalence and incidence of chronic kidney disease stage 3-5-results from KidDiCo. BMC Nephrol. 2023, 24, 17. [Google Scholar] [CrossRef]
- Dehghani, A.; Alishavandi, S.; Nourimajalan, N.; Fallahzadeh, H.; Rahmanian, V. Prevalence of chronic kidney diseases and its determinants among Iranian adults: Results of the first phase of Shahedieh cohort study. BMC Nephrol. 2022, 23, 203. [Google Scholar] [CrossRef] [PubMed]
- Weldegiorgis, M.; Woodward, M. The impact of hypertension on chronic kidney disease and end-stage renal disease is greater in men than women: A systematic review and meta-analysis. BMC Nephrol. 2020, 21, 506, Erratum in BMC Nephrol. 2020, 21, 545. https://doi.org/10.1186/s12882-020-02199-5. [Google Scholar] [CrossRef]
- Tang, Y.; Jiang, J.; Zhao, Y.; Du, D. Aging and chronic kidney disease: Epidemiology, therapy, management and the role of immunity. Clin. Kidney J. 2024, 17, sfae235. [Google Scholar] [CrossRef] [PubMed]
- Kazancioğlu, R. Risk factors for chronic kidney disease: An update. Kidney Int. Suppl. 2013, 3, 368–371. [Google Scholar] [CrossRef]
- Habas, E., Sr.; Habas, E.; Khan, F.Y.; Rayani, A.; Habas, A.; Errayes, M.; Farfar, K.L.; Elzouki, A.N. Blood Pressure and Chronic Kidney Disease Progression: An Updated Review. Cureus 2022, 14, e24244. [Google Scholar] [CrossRef]
- Nagahama, A.M.; Silva, V.D.; Banin, V.B.; Franco, R.J.; Barretti, P.; Bazan, S.G.; Martin, L.C. Association between chronic kidney disease stages and changes in ambulatory blood pressure monitoring parameters. J. Bras. Nefrol. 2024, 46, e20230066. [Google Scholar] [CrossRef]
- Theodorakopoulou, M.; Ortiz, A.; Fernandez-Fernandez, B.; Kanbay, M.; Minutolo, R.; Sarafidis, P.A. Guidelines for the management of hypertension in CKD patients: Where do we stand in 2024? Clin. Kidney J. 2024, 17 (Suppl 2), 36–50. [Google Scholar] [CrossRef]
- Krishnan, A.; Teixeira-Pinto, A.; Lim, W.H.; Howard, K.; Chapman, J.R.; Castells, A.; Roger, S.D.; Bourke, M.J.; Macaskill, P.; Williams, G.; et al. Health-Related Quality of Life in People Across the Spectrum of CKD. Kidney Int. Rep. 2020, 5, 2264–2274. [Google Scholar] [CrossRef]
- Gerasimoula, K.; Lefkothea, L.; Maria, L.; Victoria, A.; Paraskevi, T.; Maria, P. Quality of life in hemodialysis patients. Mater. Sociomed. 2015, 27, 305–309. [Google Scholar] [CrossRef]
- Subramani, T.; Kunchithapatham, S.; Ismail, S.C. Evaluation of Health-related Quality of Life among Hypertensive Post-menopausal Women Using EQ-5D in India During COVID-19 Pandemic. Indian J. Pharm. Educ. Res. 2022, 56, 1232–1239. [Google Scholar] [CrossRef]
- Wyld, M.L.R.; Morton, R.L.; Clayton, P. The impact of progressive chronic kidney disease on health-related quality-of-life: A 12-year community cohort study. Qual. Life Res. 2019, 28, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Cruz, M.C.; Andrade, C.; Urrutia, M.; Draibe, S.; Nogueira-Martins, L.A.; Sesso Rde, C. Quality of life in patients with chronic kidney disease. Clinics 2011, 66, 991–995. [Google Scholar] [CrossRef]
- Mahato, S.K.; Apidechkul, T.; Sriwongpan, P.; Hada, R.; Sharma, G.N.; Nayak, S.K.; Mahato, R.K. Factors associated with quality of life among chronic kidney disease patients in Nepal: A cross-sectional study. Health Qual. Life Outcomes 2020, 18, 207. [Google Scholar] [CrossRef] [PubMed]
- Al Salmi, I.; Kamble, P.; Lazarus, E.R.; D’Souza, M.S.; Al Maimani, Y.; Hannawi, S. Kidney Disease-Specific Quality of Life among Patients on Hemodialysis. Int. J. Nephrol. 2021, 2021, 8876559. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.A.; Collett, G.K.; Josland, E.A.; Foote, C.; Li, Q.; Brennan, F.P. CKD in elderly patients managed without dialysis: Survival, symptoms, and quality of life. Clin. J. Am. Soc. Nephrol. 2015, 10, 260–268. [Google Scholar] [CrossRef]
- Chung, Y.K.; Lim, J.H.; Jeon, Y.N.; Jeon, Y.H.; Jung, H.Y.; Choi, J.Y.; Park, S.H.; Kim, C.D.; Kim, Y.L.; Cho, J.H. The impact of quality of life on the survival of elderly patients with end-stage renal disease: A prospective multicenter cohort study in Korea. Clin. Kidney J. 2024, 17, sfae241. [Google Scholar] [CrossRef]
- Kalsoom, U. Gender role in anxiety, depression and quality of life in chronic kidney disease patients. Pak. J. Med. Sci. 2020, 36, 251–254. [Google Scholar] [CrossRef]
- Brandt, L.; Liu, S.; Heim, C.; Heinz, A. The effects of social isolation stress and discrimination on mental health. Transl. Psychiatry 2022, 12, 398. [Google Scholar] [CrossRef]
- Nambisan, P.; Gustafson, D.H.; Hawkins, R.; Pingree, S. Social support and responsiveness in online patient communities: Impact on service quality perceptions. Health Expect. 2016, 19, 87–97. [Google Scholar] [CrossRef]
- Chen, Y.R.; Schulz, P.J. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. J. Med. Internet Res. 2016, 18, e18. [Google Scholar] [CrossRef]
- Manavalan, M.; Majumdar, A.; Kumar, K.T.H.; Priyamvada, P.S. Assessment of health related quality of life and its determinants in patients with chronic kidney disease. Indian J. Nephrol. 2017, 27, 37–43. [Google Scholar] [PubMed]
- Vo, T.Q.; Tran, T.Q.; Duong, K.; Pham, C.K. Impact of chronic kidney disease on health-related quality of life: A prospective observational study using the Kdqol-36 instrument public health section. J. Clin. Diagn. Res. 2018, 12, LC66-71. [Google Scholar]
- Bay, S.S.; Kamaruzaman, L.; Mohd, R.; Azhar Shah, S. Work disability and employment status among advanced chronic kidney disease patients. PLoS ONE 2024, 19, e0297378. [Google Scholar] [CrossRef]
- Eswarappa, M.; Anish, L.S.; Prabhu, P.P.; Chennabasappa, G.K.; Gireesh, M.S.; Rajashekar, Y.M.; Gangula, R.S. Health-related quality of life of patients with chronic kidney disease on maintenance hemodialysis and its determinants: A study from a tertiary hospital in South India. Turk. J. Nephrol. 2024, 33, 279–288. [Google Scholar] [CrossRef]
- Berhe, T.; Tegegne, G.T.; Berha, A.B. Quality of life and associated factors among chronic kidney disease patients at Zewditu Memorial and Tikur Anbessa Specialised Hospitals, Ethiopia: A cross-sectional study design. BMJ Open 2023, 13, e069712. [Google Scholar] [CrossRef]
- Porter, A.C.; Lash, J.P.; Xie, D.; Pan, Q.; DeLuca, J.; Kanthety, R.; Kusek, J.W.; Lora, C.M.; Nessel, L.; Ricardo, A.C.; et al. Predictors and outcomes of health-related quality of life in adults with CKD. Clin. J. Am. Soc. Nephrol. 2016, 11, 1154–1162. [Google Scholar] [CrossRef]
- Zhou, X.; Xue, F.; Wang, H.; Qiao, Y.; Liu, G.; Huang, L.; Li, D.; Wang, S.; Wang, Q.; Li, L.; et al. The quality of life and associated factors in patienst on maintenance hemodialysis-a multcenter study in Shanxi province. J. Ren. Fail. 2017, 39, 707–711. [Google Scholar] [CrossRef]
- Fraser, S.D.; Barker, J.; Roderick, P.J.; Yuen, H.M.; Shardlow, A.; Morris, J.E.; McIntyre, N.J.; Fluck, R.J.; McIntyre, C.W.; Taal, M.W. Health-related quality of life, functional impairment and comorbidity in people with mild-to-moderate chronic kidney disease: A cross-sectional study. BMJ Open 2020, 10, e040286. [Google Scholar] [CrossRef]
- Tonelli, M.; Wiebe, N.; Guthrie, B.; James, M.T.; Quan, H.; Fortin, M.; Klarenbach, S.W.; Sargious, P.; Straus, S.; Lewanczuk, R.; et al. Comorbidity as a driver of adverse outcomes in people with chronic kidney disease. Kidney Int. 2015, 88, 859–866. [Google Scholar] [CrossRef]
| Variables | Category | Stage 3 CKD (n = 62) | Stage 4 CKD (n = 63) | Stage 5 CKD (n = 29) | p-Value |
|---|---|---|---|---|---|
| Gender | Male | 42 (67.7) | 45 (71.4) | 19 (65.52) | 0.82 |
| Female | 20 (32.3) | 18 (28.6) | 10 (34.48) | ||
| Age in years | ≤50 years | 6 (9.7) | 4 (6.3) | 3 (10.34) | 0.73 |
| >50 years | 56 (90.3) | 59 (93.7) | 26 (89.66) | ||
| Residence | Rural | 37 (59.7) | 43 (68.3) | 18 (62.07) | 0.59 |
| Urban | 25 (40.3) | 20 (31.7) | 11 (37.93) | ||
| Educational status | Illiterate | 22 (35.5) | 21 (33.8) | 8 (27.59) | 0.78 |
| Primary | 35 (56.5) | 33 (52.4) | 17 (58.62) | ||
| Secondary/Degree | 5 (8.1) | 9 (14.3) | 4 (13.79) | ||
| Employment status | Employed | 25 (40.3) | 18 (28.6) | 9 (31.03) | 0.35 |
| Unemployed/retired/Housewife | 37 (59.7) | 45 (71.4) | 20 (68.97) | ||
| Marital Status | Married | 58 (93.5) | 55 (87.3) | 27 (93.10) | 0.43 |
| Unmarried/widowed | 4 (6.5) | 8 (12.7) | 2 (6.90) | ||
| Smoking | Yes | 7 (11.3) | 12 (19) | 5 (17.24) | 0.47 |
| No | 55 (88.7) | 51(81) | 24 (82.76) | ||
| Alcohol intake | Yes | 5 (8.1) | 1(1.6) | 1 (3.45) | 0.21 |
| No | 57 (91.9) | 62 (98.4) | 28 (96.55) | ||
| Social support | Yes | 9 (14.5) | 14 (22.2) | 07 (24.14) | 0.43 |
| No | 53 (85.5) | 49 (77.8) | 22 (75.86) |
| Variables | Stage 3 CKD (n = 62) | Stage 4 CKD (n = 63) | Stage 5 CKD (n = 29) | p-Value |
|---|---|---|---|---|
| Blood Pressure | 0.015 * | |||
| Normal/Prehypertension | 42 (67.74) | 27 (42.86) | 18 (62.07) | |
| Stage 1/Stage 2 | 20 (32.26) | 36 (57.14) | 11 (37.93) | |
| Number of comorbidities | 0.0001 * | |||
| 1 | 29 (46.77) | 25 (39.68) | 3 (10.34) | |
| 2 | 23 (37.10) | 17 (26.98) | 7 (24.14) | |
| ≥3 | 8 (12.90) | 11 (17.46) | 14 (48.28) | |
| Nil | 2 (3.23) | 10 (15.87) | 5 (17.24) | |
| Specific comorbidities | ||||
| Diabetes Mellitus | 0.001 * | |||
| Yes | 8 (12.90) | 19 (30.16) | 18 (62.07) | |
| No | 54 (87.10) | 44 (69.84) | 11 (37.93) | |
| Hypertension | 0.169 | |||
| Yes | 34 (54.84) | 41 (65.08) | 13 (44.83) | |
| No | 28 (45.16) | 22 (34.92) | 16 (55.17) | |
| Dyslipidemia | 0.688 | |||
| Yes | 14 (22.58) | 16 (25.40) | 9 (31.03) | |
| No | 48 (77.42) | 47 (74.60) | 20 (68.97) | |
| CAD | 0.00007 * | |||
| Yes | 15 (24.19) | 8 (12.70) | 16 (55.17) | |
| No | 47 (75.81) | 55 (87.30) | 13 (44.83) | |
| Others | 0.002 * | |||
| Yes | 40 (64.52) | 21 (33.33) | 13 (44.83) | |
| No | 22 (35.48) | 42 (66.67) | 16 (55.17) | |
| GFR (mL/min/1.73 m2) | 49.16 ± 7.59 | 22.37 ± 3.88 | 8.79 ± 1.68 | <0.05 * |
| Hb (gm/dL) | 10.45 ± 0.84 | 8.88 ± 0.60 | 7.12 ± 0.53 | <0.001 * |
| Serum Creatinine (mg/dL) | 1.72 ± 0.40 | 3.21 ± 0.44 | 7.05 ± 1.46 | <0.001 * |
| Dimension | Level | Stage 3 (n = 62) | Stage 4 (n = 63) | Stage 5 (n = 29) | p-Value |
|---|---|---|---|---|---|
| Mobility | 1 | 38 (61.2) | 25 (39.6) | 06 (20.6) | 0.0003 * |
| 2 | 23 (37.0) | 37 (58.7) | 19 (65.5) | ||
| 3 | 1 (1.6) | 1 (1.6) | 4 (13.7) | ||
| Selfcare | 1 | 48 (77.4) | 34 (53.9) | 9 (31.03) | 0.001 * |
| 2 | 13 (20.9) | 27 (42.2) | 3 (10.3) | ||
| 3 | 1 (1.6) | 2 (3.1) | 17 (58.6) | ||
| Usual activities | 1 | 24 (39.7) | 28 (44.4) | 8 (27.5) | 0.001 * |
| 2 | 37 (59.6) | 33 (52.3) | 3 (10.3) | ||
| 3 | 1 (1.6) | 2 (3.1) | 18 (62.0) | ||
| Pain/Discomfort | 1 | 35 (58.4) | 20 (31.7) | 6 (20.6) | 0.001 * |
| 2 | 26 (41.9) | 35 (55.5) | 6 (20.6) | ||
| 3 | 1 (1.6) | 8 (12.6) | 17 (58.6) | ||
| Anxiety/depression | 1 | 41 (66.1) | 30 (47.6) | 7 (24.1) | 0.0005 * |
| 2 | 20 (32.2) | 29 (46.0) | 16 (55.1) | ||
| 3 | 1 (1.6) | 4 (6.34) | 6 (20.6) |
| Parameters | Mobility | Self-Care | Usual Activities | Pain | Anxiety/Depression | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR Ratio | CI | p Value | OR ratio | CI | p Value | OR Ratio | CI | p Value | OR Ratio | CI | p Value | OR Ratio | CI | p Value | |
| Gender | |||||||||||||||
| Male (n = 106) | Reference | ||||||||||||||
| Female (n = 48) | 1.45 | 1.12–1.87 | 0.002 | 1.32 | 1.01–1.74 | 0.045 | 1.28 | 1.02–1.61 | 0.038 | 1.41 | 1.10–1.81 | 0.005 | 1.38 | 1.09–1.74 | 0.009 |
| Age group | |||||||||||||||
| <50 years (n = 13) | Reference | ||||||||||||||
| ≥50years (n = 141) | 2.12 | 1.56-2.89 | <0.001 | 1.95 | 1.45–2.61 | <0.001 | 2.07 | 1.53–2.81 | <0.001 | 1.88 | 1.41–2.52 | <0.001 | 1.92 | 1.44–2.55 | <0.001 |
| Education | |||||||||||||||
| Illiterate (n = 51) | 1.89 | 1.42–2.51 | <0.001 | 1.75 | 1.32–2.33 | <0.001 | 1.82 | 1.38–2.41 | <0.001 | 1.68 | 1.26–2.24 | <0.001 | 1.73 | 1.30–2.31 | <0.001 |
| Primary (n = 85) | 1.44 | 1.11–1.86 | 0.006 | 1.32 | 1.01–1.72 | 0.042 | 1.37 | 1.05–1.79 | 0.020 | 1.30 | 1.01–1.68 | 0.044 | 1.33 | 1.03–1.72 | 0.036 |
| Secondary/degree (n = 18) | Reference | ||||||||||||||
| Employment status | |||||||||||||||
| Unemployed/retired/Housewife (n = 102) | 1.68 | 1.28–2.21 | <0.001 | 1.55 | 1.18–2.05 | 0.002 | 1.60 | 1.22–2.10 | <0.001 | 1.50 | 1.14–1.98 | 0.004 | 1.53 | 1.17–2.00 | 0.003 |
| Employed (n = 52) | Reference | ||||||||||||||
| No. of comorbidities | |||||||||||||||
| ≥3 (n = 32) | 2.05 | 1.53–2.74 | <0.001 | 1.89 | 1.41–2.54 | <0.001 | 2.00 | 1.49–2.69 | <0.001 | 1.85 | 1.38–2.48 | <0.001 | 1.90 | 1.42–2.55 | <0.001 |
| 0–2 (n = 122) | Reference | ||||||||||||||
| Smoking | |||||||||||||||
| No (n = 120) | Reference | ||||||||||||||
| Yes (n = 24) | 1.58 | 1.19–2.10 | 0.002 | 1.45 | 1.09–1.94 | 0.010 | 1.52 | 1.14–2.03 | 0.006 | 1.39 | 1.05–1.84 | 0.021 | 1.47 | 1.12–1.93 | 0.008 |
| Alcohol intake | |||||||||||||||
| Yes (n = 7) | 0.95 | 0.52–1.75 | 0.873 | 0.89 | 0.49–1.62 | 0.720 | 0.92 | 0.50–1.69 | 0.800 | 0.85 | 0.46–1.58 | 0.600 | 0.88 | 0.48–1.63 | 0.730 |
| No (n = 147) | Reference | ||||||||||||||
| Social Support | |||||||||||||||
| Yes (n = 30) | Reference | ||||||||||||||
| No (n = 124) | 0.72 | 0.54–0.95 | 0.022 | 0.68 | 0.51–0.91 | 0.010 | 0.70 | 0.52–0.94 | 0.018 | 0.66 | 0.49–0.90 | 0.009 | 0.69 | 0.51–0.93 | 0.015 |
| Stages of CKD GFR (mL/min/1.73 m2) | |||||||||||||||
| Stage 3 (n = 62) GFR 30-59 | Reference | ||||||||||||||
| Stage 4 to 5 (n = 92) (GFR less than 29) | 2.45 | 1.87–3.21 | <0.001 | 2.32 | 1.76–3.07 | <0.001 | 2.40 | 1.82–3.15 | <0.001 | 2.20 | 1.68–2.89 | <0.001 | 2.28 | 1.74–2.99 | <0.001 |
| Serum Creatinine | |||||||||||||||
| ≤1.2 (mg/dL) (n = 11) | Reference | ||||||||||||||
| >1.2 (mg/dL) (n = 143) | 2.85 | 2.08–3.90 | <0.001 | 2.62 | 1.91–3.60 | <0.001 | 2.78 | 2.02–3.83 | <0.001 | 2.50 | 1.81–3.46 | <0.001 | 2.65 | 1.92–3.65 | <0.001 |
| Domain | −2 Log Likelihood | Hosmer–Lemeshow χ2 (p-Value) |
|---|---|---|
| Mobility | 172.45 | 5.72 (p = 0.573) |
| Self-care | 190.88 | 6.29 (p = 0.505) |
| Usual Activities | 185.12 | 4.61 (p = 0.710) |
| Pain/Discomfort | 179.67 | 7.03 (p = 0.532) |
| Anxiety/Depression | 187.90 | 6.82 (p = 0.447) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kandasamy, G.; Subramani, T.; Almanasef, M.; Orayj, K.; Shorog, E.; Alshahrani, A.M.; Alanazi, T.S.; Balasubramanian, S. Determinants of Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Cross-Sectional Study. Healthcare 2025, 13, 1167. https://doi.org/10.3390/healthcare13101167
Kandasamy G, Subramani T, Almanasef M, Orayj K, Shorog E, Alshahrani AM, Alanazi TS, Balasubramanian S. Determinants of Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Cross-Sectional Study. Healthcare. 2025; 13(10):1167. https://doi.org/10.3390/healthcare13101167
Chicago/Turabian StyleKandasamy, Geetha, Thangamani Subramani, Mona Almanasef, Khalid Orayj, Eman Shorog, Asma M. Alshahrani, Tahani S. Alanazi, and Sangeetha Balasubramanian. 2025. "Determinants of Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Cross-Sectional Study" Healthcare 13, no. 10: 1167. https://doi.org/10.3390/healthcare13101167
APA StyleKandasamy, G., Subramani, T., Almanasef, M., Orayj, K., Shorog, E., Alshahrani, A. M., Alanazi, T. S., & Balasubramanian, S. (2025). Determinants of Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Cross-Sectional Study. Healthcare, 13(10), 1167. https://doi.org/10.3390/healthcare13101167





