Bibliometric Analysis of Research Trends and Global Collaborations in Anesthesia on Neuromuscular Blockers and Antagonists (2000–2024)
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Data Analysis and Visualization
2.3. Bibliometric Analyses
2.4. Thematic and Trend Analyses
2.5. Centrality and Clustering Metrics in Co-Word Analysis
3. Results
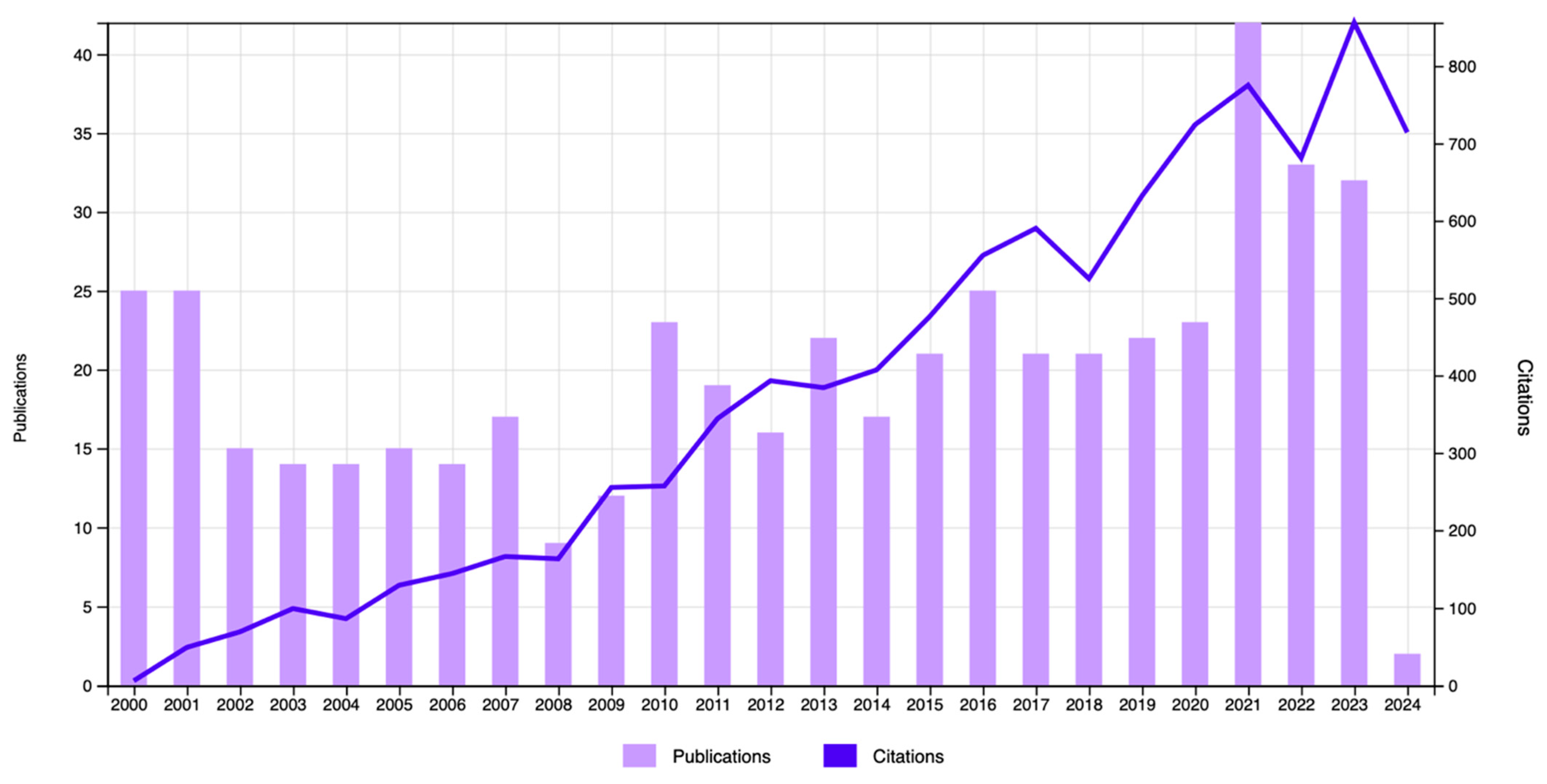
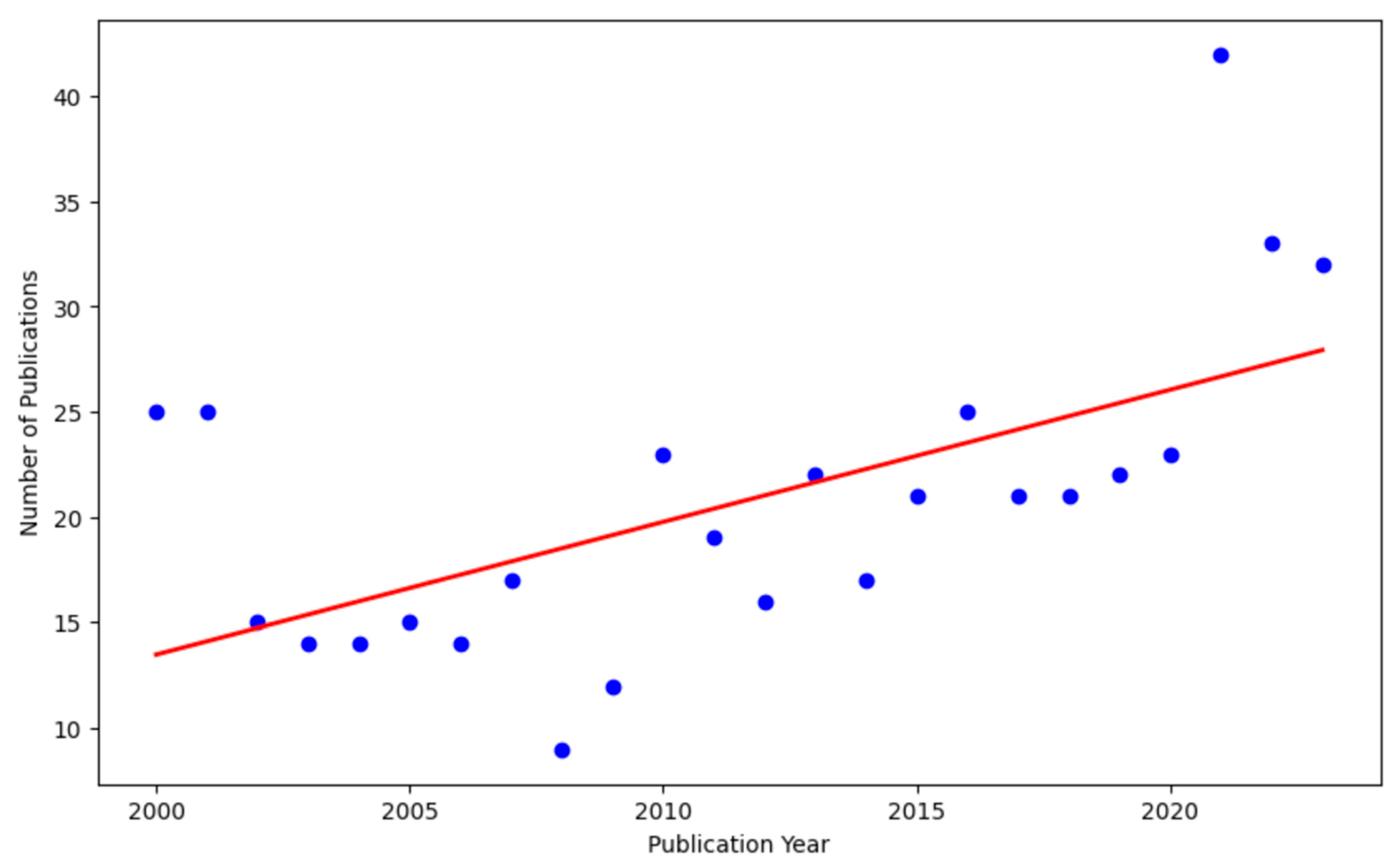
3.1. Publication Outputs in Neuromuscular Blockers and Antagonists Research
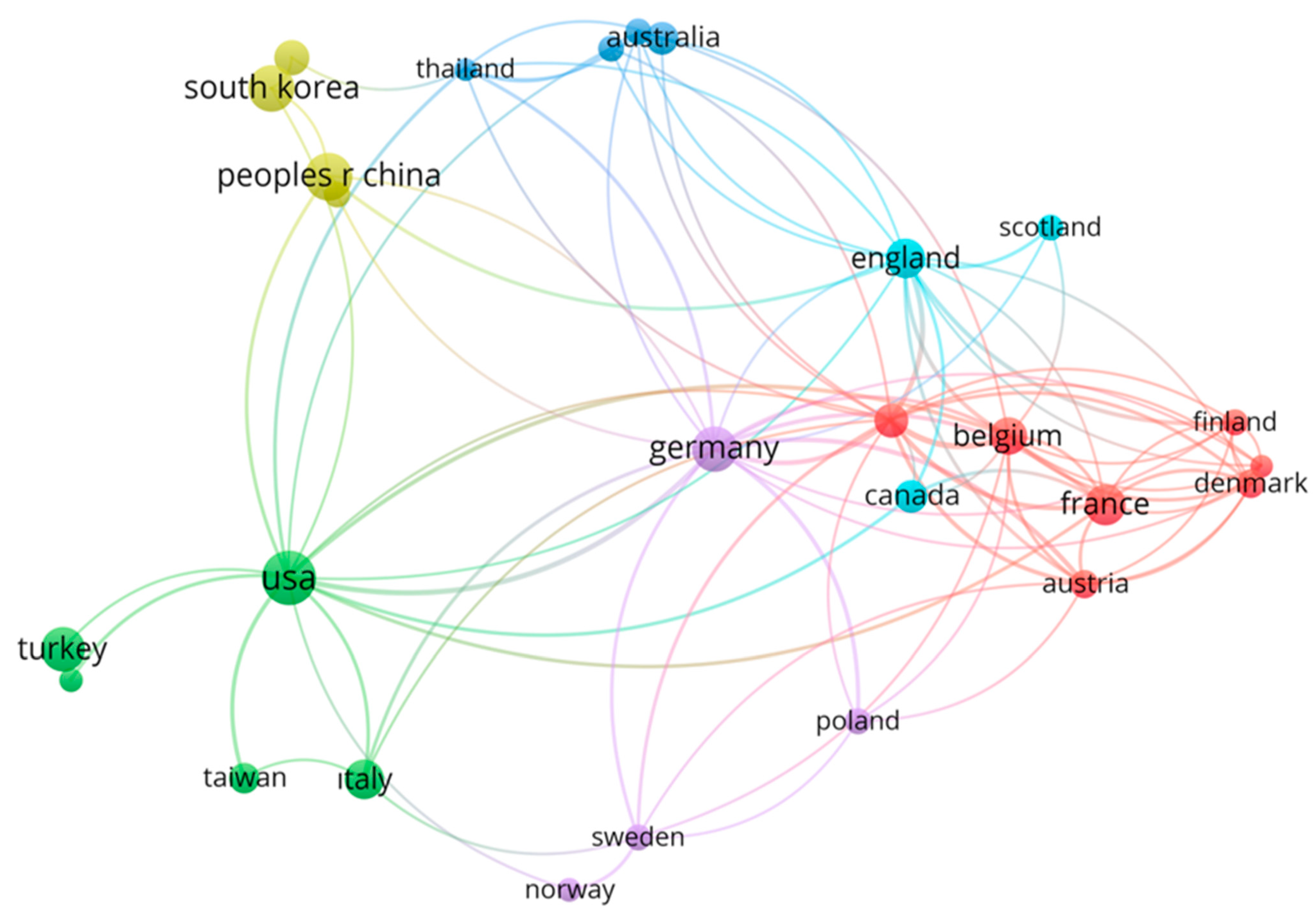
3.2. Analysis of Countries
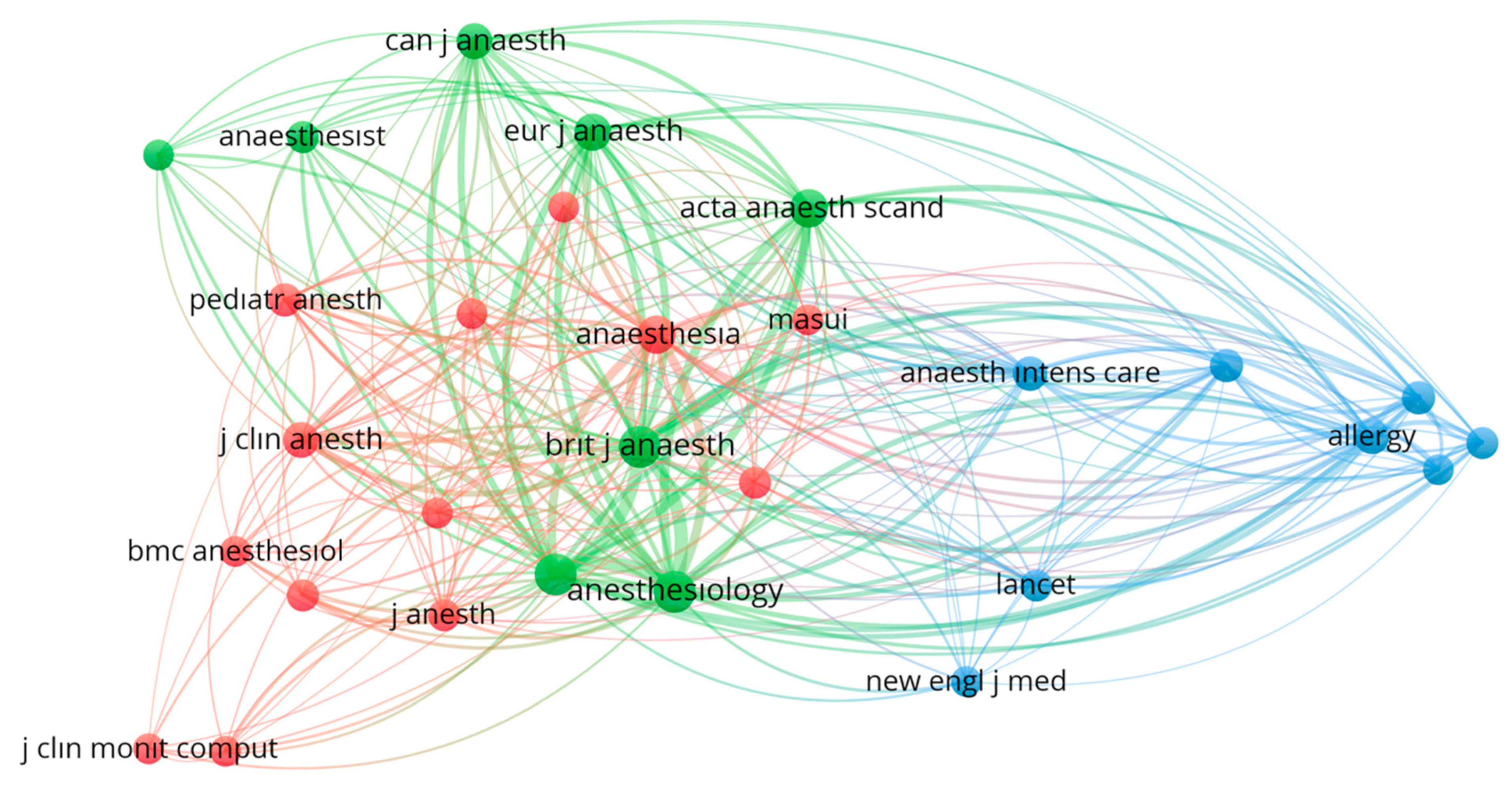
3.3. Journal Analysis
3.4. Analysis of Authors
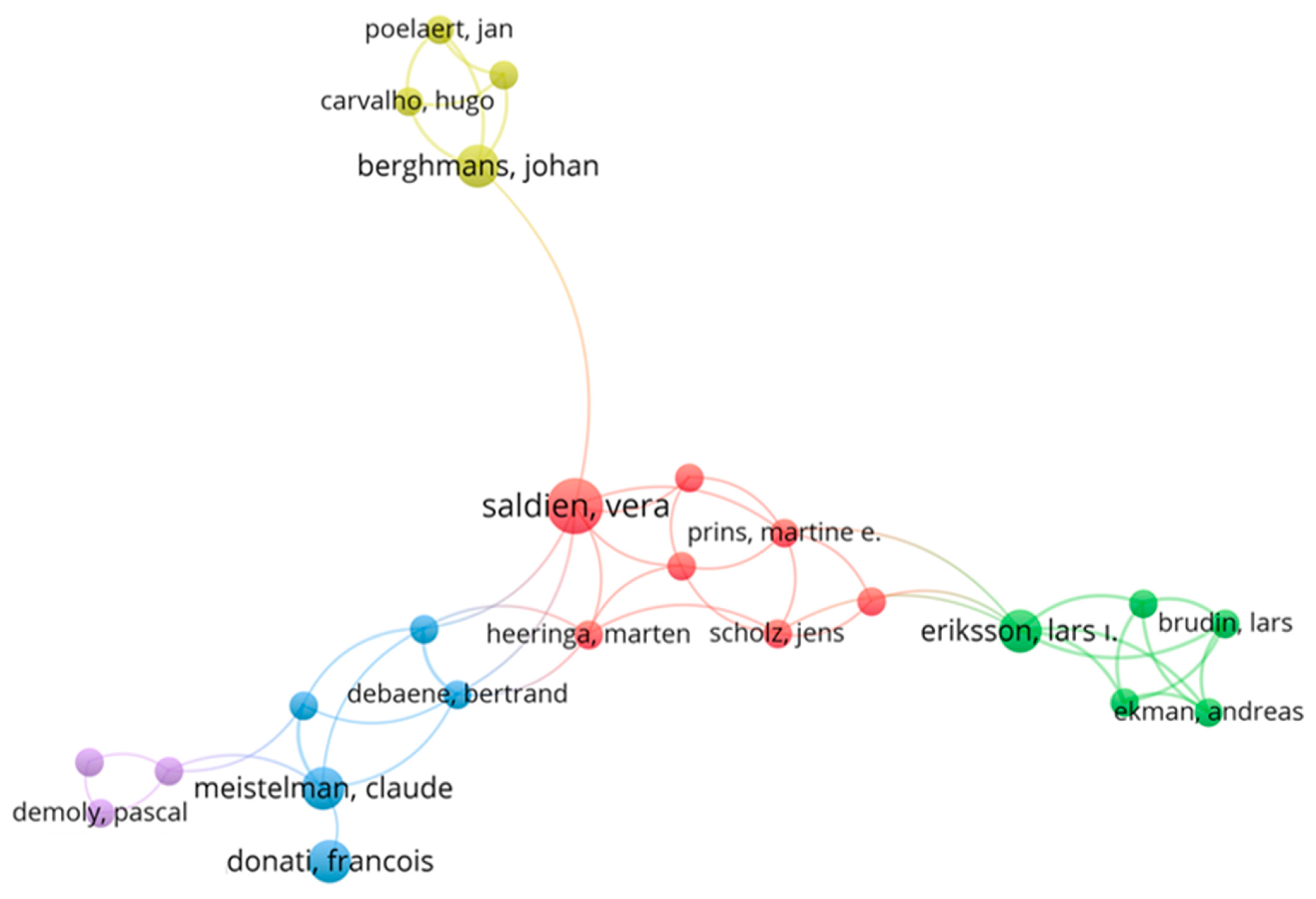
3.5. Analysis of Publications
3.6. Co-Citation Analysis
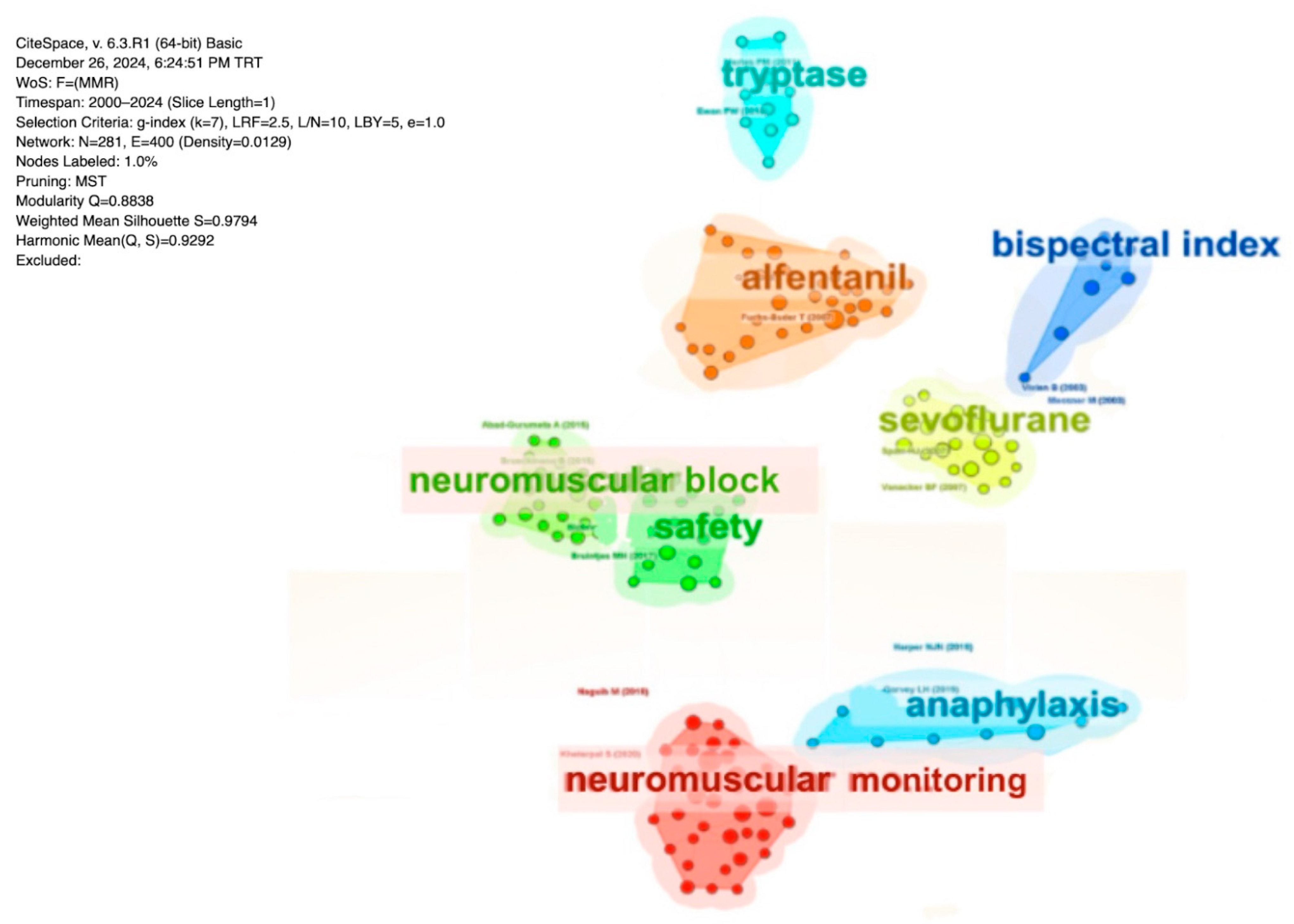
3.7. Analysis of Citation Burst
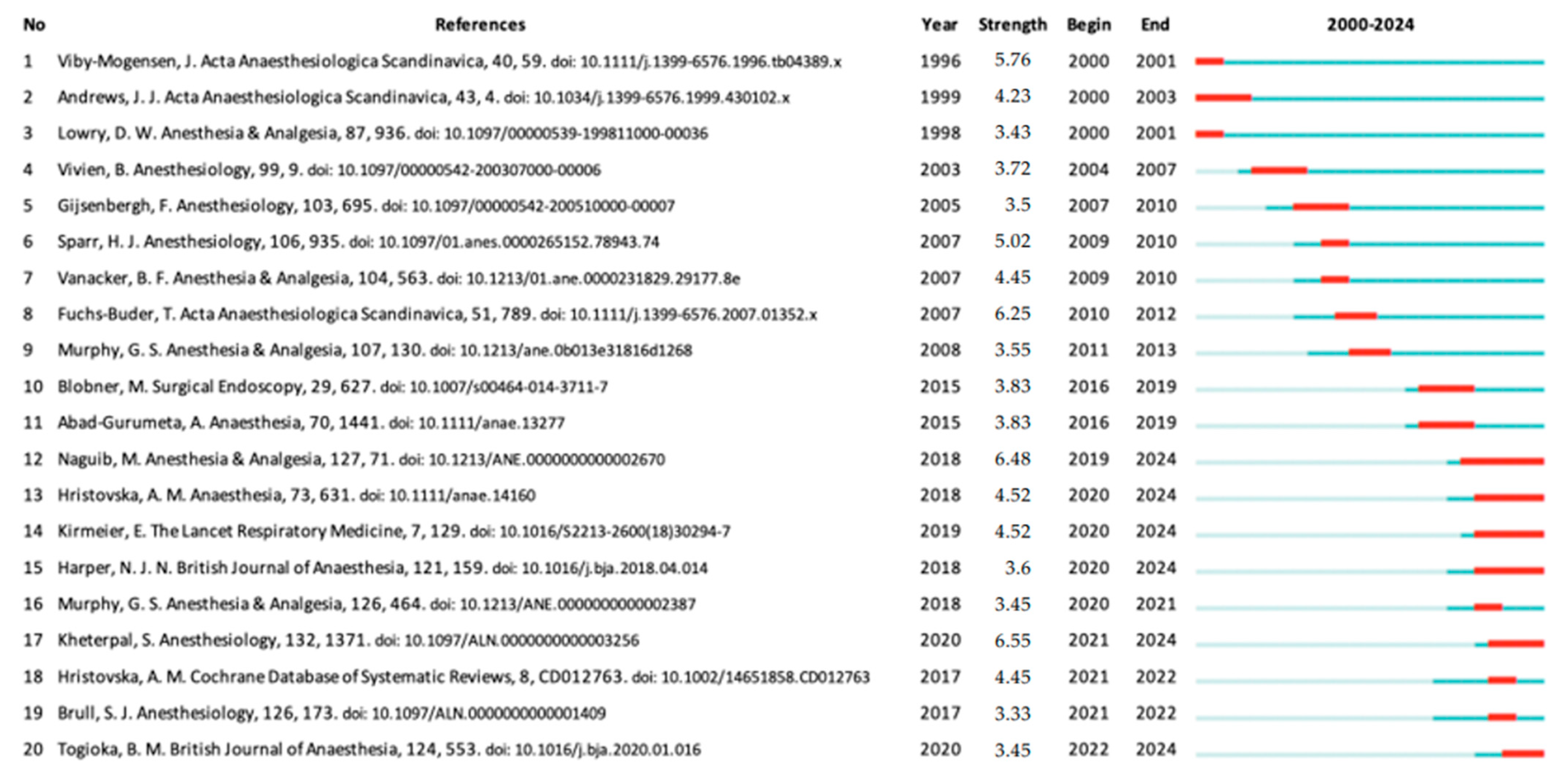
3.8. Analysis of Keywords Co-Occurrence Network
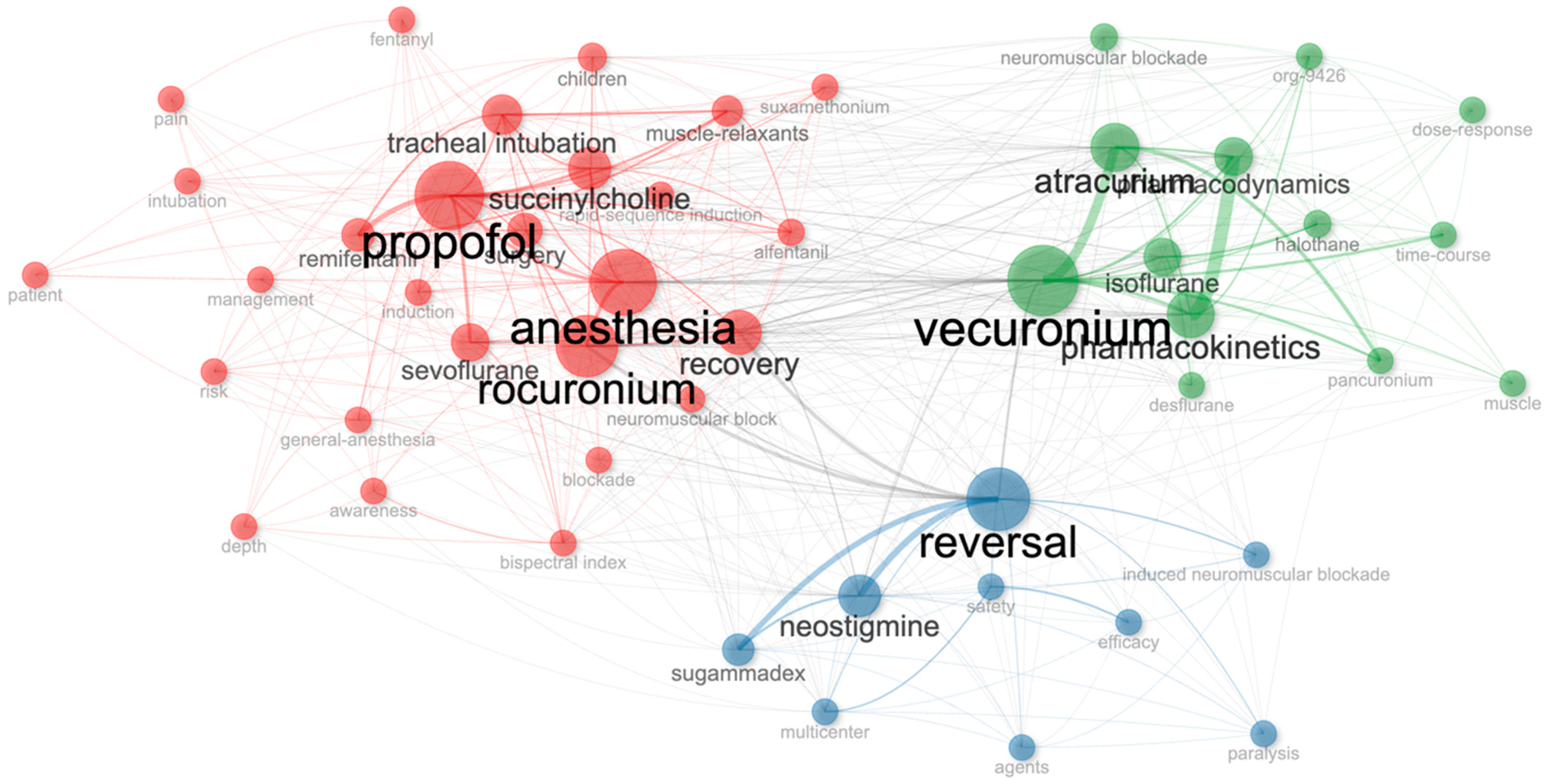
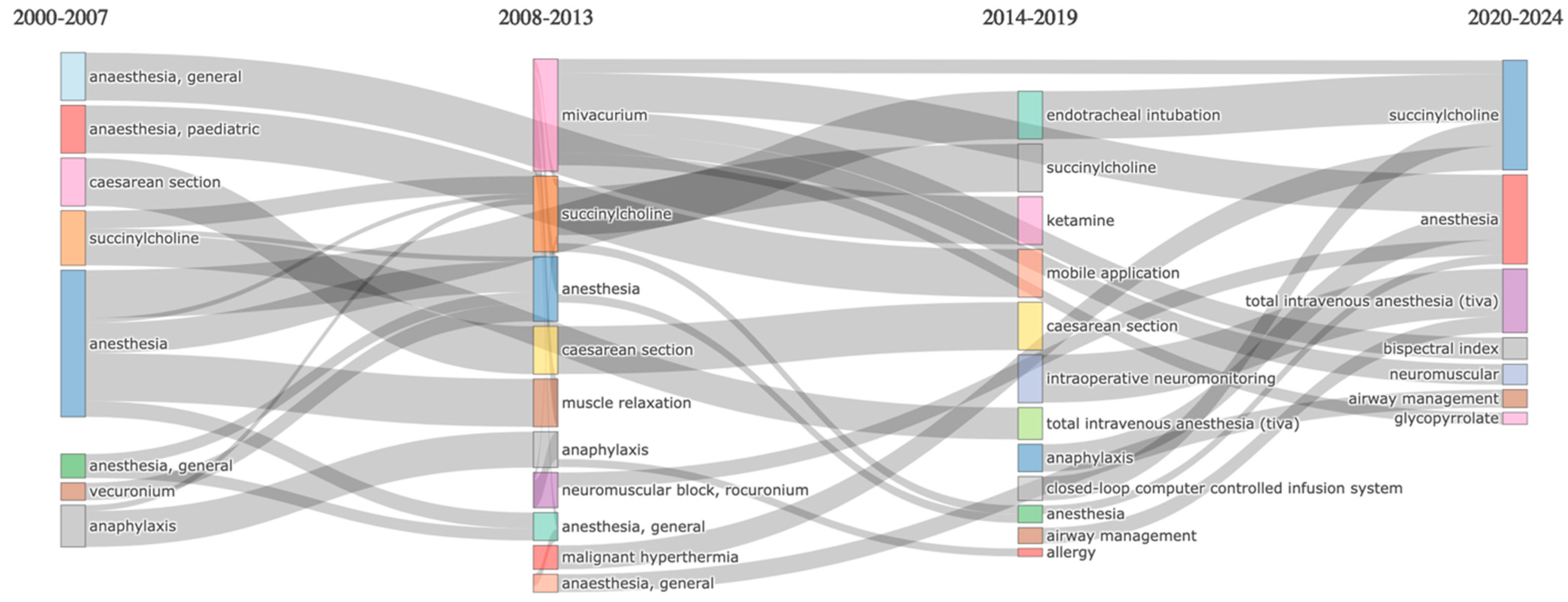
3.9. Analysis of Sankey Diagrams
3.10. Analysis of Keyword Citation Burst
3.11. Clustering and Centrality Metrics in Analysis of Keywords
4. Discussion
4.1. Current Status and Global Collaborations
4.2. Journal Analysis and Scientific Impact
4.3. Analysis of Authors’ Productivity and Scientific Collaborations
4.4. Scientific Impact of Most Highly Cited Publications
4.5. Research Trends
4.6. Thematic Shifts and Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raval, A.D.; Uyei, J.; Karabis, A.; Bash, L.D.; Brull, S.J. Incidence of Residual Neuromuscular Blockade and Use of Neuromuscular Blocking Agents with or without Antagonists: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Anesth. 2020, 64, 109818. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Wynands, J.E. Harold Randall Griffith. The Pioneer of the Use of Muscle Relaxants in Anaesthesia. Br. J. Anaesth. 1986, 58, 943–945. [Google Scholar] [CrossRef] [PubMed]
- Flood, P. The Importance of Myorelaxants in Anesthesia. Curr. Opin. Pharmacol. 2005, 5, 322–327. [Google Scholar] [CrossRef]
- Raghavendra, T. Neuromuscular Blocking Drugs: Discovery and Development. J. R. Soc. Med. 2002, 95, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Stäuble, C.G.; Blobner, M. The Future of Neuromuscular Blocking Agents. Curr. Opin. Anaesthesiol. 2020, 33, 490–498. [Google Scholar] [CrossRef]
- Lien, C.A. Development and Potential Clinical Impairment of Ultra-Short-Acting Neuromuscular Blocking Agents. Br. J. Anaesth. 2011, 107 (Suppl. 1), i60–i71. [Google Scholar] [CrossRef]
- Ohlinger, M.J.; Rhoney, D.H. Neuromuscular Blocking Agents in the Neurosurgical Intensive Care Unit. Surg. Neurol. 1998, 49, 217–221. [Google Scholar] [CrossRef]
- Rodríguez-Rubio, L.; Solis Garcia del Pozo, J.; Nava, E.; Jordán, J. Interaction between Magnesium Sulfate and Neuromuscular Blockers during the Perioperative Period. A Systematic Review and Meta-Analysis. J. Clin. Anesth. 2016, 34, 524–534. [Google Scholar] [CrossRef]
- Blauvelt, G.; Burdick, K.; Cannon, E.J. Nursing Considerations When Using Neuromuscular Blocking Agents to Assist with Intubation: A Review of Literature. Crit. Care Nurs. Q. 2019, 42, 30–40. [Google Scholar] [CrossRef]
- Meistelman, C. Effect Sites of Neuromuscular Blocking Agents and the Monitoring of Clinical Muscle Relaxation. Adv. Exp. Med. Biol. 2003, 523, 227–238. [Google Scholar] [CrossRef]
- Hua, Y.; Ou, X.; Li, Q.; Zhu, T. Neuromuscular Blockers in the Acute Respiratory Distress Syndrome: A Meta-Analysis. PLoS ONE 2020, 15, e0227664. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Blanco, J.; Rodríguez-Yanez, T.; Rodríguez-Blanco, J.D.; Almanza-Hurtado, A.J.; Martínez-Ávila, M.C.; Borré-Naranjo, D.; Acuña Caballero, M.C.; Dueñas-Castell, C. Neuromuscular Blocking Agents in the Intensive Care Unit. J. Int. Med. Res. 2022, 50, 03000605221128148. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Zou, J.; Sun, C.; Chen, G.; Gao, S. Worldwide Research Trends in Crohn’s Disease Treatment over the Past 2 Decades: A Bibliometric Analysis. Front. Pharmacol. 2024, 15, 1441785. [Google Scholar] [CrossRef]
- Duan, H.; Li, J.; Ma, J.; Chen, T.; Zhang, H.; Shang, G. Global Research Development of Chondrosarcoma from 2003 to 2022: A Bibliometric Analysis. Front. Pharmacol. 2024, 15, 1431958. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to Conduct a Bibliometric Analysis: An Overview and Guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Neuhaus, C.; Grawe, P.; Bergström, J.; St. Pierre, M. The Impact of “To Err Is Human” on Patient Safety in Anesthesiology. A Bibliometric Analysis of 20 Years of Research. Front. Med. 2022, 9, 980684. [Google Scholar] [CrossRef]
- Kong, H.; Li, M.; Deng, C.M.; Wu, Y.J.; He, S.T.; Mu, D.L. A Comprehensive Overview of Clinical Research on Dexmedetomidine in the Past 2 Decades: A Bibliometric Analysis. Front. Pharmacol. 2023, 14, 1043956. [Google Scholar] [CrossRef]
- Tian, J.; Chen, C.; Du, X.; Wang, M. Near-Infrared Photoimmunotherapy in Cancer Treatment: A Bibliometric and Visual Analysis. Front. Pharmacol. 2024, 15, 1485242. [Google Scholar] [CrossRef] [PubMed]
- Yates, E.J.; Dixon, L.C. PageRank as a Method to Rank Biomedical Literature by Importance. Source Code Biol. Med. 2015, 10, 16. [Google Scholar] [CrossRef]
- Chen, D.B.; Gao, H.; Lü, L.; Zhou, T. Identifying Influential Nodes in Large-Scale Directed Networks: The Role of Clustering. PLoS ONE 2013, 8, e77455. [Google Scholar] [CrossRef]
- Alfouzan, R.K.; Arun Gopinathan, P.; UI Haq, I.; Iyer, K.; Nawab, A.A.; Alhumaidan, A. Bibliometric Evaluation of the 100 Top-Cited Articles on Anesthesiology. Cureus 2023, 15, e50959. [Google Scholar] [CrossRef]
- Xie, G.; Zhang, K.; Wood, C.; Hoeft, A.; Liu, J.; Fang, X. China’s Contribution to Anesthesiology Research: A 10-Year Survey of the Literature. Anesth. Analg. 2016, 122, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Luo, Z.; Song, X.; Zou, K. Global Research on Sufentanil Use in Anesthesiology from 2003 to 2023: A Bibliometric Analysis. Front. Pharmacol. 2024, 15, 1412726. [Google Scholar] [CrossRef]
- Zhai, W.; Liu, H.; Yu, Z.; Jiang, Y.; Yang, J.; Li, M. Bibliometric Analysis of Research Studies on Postoperative Pain Management of Cesarean Section. J. Pain. Res. 2023, 16, 1345–1353. [Google Scholar] [CrossRef]
- Yin, B.; Wang, H.; Zhao, X.; Zhang, L.; Yu, Y. Research Hotspots and Trends in the Treatment of Postoperative Pain with Ropivacaine: A Bibliometric Analysis from 2003 to 2022. Medicine 2024, 103, e40707. [Google Scholar] [CrossRef]
- Hu, X.; Wang, B.; Hu, L.; Han, D.; Wu, J. Bibliometric Analysis of Global Trends in Remimazolam-Related Research Over the Past 15 Years: Compared with Propofol. Drug Des. Devel Ther. 2023, 17, 2119–2135. [Google Scholar] [CrossRef]
- Qian, M.; Zhong, J.; Lu, Z.; Zhang, W.; Zhang, K.; Jin, Y. Top 100 Most-Cited Articles on Pediatric Anesthesia from 1990 to 2023. World J. Pediatr. Surg. 2024, 7, e000823. [Google Scholar] [CrossRef]
- Mertes, P.M.; Petitpain, N.; Tacquard, C.; Delpuech, M.; Baumann, C.; Malinovsky, J.M.; Longrois, D.; Gouel-Cheron, A.; Le Quang, D.; Demoly, P.; et al. Pholcodine Exposure Increases the Risk of Perioperative Anaphylaxis to Neuromuscular Blocking Agents: The ALPHO Case-Control Study. Br. J. Anaesth. 2023, 131, 150–158. [Google Scholar] [CrossRef]
- Petitpain, N.; Argoullon, L.; Masmoudi, K.; Fedrizzi, S.; Cottin, J.; Latarche, C.; Mertes, P.M.; Gillet, P.; Bourneau-Martin, D.; Jantzem, H.; et al. Neuromuscular Blocking Agents Induced Anaphylaxis: Results and Trends of a French Pharmacovigilance Survey from 2000 to 2012. Allergy 2018, 73, 2224–2233. [Google Scholar] [CrossRef]
- Mertes, P.M.; Volcheck, G.W. Anaphylaxis to Neuromuscular-Blocking Drugs: All Neuromuscular-Blocking Drugs Are Not the Same. Anesthesiology 2015, 122, 5–7. [Google Scholar] [CrossRef]
- Schepens, T.; Janssens, K.; Maes, S.; Wildemeersch, D.; Vellinga, J.; Jorens, P.G.; Saldien, V. Respiratory Muscle Activity after Spontaneous, Neostigmine- or Sugammadex-Enhanced Recovery of Neuromuscular Blockade: A Double Blind Prospective Randomized Controlled Trial. BMC Anesthesiol. 2019, 19, 187. [Google Scholar] [CrossRef] [PubMed]
- Duvaldestin, P.; Kuizenga, K.; Saldien, V.; Claudius, C.; Servin, F.; Klein, J.; Debaene, B.; Heeringa, M. A Randomized, Dose-Response Study of Sugammadex given for the Reversal of Deep Rocuronium- or Vecuronium-Induced Neuromuscular Blockade under Sevoflurane Anesthesia. Anesth. Analg. 2010, 110, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Sparr, H.J.; Vermeyen, K.M.; Beaufort, A.M.; Rietbergen, H.; Proost, J.H.; Saldien, V.; Velik-Salchner, C.; Wierda, J.M.K.H. Early Reversal of Profound Rocuronium-Induced Neuromuscular Blockade by Sugammadex in a Randomized Multicenter Study: Efficacy, Safety, and Pharmacokinetics. Anesthesiology 2007, 106, 935–943. [Google Scholar] [CrossRef]
- Vanacker, B.F.; Vermeyen, K.M.; Struys, M.M.R.F.; Rietbergen, H.; Vandermeersch, E.; Saldien, V.; Kalmar, A.F.; Prins, M.E. Reversal of Rocuronium-Induced Neuromuscular Block with the Novel Drug Sugammadex Is Equally Effective under Maintenance Anesthesia with Propofol or Sevoflurane. Anesth. Analg. 2007, 104, 563–568. [Google Scholar] [CrossRef]
- Mertes, P.M.; Alla, F.; Tréchot, P.; Auroy, Y.; Jougla, E.; Cottineau, C.; Drouet, M.; Girardin, P.; Koeberlé, P.; Vigan, M.; et al. Anaphylaxis during Anesthesia in France: An 8-Year National Survey. J. Allergy Clin. Immunol. 2011, 128, 366–373. [Google Scholar] [CrossRef]
- Mertes, P.; Laxenaire, M.; Lienhart, A.; Aberer, W.; Ring, J.; Pichler, W.; Guilloux, L.; Laroche, D.; Leynadier, F.; Longrois, D.; et al. Reducing the Risk of Anaphylaxis during Anaesthesia: Guidelines for Clinical Practice Demoly 6, for ENDA** and the EAACI Interest Group on Drug Hypersensitivity ** ENDA: European Network for Drug Allergy and the EAACI Interest Group on Drug Hypersensitivity with the Following Additional Members in the Working Group. J. Investig. Allergol. Clin. Immunol. 2005, 15, 91–101. [Google Scholar]
- Laxenaire, M.C.; Mertes, P.M. Anaphylaxis during Anaesthesia. Results of a Two-Year Survey in France. Br. J. Anaesth. 2001, 87, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Blobner, M.; Eriksson, L.I.; Scholz, J.; Motsch, J.; Della Rocca, G.; Prins, M.E. Reversal of Rocuronium-Induced Neuromuscular Blockade with Sugammadex Compared with Neostigmine during Sevoflurane Anaesthesia: Results of a Randomised, Controlled Trial. Eur. J. Anaesthesiol. 2010, 27, 874–881. [Google Scholar] [CrossRef]
- Klein, A.A.; Meek, T.; Allcock, E.; Cook, T.M.; Mincher, N.; Morris, C.; Nimmo, A.F.; Pandit, J.J.; Pawa, A.; Rodney, G.; et al. Recommendations for Standards of Monitoring during Anaesthesia and Recovery 2021: Guideline from the Association of Anaesthetists. Anaesthesia 2021, 76, 1212–1223. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, J.; Wu, J.; Zhang, H.; Luan, Z.; Zhao, Z.; Li, C.; Zhao, Y.; Zhang, H.; Wang, S.; et al. A Bibliometric and Visual Analysis of the Use of Ustekinumab in Crohn’s Disease Using CiteSpace. Front. Pharmacol. 2024, 14, 1322319. [Google Scholar] [CrossRef]
- Viby-Mogensen, J.; Engbæk, J.; Eriksson, L.I.; Gramstad, L.; Jensen, E.; Jensen, F.S.; Koscielniak-Nielsen, Z.; Skovgaard, L.T.; ØStergaard, D. Good Clinical Research Practice (GCRP) in Pharmacodynamic Studies of Neuromuscular Blocking Agents. Acta Anaesthesiol. Scand. 1996, 40, 59–74. [Google Scholar] [CrossRef]
- Andrews, J.I.; Kumar, N.; Van Den Brom, R.H.G.; Olkkola, K.T.; Roest, G.J.; Wright, P.M.C. A Large Simple Randomized Trial of Rocuronium versus Succinylcholine in Rapid-Sequence Induction of Anaesthesia along with Propofol. Acta Anaesthesiol. Scand. 1999, 43, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.T.; Mirakhur, R.K.; Lowry, D.W.; McCourt, K.C.; Kerr, C. Neuromuscular Blocking Effects and Train-of-Four Fade with Cisatracurium: Comparison with Other Nondepolarising Relaxants. Anaesthesia 1998, 53, 1169–1173. [Google Scholar] [CrossRef] [PubMed]
- Vivien, B.; Di Maria, S.; Ouattara, A.; Langeron, O.; Coriat, P.; Riou, B. Overestimation of Bispectral Index in Sedated Intensive Care Unit Patients Revealed by Administration of Muscle Relaxant. Anesthesiology 2003, 99, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Gijsenbergh, F.; Ramael, S.; Houwing, N.; Van Iersel, T. First Human Exposure of Org 25969, a Novel Agent to Reverse the Action of Rocuronium Bromide. Anesthesiology 2005, 103, 695–703. [Google Scholar] [CrossRef]
- Fuchs-Buder, T.; Claudius, C.; Skovgaard, L.T.; Eriksson, L.I.; Mirakhur, R.K.; Viby-Mogensen, J. Good Clinical Research Practice in Pharmacodynamic Studies of Neuromuscular Blocking Agents II: The Stockholm Revision. Acta Anaesthesiol. Scand. 2007, 51, 789–808. [Google Scholar] [CrossRef]
- Abad-Gurumeta, A.; Ripollés-Melchor, J.; Casans-Francés, R.; Espinosa, A.; Martínez-Hurtado, E.; Fernández-Pérez, C.; Ramírez, J.M.; Lõpez-Timoneda, F.; Calvo-Vecino, J.M. A Systematic Review of Sugammadex vs Neostigmine for Reversal of Neuromuscular Blockade. Anaesthesia 2015, 70, 1441–1452. [Google Scholar] [CrossRef]
- Kheterpal, S.; Vaughn, M.T.; Dubovoy, T.Z.; Shah, N.J.; Bash, L.D.; Colquhoun, D.A.; Shanks, A.M.; Mathis, M.R.; Soto, R.G.; Bardia, A.; et al. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER): A Multicenter Matched Cohort Analysis. Anesthesiology 2020, 132, 1371–1381. [Google Scholar] [CrossRef]
- Murphy, G.S. Neuromuscular Monitoring in the Perioperative Period. Anesth. Analg. 2018, 126, 464–468. [Google Scholar] [CrossRef]
- Hristovska, A.M.; Duch, P.; Allingstrup, M.; Afshari, A. Efficacy and Safety of Sugammadex versus Neostigmine in Reversing Neuromuscular Blockade in Adults. Cochrane Database Syst. Rev. 2017, 8, CD012763. [Google Scholar] [CrossRef]
- Brull, S.J.; Kopman, A.F. Current Status of Neuromuscular Reversal and Monitoring: Challenges and Opportunities. Anesthesiology 2017, 126, 173–190. [Google Scholar] [CrossRef] [PubMed]
- Blobner, M.; Frick, C.G.; Stäuble, R.B.; Feussner, H.; Schaller, S.J.; Unterbuchner, C.; Lingg, C.; Geisler, M.; Fink, H. Neuromuscular Blockade Improves Surgical Conditions (NISCO). Surg. Endosc. 2015, 29, 627–636. [Google Scholar] [CrossRef] [PubMed]


| Component | Details |
|---|---|
| Database | WoSCC (SCI-Expanded) |
| Search Date | 20 September 2024 |
| Search Fields | Title (TI) and Author Keywords (AK) |
| Keywords Used 1 | “Neuromuscular block” OR “Neuromuscular monitoring” OR “Neuromuscular management” OR “Depolarizing agents” OR “Non-depolarizing agents” OR “Cholinesterase inhibitors” OR “Neuromuscular antagonists” OR “Succinylcholine” OR “Pancuronium” OR “Vecuronium” OR “Rocuronium” OR “Atracurium” OR “Cisatracurium” OR “Mivacurium” OR “Sugammadex” OR “Neostigmine” OR “Pyridostigmine” OR “Edrophonium” |
| Keywords Used 2 | “Anesthesia” OR “Anaesthesia” OR “Anesthesiology” |
| Boolean Combination | Keywords Used 1 AND Keywords Used 2 |
| Time Frame | 2000–2024 |
| Language | English only |
| Document Types | Articles and review articles |
| Exclusion Criteria | Veterinary publications, duplicate records, incomplete bibliographic data, and non-English articles |
| Keyword Selection | Based on expert consensus among anesthesiologists with ≥10 years of experience |
| Top 10 Most Productive Contributing Countries | Top 10 Active Countries According to Number of Citations | |||
|---|---|---|---|---|
| Country | N (%) | Country | N(%) | |
| 1 | USA | 78 (15.63) | France | 1776 (19.04) |
| 2 | People’s Republic of China | 50 (10.02) | USA | 1055 (11.31) |
| 3 | South Korea | 46 (9.21) | Germany | 908 (9.73) |
| 4 | Germany | 44 (8.81) | United Kingdom | 812 (8.70) |
| 5 | Turkey | 39 (7.81) | Belgium | 575 (6.16) |
| 6 | France | 30 (6.01) | Korea | 483 (5.18) |
| 7 | England | 29 (5.81) | Italy | 428 (4.59) |
| 8 | Italy | 29 (5.81) | Denmark | 398 (4.26) |
| 9 | Belgium | 23 (4.60) | Turkey | 308 (3.30) |
| 10 | Japan | 21 (4.20) | Australia | 306 (3.28) |
| Top 10 Most Productive Contributor Journals | Top 10 Active Journals According to Number of Citations | |||
|---|---|---|---|---|
| Journal | N (%) | Journal | N(%) | |
| 1 | British Journal of Anaesthesia | 44 (8.81) | British Journal of Anaesthesia | 1728 (18.52) |
| 2 | European Journal of Anaesthesiology | 30 (6.01) | Anesthesia & Analgesia | 756 (8.10) |
| 3 | Journal of Clinical Anesthesia | 25 (5.01) | European Journal of Anaesthesiology | 681 (7.30) |
| 4 | Acta Anaesthesiologica Scandinavica | 23 (4.60) | Acta Anaesthesiologica Scandinavica | 520 (5.57) |
| 5 | Pediatric Anesthesia | 20 (4.00) | Journal of Investigational Allergology and Clinical Immunology | 424 (4.54) |
| 6 | Anesthesia & Analgesia | 19 (3.80) | Journal of Clinical Anesthesia | 395 (4.23) |
| 7 | BMC Anesthesiology | 14 (2.80) | Journal of Allergy and Clinical Immunology | 282 (3.02) |
| 8 | Medicine | 12 (2.42) | Anaesthesia | 271 (2.90) |
| 9 | Journal of Anesthesia | 12 (2.42) | Allergy | 223 (2.39) |
| 10 | Anaesthesia and Intensive Care | 11 (2.22) | Pediatric Anesthesia | 218 (2.33) |
| Top 10 Most Productive Contributing Authors | Top 10 Active Authors According to Number of Citations | |||
|---|---|---|---|---|
| Author | N (%) | Author | N (%) | |
| 1 | Mertes P.M. | 10 (2.00) | Mertes P.M. | 1273 (2.37) |
| 2 | Fuchs-Buder T. | 9 (1.80) | Demoly P. | 553 (1.02) |
| 3 | Blobner M. | 6 (2.20) | Malinovsky J.M. | 476 (0.88) |
| 4 | Demoly P. | 6 (1.20) | Aberer W. | 424 (0.78) |
| 5 | Eikermann M. | 6 (1.20) | Laxenaire M.M. | 405 (0.75) |
| 6 | Adamus M. | 5 (1.00) | Blobner M. | 336 (0.62) |
| 7 | Donati F. | 5 (1.00) | Alla F. | 282 (0.52) |
| 8 | Malinovsky J.M. | 5 (1.00) | Auroy Y. | 283 (0.52) |
| 9 | Stourac P. | 5 (1.00) | Jougla E. | 284 (0.52) |
| 10 | Carron M. | 4 (0.80) | Tréchot P. | 285 (0.52) |
| Title | Journal | Journal Category Quartile | Journal Impact Factor (Five-Year) | First Author | Publication Year | Number of Citations | |
|---|---|---|---|---|---|---|---|
| 1 | Mertes, Paul Michel et al. “Anaphylaxis during anesthesia in France: an 8-year national survey”. Journal of Allergy and Clinical Immunology vol. 128,2 (2011): 366–373. doi:10.1016/j.jaci.2011.03.003 | Journal of Allergy and Clinical Immunology | Q1 | 10.2 | Mertes, P.M. | 2011 | 282 |
| 2 | Mertes, P M et al. “Reducing the risk of anaphylaxis during anaesthesia: guidelines for clinical practice”. Journal of Investigational Allergology and Clinical Immunology vol. 15,2 (2005): 91–101. | Journal of Investigational Allergology and Clinical Immunology | Q1 | 6.5 | Mertes, P.M. | 2011 | 273 |
| 3 | Laxenaire, M C et al. “Anaphylaxis during anaesthesia. Results of a two-year survey in France”. British Journal of Anaesthesia vol. 87,4 (2001): 549–558. doi:10.1093/bja/87.4.549 | British Journal of Anaesthesia | Q1 | 9.5 | Laxenaire, M.C. | 2001 | 253 |
| 4 | Blobner, Manfred et al. “Reversal of rocuronium-induced neuromuscular blockade with sugammadex compared with neostigmine during sevoflurane anaesthesia: results of a randomised, controlled trial”. European Journal of Anaesthesiology vol. 27,10 (2010): 874–881. doi:10.1097/EJA.0b013e32833d56b7 | European Journal of Anaesthesiology | Q1 | 4.3 | Blobner, M. | 2010 | 174 |
| 5 | Klein, A A et al. “Recommendations for standards of monitoring during anaesthesia and recovery 2021: Guideline from the Association of Anaesthetists”. Anaesthesia vol. 76,9 (2021): 1212–1223. doi:10.1111/anae.15501 | Anaesthesia | Q1 | 8 | Klein, A.A. | 2021 | 170 |
| 6 | Ebo, D G et al. “Anaphylaxis during anaesthesia: diagnostic approach”. Allergy vol. 62,5 (2007): 471–487. doi:10.1111/j.1398-9995.2007.01347.x | Allergy | Q1 | 11.8 | Ebo, D.G. | 2007 | 158 |
| 7 | Mertes, P M et al. “Reducing the risk of anaphylaxis during anaesthesia: guidelines for clinical practice”. Journal of Investigational Allergology and Clinical Immunology vol. 15,2 (2005): 91–101. | Journal of Investigational Allergology and Clinical Immunology | Q1 | 6.5 | Mertes, P.M. | 2005 | 152 |
| 8 | Schuller, P J et al. “Response of bispectral index to neuromuscular block in awake volunteers”. British Journal of Anaesthesia vol. 115 Suppl 1 (2015): i95–i103. doi:10.1093/bja/aev072 | British Journal of Anaesthesia | Q1 | 9.5 | Schuller, P.J. | 2015 | 135 |
| 9 | Ryu, J-H et al. “Effects of magnesium sulphate on intraoperative anaesthetic requirements and postoperative analgesia in gynaecology patients receiving total intravenous anaesthesia”. British Journal of Anaesthesia vol. 100,3 (2008): 397–403. doi:10.1093/bja/aem407 | British Journal of Anaesthesia | Q1 | 9.5 | Ryu, J.H. | 2008 | 135 |
| 10 | Ewan, P W et al. “BSACI guidelines for the investigation of suspected anaphylaxis during general anaesthesia”. Clinical and Experimental Allergy: Journal of the British Society for Allergy and Clinical Immunology vol. 40,1 (2010): 15–31. doi:10.1111/j.1365-2222.2009.03404.x | Clinical and Experimental Allergy | Q1 | 5.2 | Ewan, P.W. | 2010 | 134 |
| Keyword | Cluster | Betweenness | Closeness | Page Rank | |
|---|---|---|---|---|---|
| 1 | anesthesia | 2 | 484.51 | 0.019 | 0.158 |
| 2 | neuromuscular block | 2 | 144.938 | 0.017 | 0.095 |
| 3 | anesthetics | 2 | 166.74 | 0.017 | 0.094 |
| 4 | neuromuscular blocking agents | 1 | 84.804 | 0.015 | 0.056 |
| 5 | sugammadex | 2 | 7.89 | 0.013 | 0.048 |
| 6 | anaphylaxis | 1 | 9.585 | 0.013 | 0.042 |
| 7 | propofol | 2 | 5.232 | 0.013 | 0.028 |
| 8 | neostigmine | 2 | 0.668 | 0.011 | 0.024 |
| 9 | cisatracurium | 2 | 2.753 | 0.013 | 0.022 |
| 10 | tryptase | 1 | 0.972 | 0.012 | 0.022 |
| 11 | monitoring | 2 | 3.171 | 0.012 | 0.021 |
| 12 | remifentanil | 2 | 1.705 | 0.012 | 0.018 |
| 13 | skin test | 1 | 0.278 | 0.012 | 0.018 |
| 14 | latex | 1 | 0.14 | 0.011 | 0.017 |
| 15 | antibiotics | 1 | 0.471 | 0.012 | 0.017 |
| 16 | general anesthesia | 2 | 4.251 | 0.012 | 0.017 |
| 17 | bispectral index | 2 | 2.507 | 0.012 | 0.016 |
| 18 | succinylcholine | 3 | 4.475 | 0.012 | 0.015 |
| 19 | intubation | 2 | 0.56 | 0.012 | 0.015 |
| 20 | vecuronium | 2 | 1.115 | 0.012 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evran, T.; Özçınar, H.; Çopur, İ.; Bilgili, B. Bibliometric Analysis of Research Trends and Global Collaborations in Anesthesia on Neuromuscular Blockers and Antagonists (2000–2024). Healthcare 2025, 13, 1146. https://doi.org/10.3390/healthcare13101146
Evran T, Özçınar H, Çopur İ, Bilgili B. Bibliometric Analysis of Research Trends and Global Collaborations in Anesthesia on Neuromuscular Blockers and Antagonists (2000–2024). Healthcare. 2025; 13(10):1146. https://doi.org/10.3390/healthcare13101146
Chicago/Turabian StyleEvran, Turan, Hüseyin Özçınar, İsmet Çopur, and Beliz Bilgili. 2025. "Bibliometric Analysis of Research Trends and Global Collaborations in Anesthesia on Neuromuscular Blockers and Antagonists (2000–2024)" Healthcare 13, no. 10: 1146. https://doi.org/10.3390/healthcare13101146
APA StyleEvran, T., Özçınar, H., Çopur, İ., & Bilgili, B. (2025). Bibliometric Analysis of Research Trends and Global Collaborations in Anesthesia on Neuromuscular Blockers and Antagonists (2000–2024). Healthcare, 13(10), 1146. https://doi.org/10.3390/healthcare13101146








