Patient Satisfaction in Primary and Specialised Ambulatory Healthcare: A Web-Based Cross-Sectional Study in the Polish Population
Abstract
1. Background
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Variables and Data Measurement
2.5. Study Size
2.6. Statistical Analysis
2.7. Ethics Consideration
3. Results
3.1. Characteristics of the Study Group
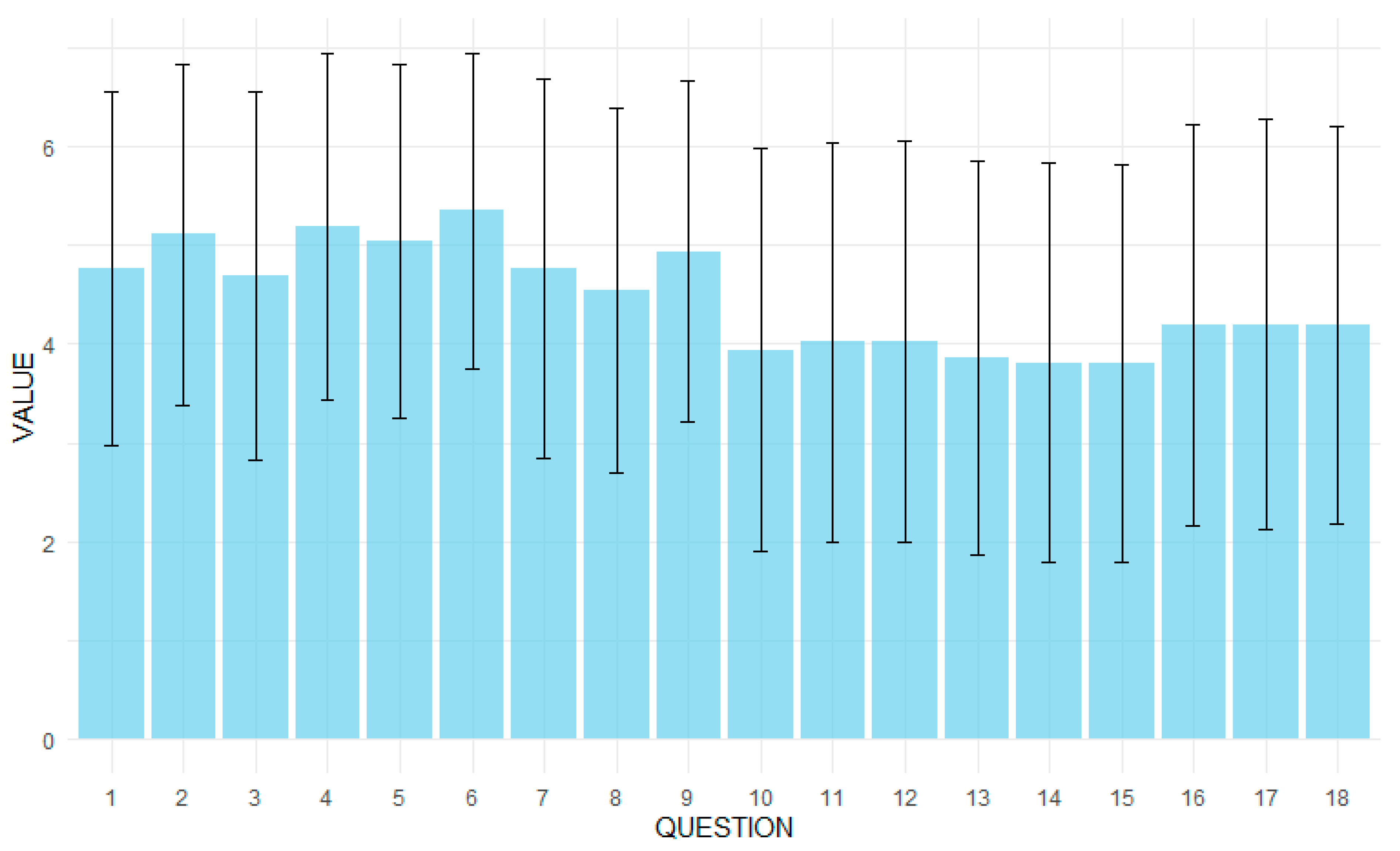
3.2. Patients’ Expectations
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Global Patient Safety Action Plan; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan (accessed on 5 May 2025).
- Chassin, M.R. The Urgent Need to Improve Health Care Quality—Institute of Medicine National Roundtable on Health Care Quality. JAMA 1998, 280, 1000. [Google Scholar] [CrossRef] [PubMed]
- Krot, K. Quality and Marketing of Medical Services; Wolters Kluwer Polska: Warsaw, Poland, 2021. [Google Scholar]
- Kędra, E.; Chudak, B. Quality of Medical Services and Medical Effectiveness. Public Health Nurs. 2011, 1, 83–87. [Google Scholar]
- Kurji, Z.; Shaheen, Z.; Mithani, Y. Review and Analysis of Quality Healthcare System Enhancement in Developing Countries. JPMA J. Pak. Med. Assoc. 2015, 65, 776–781. [Google Scholar]
- Brown, A. Communication and Leadership in Healthcare Quality Governance: Findings from Comparative Case Studies of Eight Public Hospitals in Australia. J. Health Organ. Manag. 2020, 34, 144–161. [Google Scholar] [CrossRef] [PubMed]
- Mühlbacher, A.; Stolk, E. Patient-Reported Satisfaction, Experiences, and Preferences: Same but Different? Value Health 2023, 26, 1–3. [Google Scholar] [CrossRef]
- Hoff, T.; Prout, K.; Carabetta, S. How Teams Impact Patient Satisfaction: A Review of the Empirical Literature. Health Care Manag. Rev. 2021, 46, 75. [Google Scholar] [CrossRef]
- Maślach, D.; Karczewska, B.; Szpak, A.; Charkiewicz, A.; Krzyżak, M. Does Place of Residence Affect Patient Satisfaction with Hospital Health Care? Ann. Agric. Environ. Med. 2020, 27, 86–90. [Google Scholar] [CrossRef]
- Świątoniowska-Lonc, N.; Polański, J.; Tański, W.; Jankowska-Polańska, B. Impact of Satisfaction with Physician—Patient Communication on Self-Care and Adherence in Patients with Hypertension: Cross-Sectional Study. BMC Health Serv. Res. 2020, 20, 1046. [Google Scholar] [CrossRef]
- Arraras, J.I.; Giesinger, J.; Shamieh, O.; Bahar, I.; Koller, M.; Bredart, A.; Kuljanic, K.; Costantini, A.; Greimel, E.; Sztankay, M.; et al. Cancer Patient Satisfaction with Health Care Professional Communication: An International EORTC Study. Psychooncology 2022, 31, 541–547. [Google Scholar] [CrossRef]
- Ćwik, K. The Impact of Quality Management Systems on the Efficiency of Public Hospital Services in Poland. Ph.D. Thesis, University of Gdansk, Gdansk, Poland, 2024. Available online: https://repozytorium.bg.ug.edu.pl/info/phd/UOGf58bc44d40f044048b1a1b8161629b5f (accessed on 9 August 2024).
- Act of 16 June 2023 on Quality in Health Care and Patient Safety. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20230001692 (accessed on 10 May 2025).
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Int. Res. 2004, 6, e132. [Google Scholar] [CrossRef] [PubMed]
- Rzadkiewicz, M.; Chylinska, J.; Jaworski, M.; Lazarewicz, M.; Adamus, M.; Haugan, G.; Lillefjell, M.; Espnes, G.A.; Wlodarczyk, D. Activation of older patients through PRACTA intervention for primary healthcare doctors: Does the method matter? Eur. J. Public Health 2017, 27, 998–1003. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Krot, K. Trust in the Doctor-Patient Relationship: Implications for Healthcare Facility Management; CeDeWu: Warsaw, Poland, 2019. [Google Scholar]
- Donabedian, A. Evaluating the Quality of Medical Care. Milbank Q. 2005, 83, 691–729. [Google Scholar] [CrossRef] [PubMed]
- Pawelczyk, K.; Maniecka-Bryła, I.; Targowski, M.; Samborska-Sablik, A. Patient Satisfaction as One of the Indicators of Healthcare Quality: A Case Study of a Primary Care Clinic. Acta Clin. Morphol. 2006, 3, 20–21. [Google Scholar]
- Andaleeb, S.S. Service Quality Perceptions and Patient Satisfaction: A Study of Hospitals in a Developing Country. Soc. Sci. Med. 2001, 52, 1359–1370. [Google Scholar] [CrossRef]
- Zineldin, M. The Quality of Health Care and Patient Satisfaction: An Exploratory Investigation of the 5Qs Model at Some Egyptian and Jordanian Medical Clinics. Int. J. Health Care Qual. Assur. 2006, 19, 60–92. [Google Scholar] [CrossRef]
- Choi, K.; Lee, H.; Kim, C.; Lee, S. The Service Quality Dimensions and Patient Satisfaction Relationships in South Korea: Comparisons Across Gender, Age, and Types of Service. J. Serv. Mark. 2005, 19, 140–149. [Google Scholar] [CrossRef]
- Van Den Assem, B.; Dulewicz, V. Doctors’ Trustworthiness, Practice Orientation, Performance, and Patient Satisfaction. Int. J. Health Care Qual. Assur. 2015, 28, 82–95. [Google Scholar] [CrossRef]
- Johnson, D.M.; Russell, R.S.; White, S.W. Perceptions of Care Quality and the Effect on Patient Satisfaction. Int. J. Qual. Reliab. Manag. 2016, 33, 1202–1229. [Google Scholar] [CrossRef]
- Naoum, S.; Konstantinidis, T.I.; Spinthouri, M.; Mitseas, P.; Sarafis, P. Patient Satisfaction and Physician Empathy at a Hellenic Air Force Health Service. Mil. Med. 2021, 186, 1029–1036. [Google Scholar] [CrossRef]
- Lewis, J.R. Patient Views on Quality Care in General Practice: Literature Review. Soc. Sci. Med. 1994, 39, 655–670. [Google Scholar] [CrossRef] [PubMed]
- Gabel, L.L.; Lucas, J.B.; Westbury, R.C. Why Do Patients Continue to See the Same Physician? Fam. Pract. Res. J. 1993, 13, 133–147. [Google Scholar]
- Hashim, M.J. Patient-Centered Communication: Basic Skills. Am. Fam. Physician 2017, 95, 29–34. [Google Scholar] [PubMed]
- Bradshaw, A.; Raphaelson, S. Improving Patient Satisfaction with Wait Times. Nursing2024 2021, 51, 67. [Google Scholar] [CrossRef]
- Dansky, K.H.; Miles, J. Patient Satisfaction with Ambulatory Healthcare Services: Waiting Time and Filling Time. J. Healthc. Manag. 1997, 42, 165. [Google Scholar]
- Piekutowski, J. Migration: An Untapped (for Now) Opportunity for Poland; Warsaw Enterprise Institute: Warsaw, Poland, 2023; Available online: https://wei.org.pl/wp-content/uploads/2023/09/Migracje-niewykorzystana-na-razie-szansa-Polski-raport.pdf (accessed on 17 May 2024).
- Govere, L.; Govere, E.M. How Effective is Cultural Competence Training of Healthcare Providers on Improving Patient Satisfaction of Minority Groups? A Systematic Review of Literature. Worldviews Evid. Based Nurs. 2016, 13, 402–410. [Google Scholar] [CrossRef]
- Wlodarczyk, D.; Chylińska, J.; Lazarewicz, M.; Rzadkiewicz, M.; Jaworski, M.; Adamus, M.; Haugan, G.; Lillefjell, M.; Espnes, G.A. Enhancing Doctors’ Competencies in Communication with and Activation of Older Patients: The Promoting Active Aging (PRACTA) Computer-Based Intervention Study. J. Med. Internet Res. 2017, 19, e45. [Google Scholar] [CrossRef]
- Jaworski, M.; Rzadkiewicz, M.; Adamus, M.; Chylinska, J.; Lazarewicz, M.; Haugan, G.; Lillefjell, M.; Espnes, G.A.; Wlodarczyk, D. Primary Care Patients’ Expectations Regarding Medical Appointments and Their Experiences During a Visit: Does Age Matter? Patient Prefer. Adherence 2017, 11, 1221–1233. [Google Scholar] [CrossRef]

| Category | Subcategory | N | % |
|---|---|---|---|
| Sex | Female | 406 | 56.00 |
| Male | 319 | 44.00 | |
| Age | 18–24 years | 80 | 11.03 |
| 25–34 years | 142 | 19.59 | |
| 35–44 years | 106 | 14.62 | |
| 45–54 years | 131 | 18.07 | |
| 55+ years | 266 | 36.69 | |
| Marital status | Miss/bachelor | 142 | 19.59 |
| Separated/divorced | 62 | 8.55 | |
| Widow/widower | 31 | 4.28 | |
| Married | 490 | 67.59 | |
| Education | Primary | 20 | 2.76 |
| Vocational | 60 | 8.28 | |
| Secondary school, no final exams | 93 | 12.83 | |
| Secondary school, with exam | 261 | 36.00 | |
| Higher | 291 | 40.14 | |
| Domicile | Very big city (500+ thousand) | 100 | 13.79 |
| Big city (100–500 thousand) | 130 | 17.93 | |
| Average city (20–99 thousand) | 152 | 20.97 | |
| Small city (under 20 thousand) | 86 | 11.86 | |
| Village | 257 | 35.45 | |
| Lives with: * | Alone | 87 | 12.00 |
| Spouse | 467 | 64.41 | |
| Children | 251 | 34.62 | |
| Grandchildren | 14 | 1.93 | |
| Other members of family | 170 | 23.45 | |
| Other persons | 15 | 2.07 | |
| Working person | 455 | 62.76 | |
| Financial situation | Good | 38 | 5.24 |
| Rather good | 173 | 23.86 | |
| Average | 379 | 52.28 | |
| Rather bad | 94 | 12.97 | |
| Bad | 41 | 5.66 | |
| Current health status | Very good | 21 | 2.90 |
| Good | 279 | 38.48 | |
| Average | 305 | 42.07 | |
| Bad | 106 | 14.62 | |
| Very bad | 14 | 1.93 | |
| Number of diseases | None | 178 | 24.55 |
| 1 disease | 237 | 32.69 | |
| 2 diseases | 177 | 24.41 | |
| 3 diseases | 94 | 12.97 | |
| More | 39 | 5.38 | |
| Type of visit | POZ/family medicine | 327 | 45.10 |
| AOS/specialised healthcare | 398 | 54.90 | |
| Category | Subcategory | Sum (M ± SD) | Statistic (t-Test or ANOVA) | p-Value (sum) | Overall Rating (M ± SD) | Statistic (t-Test or ANOVA | p-Value (Overall Rating) |
|---|---|---|---|---|---|---|---|
| Sex | Female | 80.43 ± 19.20 | −0.02 | 0.98 | 7.37 ± 2.48 | −0.49 | 0.62 |
| Male | 80.46 ± 18.85 | 7.46 ± 2.16 | |||||
| Age | 18–24 years | 78.75 ± 20.13 | 1.36 | 0.25 | 7.11 ± 2.37 | 1.24 | 0.29 |
| 25–34 years | 80.04 ± 20.44 | 7.25 ± 2.19 | |||||
| 35–44 years | 81.46 ± 16.84 | 7.47 ± 2.18 | |||||
| 45–54 years | 77.82 ± 18.75 | 7.27 ± 2.44 | |||||
| 55+ years | 82.06 ± 18.83 | 7.64 ± 2.41 | |||||
| Marital status | Miss/bachelor | 77.51 ± 20.20 | 2.30 | 0.08 | 7.11 ± 2.37 | 1.87 | 0.13 |
| Separated/divorced | 84.89 ± 20.47 | 7.94 ± 2.38 | |||||
| Widow/widower | 81.23 ± 18.42 | 7.58 ± 2.66 | |||||
| Married | 80.68 ± 18.46 | 7.42 ± 2.30 | |||||
| Education | Primary | 81.45 ± 17.86 | 0.52 | 0.73 | 7.90 ± 2.17 | 0.64 | 0.64 |
| Vocational | 79.77 ± 21.76 | 7.43 ± 2.26 | |||||
| Secondary school, no final exams | 81.91 ± 19.13 | 7.46 ± 2.11 | |||||
| Secondary school, with exam | 79.26 ± 19.21 | 7.25 ± 2.49 | |||||
| Higher | 81.11 ± 18.38 | 7.50 ± 2.30 | |||||
| Domicile | Very big city (500+ thousand) | 79.52 ± 18.31 | 0.46 | 0.76 | 7.28 ± 2.47 | 0.73 | 0.57 |
| Big city (100–500 thousand) | 80.80 ± 20.36 | 7.18 ± 2.46 | |||||
| Average city (20–99 thousand) | 78.96 ± 17.78 | 7.44 ± 2.15 | |||||
| Small city (under 20 thousand) | 81.65 ± 20.00 | 7.67 ± 2.27 | |||||
| Village | 81.10 ± 19.09 | 7.48 ± 2.37 | |||||
| Lives alone | No | 80.74 ± 18.71 | 1.03 | 0.26 | 7.46 ± 2.29 | 1.41 | 0.16 |
| Yes | 78.28 ± 21.24 | 7.08 ± 2.67 | |||||
| Lives with spouse | No | 79.21 ± 20.94 | −1.24 | 0.19 | 7.31 ± 2.49 | −0.91 | 0.36 |
| Yes | 81.13 ± 17.89 | 7.47 ± 2.25 | |||||
| Lives with children | No | 80.39 ± 19.79 | −0.12 | 0.91 | 7.34 ± 2.41 | −1.18 | 0.24 |
| Yes | 80.56 ± 17.56 | 7.55 ± 2.19 | |||||
| Lives with grandchildren | No | 80.50 ± 19.08 | 0.56 | 0.61 | 7.41 ± 2.34 | −0.37 | 0.71 |
| Yes | 77.86 ± 17.37 | 7.64 ± 2.56 | |||||
| Lives with other family members | No | 79.98 ± 18.23 | −1.09 | 0.23 | 7.34 ± 2.31 | −1.42 | 0.16 |
| Yes | 81.96 ± 21.46 | 7.64 ± 2.43 | |||||
| Lives with other people | No | 80.41 ± 19.05 | −0.35 | 0.73 | 7.40 ± 2.35 | −0.65 | 0.52 |
| Yes | 82.13 ± 18.85 | 7.80 ± 1.47 | |||||
| Working person | No | 81.17 ± 19.96 | 0.77 | 0.43 | 7.43 ± 2.32 | 0.66 | 0.51 |
| Yes | 80.02 ± 18.48 | 7.18 ± 2.69 | |||||
| Financial situation | Good | 83.39 ± 19.43 | 1.46 | 0.21 | 7.42 ± 2.48 | 3.56 | 0.01 |
| Rather good | 81.35 ± 18.00 | 7.75 ± 2.11 | |||||
| Average | 80.18 ± 19.49 | 7.43 ± 2.27 | |||||
| Rather bad | 77.06 ± 16.87 | 6.64 ± 2.66 | |||||
| Bad | 84.05 ± 22.64 | 7.59 ± 2.70 | |||||
| Current health status | Very good | 80.81 ± 18.12 | 0.59 | 0.66 | 7.52 ± 2.23 | 1.92 | 0.11 |
| Good | 81.49 ± 18.45 | 7.58 ± 2.15 | |||||
| Average | 79.60 ± 19.14 | 7.32 ± 2.35 | |||||
| Bad | 80.70 ± 19.92 | 7.39 ± 2.62 | |||||
| Very bad | 75.57 ± 23.53 | 5.93 ± 3.27 | |||||
| Number of diseases | None | 77.75 ± 18.89 | 1.53 | 0.19 | 7.11 ± 2.31 | 1.09 | 0.36 |
| 1 disease | 80.45 ± 18.87 | 7.51 ± 2.21 | |||||
| 2 diseases | 82.54 ± 19.69 | 7.55 ± 2.34 | |||||
| 3 diseases | 81.71 ± 18.24 | 7.40 ± 2.62 | |||||
| More | 80.15 ± 19.06 | 7.62 ± 2.50 | |||||
| Type of visit | POZ | 77.52 ± 19.04 | −3.78 | <0.001 | 7.20 ± 2.30 | −2.23 | 0.03 |
| AOS | 82.85 ± 18.71 | 7.59 ± 2.36 |
| During the Visit, the Doctor | AOS M ± SD | POZ M ± SD | Statistic t-test | p-Value |
|---|---|---|---|---|
| found the cause of my symptoms | 4.85 ± 1.85 | 4.68 ± 1.70 | −1.35 | 0.071 |
| presented me a probable further course of treatment | 5.38 ± 1.66 | 4.79 ± 1.76 | −4.59 | 0.000 |
| discussed the possible consequences of the disease | 4.87 ± 1.85 | 4.46 ± 1.86 | −2.94 | 0.002 |
| presented the results of the research conducted | 5.51 ± 1.62 | 4.80 ± 1.84 | −5.45 | 0.000 |
| gave me advice about the medicines I take | 5.18 ± 1.79 | 4.87 ± 1.79 | −2.34 | 0.008 |
| presented treatment recommendations | 5.59 ± 1.49 | 5.06 ± 1.68 | −4.48 | 0.000 |
| talked to me about how I was feeling and how I was coping | 4.97 ± 1.87 | 4.52 ± 1.95 | −3.16 | 0.001 |
| encouraged me | 4.70 ± 1.87 | 4.34 ± 1.81 | −2.64 | 0.004 |
| showed me concern | 5.15 ± 1.69 | 4.69 ± 1.76 | −3.57 | 0.000 |
| talked to me about what was harmful to my health | 4.11 ± 2.03 | 3.75 ± 2.04 | −2.37 | 0.018 |
| advised me what I could do to improve my functioning in everyday life | 4.14 ± 2.04 | 3.87 ± 1.99 | −1.76 | 0.078 |
| encouraged me to introduce favourable changes | 4.13 ± 2.01 | 3.90 ± 2.06 | −1.49 | 0.141 |
| suggested how to maintain contacts with other people | 3.87 ± 2.01 | 3.84 ± 2.00 | −0.21 | 0.835 |
| talked to me about how I can spend my time actively | 3.72 ± 2.00 | 3.91 ± 2.04 | 1.22 | 0.216 |
| told me how to maintain life satisfaction | 3.73 ± 1.98 | 3.91 ± 2.04 | 1.20 | 0.232 |
| was kind towards me | 4.31 ± 2.03 | 4.04 ± 2.01 | −1.75 | 0.077 |
| treated me seriously | 4.36 ± 2.06 | 4.00 ± 2.09 | −2.30 | 0.022 |
| showed me respect | 4.23 ± 1.99 | 4.09 ± 2.03 | −1.29 | 0.196 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pochrzęst-Motyczyńska, A.; Ostrowski, J.; Sys, D.; Pinkas, J.; Religioni, U. Patient Satisfaction in Primary and Specialised Ambulatory Healthcare: A Web-Based Cross-Sectional Study in the Polish Population. Healthcare 2025, 13, 1147. https://doi.org/10.3390/healthcare13101147
Pochrzęst-Motyczyńska A, Ostrowski J, Sys D, Pinkas J, Religioni U. Patient Satisfaction in Primary and Specialised Ambulatory Healthcare: A Web-Based Cross-Sectional Study in the Polish Population. Healthcare. 2025; 13(10):1147. https://doi.org/10.3390/healthcare13101147
Chicago/Turabian StylePochrzęst-Motyczyńska, Agnieszka, Janusz Ostrowski, Dorota Sys, Jarosław Pinkas, and Urszula Religioni. 2025. "Patient Satisfaction in Primary and Specialised Ambulatory Healthcare: A Web-Based Cross-Sectional Study in the Polish Population" Healthcare 13, no. 10: 1147. https://doi.org/10.3390/healthcare13101147
APA StylePochrzęst-Motyczyńska, A., Ostrowski, J., Sys, D., Pinkas, J., & Religioni, U. (2025). Patient Satisfaction in Primary and Specialised Ambulatory Healthcare: A Web-Based Cross-Sectional Study in the Polish Population. Healthcare, 13(10), 1147. https://doi.org/10.3390/healthcare13101147







