The Impact of Toothbrushing on Oral Health, Gingival Recession, and Tooth Wear—A Narrative Review
Abstract
1. Introduction
2. Methodology
3. Toothbrushing Effects on Hard/Soft Issue
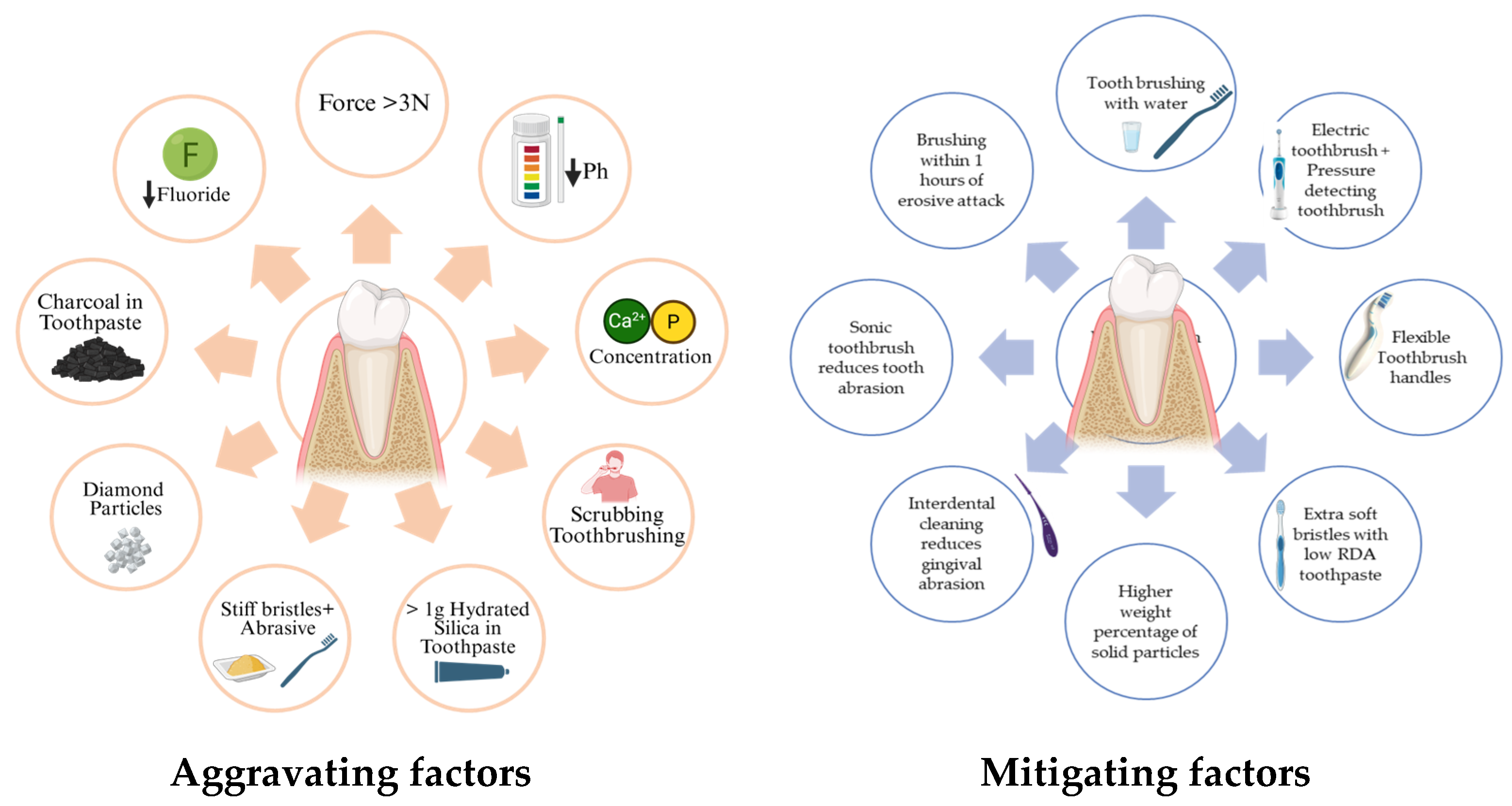
4. Patient-Related Factors Associated with Tooth Wear
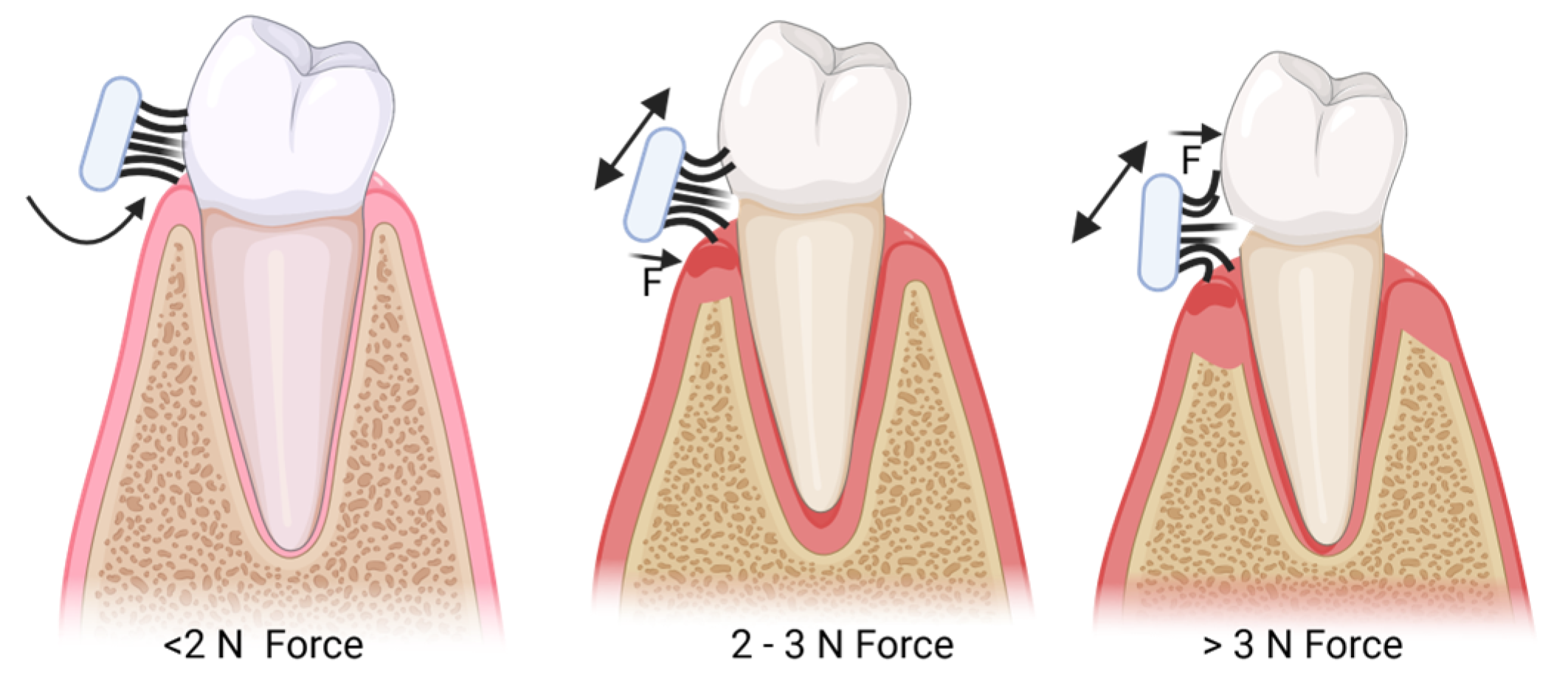
4.1. Brushing Force
| Author and Year | Aim | Study Type, Sample Size, Pressure/Force | Outcome |
|---|---|---|---|
| Souza C et al. (2021) [13] | Manual toothbrushes’ brushing loads on the progression of erosive tooth wear (ETW) on enamel. | In vitro 60 bovine incisors allocated into 6 groups and divided into 6 different toothbrushes. Brushing load of 3 N and 1.5 N forces. | Hard brushes are not recommended for use by patients with erosive tooth wear. |
| Bizhang M et al. (2017) [19] | Susceptibility of dentin to brushing abrasion using four different toothbrushes with the same brushing forces. | In vitro 72 impacted third molars; rotating–oscillating, sonic, and two types of manual toothbrushes. Brushing force was set to 2 N (260 min of brushing). | Manual toothbrushes are significantly less abrasive compared to powered toothbrushes in a 8.5-year simulation. |
| Rosema et al. (2014) [18] | Manual toothbrush and an oscillating–rotating toothbrush. Compare groups in terms of both the level of existing gingival recession and the extent of gingival abrasion before and after a single toothbrushing exercise. | Cross-sectional Uncontrolled epidemiological study with 181 participants ranging from 18 to 35 years. | The powered toothbrush is as safe as a manual one. The force exerted by the powered toothbrush is lower than that of the manual one. |
| Wiegand A et al. (2013) [4] | Determine and compare the brushing forces with manual and sonic toothbrushes; brushing forces on abrasion of sound and eroded enamel and dentin. | In vivo 27 Volunteers (5 males and 22 females; 18–55 Years); one manual and two sonic toothbrushes. | Manual toothbrush, 1.6 ± 0.3 N; sonic toothbrush, 0.9 ± 0.2 N. The manual toothbrush caused the highest abrasion of sound and eroded dentin; patients with severe tooth wear and exposed (eroded) dentin surfaces should use sonic toothbrushes. |
4.2. Brushing Technique
5. Toothbrush-Related Factors Influencing Tooth Surface Wear
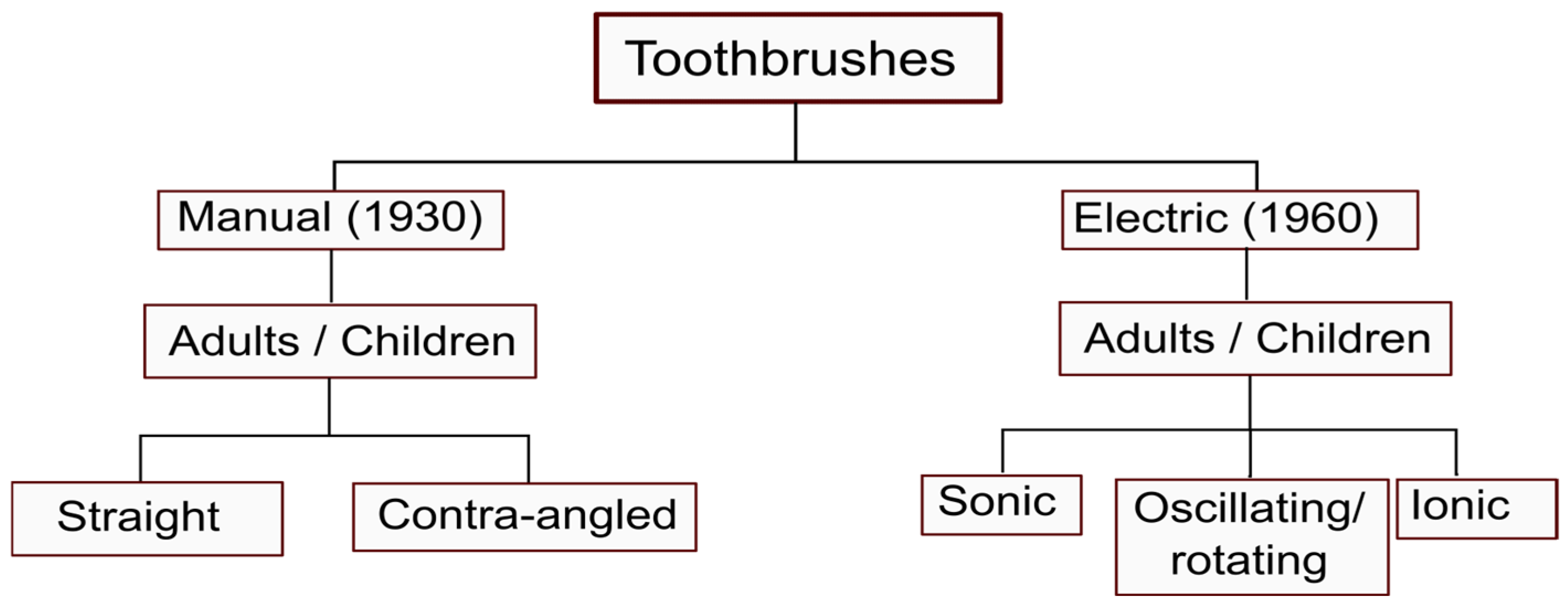
5.1. Toothbrush
5.2. Handle
5.3. Bristles (Filaments)
| Bristle Type | Diameter | Authors |
|---|---|---|
| Ultrasoft | 0.09–0.11 mm | Souza C [13] |
| Soft | 0.15–0.2 mm | Burgett F, Souza C, Fraleigh C, Bizhang M [10,12,13,17] |
| Medium | 0.18–0.19 mm | Fraleigh C, Souza C [13,32] |
| Hard | 0.20–0.30 mm | Burgett F, Fraleigh C Souza C [10,13,32] |
5.4. Electric vs. Manual Toothbrushes
5.5. Toothpastes
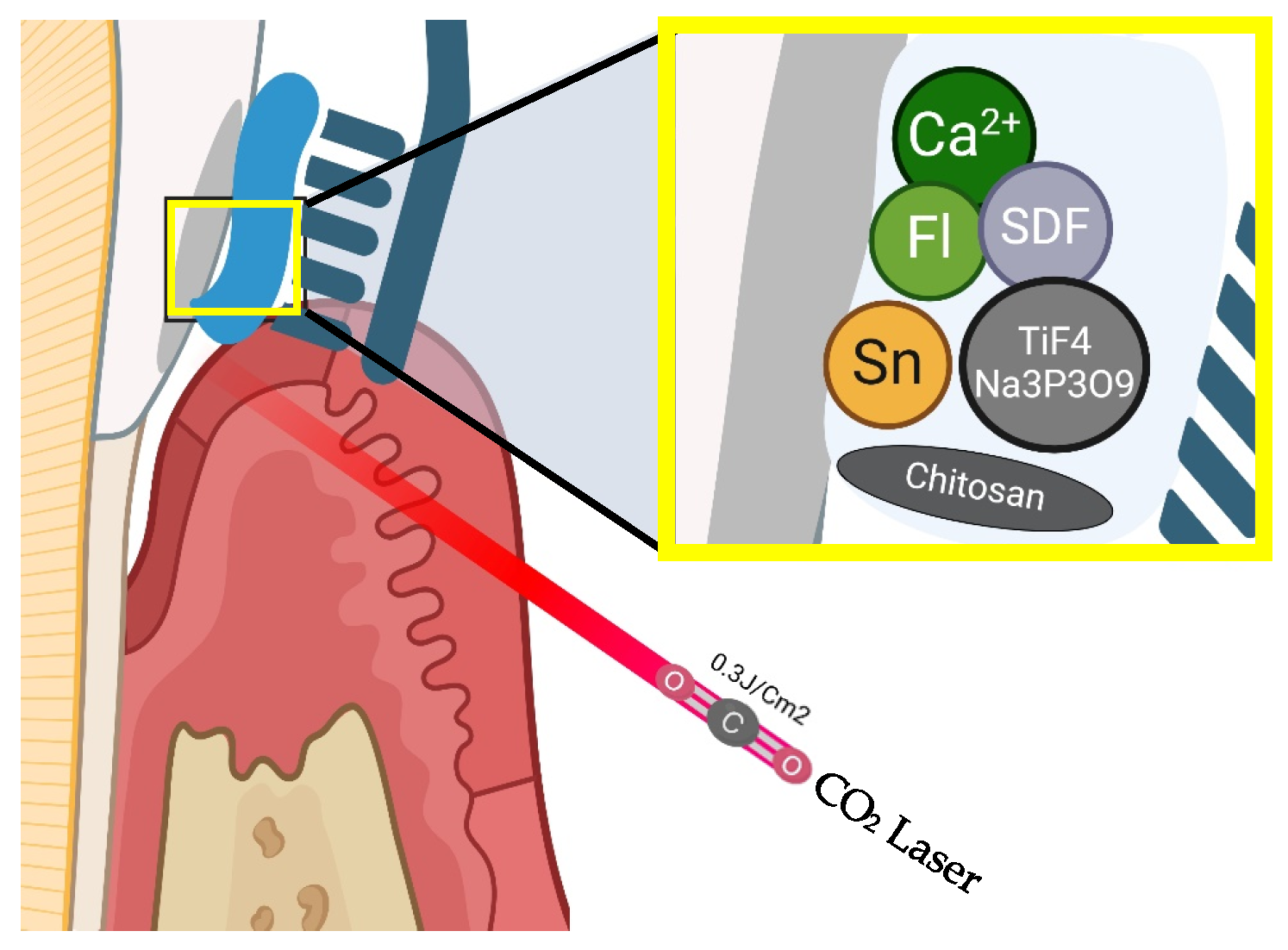
6. Management
| Author and Year | Aim | Study Type, Sample Size | Outcome |
|---|---|---|---|
| Systematic reviews | |||
| Tomás, D.B.M. et al. (2023) [117] | Qualitative synthesis of the available literature on the use of activated charcoal-based toothpaste for tooth whitening. | Out of 208 articles, 11 met the inclusion criteria, the risk of bias of the selected studies was determined as medium–high. | Most studies agree that activated charcoal toothpaste has a higher abrasive potential. |
| Van der Weijden, F et al. (2022) [103] | Efficacy of a rubber-bristled interdental cleaner (RBIC) as an adjunct to toothbrushing (TB) compared to other interdental cleaning devices on plaque and gingivitis parameters. | The search retrieved 142 unique papers; 6 studies with 10 comparisons were included in a descriptive analysis. Five RCTs compared RBICs with interdental brushes (IDBs), four with dental floss (DF) and one with manual TBs only. | A weak certainty exists that a RBIC is indicated for gingivitis and plaque reduction. |
| Jamwal, N et al. (2022) [85] | The relationship between whitening toothpastes and surface roughness as well as the microhardness of human teeth. | A total of 125 articles were obtained through a key word search. After duplicate removal and title screening, 17 articles were eligible for full-text review. Finally, 7 studies were included for systematic review, and meta-analysis was conducted on 4 studies. | Whitening toothpaste lightens the tooth color but can cause increases in surface microroughness. |
| Ranzan, N et al. (2019) [42] | To examine soft tissue lesions caused by different bristle stiffnesses and bristle end shapes in manual toothbrushes in adult individuals. | Thirteen studies were included from 1945 initially retrieved papers. The toothbrush bristle end shape was investigated in six studies and bristle stiffness in two, and both features were investigated in five studies. | Soft and extra-soft toothbrushes tend to be safer. Oral lesions are similar in tapered and round-ended bristles. |
| Muller-Bolla, M.; Courson, F. (2013) [24] | The most effective technique of toothbrushing in children. | The level of evidence was moderate and 6 out of 534 articles were included. | The horizontal technique was the most effective up to 6–7 years of age. |
| Randomized clinical trials | |||
| Sutor, S et al. (2025) [45] | Powered toothbrush (PT) on the size and number of pre-existing gingival recessions (GR) in comparison to a manual toothbrush (MT). | Prospective, single-blind, parallel-group, randomized controlled clinical study. In total, 87 out of 92 participants completed the study (MT/PT: n = 42/n = 45). GR ≥ 2 mm; twice daily brushing with a manual or power toothbrush. Primary outcome–mean change in GR over 36 months. | PT seems to be favorable in patients with pre exiting gingival recession. |
| Hennequin-Hoenderdos, N.L et al. (2018) [104] | Efficacy of a rubber-bristled interdental cleaner (RBIC) compared to an interdental brush (IDB) in reducing gingivitis. | Two-treatment, parallel, split-mouth, examiner-blind RCT, evaluating the reversal of experimental gingivitis in 46 healthy patients. | A RBIC, in conjunction with manual toothbrushing, was found to be more effective in reducing gingival inflammation after 4 weeks. The RBIC caused less abrasion of the gingiva and was appreciated more by the participants. |
| Graetz, C et al. (2017) [46] | Link between bristle splaying and gingival recession. | A parallel-group, randomized, controlled, clinical trial, With 110 healthy participants, pre-existing gingival recessions, and a 12-month duration; manual (MT) vs. powered toothbrush (PT). Wear was measured using the Bristle Splaying Index (BSI). | After 3 months, the PT group demonstrated a lower BSI than the MT group. Greater bristle splaying was associated with a higher risk of increase in GR in subjects using a MT but not a PT. |
| N L -Hoenderdos et al. (2017) [118] | Filament end-rounding and gingival abrasion. |
Crossover, split-mouth, contralateral, double-blinded, randomized design with 46 healthy participants. Oral soft tissue and gingival abrasion were assessed. | If the brushes have 40–50% of bristles with end roundedness it can provide greater reduction in gingival abrasion. |
| Dörfer, C.E et al. (2016) [47] | Oscillating–rotating power toothbrush or an ADA reference manual toothbrush on pre-existing gingival recession. | Controlled, prospective, single-blind, parallel-group study; healthy subjects with pre-existing recession were randomized and brushed with a power toothbrush (n = 55) or an ADA reference manual toothbrush (n = 54) for a 3-year study period. | Recession significantly reduced after 3 years of brushing with either of the toothbrushes. |
| Sälzer, S et al. (2016) [48] | Effect of brushing with either a multidirectional PT or American Dental Association reference manual toothbrush (MT) on mid-buccal preexisting GR (PreGR). | 12-month prospective, single-masked, parallel-group, randomized, controlled clinical study. 107 participants without periodontitis with at least two teeth showing PreGR ≥ 2 mm were randomized to a group brushing with either an manual or powered toothbrush. | Neither the PT nor MT led to an increase in PreGR during 12 months of daily use. |
| Greggianin, B.F et al. (2013) [43] | Incidence of gingival fissures after the use of soft and medium–hard toothbrushes. | 35 participants (14–20 years old), with periodontal attachment loss (PAL) < 1 mm, were assigned to soft or medium–hard toothbrushes in a crossover design with a wash-out of 10 days between two 28-day periods. | Gingival fissures are a common feature associated with toothbrushing. Medium–hard toothbrushes, male gender, time, and previous PAL are significant risk factors for the incidence of gingival fissures. |
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| PTB | Polybutylene terephthalate |
| ETW | Erosive tooth wear |
| REA | Relative Enamel Abrasivity |
| RDA | Relative Dentin Abrasivity |
| ADA | American Dental Association |
| RBIC | Rubber-bristled interdental cleaner |
| IDB | Interdental brush |
References
- Shah, N.; Mathur, V.; Jain, V.; Logani, A. Association between Traditional Oral Hygiene Methods with Tooth Wear, Gingival Bleeding, and Recession: A Descriptive Cross-Sectional Study. Indian J. Dent. Res. 2018, 29, 150. [Google Scholar] [CrossRef] [PubMed]
- Couteau, C.; Domejean, S.; Lecoq, M.; Ali, A.; Bernet, M.; Abbe-Denizot, A.; Coiffard, L.J.M. A Study of 84 Homemade Toothpaste Recipes and the Problems Arising from the Type of Product. Br. Dent. J. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Ganss, C.; Schlueter, N.; Preiss, S.; Klimek, J. Tooth Brushing Habits in Uninstructed Adults—Frequency, Technique, Duration and Force. Clin. Oral Investig. 2009, 13, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, A.; Burkhard, J.P.M.; Eggmann, F.; Attin, T. Brushing Force of Manual and Sonic Toothbrushes Affects Dental Hard Tissue Abrasion. Clin. Oral Investig. 2013, 17, 815–822. [Google Scholar] [CrossRef]
- Splieth, C.H.; Tachou, A. Epidemiology of Dentin Hypersensitivity. Clin. Oral Investig. 2013, 17, 3–8. [Google Scholar] [CrossRef]
- Mythri, S.; Arunkumar, S.; Hegde, S.; Rajesh, S.; Munaz, M.; Ashwin, D. Etiology and Occurrence of Gingival Recession—An Epidemiological Study. J. Indian Soc. Periodontol. 2015, 19, 671–675. [Google Scholar] [CrossRef]
- Hamza, B.; Martinola, L.; Körner, P.; Gubler, A.; Attin, T.; Wegehaupt, F.J. Effect of Brushing Force on the Abrasive Dentin Wear Using Slurries with Different Abrasivity Values. Int. J. Dent. Hyg. 2023, 21, 172–177. [Google Scholar] [CrossRef]
- Mullan, F.; Paraskar, S.; Bartlett, D.W.; Olley, R.C. Effects of Tooth-Brushing Force with a Desensitising Dentifrice on Dentine Tubule Patency and Surface Roughness. J. Dent. 2017, 60, 50–55. [Google Scholar] [CrossRef][Green Version]
- McCracken, G.I.; Janssen, J.; Swan, M.; Steen, N.; De Jager, M.; Heasman, P.A. Effect of Brushing Force and Time on Plaque Removal Using a Powered Toothbrush. J. Clin. Periodontol. 2003, 30, 409–413. [Google Scholar] [CrossRef]
- Fraleigh, C.M.; MC Elhaney, J.H.; Heiser, R.A. Toothbrushing Force Study. J. Dent. Res. 1967, 46, 209–214. [Google Scholar] [CrossRef]
- Boyd, R.L.; McLey, L.; Zahradnik, R. Clinical and Laboratory Evaluation of Powered Electric Toothbrushes: In Vivo Determination of Average Force for Use of Manual and Powered Toothbrushes. J. Clin. Dent. 1997, 8, 72–75. [Google Scholar] [PubMed]
- Burgett, F.G.; Ash, M.M. Comparative Study of the Pressure of Brushing with Three Types of Toothbrushes. J. Periodontol. 1974, 45, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.d.M.S.; Sakae, L.O.; Carneiro, P.M.A.; Esteves, R.A.; Scaramucci, T. Interplay between Different Manual Toothbrushes and Brushing Loads on Erosive Tooth Wear. J. Dent. 2021, 105, 103577. [Google Scholar] [CrossRef] [PubMed]
- Janusz, K.; Nelson, B.; Bartizek, R.D.; Walters, P.A.; Biesbrock, A.R. Impact of a Novel Power Toothbrush with SmartGuide Technology on Brushing Pressure and Thoroughness. J. Contemp. Dent. Pract. 2008, 9, 1–8. [Google Scholar]
- Heasman, P.A.; Heynderickx, I.; de Jager, M.; Sturm, D. Influence of a Controlled Pressure System on Toothbrushing Behavior. J. Clin. Dent. 2001, 12, 2–6. [Google Scholar]
- McLey, L.; Boyd, R.L.; Sarker, S. Clinical and Laboratory Evaluation of Powered Electric Toothbrushes: Laboratory Determination of Relative Abrasion of Three Powered Toothbrushes. J. Clin. Dent. 1997, 8, 76–80. [Google Scholar]
- Bizhang, M.; Riemer, K.; Arnold, W.H.; Domin, J.; Zimmer, S. Influence of Bristle Stiffness of Manual Toothbrushes on Eroded and Sound Human Dentin—An In Vitro Study. PLoS ONE 2016, 11, e0153250. [Google Scholar] [CrossRef]
- Rosema, N.; Adam, R.; Grender, J.; Van der Sluijs, E.; Supranoto, S.; Van der Weijden, G. Gingival Abrasion and Recession in Manual and Oscillating–Rotating Power Brush Users. Int. J. Dent. Hyg. 2014, 12, 257–266. [Google Scholar] [CrossRef]
- Bizhang, M.; Schmidt, I.; Chun, Y.-H.P.; Arnold, W.H.; Zimmer, S. Toothbrush Abrasivity in a Long-Term Simulation on Human Dentin Depends on Brushing Mode and Bristle Arrangement. PLoS ONE 2017, 12, e0172060. [Google Scholar] [CrossRef]
- Ganss, C.; Hardt, M.; Blazek, D.; Klimek, J.; Schlueter, N. Effects of Toothbrushing Force on the Mineral Content and Demineralized Organic Matrix of Eroded Dentine. Eur. J. Oral Sci. 2009, 117, 255–260. [Google Scholar] [CrossRef]
- Hayasaki, H.; Saitoh, I.; Nakakura-Ohshima, K.; Hanasaki, M.; Nogami, Y.; Nakajima, T.; Inada, E.; Iwasaki, T.; Iwase, Y.; Sawami, T.; et al. Tooth Brushing for Oral Prophylaxis. Jpn. Dent. Sci. Rev. 2014, 50, 69–77. [Google Scholar] [CrossRef]
- Ganesh, M.; Shah, S.; Parikh, D.; Choudhary, P.; Bhaskar, V. The Effectiveness of a Musical Toothbrush for Dental Plaque Removal: A Comparative Study. J. Indian Soc. Pedod. Prev. Dent. 2012, 30, 139. [Google Scholar] [CrossRef] [PubMed]
- Padbury, A.D.; Ash, M.M. Abrasion Caused by Three Methods of Toothbrushing. J. Periodontol. 1974, 45, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Muller-Bolla, M.; Courson, F. Toothbrushing Methods to Use in Children: A Systematic Review. Oral Health Prev. Dent. 2013, 11, 341–347. [Google Scholar] [CrossRef]
- Geyer, R.; Jambeck, J.R.; Law, K.L. Production, Use, and Fate of All Plastics Ever Made. Sci. Adv. 2017, 3, e1700782. [Google Scholar] [CrossRef]
- Kaneyasu, Y.; Shigeishi, H.; Ohta, K.; Sugiyama, M. Analysis of the Deflection, Bristle Splaying, and Abrasion of a Single Tuft of a Polybutylene Terephthalate Toothbrush after Use: A Randomized Controlled Trial. Materials 2022, 15, 4890. [Google Scholar] [CrossRef]
- Vowles, A.D.; Wade, A.B. Importance of Filament Diameter When Using Bass Brushing Technique. J. Periodontol. 1977, 48, 460–463. [Google Scholar] [CrossRef]
- Tellefsen, G.; Liljeborg, A.; Johannsen, A.; Johannsen, G. The Role of the Toothbrush in the Abrasion Process. Int. J. Dent. Hyg. 2011, 9, 284–290. [Google Scholar] [CrossRef]
- Alzahrani, L.; Denucci, G.C.; Lippert, F.; Al Dehailan, L.; Bhamidipalli, S.S.; Hara, A.T. Impact of Toothbrush Head Configuration and Dentifrice Abrasivity on Non-Carious Cervical Lesions in-Vitro. J. Dent. 2024, 140, 104798. [Google Scholar] [CrossRef]
- Mishra, D.; Moothedath, M.; Maben, S.; Sahoo, N.; Bhola, L.; Unnikrishnan, K.R.; Chinnannavar, S.N.; Kuruvilla, L. In Vitro Assessment of Different Toothbrush Designs on Enamel Surface Abrasion: A Profilometric Study. J. Contemp. Dent. Pract. 2023, 24, 757–760. [Google Scholar] [CrossRef]
- Pereira, T.P.; Vieira, T.A.F.; dos Santos, W.; Bezerra, S.J.C.; Sobral, M.Â.P.; Scaramucci, T. Influence of Different Ultra-Soft Toothbrushes on Erosive Tooth Wear. J. Dent. 2023, 132, 104502. [Google Scholar] [CrossRef] [PubMed]
- Dyer, D.; Addy, M.; Newcombe, R.G. Studies in Vitro of Abrasion by Different Manual Toothbrush Heads and a Standard Toothpaste. J. Clin. Periodontol. 2000, 27, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Wetselaar, P.; Lobbezoo, F. The Tooth Wear Evaluation System: A Modular Clinical Guideline for the Diagnosis and Management Planning of Worn Dentitions. J. Oral Rehabil. 2016, 43, 69–80. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, G.; de Aveiro, J.; Pavone, C.; Marcantonio, R. Influence of Different Toothpaste Abrasives on the Bristle End-Rounding Quality of Toothbrushes. Int. J. Dent. Hyg. 2015, 13, 18–24. [Google Scholar] [CrossRef]
- Zimmer, S.; Öztürk, M.; Barthel, C.R.; Bizhang, M.; Jordan, R.A. Cleaning Efficacy and Soft Tissue Trauma After Use of Manual Toothbrushes with Different Bristle Stiffness. J. Periodontol. 2011, 82, 267–271. [Google Scholar] [CrossRef]
- Sgan-Cohen, H.D.; Vered, Y. Plaque Removal and Oral Health Promotion Potential for the Elmex InterX Medium Toothbrush: Clinical Efficacy and Safety Evaluation. J. Clin. Dent. 2003, 14, 70–73. [Google Scholar]
- Rosing, C.K.; Cavagni, J.; Gaio, E.J.; Muniz, F.W.M.G.; Oballe, H.J.R.; Ranzan, N.; Friedrich, S.A.; Severo, R.M.; Gittins, E.; Stewart, B.; et al. Efficacy of Two Soft-Bristle Toothbrushes in Plaque Removal: A Randomized Controlled Trial. Braz. Oral Res. 2016, 30, e134. [Google Scholar] [CrossRef]
- Sgan-Cohen, H.D.; Livny, A.; Vered, Y. The Elmex SENSITIVE Toothbrush: Effect on Plaque Reduction and Subjective Satisfaction after Two Months. J. Clin. Dent. 2008, 19, 22–27. [Google Scholar]
- Harpenau, L.; Meyers, G.; Lyon, C.; Chambers, D.; Lundergan, W. Blinded Clinical Evaluation of a New Manual Toothbrush. J. Clin. Dent. 2006, 17, 1–4. [Google Scholar]
- Sharma, N.C.; Qaqish, J.G.; Galustians, H.J.; King, D.W.; Low, M.A.; Jacobs, D.M.; Weber, D.A. A 3-Month Comparative Investigation of the Safety and Efficacy of a New Toothbrush: Results from Two Independent Clinical Studies. Am. J. Dent. 2000, 13, 27A–32A. [Google Scholar]
- Ren, Y.-F.; Cacciato, R.; Whelehan, M.T.; Ning, L.; Malmstrom, H.S. Effects of Toothbrushes with Tapered and Cross Angled Soft Bristle Design on Dental Plaque and Gingival Inflammation: A Randomized and Controlled Clinical Trial. J. Dent. 2007, 35, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Ranzan, N.; Muniz, F.W.M.G.; Rösing, C.K. Are Bristle Stiffness and Bristle End-Shape Related to Adverse Effects on Soft Tissues during Toothbrushing? A Systematic Review. Int. Dent. J. 2019, 69, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Greggianin, B.F.; Oliveira, S.C.; Haas, A.N.; Oppermann, R.V. The Incidence of Gingival Fissures Associated with Toothbrushing: Crossover 28-Day Randomized Trial. J. Clin. Periodontol. 2013, 40, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Voelker, M.A.; Bayne, S.C.; Liu, Y.; Walker, M.P. Catalogue of Tooth Brush Head Designs. J. Dent. Hyg. 2013, 87, 118–133. [Google Scholar]
- Sutor, S.; Graetz, C.; Geiken, A.; Straßburger, M.; Löwe, C.; Holtmann, B.; Conrad, J.; Sälzer, S.; Dörfer, C.E. Effect of a Powered and a Manual Toothbrush in Subjects Susceptible to Gingival Recession: A 36-month Randomized Controlled Clinical Study. Int. J. Dent. Hyg. 2025, 23, 26–36. [Google Scholar] [CrossRef]
- Graetz, C.; Plaumann, A.; Heinevetter, N.; Sälzer, S.; Bielfeldt, J.; Dörfer, C.E. Bristle Splaying and Its Effect on Pre-Existing Gingival Recession-a 12-Month Randomized Controlled Trial. Clin. Oral Investig. 2017, 21, 1989–1995. [Google Scholar] [CrossRef]
- Dörfer, C.E.; Staehle, H.J.; Wolff, D. Three-Year Randomized Study of Manual and Power Toothbrush Effects on Pre-Existing Gingival Recession. J. Clin. Periodontol. 2016, 43, 512–519. [Google Scholar] [CrossRef]
- Sälzer, S.; Graetz, C.; Plaumann, A.; Heinevetter, N.; Grender, J.; Klukowska, M.; Schneider, C.A.; Springer, C.; Van der Weijden, F.A.; Dörfer, C.E. Effect of a Multidirectional Power Toothbrush and a Manual Toothbrush in Individuals Susceptible to Gingival Recession: A 12-Month Randomized Controlled Clinical Study. J. Periodontol. 2016, 87, 548–556. [Google Scholar] [CrossRef]
- Hamza, B.; Uka, E.; Körner, P.; Attin, T.; Wegehaupt, F.J. Effect of a Sonic Toothbrush on the Abrasive Dentine Wear Using Toothpastes with Different Abrasivity Values. Int. J. Dent. Hyg. 2021, 19, 407–412. [Google Scholar] [CrossRef]
- Heasman, P.A.; Holliday, R.; Bryant, A.; Preshaw, P.M. Evidence for the Occurrence of Gingival Recession and Non-carious Cervical Lesions as a Consequence of Traumatic Toothbrushing. J. Clin. Periodontol. 2015, 42 (Suppl. S16), S237–S255. [Google Scholar] [CrossRef]
- Maldupa, I.; Brinkmane, A.; Rendeniece, I.; Mihailova, A. Evidence Based Toothpaste Classification, According to Certain Characteristics of Their Chemical Composition. Stomatologija 2012, 14, 12–22. [Google Scholar] [PubMed]
- Ferreira, M.C.; Ramos-Jorge, M.L.; Delbem, A.C.B.; Vieira, R.S. Effect of Toothpastes with Different Abrasives on Eroded Human Enamel: An in Situ/Ex Vivo Study. Open Dent. J. 2013, 7, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Almansour, A.; Addison, O.; Bartlett, D. The Effect of Location/Site on Polished Human Enamel after Mechanical and Chemical Wear. J. Dent. 2024, 141, 104803. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Kim, S.; Park, Y.-S. Effects of a Commercial Whitening Toothpaste Containing Hydrogen Peroxide and Citric Acid on Dentin Abrasion and Erosion. BMC Oral Health 2023, 23, 619. [Google Scholar] [CrossRef]
- Council on Dental Therapeutics. Abrasivity of Current Dentifrices. J. Am. Dent. Assoc. 1970, 81, 1177–1178. [Google Scholar] [CrossRef]
- Hunter, M.L.; Addy, M.; Pickles, M.J.; Joiner, A. The Role of Toothpastes and Toothbrushes in the Aetiology of Tooth Wear. Int. Dent. J. 2002, 52, 399–405. [Google Scholar] [CrossRef]
- Gyurkovics, M.; Baumann, T.; Carvalho, T.S.; Assunção, C.M.; Lussi, A. In Vitro Evaluation of Modified Surface Microhardness Measurement, Focus Variation 3D Microscopy and Contact Stylus Profilometry to Assess Enamel Surface Loss after Erosive-Abrasive Challenges. PLoS ONE 2017, 12, e0175027. [Google Scholar] [CrossRef]
- Dobler, L.; Hamza, B.; Attin, T.; Wegehaupt, F.J. Abrasive Enamel and Dentin Wear Resulting from Brushing with Toothpastes with Highly Discrepant Relative Enamel Abrasivity (REA) and Relative Dentin Abrasivity (RDA) Values. Oral Health Prev. Dent. 2023, 21, 41–48. [Google Scholar] [CrossRef]
- Sakae, L.O.; Renzo, A.L.M.; Viana, Í.E.L.; Niemeyer, S.H.; Carvalho, T.S.; Scaramucci, T. Impact of Different Brushing/Abrasion Protocols on Erosive Tooth Wear for in Vitro Studies. Arch. Oral Biol. 2023, 148, 105657. [Google Scholar] [CrossRef]
- Fischer, M.; Schlueter, N.; Rupf, S.; Ganss, C. In Vitro Evaluation of the Effects of Different Particle Types in Toothpastes on the Efficacy against Enamel Erosion and Wear. Sci. Rep. 2022, 12, 9627. [Google Scholar] [CrossRef]
- Ganss, C.; Marten, J.; Hara, A.T.; Schlueter, N. Toothpastes and Enamel Erosion/Abrasion—Impact of Active Ingredients and the Particulate Fraction. J. Dent. 2016, 54, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Sarembe, S.; Ufer, C.; Kiesow, A.; Limeback, H.; Meyer, F.; Fuhrmann, I.; Enax, J. Influence of the Amount of Toothpaste on Cleaning Efficacy: An In Vitro Study. Eur. J. Dent. 2023, 17, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Enax, J.; Meyer, F.; Schulze zur Wiesche, E.; Fuhrmann, I.C.; Fabritius, H.-O. Toothpaste Abrasion and Abrasive Particle Content: Correlating High-Resolution Profilometric Analysis with Relative Dentin Abrasivity (RDA). Dent. J. 2023, 11, 79. [Google Scholar] [CrossRef] [PubMed]
- Hara, A.T.; Turssi, C.P. Baking Soda as an Abrasive in Toothpastes. J. Am. Dent. Assoc. 2017, 148, S27–S33. [Google Scholar] [CrossRef]
- Wiegand, A.; Schneider, S.; Sener, B.; Roos, M.; Attin, T. Stability against Brushing Abrasion and the Erosion-Protective Effect of Different Fluoride Compounds. Caries Res. 2014, 48, 154–162. [Google Scholar] [CrossRef]
- Luka, B.; Duerrschnabel, A.; Neumaier, S.; Schlueter, N.; Vach, K. Interaction between Hexametaphosphate, Other Active Ingredients of Toothpastes, and Erosion-Abrasion in Enamel in Vitro. Caries Res. 2023, 57, 265–275. [Google Scholar] [CrossRef]
- Wegehaupt, F.J.; Attin, T. The Role of Fluoride and Casein Phosphopeptide/Amorphous Calcium Phosphate in the Prevention of Erosive/Abrasive Wear in an in Vitro Model Using Hydrochloric Acid. Caries Res. 2010, 44, 358–363. [Google Scholar] [CrossRef]
- Hamza, B.; Attin, T.; Cucuzza, C.; Gubler, A.; Wegehaupt, F.J. RDA and REA Values of Commercially Available Toothpastes Utilising Diamond Powder and Traditional Abrasives. Oral Health Prev. Dent. 2020, 18, 807–814. [Google Scholar] [CrossRef]
- Zhao, Y.-L.; Yang, D.-S. Brushing Abrasion of Eroded Enamel Using Bioactive Glass Toothpaste in Different Time after Acid Etching. Chin. J. Tissue Eng. Res. 2015, 19, 4022–4026. [Google Scholar] [CrossRef]
- Kodaka, T.; Kobori, M.; Hirayama, A.; Masayuki, A. Abrasion of Human Enamel by Brushing with a Commercial Dentifrice Containing Hydroxyapatite Crystals in Vitro. J. Electron. Microsc. 1999, 48, 167–172. [Google Scholar] [CrossRef]
- Wiegand, A.; Schwerzmann, M.; Sener, B.; Carolina Magalhães, A.; Roos, M.; Ziebolz, D.; Imfeld, T.; Attin, T. Impact of Toothpaste Slurry Abrasivity and Toothbrush Filament Stiffness on Abrasion of Eroded Enamel—An in Vitro Study. Acta Odontol. Scand. 2008, 66, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Turssi, C.P.; Binsaleh, F.; Lippert, F.; Bottino, M.C.; Eckert, G.J.; Moser, E.A.S.; Hara, A.T. Interplay between Toothbrush Stiffness and Dentifrice Abrasivity on the Development of Non-Carious Cervical Lesions. Clin. Oral Investig. 2019, 23, 3551–3556. [Google Scholar] [CrossRef]
- Sabrah, A.H.; Turssi, C.P.; Lippert, F.; Eckert, G.J.; Kelly, A.B.; Hara, A.T. 3D-Image Analysis of the Impact of Toothpaste Abrasivity on the Progression of Simulated Non-Carious Cervical Lesions. J. Dent. 2018, 73, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, A.; Mneimne, M.; Zou, L.F.; Hill, R.G.; Gillam, D.G. Abrasive Wear of Enamel by Bioactive Glass-Based Toothpastes. Am. J. Dent. 2014, 27, 263–267. [Google Scholar] [PubMed]
- Rodriguez, J.M.; Bartlett, D.W. A Comparison of Two-Dimensional and Three-Dimensional Measurements of Wear in a Laboratory Investigation. Dent. Mater. 2010, 26, e221–e225. [Google Scholar] [CrossRef]
- Voronets, J.; Lussi, A. Thickness of Softened Human Enamel Removed by Toothbrush Abrasion: An in Vitro Study. Clin. Oral Investig. 2010, 14, 251–256. [Google Scholar] [CrossRef]
- Rios, D.; Honório, H.M.; Magalhães, A.C.; da Silva, S.M.B.; Delbem, A.C.B.; Machado, M.A.d.A.M.; Buzalaf, M.A.R. Scanning Electron Microscopic Study of the in Situ Effect of Salivary Stimulation on Erosion and Abrasion in Human and Bovine Enamel. Braz. Oral Res. 2008, 22, 132–138. [Google Scholar] [CrossRef]
- Wiegand, A.; Köwing, L.; Attin, T. Impact of Brushing Force on Abrasion of Acid-Softened and Sound Enamel. Arch. Oral Biol. 2007, 52, 1043–1047. [Google Scholar] [CrossRef]
- Kuroiwa, M.; Kodaka, T.; Kuroiwa, M.; Abe, M. Brushing-Lnduced Effects with and without a Non-Fluoride Abrasive Dentifrice on Remineralization of Enamel Surfaces Etched with Phosphoric Acid. Caries Res. 1994, 28, 309–314. [Google Scholar] [CrossRef]
- Wiegand, A.; Wegehaupt, F.; Werner, C.; Attin, T. Susceptibility of Acid-Softened Enamel to Mechanical Wear—Ultrasonication versus Toothbrushing Abrasion. Caries Res. 2007, 41, 56–60. [Google Scholar] [CrossRef]
- Rios, D.; Honório, H.M.; Magalhães, A.C.; Buzalaf, M.A.R.; Palma-Dibb, R.G.; De Andrade Moreira Machado, M.A.; da Silva, S.M.B. Influence of Toothbrushing on Enamel Softening and Abrasive Wear of Eroded Bovine Enamel: An in Situ Study. Braz. Oral Res. 2006, 20, 148–154. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Attin, T.; Koidl, U.; Buchalla, W.; Schaller, H.G.; Kielbassa, A.M.; Hellwig, E. Correlation of Microhardness and Wear in Differently Eroded Bovine Dental Enamel. Arch. Oral Biol. 1997, 42, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, A.; Schlueter, N. The Role of Oral Hygiene: Does Toothbrushing Harm? In Erosive Tooth Wear: From Diagnosis to Therapy; Karger Publishers: Basel, Switzerland, 2014; Volume 25, pp. 215–219. [Google Scholar] [CrossRef]
- Maden, E.A.; Altun, C.; Polat, G.G.; Basak, F. The In Vitro Evaluation of the Effect of Xyliwhite, Probiotic, and the Conventional Toothpastes on the Enamel Roughness and Microhardness. Niger. J. Clin. Pract. 2018, 21, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Jamwal, N.; Rao, A.; Shenoy, R.; Pai, M.; Ks, A.; Br, A. Effect of Whitening Toothpaste on Surface Roughness and Microhardness of Human Teeth: A Systematic Review and Meta-Analysis. F1000Research 2022, 11, 22. [Google Scholar] [CrossRef]
- Shamel, M.; Al-Ankily, M.M.; Bakr, M.M. Influence of Different Types of Whitening Tooth Pastes on the Tooth Color, Enamel Surface Roughness and Enamel Morphology of Human Teeth. F1000Research 2019, 8, 1764. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, S.; Truong, V.M.; Lee, J.W.; Park, Y.-S. Is Whitening Toothpaste Safe for Dental Health?: RDA-PE Method. Dent. Mater. J. 2022, 41, 731–740. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, S.; Garcia-Godoy, F.; Park, Y.-S. Dentin Abrasion Using Whitening Toothpaste with Various Hydrogen Peroxide Concentrations. Am. J. Dent. 2023, 36, 55–61. [Google Scholar]
- Shaikh, M.; Lund, G.; Ko, J.; Roque-Torres, G.; Oyoyo, U.; Kwon, S.R. Micro Computed Tomography Analysis of Abrasivity of Toothpaste Tablets Compared to Conventional Toothpaste. Am. J. Dent. 2021, 34, 235–239. [Google Scholar]
- Koc Vural, U.; Bagdatli, Z.; Yilmaz, A.E.; Yalçın Çakır, F.; Altundaşar, E.; Gurgan, S. Effects of Charcoal-Based Whitening Toothpastes on Human Enamel in Terms of Color, Surface Roughness, and Microhardness: An in Vitro Study. Clin. Oral Investig. 2021, 25, 5977–5985. [Google Scholar] [CrossRef]
- Hamza, B.; Abdulahad, A.; Attin, T.; Wegehaupt, F.J. Diamond Particles in Toothpastes: In-Vitro Effect on the Abrasive Enamel Wear. BMC Oral Health 2022, 22, 248. [Google Scholar] [CrossRef]
- Dionysopoulos, D.; Papageorgiou, S.; Papadopoulos, C.; Davidopoulou, S.; Konstantinidis, A.; Tolidis, K. Effect of Whitening Toothpastes with Different Active Agents on the Abrasive Wear of Dentin Following Tooth Brushing Simulation. J. Funct. Biomater. 2023, 14, 268. [Google Scholar] [CrossRef] [PubMed]
- Greuling, A.; Emke, J.M.; Eisenburger, M. Abrasion Behaviour of Different Charcoal Toothpastes When Using Electric Toothbrushes. Dent. J. 2021, 9, 97. [Google Scholar] [CrossRef] [PubMed]
- Viana, Í.E.L.; Weiss, G.S.; Sakae, L.O.; Niemeyer, S.H.; Borges, A.B.; Scaramucci, T. Activated Charcoal Toothpastes Do Not Increase Erosive Tooth Wear. J. Dent. 2021, 109, 103677. [Google Scholar] [CrossRef] [PubMed]
- Zoller, M.J.; Hamza, B.; Cucuzza, C.; Gubler, A.; Attin, T.; Wegehaupt, F.J. Relative Dentin and Enamel Abrasivity of Charcoal Toothpastes. Int. J. Dent. Hyg. 2023, 21, 149–156. [Google Scholar] [CrossRef]
- Buedel, S.; Lippert, F.; Zero, D.T.; Eckert, G.J.; Hara, A.T. Impact of Dentifrice Abrasivity and Remineralization Time on Erosive Tooth Wear in Vitro. Am. J. Dent. 2018, 31, 29–33. [Google Scholar]
- West, N.; Addy, M.; Hughes, J. Dentine Hypersensitivity: The Effects of Brushing Desensitizing Toothpastes, Their Solid and Liquid Phases, and Detergents on Dentine and Acrylic: Studies in Vitro. J. Oral Rehabil. 1998, 25, 885–895. [Google Scholar] [CrossRef]
- Arnold, W.H.; Gröger, C.; Bizhang, M.; Naumova, E.A. Dentin Abrasivity of Various Desensitizing Toothpastes. Head. Face Med. 2016, 12, 16. [Google Scholar] [CrossRef]
- Lopes, R.M.; Scaramucci, T.; Walker, C.L.; Feitosa, S.A.; Aranha, A.C.C. In Situ Evaluation of Desensitizing Toothpastes for Protecting against Erosive Tooth Wear and Its Characterization. Clin. Oral Investig. 2021, 25, 6857–6870. [Google Scholar] [CrossRef]
- Nassar, H.M.; Hara, A.T. Effect of Dentifrice Slurry Abrasivity and Erosive Challenge on Simulated Non-Carious Cervical Lesions Development in Vitro. J. Oral Sci. 2021, 63, 191–194. [Google Scholar] [CrossRef]
- João-Souza, S.H.; Sakae, L.O.; Lussi, A.; Aranha, A.C.C.; Hara, A.; Baumann, T.; Scaramucci, T. Toothpaste factors related to dentine tubule occlusion and dentine protection against erosion and abrasion. Clin. Oral. Investig. 2020, 24, 2051–2060. [Google Scholar] [CrossRef]
- Jang, Y.; Ihm, J.-J.; Baik, S.-J.; Yoo, K.-J.; Jang, D.-H.; Roh, B.-D.; Seo, D.-G. Dentin Wear after Simulated Toothbrushing with Water, a Liquid Dentifrice or a Standard Toothpaste. Am. J. Dent. 2015, 28, 333–336. [Google Scholar] [PubMed]
- van der Weijden, F.; Slot, D.E.; van der Sluijs, E.; Hennequin-Hoenderdos, N.L. The Efficacy of a Rubber Bristles Interdental Cleaner on Parameters of Oral Soft Tissue Health-a Systematic Review. Int. J. Dent. Hyg. 2022, 20, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Hennequin-Hoenderdos, N.L.; van der Sluijs, E.; van der Weijden, G.A.; Slot, D.E. Efficacy of a Rubber Bristles Interdental Cleaner Compared to an Interdental Brush on Dental Plaque, Gingival Bleeding and Gingival Abrasion: A Randomized Clinical Trial. Int. J. Dent. Hyg. 2018, 16, 380–388. [Google Scholar] [CrossRef] [PubMed]
- De Nutte, M.; Behaeghe, E.; van der Weijden, G.A.; Coucke, W.; Teughels, W.; Quirynen, M. Healing of Toothbrush-Induced Abrasions to Keratinized Mucosa of the Palate in Humans: A Pilot Study. J. Periodontal Res. 2018, 53, 506–513. [Google Scholar] [CrossRef]
- Attin, T.; Knöfel, S.; Buchalla, W.; Tütüncü, R. In Situ Evaluation of Different Remineralization Periods to Decrease Brushing Abrasion of Demineralized Enamel. Caries Res. 2001, 35, 216–222. [Google Scholar] [CrossRef]
- Jaeggi, T.; Lussi, A. Toothbrush Abrasion of Erosively Altered Enamel after Intraoral Exposure to Saliva: An in Situ Study. Caries Res. 1999, 33, 455–461. [Google Scholar] [CrossRef]
- Toti, Ç.; Meto, A.; Kaçani, G.; Droboniku, E.; Hysi, D.; Tepedino, M.; Zaja, E.; Fiorillo, L.; Meto, A.; Buci, D.; et al. White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment. Healthcare 2022, 10, 320. [Google Scholar] [CrossRef]
- Ganss, C.; Von Hinckeldey, J.; Tolle, A.; Schulze, K.; Klimek, J.; Schlueter, N. Efficacy of the Stannous Ion and a Biopolymer in Toothpastes on Enamel Erosion/Abrasion. J. Dent. 2012, 40, 1036–1043. [Google Scholar] [CrossRef]
- Carvalho, T.S.; Lussi, A. Combined Effect of a Fluoride-, Stannous- and Chitosan-Containing Toothpaste and Stannous-Containing Rinse on the Prevention of Initial Enamel Erosion-Abrasion. J. Dent. 2014, 42, 450–459. [Google Scholar] [CrossRef]
- Machado, A.; Sakae, L.; Niemeyer, S.H.; Carvalho, T.S.; Amaechi, B.; Scaramucci, T. Anti-Erosive Effect of Rinsing before or after Toothbrushing with a Fluoride/Stannous Ions Solution: An in Situ Investigation. J. Dent. 2020, 101, 103450. [Google Scholar] [CrossRef]
- Körner, P.; Inauen, D.S.; Attin, T.; Wegehaupt, F.J. Erosive/Abrasive Enamel Wear While Using a Combination of Anti-Erosive Toothbrush/-Paste. Oral Health Prev. Dent. 2020, 18, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Memarpour, M.; Jafari, S.; Rafiee, A.; Alizadeh, M.; Vossoughi, M. Protective Effect of Various Toothpastes and Mouthwashes against Erosive and Abrasive Challenge on Eroded Dentin: An in Vitro Study. Sci. Rep. 2024, 14, 9387. [Google Scholar] [CrossRef] [PubMed]
- Moretto, M.J.; Delbem, A.C.B.; Manarelli, M.M.; Pessan, J.P.; Martinhon, C.C.R. Effect of Fluoride Varnish Supplemented with Sodium Trimetaphosphate on Enamel Erosion and Abrasion: An in Situ/Ex Vivo Study. J. Dent. 2013, 41, 1302–1306. [Google Scholar] [CrossRef] [PubMed]
- Sales-Peres, S.H.C.; Pessan, J.P.; Buzalaf, M.A.R. Effect of an Iron Mouthrinse on Enamel and Dentine Erosion Subjected or Not to Abrasion: An in Situ/Ex Vivo Study. Arch. Oral Biol. 2007, 52, 128–132. [Google Scholar] [CrossRef]
- Esteves-Oliveira, M.; Pasaporti, C.; Heussen, N.; Eduardo, C.P.; Lampert, F.; Apel, C. Prevention of Toothbrushing Abrasion of Acid-Softened Enamel by CO2 Laser Irradiation. J. Dent. 2011, 39, 604–611. [Google Scholar] [CrossRef]
- Tomás, D.B.M.; Pecci-Lloret, M.P.; Guerrero-Gironés, J. Effectiveness and Abrasiveness of Activated Charcoal as a Whitening Agent: A Systematic Review of in Vitro Studies. Ann. Anat.-Anat. Anz. 2023, 245, 151998. [Google Scholar] [CrossRef]
- Hennequin-Hoenderdos, N.; Slot, D.; Van der Sluijs, E.; Adam, R.; Grender, J.; Van der Weijden, G. The Effects of Different Levels of Brush End Rounding on Gingival Abrasion: A Double-blind Randomized Clinical Trial. Int. J. Dent. Hyg. 2017, 15, 335–344. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, S.; Gopalkrishna, P.; Syed, A.K.; Sathiyabalan, A. The Impact of Toothbrushing on Oral Health, Gingival Recession, and Tooth Wear—A Narrative Review. Healthcare 2025, 13, 1138. https://doi.org/10.3390/healthcare13101138
Kumar S, Gopalkrishna P, Syed AK, Sathiyabalan A. The Impact of Toothbrushing on Oral Health, Gingival Recession, and Tooth Wear—A Narrative Review. Healthcare. 2025; 13(10):1138. https://doi.org/10.3390/healthcare13101138
Chicago/Turabian StyleKumar, Santhosh, Pratibha Gopalkrishna, Ayman K. Syed, and Abishikka Sathiyabalan. 2025. "The Impact of Toothbrushing on Oral Health, Gingival Recession, and Tooth Wear—A Narrative Review" Healthcare 13, no. 10: 1138. https://doi.org/10.3390/healthcare13101138
APA StyleKumar, S., Gopalkrishna, P., Syed, A. K., & Sathiyabalan, A. (2025). The Impact of Toothbrushing on Oral Health, Gingival Recession, and Tooth Wear—A Narrative Review. Healthcare, 13(10), 1138. https://doi.org/10.3390/healthcare13101138







