Unraveling the Causal Relationship Between Non-Communicable Diseases, Obesity, and Health Expenditure: Insights from the Toda–Yamamoto Approach
Abstract
1. Introduction
2. Materials and Methods
- H0a: Obesity is not the cause of the burden of NCDs.
- H1a: Obesity is the cause of the burden of NCDs.
- H0b: Obesity is not the cause of health expenditures.
- H1b: Obesity is the cause of health expenditures.
- H0c: The burden of NCDs is not the cause of health expenditures.
- H1c: The burden of NCDs is the cause of health expenditures.
- H0d: The interaction between NCDs and obesity is not the cause health of expenditures.
- H1d: The interaction between NCDs and obesity is the cause of health expenditures.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Non Communicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 3 November 2024).
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef] [PubMed]
- TUIK. Nedenlerine Göre Ölüm Istatistikleri. Available online: https://data.tuik.gov.tr/Bulten/Index?p=Causes-of-Death-Statistics-2010,-2011-and-2012-15847 (accessed on 3 November 2024).
- Suhrcke, M.; Urban, D. Are Cardiovascular Diseases Bad for Economic Growth? Health Econ. 2010, 19, 1478–1496. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Reference Life Table. 2021. Available online: https://ghdx.healthdata.org/record/ihme-data/global-burden-disease-study-2019-gbd-2019-reference-life-table (accessed on 3 November 2024). [CrossRef]
- Rohana, N.H.; Chandrika, N.W.; Upul, S. Chapter 1—Worldwide Epidemic of Obesity, Obesity and Obstetrics, 2nd ed.; Mahmood, T.A., Arulkumaran, S., Chervenak, F.A., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 3–8. ISBN 9780128179215. [Google Scholar] [CrossRef]
- Tremmel, M.; Gerdtham, U.-G.; Nilsson, P.M.; Saha, S. Economic Burden of Obesity: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 435. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 November 2024).
- GHO | By Category | Prevalence of Obesity Among Adults, BMI ≥ 30, Crude—Estimates by Country. Available online: https://apps.who.int/gho/data/view.main.BMI30Cv?lang=en (accessed on 3 November 2024).
- Okunogbe, A.; Nugent, R.; Spencer, G.; Ralston, J.; Wilding, J. Economic Impacts of Overweight and Obesity: Current and Future Estimates for Eight Countries. BMJ Glob. Health 2021, 6, e006351. [Google Scholar] [CrossRef] [PubMed]
- Orhan, O.; Nergiz, E. Turkey’s Current Account Deficit Problem and Its Effects on the European Union Accession. İstanbul Gelişim Üniversitesi Sos. Bilim. Derg. 2014, 1, 137–158. [Google Scholar] [CrossRef][Green Version]
- Kortt, M.A.; Langley, P.C.; Cox, E.R. A Review of Cost-of-Illness Studies on Obesity. Clin. Ther. 1998, 20, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Torun, P.; Kutlar, A. Türkiye’de Kanserin Ekonomik Maliyetleri: Bir Hesaplanabilir Genel Denge Modeli Yaklaşımı * Economic Costs of The Cancer: A Computable General Equilibrium Model Approach. Hacet. Sos. Beşerî Bilim. Derg. 2018, 21, 31–39. [Google Scholar]
- Bloom, D.; Cafiero-Fonseca, E.; McGovern, M.; Prettner, K.; Stanciole, A.; Weiss, J.; Bakkila, S.; Rosenberg, L. The Economic Impact of Non-Communicable Disease in China and India: Estimates, Projections, and Comparisons. SSRN Electron. J. 2013, 7563, 1–30. [Google Scholar] [CrossRef]
- Vandenberghe, D.; Albrecht, J. The Financial Burden of Non-Communicable Diseases in the European Union: A Systematic Review. Eur. J. Public Health 2020, 30, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Muka, T.; Imo, D.; Jaspers, L.; Colpani, V.; Chaker, L.; van der Lee, S.J.; Mendis, S.; Chowdhury, R.; Bramer, W.M.; Falla, A.; et al. The Global Impact of Non-Communicable Diseases on Healthcare Spending and National Income: A Systematic Review. Eur. J. Epidemiol. 2015, 30, 251–277. [Google Scholar] [CrossRef]
- Schmid, T. Costs of Treating Cardiovascular Events in Germany: A Systematic Literature Review. Health Econ. Rev. 2015, 5, 27. [Google Scholar] [CrossRef] [PubMed]
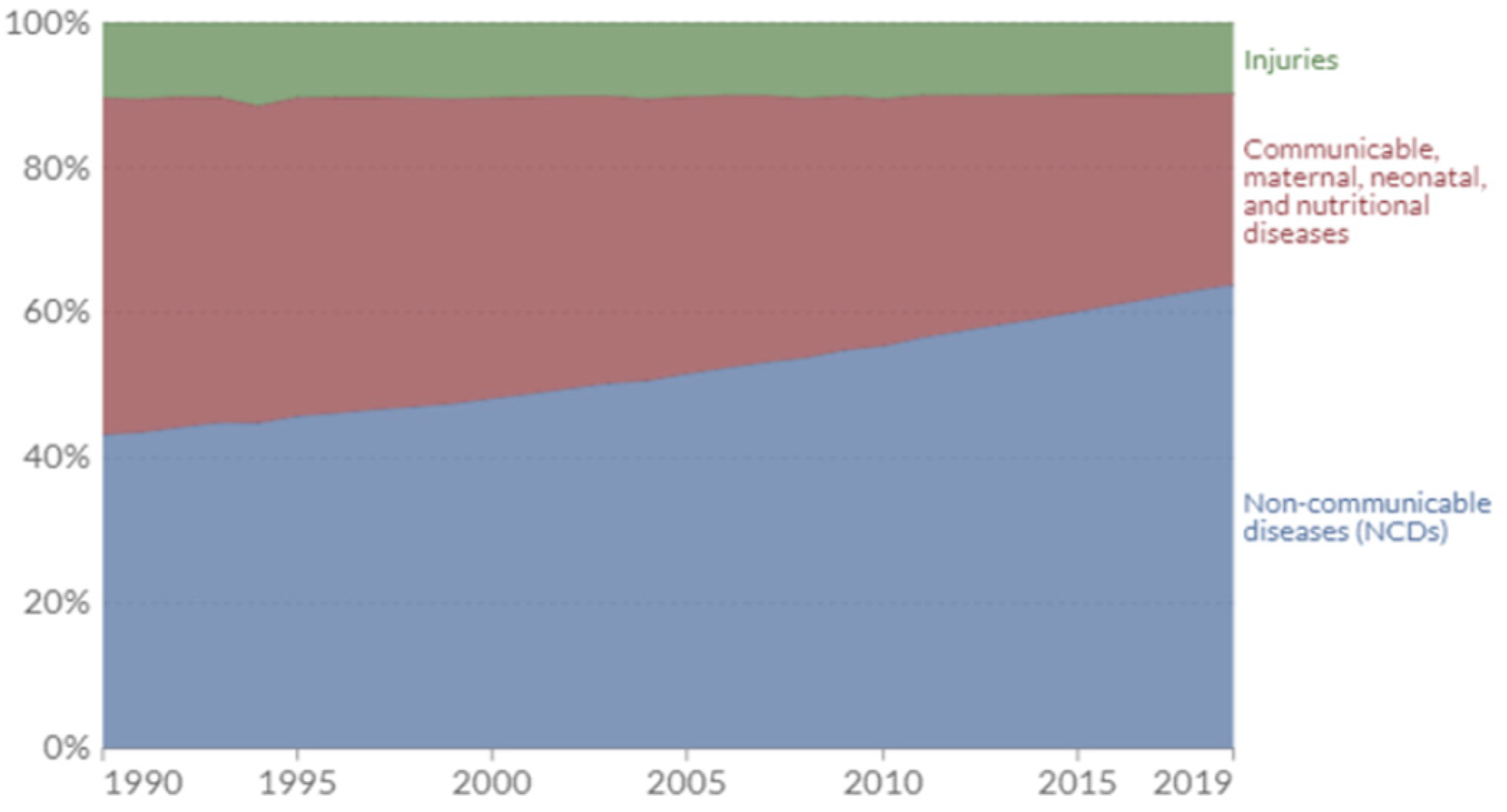
- Roser, M.; Ritchie, H.; Spooner, F. Burden of Disease. Our World Data. 2024. Available online: https://ourworldindata.org/burden-of-disease (accessed on 19 October 2024).
- Toda, H.Y.; Yamamoto, T. Statistical inference in vector autoregressions with possibly integrated processes. J. Econom. 1995, 66, 225–250. [Google Scholar] [CrossRef]
- Granger, C.W.J. Investigating Causal Relations by Econometric Models and Cross-Spectral Methods. Econometrica 1969, 37, 424–438. [Google Scholar] [CrossRef]
- Sims, C. Macroeconomis and Reality. Econometrica 1980, 48, 1–48. [Google Scholar] [CrossRef]
- Engeloğlu, Ö.; Meral, İ.; Kübra, G. Türkiye İçin Yapılan Nedensellik Uygulamaları Üzerine Literatür Araştırması. Soc. Sci. Res. J. 2015, 4, 142–154. [Google Scholar]
- Akkas, M.; Sayilgan, G. Housing Prices and Mortgage Interest ratesToda-Yamamoto Causality Test. Pressacademia 2015, 2, 572. [Google Scholar] [CrossRef]
- Doğan, B. Ekonomik Küreselleşme ve Büyüme İlişkisi: Türkiye Örneği Toda-Yamamoto Nedensellik Analizi. Finans Polit. Ekon. Yorumlar 2017, 628, 19–27. [Google Scholar]
- Schwert, W. Test for Unit Roots: A Monte Carlo Investigation. J. Bus. Econ. Stat. 1989, 7, 147–159. [Google Scholar] [CrossRef]
- Lin, X.; Xu, Y.; Xu, J.; Pan, X.; Song, X.; Shan, L.; Zhao, Y.; Shan, P.F. Global Burden of Noncommunicable Disease Attributable to High Body Mass Index in 195 Countries and Territories, 1990. Endocrine 2020, 69, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Anakök, G.A.; Awad, S.F.; Çağlayan, Ç.; Huangfu, P.; Abu-Raddad, L.J.; Unal, B.; Critchley, J.A. Impact of Trends and Gender Disparity in Obesity on Future Type 2 Diabetes in Turkey: A Mathematical Modelling Analysis. BMJ Open 2022, 12, e053541. [Google Scholar] [CrossRef] [PubMed]
- Tokgozoglu, L.; Kayikcioglu, M.; Ekinci, B. The Landscape of Preventive Cardiology in Turkey: Challenges and Successes. Am. J. Prev. Cardiol. 2021, 6, 100184. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Ke, K.; Liu, Z.; Yang, L.; Wang, L.; Zhou, J.; Dong, Q. Body Mass Index and Cancer Risk: An Umbrella Review of Meta-Analyses of Observational Studies. Nutr. Cancer 2023, 75, 1051–1064. [Google Scholar] [CrossRef] [PubMed]
- Al-Jawaldeh, A.; Abbass, M.M.S. Unhealthy Dietary Habits and Obesity: The Major Risk Factors Beyond Non-Communicable Diseases in the Eastern Mediterranean Region. Front. Nutr. 2022, 9, 817808. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, D.; Sharma, S. Abdominal Obesity, Adipokines and Non-Communicable Diseases. J. Steroid Biochem. Mol. Biol. 2020, 203, 105737. [Google Scholar] [CrossRef] [PubMed]
- Nilson, E.A.F.; Gianicchi, B.; Ferrari, G.; Rezende, L.F.M. The Projected Burden of Non-Communicable Diseases Attributable to Overweight in Brazil from 2021 to 2030. Sci. Rep. 2022, 12, 22483. [Google Scholar] [CrossRef]
- Withrow, D.; Alter, D.A. The Economic Burden of Obesity Worldwide: A Systematic Review of the Direct Costs of Obesity. Obes. Rev. 2011, 12, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Lartey, S.T.; de Graaff, B.; Magnussen, C.G.; Boateng, G.O.; Aikins, M.; Minicuci, N.; Kowal, P.; Si, L.; Palmer, A.J. Health Service Utilization and Direct Healthcare Costs Associated with Obesity in Older Adult Population in Ghana. Health Policy Plan. 2020, 35, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Biener, A.; Meyerhoefer, C.; Ding, Y.; Zvenyach, T.; Smolarz, B.G.; Ramasamy, A. Direct Medical Costs of Obesity in the United States and the Most Populous States. J. Manag. Care Spec. Pharm. 2021, 27, 354–366. [Google Scholar] [CrossRef] [PubMed]
- Okunogbe, A.; Nugent, R.; Spencer, G.; Powis, J.; Ralston, J.; Wilding, J. Economic Impacts of Overweight and Obesity: Current and Future Estimates for 161 Countries. BMJ Glob. Health 2022, 7, e009773. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; McPherson, K.; Marsh, T.; Gortmaker, S.L.; Brown, M. Health and Economic Burden of the Projected Obesity Trends in the USA and the UK. Lancet 2011, 378, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Chaker, L.; Falla, A.; van der Lee, S.J.; Muka, T.; Imo, D.; Jaspers, L.; Colpani, V.; Mendis, S.; Chowdhury, R.; Bramer, W.M.; et al. The Global Impact of Non-Communicable Diseases on Macro-Economic Productivity: A Systematic Review. Eur. J. Epidemiol. 2015, 30, 357–395. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Sheng, Z. Beyond Weight: Examining the Association of Obesity with Cardiometabolic Related Inpatient Costs among Canadian Adults Using Linked Population Based Survey and Hospital Administrative Data. BMC Health Serv. Res. 2021, 21, 54. [Google Scholar] [CrossRef] [PubMed]
- Hacker, K. The Burden of Chronic Disease. Mayo Clin. Proc. Innov. Qual. Outcomes 2024, 8, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Boachie, M.K.; Thsehla, E.; Immurana, M.; Kohli-Lynch, C.; Hofman, K.J. Estimating the Healthcare Cost of Overweight and Obesity in South Africa. Glob. Health Action 2022, 15, 2045092. [Google Scholar] [CrossRef] [PubMed]

| Abbreviation | Variable Definition | Source |
|---|---|---|
| Obesity | Proportion of individuals with a BMI of ≥30 | https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-obesity-among-adults-bmi-=-30-(age-standardized-estimate)-(-) (accessed on 24 July 2024) |
| NCD | Burden of NCDs is represented by the total disease impact, measured in DALYs per year | https://ourworldindata.org/grapher/burden-of-disease-rates-from-ncds (accessed on 24 July 2024) |
| Health expenditure | Current health expenditure (% of GDP) | https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS (accessed on 24 July 2024) |
| Test Critical Values | |||||
|---|---|---|---|---|---|
| t-Stat | %1 | %5 | %10 | p-Value | |
| Health expenditure (∆) | −6.338283 [0] | −3.689 | −2.971 | −2.625 | <0.00001 * |
| NCD (∆) | −5.270350 * [0] | −3.689 | −2.971 | −2.625 | 0.0002 * |
| Obesity (∆∆) | −17.27366 * [1] | −3.699 | −2.976 | −2.627 | 0.0001 * |
| NCD × Obesity Interaction (∆∆) | −3.810492 * [1] | −3.580 | −2.930 | −2.600 | 0.03421 * |
| Hypothesis | χ2 | df | p | Result |
|---|---|---|---|---|
| Obesity ⇏ NCD H0: no causality | 11.82509 | 2 | 0.0005 ** | H0: rejected |
| Obesity ⇏ health expenditure H0: no causality | 16.841 07 | 2 | <0.00001 ** | H0: rejected |
| NCD ⇏ health expenditure H0: no causality | 15.04441 | 2 | 0.00001 ** | H0: rejected |
| Obesity×NCD Interaction ⇏ health expenditure H0: no causality | 2.085039 | 4 | 0.104401 | H0: cannot rejected |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yılmaz, S.; Boz, C.; Eren, F.A.; Günal, A.M. Unraveling the Causal Relationship Between Non-Communicable Diseases, Obesity, and Health Expenditure: Insights from the Toda–Yamamoto Approach. Healthcare 2025, 13, 1. https://doi.org/10.3390/healthcare13010001
Yılmaz S, Boz C, Eren FA, Günal AM. Unraveling the Causal Relationship Between Non-Communicable Diseases, Obesity, and Health Expenditure: Insights from the Toda–Yamamoto Approach. Healthcare. 2025; 13(1):1. https://doi.org/10.3390/healthcare13010001
Chicago/Turabian StyleYılmaz, Salim, Canser Boz, Furkan Alp Eren, and Ahmet Murat Günal. 2025. "Unraveling the Causal Relationship Between Non-Communicable Diseases, Obesity, and Health Expenditure: Insights from the Toda–Yamamoto Approach" Healthcare 13, no. 1: 1. https://doi.org/10.3390/healthcare13010001
APA StyleYılmaz, S., Boz, C., Eren, F. A., & Günal, A. M. (2025). Unraveling the Causal Relationship Between Non-Communicable Diseases, Obesity, and Health Expenditure: Insights from the Toda–Yamamoto Approach. Healthcare, 13(1), 1. https://doi.org/10.3390/healthcare13010001







