Effect of Therapeutic Gardening Program in Urban Gardens on the Mental Health of Children and Their Caregivers with Atopic Dermatitis
Abstract
1. Introduction
2. Materials and Methods
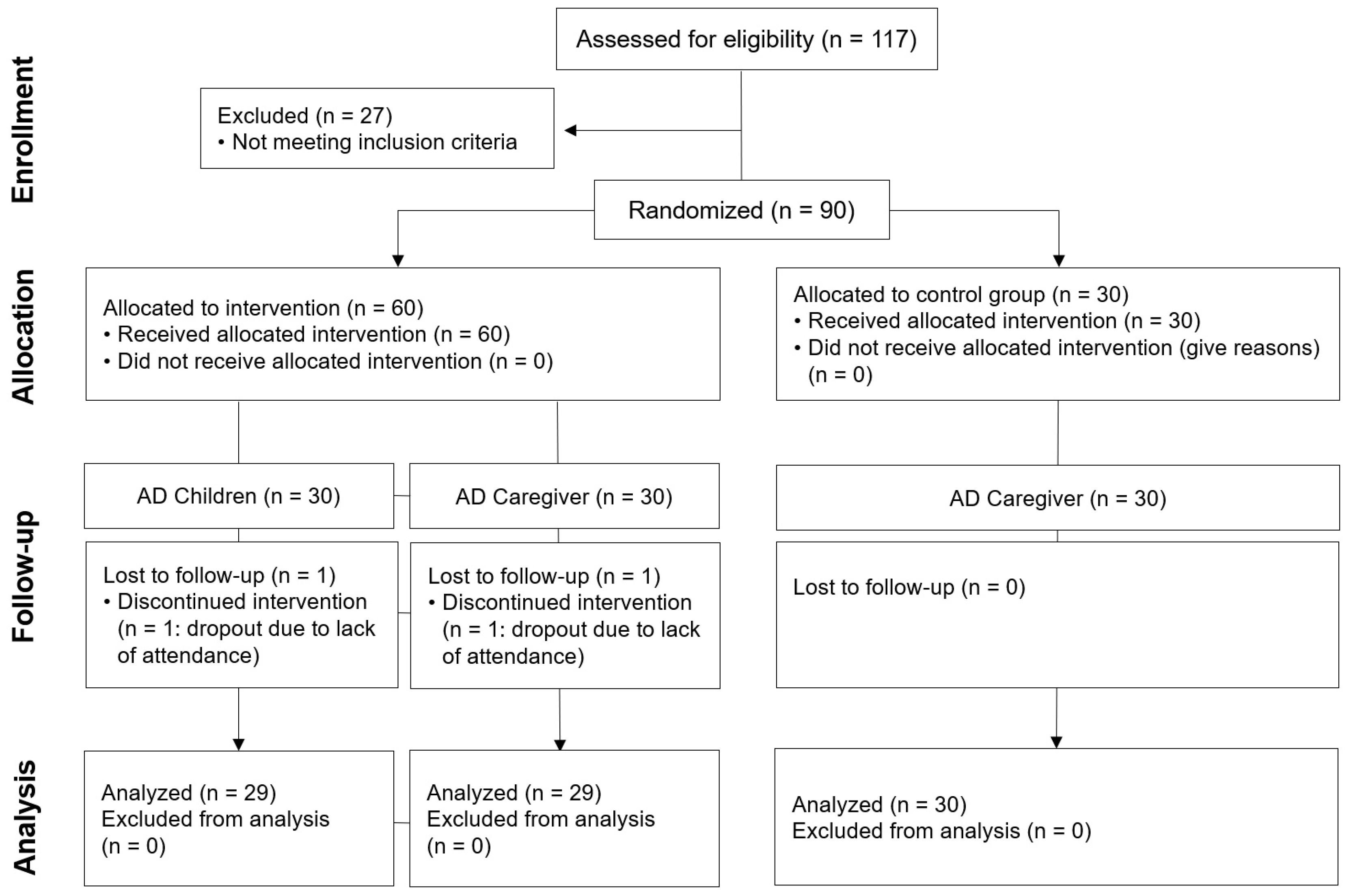
2.1. Participants
2.2. Procedure
2.3. Therapeutic Gardening Program Design
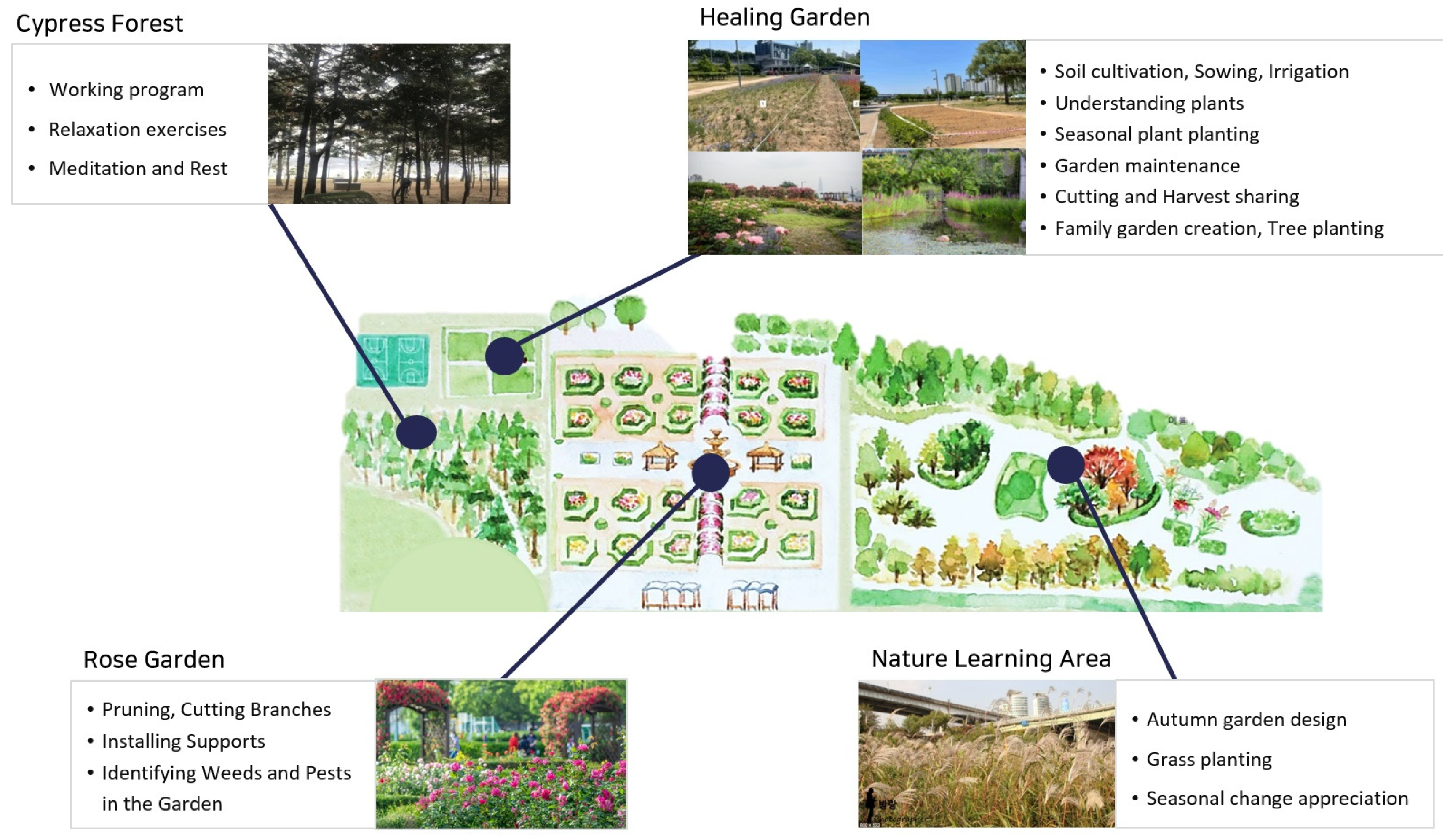
2.3.1. Program Site
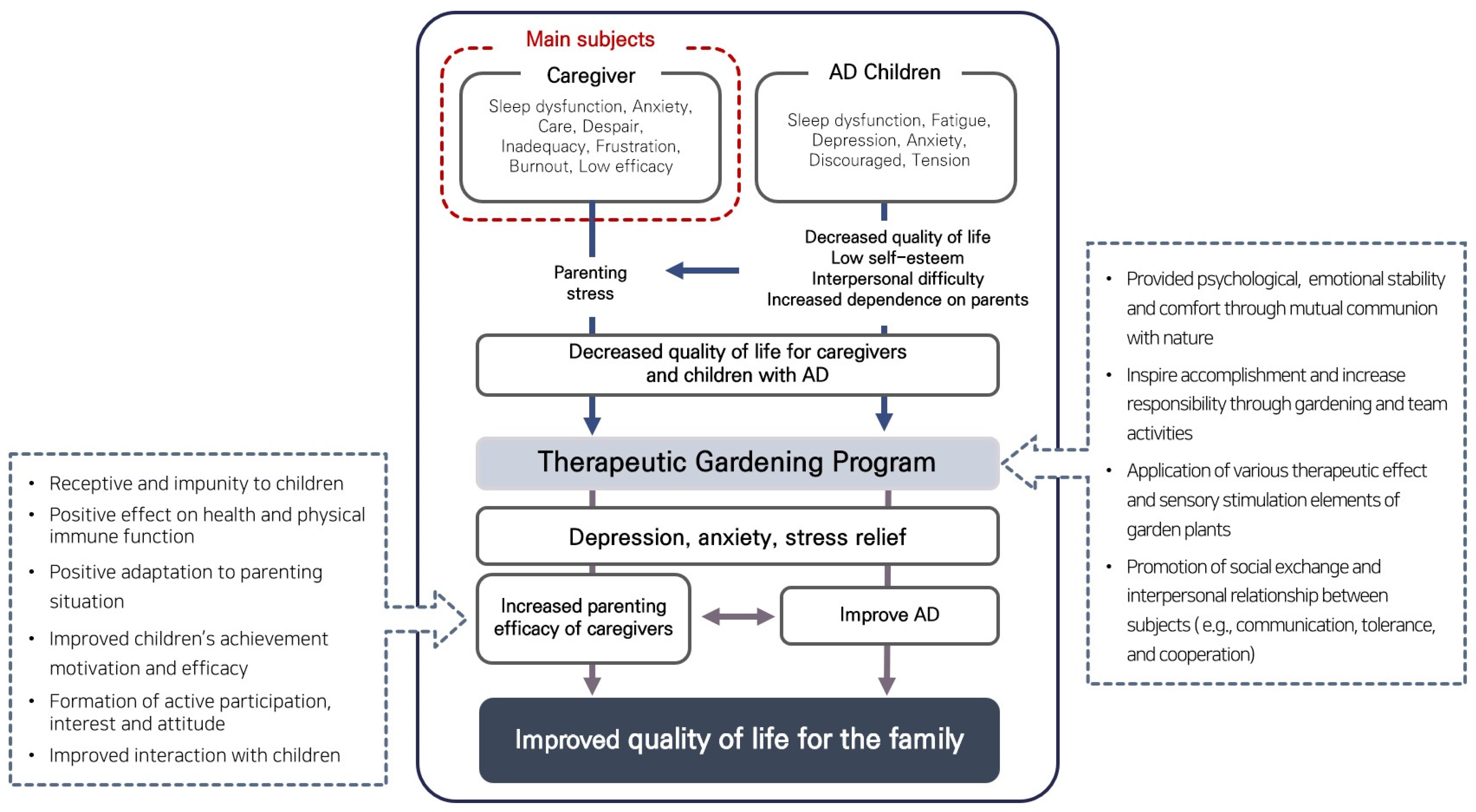
2.3.2. Program Goal-Setting
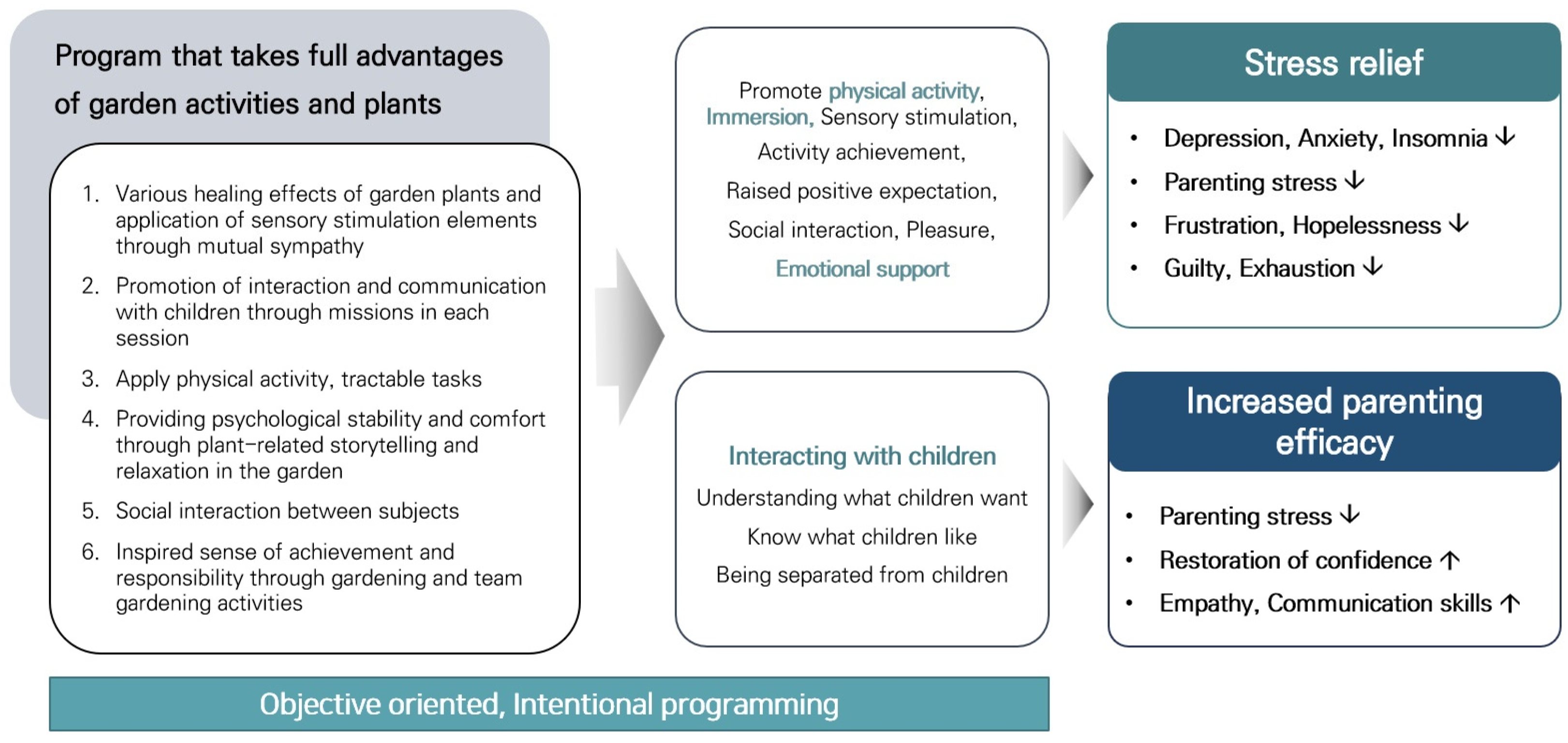
2.3.3. Program Composition
2.3.4. A Phased Plan for the TGP
2.4. Psychosocial Effect Measures
2.4.1. Mental Health Screening Tool for Depressive and Anxiety Disorders
2.4.2. Core Life Activities Index
2.4.3. Korean Version of the Satisfaction with the Life Scale
2.4.4. Perceived Stress Scale
2.4.5. Parenting Self-Efficacy
2.4.6. Children’s Depression Inventory
2.5. Physiological Effect Measures
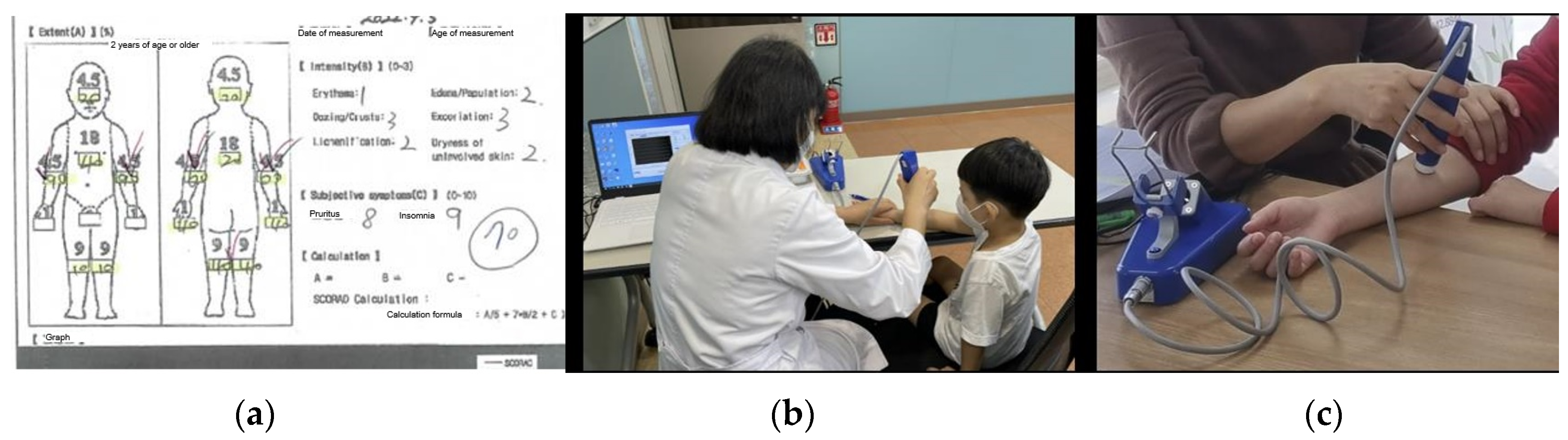
2.5.1. Scoring Atopic Dermatitis Index
2.5.2. Transepidermal Water Loss
2.6. Statistical Analysis
3. Results
3.1. Caregivers of Children with AD
3.2. Children with AD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Janković, J.; Ćirković, A.; Rašić, J.; Vitković, L.; Janković, S. Impact of atopic dermatitis on the quality of life of children and their families. Ital. J. Dermatol. Venerol. 2020, 156, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Choi, M.H. Knowledge, compliance and quality of life of mothers of children with atopic dermatitis. Child Health Nurs. Res. 2011, 17, 272–280. [Google Scholar] [CrossRef]
- Lawson, V.; Lewis-Jones, M.S.; Finlay, A.Y.; Reid, P.; Owens, R.G. The family impact of childhood atopic dermatitis: The Dermatitis Family Impact Questionnaire. Br. J. Dermatol. 1998, 138, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Basra, M.; Finlay, A.Y. The family impact of skin diseases: The Greater Patient concept. Br. J. Dermatol. 2007, 156, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Lewis-Jones, S. Quality of life and childhood atopic dermatitis: The misery of living with childhood eczema. Int. J. Clin. Pract. 2006, 60, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Yoo, I.Y. Parenting stress and needs of mothers of children with atopic dermatitis. Child Health Nurs. Res. 2004, 10, 423–430. [Google Scholar]
- Carroll, C.L.; Balkrishnan, R.; Feldman, S.R.; Fleischer, A.B., Jr.; Manuel, J.C. The burden of atopic dermatitis: Impact on the patient, family, and society. Pediatr. Dermatol. 2005, 22, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.J.; Beck, K.M.; Sekhon, S.; Bhutani, T.; Koo, J. The impact of pediatric atopic dermatitis on families: A review. Pediatr. Dermatol. 2019, 36, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Whipple, E.E.; Webster-Stratton, C. The role of parental stress in physically abusive families. Child Abus. Negl. 1991, 15, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.-L.; Doh, H.-S.; Choi, M.-K. The Effects of Preschool Children’s Age and Mothers’ Modes of Verbal Control on Children’s Lying. J. Fam. Better Life 2008, 26, 191–201. [Google Scholar]
- Dix, T. Parenting on behalf of the child: Empathic goals in the regulation of responsive parenting. In Parental Belief Systems; Taylor & Francis Group: Abingdon, UK, 2014; pp. 319–346. [Google Scholar]
- Letourneau, C. Empathy and stress: How they affect parental aggression. J. Soc. Work 1981, 26, 383–389. [Google Scholar] [CrossRef]
- Kotchick, B.A.; Forehand, R.; Brody, G.; Armistead, L.; Simon, P.; Morse, E.; Clark, L. The impact of maternal HIV infection on parenting in inner-city African American families. J. Fam. Psychol. 1997, 11, 447. [Google Scholar] [CrossRef]
- Yoon, S.P.; Kim, B.S.; Ree, J.H.; Lee, S.C.; Kim, Y.K. The environment and lifestyles of atopic dermatitis patients. Korean J. Dermatol. 1999, 983–991. [Google Scholar]
- Choi, K.M.; Kim, K.Y.; Lee, M.S.; Hong, J.Y.; Bae, S.H.; Hwang, H.J. The related factors of atopic dermatitis severity in elementary school students. JKAIS 2011, 12, 759–764. [Google Scholar] [CrossRef]
- Buske-Kirschbaum, A.; Geiben, A.; Hellhammer, D. Psychobiological aspects of atopic dermatitis: An overview. Psychother. Psychosom. 2001, 70, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K. Stress, personal relationships, and immune function: Health implications. Brain Behav. Immun. 1999, 13, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Helmbold, P.; Gaisbauer, G.; Kupfer, J.; Haustein, U.-F. Longitudinal case analysis in atopic dermatitis. Acta Derm. Venereol. 2000, 80, 348–352. [Google Scholar] [CrossRef] [PubMed]
- King, R.M.; Wilson, G.V. Use of a diary technique to investigate psychosomatic relations in atopic dermatitis. J. Psychosom. Res. 1991, 35, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Gieler, U.; Niemeier, V.; Brosig, B. Psychoimmunology and evaluation of therapeutic approaches. In Ato Derm; CRC Press: Boca Raton, FL, USA, 2002; pp. 50–70. [Google Scholar]
- Chung, S.W.; Chang, E.Y.; Lee, H.C.; Shin, M.Y.; Kim, B.E.; Ahn, K.M.; Lee, S.I. The relationships among severity score, behavioral problem, parental stress, maternal depression, and social support in children with atopic dermatitis. J. Asthma Allergy Clin. Immunol. 2005, 25, 39–44. [Google Scholar] [CrossRef]
- Lee, D.W.; Byun, D.G.; Kim, J.W. Diagnostic significance of clinical history of atopic dermatitis in Koreans by questionnaire. Korean J. Dermatol. 1997, 35, 443–449. [Google Scholar]
- Möller, H. Clinical aspects of atopic dermatitis in childhood. Acta Derm. Venereol. Suppl. 1981, 95, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Uehara, M.; Ofuji, S. Abnormal vascular reactions in atopic dermatitis. Arch. Dermatol. 1977, 113, 627–629. [Google Scholar] [CrossRef] [PubMed]
- Van Hecke, E.; Leys, G. Evolution of atopic dermatitis. Dermatology 1981, 163, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Staats, H.; Kieviet, A.; Hartig, T. Where to recover from attentional fatigue: An expectancy-value analysis of environmental preference. J. Environ. Psychol. 2003, 23, 147–157. [Google Scholar] [CrossRef]
- Buck, D. Gardens and Health: Implications for Policy and Practice; The Kong’s Fund: London, UK, 2016. [Google Scholar]
- Kaplan, R.; Kaplan, S. The Experience of Nature: A Psychological Perspective; Cambridge University Press: Cambridge, UK, 1989. [Google Scholar]
- Kaplan, S. The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar] [CrossRef]
- Soga, M.; Gaston, K.J.; Yamaura, Y. Gardening is beneficial for health: A meta-analysis. Prev. Med. Rep. 2017, 5, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.-Y.; Ko, D.-S.; Noh, J.-S.; Lee, B.-H.; Park, H.-S.; Park, J. Relation of physical activity and health-related quality of life in Korean elderly. J. Korea Contents Assoc. 2010, 10, 255–266. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Herzog, T.R.; Black, A.M.; Fountaine, K.A.; Knotts, D.J. Reflection and attentional recovery as distinctive benefits of restorative environments. J. Environ. Psychol. 1997, 17, 165–170. [Google Scholar] [CrossRef]
- Theodorou, A.; Panno, A.; Carrus, G.; Carbone, G.A.; Massullo, C.; Imperatori, C. Stay home, stay safe, stay green: The role of gardening activities on mental health during the COVID-19 home confinement. Urban For. Urban Green 2021, 61, 127091. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. Experimental study on the health benefits of garden landscape. Int. J. Environ. Res. Public Health 2017, 14, 829. [Google Scholar] [CrossRef] [PubMed]
- Thaneshwari, P.K.; Sharma, R.; Sahare, H.A. Therapeutic gardens in healthcare: A review. Ann. Biol. 2018, 34, 162–166. [Google Scholar]
- Ghanbari, S.; Jafari, F.; Bagheri, N.; Neamtolahi, S.; Shayanpour, R. Study of the effect of using purposeful activity (gardening) on depression of female resident in Golestan Dormitory of Ahvaz Jundishapur University of Medical Sciences. J. Rehabil. Sci. Res. 2015, 2, 8–11. [Google Scholar] [CrossRef]
- Gonzalez, M.T.; Hartig, T.; Patil, G.G.; Martinsen, E.W.; Kirkevold, M. Therapeutic horticulture in clinical depression: A prospective study of active components. J. Adv. Nurs. 2010, 66, 2002–2013. [Google Scholar] [CrossRef]
- Kam, M.C.; Siu, A.M. Evaluation of a horticultural activity programme for persons with psychiatric illness. Hong Kong J. Occup. Ther. 2010, 20, 80–86. [Google Scholar] [CrossRef]
- Baik, H.J.; Choi, S.R.; An, M.A.; Jin, H.Y. Garden Therapy; Korea Research Institute for People & Environment: Seoul, Republic of Korea, 2022. [Google Scholar]
- Yao, W.; Zhang, X.; Gong, Q. The effect of exposure to the natural environment on stress reduction: A meta-analysis. Urban For. Urban Green 2021, 57, 126932. [Google Scholar] [CrossRef]
- Söderback, I.; Söderström, M.; Schälander, E. Horticultural therapy: The ‘healing garden’and gardening in rehabilitation measures at Danderyd Hospital Rehabilitation Clinic, Sweden. Pediatr. Rehabil. 2004, 7, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Ro, E.; Lee, T.-J.; An, B.-C.; Hong, K.-P.; Yun, H.-J.; Park, E.-Y.; Cho, H.-R.; Yun, S.-Y.; Park, M. The multi-sites trial on the effects of therapeutic gardening on mental health and well-being. Int. J. Environ. Res. Public Health 2022, 19, 8046. [Google Scholar] [CrossRef] [PubMed]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Grahn, P.; Stigsdotter, U.A. Landscape planning and stress. Urban For. Urban Green 2003, 2, 1–18. [Google Scholar] [CrossRef]
- Baik, H.J.; Kim, H.J.; Jae, S.Y.; Yi, B.Y. Effects of Fragrance Components of Abies holophylla Max. on Stress Relief and Improvement of Vascular Function. J. People Plants Environ. 2018, 21, 223–232. [Google Scholar] [CrossRef]
- Teti, D.M.; Gelfand, D.M. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Dev. 1991, 62, 918–929. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.W.; Lee, B.; Park, K.H.; Jung, S.Y.; Kim, S.; Park, Y.S.; Baik, S.Y.; Kim, C.L.; Lee, W.H.; Lee, S.H.; et al. Development of Korean depression screening assessment: Phase II preliminary validation study. Korean J. Clin. Psychol. 2018, 37, 252–262. [Google Scholar] [CrossRef]
- Han, Y.; Jang, J.; Cho, E.; Choi, K.-H. Investigating how individual differences influence responses to the COVID-19 crisis: The role of maladaptive and five-factor personality traits. Pers. Individ. Dif. 2021, 176, 110786. [Google Scholar] [CrossRef] [PubMed]
- Bahk, Y.C.; Park, K.; Kim, N.; Lee, J.; Cho, S.; Jang, J.; Jung, D.; Chang, E.; Choi, K.-H. Psychological impact of COVID-19 in South Korea: A preliminary study. Korean J. Clin. Psychol. 2020, 39, 355–367. [Google Scholar] [CrossRef]
- Lim, Y.J. Psychometric properties of the satisfaction with life scale among Korean police officers, university students, and adolescents. Korean J. Psychol. Gen. 2012, 31, 877–896. [Google Scholar]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The satisfaction with life scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Hong, G.R.S.; Kang, H.-K.; Oh, E.; Park, Y.; Kim, H. Reliability and validity of the Korean version of the perceived stress scale-10 (K-PSS-10) in older adults. Res. Gerontol. Nurs. 2016, 9, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Choe, H.S.; Chung, O.B. The development of an inventory for measuring the parenting self-efficacy of Korean mothers. Korean J. Child Stud. 2001, 22, 1–15. [Google Scholar]
- Cho, S.C.; Lee, Y.S. Development of the Korean form of the Kovacs’ Children’s Depression Inventory. J. Korean Neuropsychiatr. Assoc. 1990, 29, 943–956. [Google Scholar]
- Stalder, J.; Taieb, A.; Atherton, D.; Bieber, P.; Bonifazi, E.; Broberg, A.; Calza, A.; Coleman, R.; De Prost, Y.; Gelmetti, C. Severity scoring of atopic dermatitis: The SCORAD index: Consensus report of the european task force on atopic dermatitis. Dermatology 1993, 186, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Park, G.H.; Park, J.H.; Hwang, Y.H.; Sung, M.S.; Kim, S.W. The correlation between the severity of atopic dermatitis classified by SCORing atopic dermatitis index and the laboratory tests. Allergy Asthma Respir. Dis. 2013, 1, 79–83. [Google Scholar] [CrossRef][Green Version]
- Park, S.G.; Noh, H.M.; Kweon, S.H.; Jo, E.H.; Jang, H.C.; Kim, H.k.; Park, H.J.; Kim, W.J.; Park, M.C. The Study on the Environmental Factors of Atopic Dermatitis in Oriental-Western Medicine. J. Korean Med. Ophthalmol. Otolaryngol. Derma 2018, 31, 52–70. [Google Scholar] [CrossRef]
- Imhof, R.E.; Berg, E.P.; Chilcott, R.P.; Ciortea, L.I.; Pascut, F.C.; Xiao, P. New instrument for measuring water vapour flux density from arbitrary surfaces. IFSCC Mag. 2002, 5, 297–301. [Google Scholar]
- Lee, S.M.; Jang, H.J.; Yun, H.K.; Jung, Y.B.; Hong, I.K. Effect of apartment community garden program on sense of community and stress. Int. J. Environ. Res. Public Health 2022, 19, 708. [Google Scholar] [CrossRef]
- Kim, M.Y.; Park, W.Y.; Kim, S.R. Effects of horticultural occupational therapy program using healing garden on quality of life of chronic stroke patients. J. People Plants Environ. 2014, 17, 451–455. [Google Scholar] [CrossRef]
- Howarth, M.; Brettle, A.; Hardman, M.; Maden, M. What is the evidence for the impact of gardens and gardening on health and well-being: A scoping review and evidence-based logic model to guide healthcare strategy decision making on the use of gardening approaches as a social prescription. BMJ Open 2020, 10, e036923. [Google Scholar] [CrossRef] [PubMed]
- Momtaz, R.I. Healing gardens-A review of design guidelines. Int. J. Curr. Eng. Technol. 2017, 7, 1864–1871. [Google Scholar]
- Dadvand, P.; Bartoll, X.; Basagaña, X.; Dalmau-Bueno, A.; Martinez, D.; Ambros, A.; Cirach, M.; Triguero-Mas, M.; Gascon, M.; Borrell, C. Green spaces and general health: Roles of mental health status, social support, and physical activity. Environ. Int. 2016, 91, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Murroni, V.; Cavalli, R.; Basso, A.; Borella, E.; Meneghetti, C.; Melendugno, A.; Pazzaglia, F. Effectiveness of therapeutic gardens for people with dementia: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 9595. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.H.; Kim, J.H. Update on management of pediatric atopic dermatitis. Allergy Asthma Respir. Dis. 2021, 9, 59–68. [Google Scholar] [CrossRef]
- Chida, Y.; Hamer, M.; Steptoe, A. A Bidirectional Relationship between Psychosocial Factors and Atopic Disorders: A Systematic Review and Meta-Analysis. Psychiatr. Med. 2008, 70, 102–116. [Google Scholar] [CrossRef] [PubMed]

| Variables | N (%) | ||
|---|---|---|---|
| CCT | NPC | ||
| Age | 41.55 ± 4.14 | 43.73 ± 4.14 | |
| Education | High school diploma | 3 (10.3) | 3 (10.0) |
| University degree | 23 (79.4) | 24 (80.0) | |
| Graduate school or higher | 3 (10.3) | 3 (10.0) | |
| Occupation | Housewife | 10 (34.5) | 9 (30.0) |
| Office worker | 16 (55.2) | 11 (36.7) | |
| Entrepreneur | 2 (6.9) | 6 (20.0) | |
| Other | 1 (3.4) | 7 (3.3) | |
| Number of Children | 1 | 3 (10.3) | 14 (46.7) |
| 2 | 17 (58.7) | 15 (50.0) | |
| 3 or more | 9 (31.0) | 1 (3.3) | |
| Age of Children | 9.45 ± 3.30 | 9.9 ± 3.58 | |
| Variables | Mean ± SD | N (%) |
|---|---|---|
| Age | 9.45 ± 3.30 | - |
| Height (cm) | 137.9 ± 22.5 | - |
| Weight (kg) | 36.6 ± 17.5 | - |
| Current medication use | Steroid ointment or lotion | 17 (58.6) |
| Antihistamine | 3 (10.3) | |
| Other | 2 (6.9) | |
| No use | 7 (24.1) | |
| Comorbid allergic disease | Asthma | 2 (6.9) |
| Allergic rhinitis | 17 (58.6) | |
| Urticaria | 1 (3.4) | |
| Food allergy | 2 (6.9) | |
| Metal allergy | 1 (3.4) | |
| None | 6 (20.7) |
| Variables | Group | df | Pre-Test | Post-Test | Cohen’s d | t | p |
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||||
| MHS:D | NPC | 29 | 9.28 (5.07) | 8.46 (7.26) | 0.13 | 0.531 | 0.531 NS |
| CCT | 28 | 8.59 (6.93) | 2.96 (2.47) | 1.08 | 4.554 | 0.000 *** | |
| MHS:A | NPC | 29 | 11.70 (7.34) | 11.35 (8.98) | 0.42 | 0.837 | 0.837 NS |
| CCT | 28 | 11.41 (7.33) | 4.54 (4.10) | 1.16 | 5.103 | 0.000 *** | |
| CORE | NPC | 29 | 2.77 (0.66) | 2.95(0.58) | 0.28 | 0.214 | 0.214 NS |
| CCT | 28 | 3.04 (0.70) | 3.57 (0.76) | 0.72 | −3.223 | 0.003 ** | |
| K-SWLS | NPC | 29 | 4.15 (1.26) | 3.84 (1.25) | 0.24 | 0.148 | 0.148 NS |
| CCT | 28 | 4.09 (1.26) | 4.69 (1.10) | 0.51 | −2.943 | 0.006 ** | |
| PSE | NPC | 29 | 3.73 (0.40) | 3.66 (0.44) | 0.17 | 0.205 | 0.205 NS |
| CCT | 28 | 3.71 (0.46) | 3.97 (0.48) | 0.57 | −2.990 | 0.006 ** | |
| PSS | NPC | 29 | 1.90 (0.50) | 1.82 (0.51) | 0.17 | 0.373 | 0.373 NS |
| CCT | 28 | 1.83 (0.39) | 1.39 (0.49) | 1.01 | 4.093 | 0.000 *** |
| Variables | MHS:D | MHS:A | CORE | K-SWLS | PSE | PSS |
|---|---|---|---|---|---|---|
| MHS:D | 1 | |||||
| MHS:A | 0.860 ** | 1 | ||||
| CORE | −0.543 ** | −0.522 ** | 1 | |||
| K-SWLS | −0.425 ** | −0.481 ** | 0.410 ** | 1 | ||
| PSE | −0.480 ** | −0.493 ** | 0.481 ** | 0.602 ** | 1 | |
| PSS | 0.608 ** | 0.606 ** | −0.624 ** | −0.506 ** | −0.566 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baik, H.; Choi, S.; An, M.; Jin, H.; Kang, I.; Yoon, W.; Yoo, Y. Effect of Therapeutic Gardening Program in Urban Gardens on the Mental Health of Children and Their Caregivers with Atopic Dermatitis. Healthcare 2024, 12, 919. https://doi.org/10.3390/healthcare12090919
Baik H, Choi S, An M, Jin H, Kang I, Yoon W, Yoo Y. Effect of Therapeutic Gardening Program in Urban Gardens on the Mental Health of Children and Their Caregivers with Atopic Dermatitis. Healthcare. 2024; 12(9):919. https://doi.org/10.3390/healthcare12090919
Chicago/Turabian StyleBaik, Hyunjin, Sueran Choi, Miae An, Hyeyoung Jin, Insoon Kang, Wonsuck Yoon, and Young Yoo. 2024. "Effect of Therapeutic Gardening Program in Urban Gardens on the Mental Health of Children and Their Caregivers with Atopic Dermatitis" Healthcare 12, no. 9: 919. https://doi.org/10.3390/healthcare12090919
APA StyleBaik, H., Choi, S., An, M., Jin, H., Kang, I., Yoon, W., & Yoo, Y. (2024). Effect of Therapeutic Gardening Program in Urban Gardens on the Mental Health of Children and Their Caregivers with Atopic Dermatitis. Healthcare, 12(9), 919. https://doi.org/10.3390/healthcare12090919






