Harnessing the Synergy of SGLT2 Inhibitors and Continuous Ketone Monitoring (CKM) in Managing Heart Failure among Patients with Type 1 Diabetes
Abstract
1. Introduction
2. Methodology
3. Epidemiology of HF in T1D
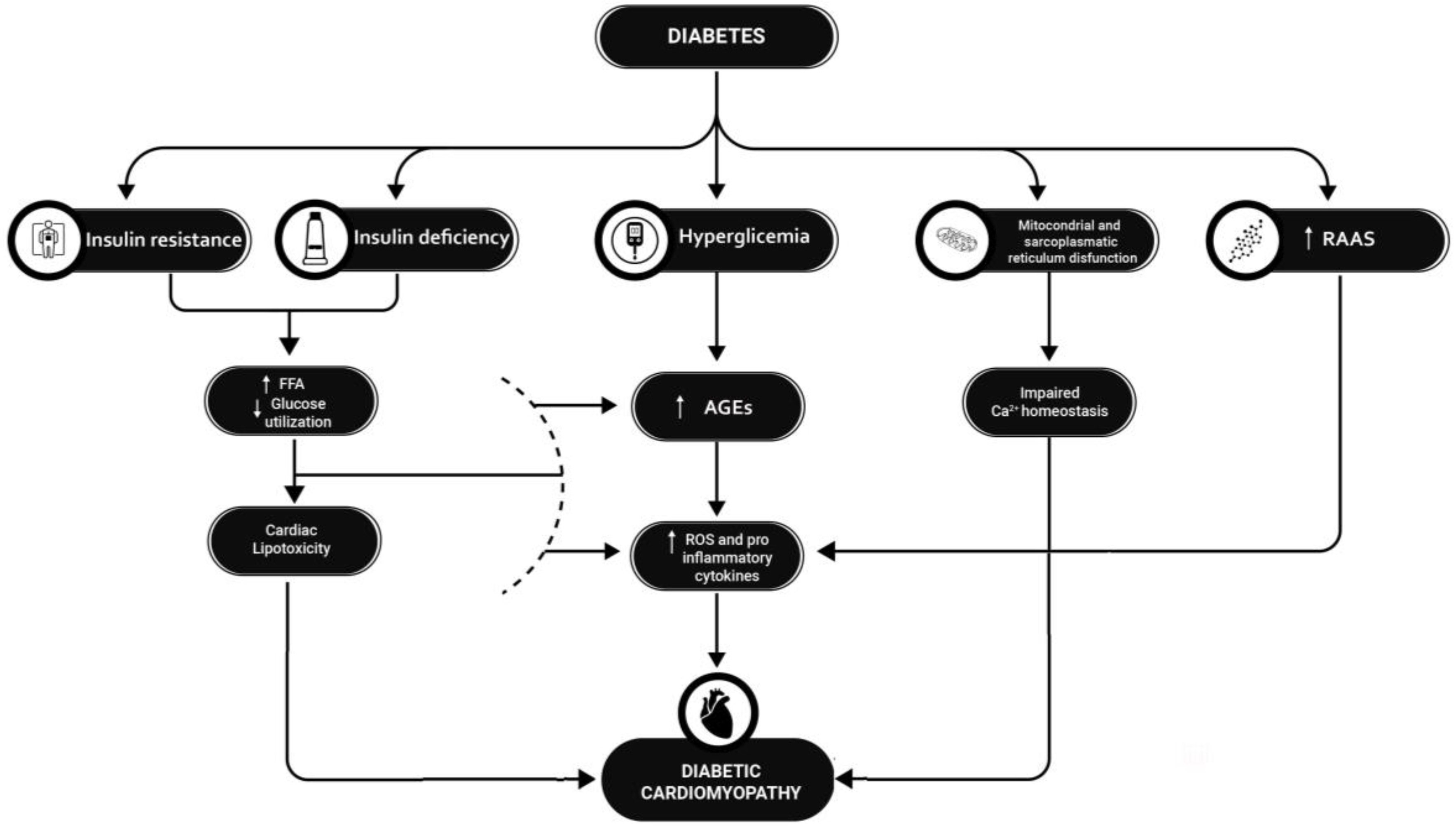
4. Pathophysiology
4.1. Abnormal Insulin Metabolic Signaling
4.2. Hyperglycemia and AGEs
4.3. Cardiac Lipotoxicity
4.4. Autonomic Neuropathy
4.5. Insulin Deficiency
4.6. Mitochondrial and Myocardial Sarcoplasmic Reticulum Dysfunction
4.7. Inappropriate Activation of RAAS System
5. Diagnosis
6. Prognosis
7. SGLT2-is in Subjects with Type 1 Diabetes and Heart Failure
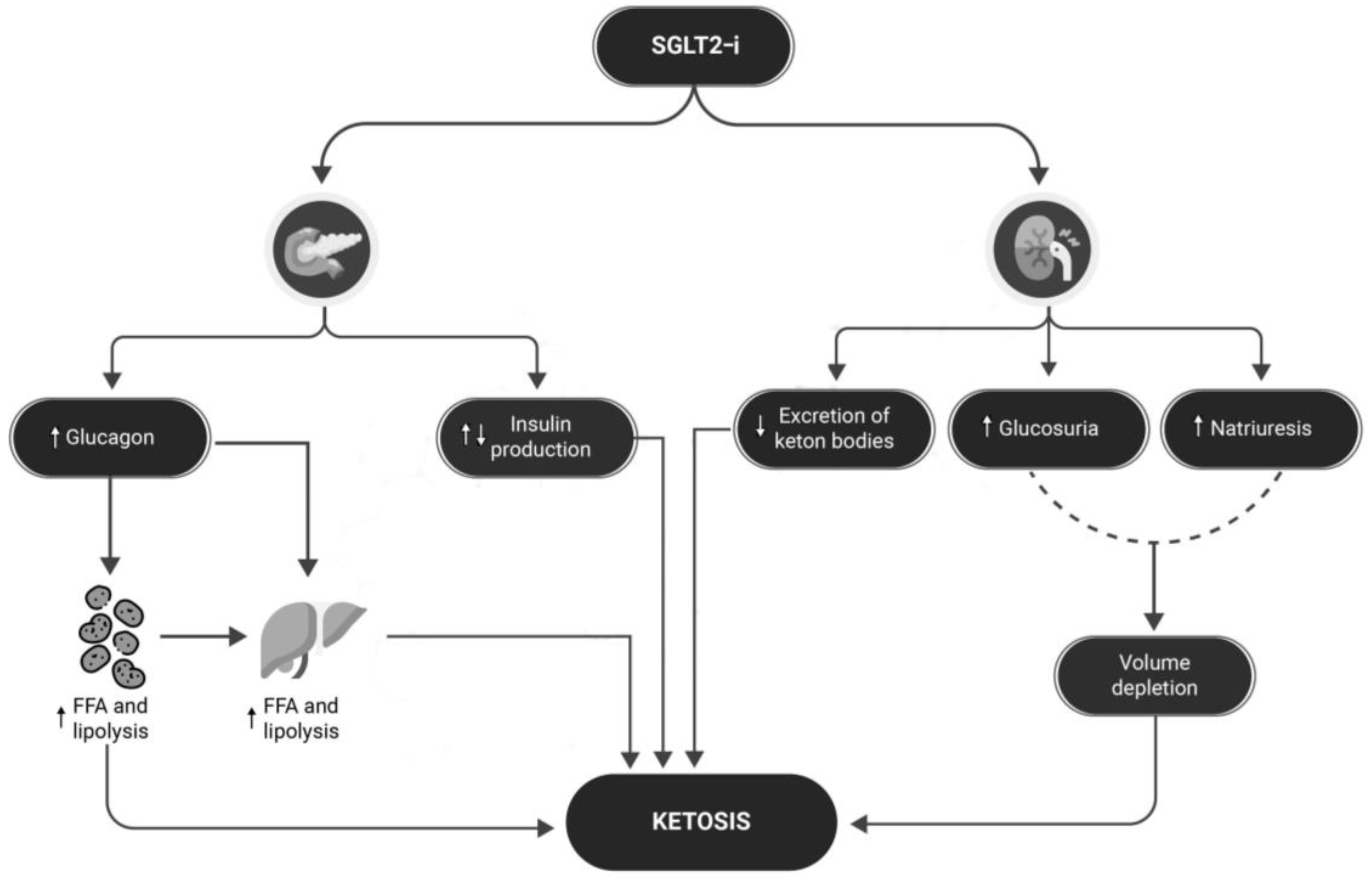
8. Ketoacidosis: Could This Problem Be Overcome?
9. Sensors for Continuous Monitoring of Ketonemia
9.1. Continuous Ketone Monitoring: A New Paradigm for Physiologic Monitoring
9.2. Utility of Ketone Measurement in the Prevention, Diagnosis, and Management of DKA
10. Limitations
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HF | Heart Failure |
| T1D | Type 1 Diabetes |
| T2D | Type 2 Diabetes |
| CV | Cardiovascular |
| SGLT2-i | Sodium–Glucose Cotransporter-2 Inhibitors |
| LVEF | Left Ventricular Ejection Fraction |
| HFrEF | Heart Failure with Reduced Ejection Fraction |
| HFpEF | Heart Failure with Preserved Ejection Fraction |
| RR | Relative Risk |
| CI | Confidence Interval |
| CV | Cardiovascular |
| DKA | Diabetic Ketoacidosis |
| IRS-1 | Insulin Receptor Substrate-1 |
| AKT | Protein Kinase B (also known as AKT) |
| GLUT4 | Glucose Transporter Type 4 |
| MAPK | Mitogen-Activated Protein Kinase |
| FFAs | Free Fatty Acids |
| AGEs | Advanced Glycation End-Products |
| ROS | Reactive Oxygen Species |
| RAAS | Renin–Angiotensin–Aldosterone System |
| LA | Left Atrial |
| HR | Hazard Ratio |
| DM | Diabetes Mellitus |
| PARs | Peroxisome Proliferator-Activated Receptors |
| MFAU | Myocardial Fatty Acid Utilization |
| MFAO | Myocardial Fatty Acid Oxidation |
| MGU | Myocardial Glucose Utilization |
| SERCA | Sarcoplasmic Reticulum Ca²⁺ ATPase |
| PERK | PKR-like ER Kinase |
| RCTs | Randomized Controlled Trials |
| GLP-1 | Glucagon-Like Peptide-1 |
| GIP | Glucose-Dependent Insulinotropic Polypeptide |
| CGM | Continuous Glucose Monitoring |
| METs | Metabolic Equivalents |
| CKM | Continuous Ketone Monitoring |
| CSIIs | Continuous Subcutaneous Insulin Infusion Systems |
References
- American Diabetes Association. Introduction: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021, 45 (Suppl. S1), S1–S2. [Google Scholar]
- McHugh, K.; DeVore, A.D.; Wu, J.; Matsouaka, R.A.; Fonarow, G.C.; Heidenreich, P.A.; Yancy, C.W.; Green, J.B.; Altman, N.; Hernandez, A.F. Heart Failure with Preserved Ejection Fraction and Diabetes: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 602–611. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [PubMed]
- Ohkuma, T.; Komorita, Y.; Peters, S.A.E.; Woodward, M. Diabetes as a risk factor for heart failure in women and men: A systematic review and meta-analysis of 47 cohorts including 12 million individuals. Diabetologia 2019, 62, 1550–1560. [Google Scholar] [CrossRef] [PubMed]
- Lehrke, M.; Marx, N. Diabetes Mellitus and Heart Failure. Am. J. Med. 2017, 130 (Suppl. S6), S40–S50. [Google Scholar] [CrossRef] [PubMed]
- Haji, M.; Erqou, S.; Fonarow, G.C.; Echouffo-Tcheugui, J.B. Type 1 diabetes and risk of heart failure: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2023, 202, 110805. [Google Scholar] [CrossRef] [PubMed]
- McAllister, D.A.; Read, S.H.; Kerssens, J.; Livingstone, S.; McGurnaghan, S.; Jhund, P.; Petrie, J.; Sattar, N.; Fischbacher, C.; Kristensen, S.L.; et al. Incidence of Hospitalization for Heart Failure and Case-Fatality Among 3.25 Million People with and without Diabetes Mellitus. Circulation 2018, 138, 2774–2786. [Google Scholar] [CrossRef] [PubMed]
- Kenny, H.C.; Abel, E.D. Heart Failure in Type 2 Diabetes Mellitus. Circ. Res. 2019, 124, 121–141. [Google Scholar] [CrossRef] [PubMed]
- Seferović, P.M.; Petrie, M.C.; Filippatos, G.S.; Anker, S.D.; Rosano, G.; Bauersachs, J.; Paulus, W.J.; Komajda, M.; Cosentino, F.; de Boer, R.A.; et al. Type 2 diabetes mellitus and heart failure: A position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 853–872. [Google Scholar] [CrossRef] [PubMed]
- Julián, M.T.; de Oca, A.P.-M.; Julve, J.; Alonso, N. The double burden: Type 1 diabetes and heart failure—A comprehensive review. Cardiovasc. Diabetol. 2024, 23, 65. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [PubMed]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin–Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Pfeffer, M.A.; Swedberg, K.; Granger, C.B.; Held, P.; McMurray, J.J.; Michelson, E.L.; Olofsson, B.; Ostergren, J. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-Preserved Trial. Lancet 2003, 362, 777–781. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. Type 1 Diabetes. I.D. Federation. 2020. Available online: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf (accessed on 1 January 2024).
- Avogaro, A.; Azzolina, D.; Fadini, G.P.; Baldi, I. Incidence of heart failure in patients with type 1 diabetes: A systematic review of observational studies. J. Endocrinol. Investig. 2021, 44, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Kluger, A.Y.; Tecson, K.M.; Barbin, C.M.; Lee, A.Y.; Lerma, E.V.; Rosol, Z.P.; Rangaswami, J.; Lepor, N.E.; Cobble, M.E.; McCullough, P.A. Cardiorenal Outcomes in the CANVAS, DECLARE-TIMI 58, and EMPA-REG OUTCOME Trials: A Systematic Review. Rev. Cardiovasc. Med. 2018, 19, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Petrie, D.; Lung, T.W.; Rawshani, A.; Palmer, A.J.; Svensson, A.M.; Eliasson, B.; Clarke, P. Recent trends in life expectancy for people with type 1 diabetes in Sweden. Diabetologia 2016, 59, 1167–1176. [Google Scholar] [CrossRef] [PubMed]
- Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Mortality in Type 1 Diabetes in the DCCT/EDIC Versus the General Population. Diabetes Care 2016, 39, 1378–1383. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.B.; Han, K.; Kim, B.; Lee, S.E.; Jun, J.E.; Ahn, J.; Kim, G.; Jin, S.M.; Kim, J.H. Risk of early mortality and cardiovascular disease in type 1 diabetes: A comparison with type 2 diabetes, a nationwide study. Cardiovasc. Diabetol. 2019, 18, 157. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, M.R.; Petrie, M.C.; Varyani, F.; Östergren, J.; Michelson, E.L.; Young, J.B.; Solomon, S.D.; Granger, C.B.; Swedberg, K.; Yusuf, S.; et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: An analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur. Heart J. 2008, 29, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Gerber, Y.; Weston, S.A.; Redfield, M.M.; Chamberlain, A.M.; Manemann, S.M.; Jiang, R.; Killian, J.M.; Roger, V.L. A Contemporary Appraisal of the Heart Failure Epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern. Med. 2015, 175, 996. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Lyass, A.; Enserro, D.; Larson, M.G.; Ho, J.E.; Kizer, J.R.; Gottdiener, J.S.; Psaty, B.M.; Vasan, R.S. Temporal Trends in the Incidence of and Mortality Associated with Heart Failure with Preserved and Reduced Ejection Fraction. JACC Heart Fail. 2018, 6, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Bode, D.; Semmler, L.; Wakula, P.; Hegemann, N.; Primessnig, U.; Beindorff, N.; Powell, D.; Dahmen, R.; Ruetten, H.; Oeing, C.; et al. Dual SGLT-1 and SGLT-2 inhibition improves left atrial dysfunction in HFpEF. Cardiovasc. Diabetol. 2021, 20, 7. [Google Scholar] [CrossRef] [PubMed]
- Kumbhani, D.J. FACC Breakthrough Results for Jardiance® (Empagliflozin) Confirm EMPEROR-Preserved as First and only Successful Trial for Heart Failure with Preserved Ejection Fraction. 2021. Available online: https://investor.lilly.com/news-releases/news-release-details/breakthrough-results-jardiancer-empagliflozin-confirm-emperor (accessed on 1 January 2024).
- AIFA. Nota Informativa Importante su FORXIGA (Dapagliflozin). 2021. Available online: https://www.aifa.gov.it/-/nota-informativa-importante-su-forxiga-dapagliflozin- (accessed on 1 January 2024).
- Dapagliflozin (Forxiga): No Longer Authorised for Treatment of Type 1 Diabetes Mellitus. Available online: https://www.gov.uk/drug-safety-update/dapagliflozin-forxiga-no-longer-authorised-for-treatment-of-type-1-diabetes-mellitus (accessed on 1 January 2024).
- Lind, M.; Bounias, I.; Olsson, M.; Gudbjörnsdottir, S.; Svensson, A.M.; Rosengren, A. Glycaemic control and incidence of heart failure in 20,985 patients with type 1 diabetes: An observational study. Lancet 2011, 378, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmsen, L.; Rosengren, A.; Eriksson, H.; Lappas, G. Heart failure in the general population of men--morbidity, risk factors and prognosis. J. Intern. Med. 2001, 249, 253–261. [Google Scholar]
- Chadalavada, S.; Jensen, M.T.; Aung, N.; Cooper, J.; Lekadir, K.; Munroe, P.B.; Petersen, S.E. Women with Diabetes Are at Increased Relative Risk of Heart Failure Compared to Men: Insights from UK Biobank. Front. Cardiovasc. Med. 2021, 8, 658726. [Google Scholar] [CrossRef] [PubMed]
- Rawshani, A.; Sattar, N.; Franzén, S.; Rawshani, A.; Hattersley, A.T.; Svensson, A.M.; Eliasson, B.; Gudbjörnsdottir, S. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: A nationwide, register-based cohort study. Lancet 2018, 392, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Demarco, V.G.; Sowers, J.R. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat. Rev. Endocrinol. 2016, 12, 144–153. [Google Scholar] [CrossRef]
- Dhalla, N.S.; Pierce, G.N.; Innes, I.R.; Beamish, R.E. Pathogenesis of cardiac dysfunction in diabetes mellitus. Can. J. Cardiol. 1985, 1, 263–281. [Google Scholar] [PubMed]
- Belke, D.D.; Larsen, T.S.; Gibbs, E.M.; Severson, D.L. Altered metabolism causes cardiac dysfunction in perfused hearts from diabetic (db/db) mice. Am. J. Physiol.-Endocrinol. Metab. 2000, 279, E1104–E1113. [Google Scholar] [CrossRef] [PubMed]
- Wallace, A.S.; Chang, A.R.; Shin, J.-I.; Reider, J.; Echouffo-Tcheugui, J.B.; Grams, M.E.; Selvin, E. Obesity and Chronic Kidney Disease in US Adults with Type 1 and Type 2 Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2022, 107, 1247–1256. [Google Scholar] [CrossRef] [PubMed]
- Erqou, S.; Lee, C.-T.C.; Suffoletto, M.; Echouffo-Tcheugui, J.B.; De Boer, R.A.; Van Melle, J.P.; Adler, A.I. Association between glycated haemoglobin and the risk of congestive heart failure in diabetes mellitus: Systematic review and meta-analysis. Eur. J. Heart Fail. 2013, 15, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.B.; Goldfine, A.B.; Timimi, F.K.; Ting, H.H.; Roddy, M.-A.; Simonson, D.C.; Creager, M.A. Acute Hyperglycemia Attenuates Endothelium-Dependent Vasodilation in Humans In Vivo. Circulation 1998, 97, 1695–1701. [Google Scholar] [CrossRef] [PubMed]
- Way, K.J.; Katai, N.; King, G.L. Protein kinase C and the development of diabetic vascular complications. Diabet. Med. 2001, 18, 945–959. [Google Scholar] [CrossRef] [PubMed]
- Genuth, S.; Sun, W.; Cleary, P.; Sell, D.R.; Dahms, W.; Malone, J.; Sivitz, W.; Monnier, V.M. Glycation and carboxymethyllysine levels in skin collagen predict the risk of future 10-year progression of diabetic retinopathy and nephropathy in the diabetes control and complications trial and epidemiology of diabetes interventions and complications participants with type 1 diabetes. Diabetes 2005, 54, 3103–3111. [Google Scholar] [PubMed]
- Xanthis, A.; Hatzitolios, A.; Fidani, S.; Befani, C.; Giannakoulas, G.; Koliakos, G. Receptor of Advanced Glycation End Products (RAGE) Positively Regulates CD36 Expression and Reactive Oxygen Species Production in Human Monocytes in Diabetes. Angiology 2009, 60, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Soro-Paavonen, A.; Zhang, W.Z.; Venardos, K.; Coughlan, M.T.; Harris, E.; Tong, D.C.; Brasacchio, D.; Paavonen, K.; Chin-Dusting, J.; Cooper, M.E.; et al. Advanced glycation end-products induce vascular dysfunction via resistance to nitric oxide and suppression of endothelial nitric oxide synthase. J. Hypertens. 2010, 28, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.-W.; Bai, K.-J.; Lee, T.-I.; Chao, T.-F.; Kao, Y.-H.; Chen, Y.-J. PPARs modulate cardiac metabolism and mitochondrial function in diabetes. J. Biomed. Sci. 2017, 24, 5. [Google Scholar] [CrossRef] [PubMed]
- Balcıoğlu, A.S. Diabetes and cardiac autonomic neuropathy: Clinical manifestations, cardiovascular consequences, diagnosis and treatment. World J. Diabetes 2015, 6, 80. [Google Scholar] [CrossRef] [PubMed]
- Raev, D.C. Which left ventricular function is impaired earlier in the evolution of diabetic cardiomyopathy? An echocardiographic study of young type I diabetic patients. Diabetes Care 1994, 17, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Fein, F.S.; Strobeck, J.E.; Malhotra, A.; Scheuer, J.; Sonnenblick, E.H. Reversibility of diabetic cardiomyopathy with insulin in rats. Circ. Res. 1981, 49, 1251–1261. [Google Scholar] [CrossRef] [PubMed]
- Penpargkul, S.; Schaible, T.; Yipintsoi, T.; Scheuer, J. The effect of diabetes on performance and metabolism of rat hearts. Circ. Res. 1980, 47, 911–921. [Google Scholar] [CrossRef] [PubMed]
- Herrero, P.; Peterson, L.R.; McGill, J.B.; Matthew, S.; Lesniak, D.; Dence, C.; Gropler, R.J. Increased myocardial fatty acid metabolism in patients with type 1 diabetes mellitus. J. Am. Coll. Cardiol. 2006, 47, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Dillmann, W.H. Diabetic Cardiomyopathy. Circ. Res. 2019, 124, 1160–1162. [Google Scholar] [CrossRef] [PubMed]
- Hölscher, M.E.; Bode, C.; Bugger, H. Diabetic Cardiomyopathy: Does the Type of Diabetes Matter? Int. J. Mol. Sci. 2016, 17, 2136. [Google Scholar] [CrossRef]
- Lin, Y.; Tang, Y.; Wang, F. The Protective Effect of HIF-1α in T Lymphocytes on Cardiac Damage in Diabetic Mice. Ann. Clin. Lab. Sci. 2016, 46, 32–43. [Google Scholar]
- Liu, Z.W.; Zhu, H.T.; Chen, K.L.; Dong, X.; Wei, J.; Qiu, C.; Xue, J.H. Protein kinase RNA-like endoplasmic reticulum kinase (PERK) signaling pathway plays a major role in reactive oxygen species (ROS)-mediated endoplasmic reticulum stress-induced apoptosis in diabetic cardiomyopathy. Cardiovasc. Diabetol. 2013, 12, 158. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.-Y.; Hu, S.-J.; Li, J.; Mou, Y.; Chen, B.-P.; Xia, Q. Decreased cardiac sarcoplasmic reticulum Ca2+-ATPase activity contributes to cardiac dysfunction in streptozotocin-induced diabetic rats. J. Physiol. Biochem. 2006, 62, 1. [Google Scholar] [CrossRef] [PubMed]
- Marciniak, S.J.; Ron, D. Endoplasmic Reticulum Stress Signaling in Disease. Physiol. Rev. 2006, 86, 1133–1149. [Google Scholar] [CrossRef] [PubMed]
- Yi, C.H.; Vakifahmetoglu-Norberg, H.; Yuan, J. Integration of apoptosis and metabolism. Cold Spring Harb. Symp. Quant. Biol. 2011, 76, 375–387. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.P.; Le, B.; Khode, R.; Baker, K.M.; Kumar, R. Intracellular angiotensin II production in diabetic rats is correlated with cardiomyocyte apoptosis, oxidative stress, and cardiac fibrosis. Diabetes 2008, 57, 3297–3306. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.A. Impact of hyperglycemia on the renin angiotensin system in early human type 1 diabetes mellitus. J. Am. Soc. Nephrol. 1999, 10, 1778–1785. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.E.; Zern, E.K.; Wooster, L.; Bailey, C.S.; Cunningham, T.; Eisman, A.S.; Hardin, K.M.; Zampierollo, G.A.; Jarolim, P.; Pappagianopoulos, P.P.; et al. Differential Clinical Profiles, Exercise Responses, and Outcomes Associated with Existing HFpEF Definitions. Circulation 2019, 140, 353–365. [Google Scholar] [CrossRef]
- Reddy, Y.N.V.; Carter, R.E.; Obokata, M.; Redfield, M.M.; Borlaug, B.A. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure with Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Schilling, J.D.; Mann, D.L. Diabetic Cardiomyopathy. Heart Fail. Clin. 2012, 8, 619–631. [Google Scholar] [CrossRef]
- Tofte, N.; Theilade, S.; Winther, S.A.; Birkelund, S.; Goetze, J.P.; Hansen, T.W.; Rossing, P. Comparison of Natriuretic Peptides as Risk Markers for All-Cause Mortality and Cardiovascular and Renal Complications in Individuals with Type 1 Diabetes. Diabetes Care 2021, 44, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Gohar, A.; Rutten, F.H.; den Ruijter, H.; Kelder, J.C.; von Haehling, S.; Anker, S.D.; Möckel, M.; Hoes, A.W. Mid-regional pro-atrial natriuretic peptide for the early detection of non-acute heart failure. Eur. J. Heart Fail. 2019, 21, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Costacou, T.; Saenger, A.K.; Orchard, T.J. High-Sensitivity Cardiac Troponin-T and N-Terminal Prohormone of B-Type Natriuretic Peptide in Relation to Cardiovascular Outcomes in Type 1 Diabetes. Diabetes Care 2020, 43, 2199–2207. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, M.; Bjornstad, P.; Frank, B.S.; Baumgartner, A.; Truong, U.; Enge, D.; von Alvensleben, J.C.; Mitchell, M.B.; Ivy, D.D.; Barker, A.J.; et al. Frequency of Reduced Left Ventricular Contractile Efficiency and Discoordinated Myocardial Relaxation in Patients Aged 16 to 21 Years with Type 1 Diabetes Mellitus (from the Emerald Study). Am. J. Cardiol. 2020, 128, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, I.; Brendorp, B.; Seibæk, M.; Burchardt, H.; Hildebrandt, P.; Køber, L.; Torp-Pedersen, C. Influence of diabetes and diabetes-gender interaction on the risk of death in patients hospitalized with congestive heart failure. J. Am. Coll. Cardiol. 2004, 43, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; Espeland, M.A.; et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N. Engl. J. Med. 2013, 369, 145–154. [Google Scholar] [PubMed]
- Gregg, E.W.; Jakicic, J.M.; Blackburn, G.; Bloomquist, P.; Bray, G.A.; Clark, J.M.; Coday, M.; Curtis, J.M.; Egan, C.; Evans, M.; et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar] [PubMed]
- Liu, C.; Wu, D.; Zheng, X.; Li, P.; Li, L. Efficacy and safety of metformin for patients with type 1 diabetes mellitus: A meta-analysis. Diabetes Technol. Ther. 2015, 17, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.; Perkovic, V.; Matthews, D.R. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 2099. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Szarek, M.; Steg, P.G.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Voors, A.A.; Metra, M.; et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N. Engl. J. Med. 2021, 384, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Szarek, M.; Pitt, B.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Inzucchi, S.E.; Kosiborod, M.N.; et al. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. N. Engl. J. Med. 2020, 384, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Filippatos, G.; Butler, J.; Farmakis, D.; Zannad, F.; Ofstad, A.P.; Ferreira, J.P.; Green, J.B.; Rosenstock, J.; Schnaidt, S.; Brueckmann, M.; et al. Empagliflozin for Heart Failure with Preserved Left Ventricular Ejection Fraction with and without Diabetes. Circulation 2022, 146, 676–686. [Google Scholar] [CrossRef]
- Modi, A.; Agrawal, A.; Morgan, F. Euglycemic Diabetic Ketoacidosis: A Review. Curr. Diabetes Rev. 2017, 13, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Calimag, A.P.P.; Chlebek, S.; Lerma, E.V.; Chaiban, J.T. Diabetic ketoacidosis. Dis. Mon. 2023, 69, 101418. [Google Scholar] [CrossRef] [PubMed]
- Plewa, M.C.; Bryant, M.; King-Thiele, R. Euglycemic Diabetic Ketoacidosis. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2024. [Google Scholar]
- Abu-Zaid, A.; Altowairqi, A.K.; Dissanayaka, T.; Oganesyan, A.; Bhagavathul, A.S.; Alhabeeb, H.; Baradhwan, A.; Alomar, S.; Tom, S. A systematic review and dose-response meta-analysis on the efficacy of dapagliflozin in patients with type 1 diabetes mellitus. Pharmacol. Res. 2021, 165, 105456. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Cassader, M.; Paschetta, E. Efficacy and safety of dual SGLT 1/2 inhibitor sotagliflozin in type 1 diabetes: Meta-analysis of randomised controlled trials. BMJ 2019, 365, l1328. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Marquard, J.; Laffel, L.M.; Neubacher, D.; Kaspers, S.; Cherney, D.Z.; Zinman, B.; Skyler, J.S.; George, J.; Soleymanlou, N.; et al. Empagliflozin as Adjunctive to Insulin Therapy in Type 1 Diabetes: The EASE Trials. Diabetes Care 2018, 41, 2560–2569. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Hwang, S.D.; Lim, S. Effects of Sodium-Glucose Cotransporter Inhibitor/Glucagon-Like Peptide-1 Receptor Agonist Add-On to Insulin Therapy on Glucose Homeostasis and Body Weight in Patients with Type 1 Diabetes: A Network Meta-Analysis. Front. Endocrinol. 2020, 11, 553. [Google Scholar] [CrossRef] [PubMed]
- Merovci, A.; Solis-Herrera, C.; Daniele, G.; Eldor, R.; Fiorentino, T.V.; Tripathy, D.; Xiong, J.; Perez, Z.; Norton, L.; Abdul-Ghani, M.A.; et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J. Clin. Investig. 2014, 124, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.I.; Blau, J.E.; Rother, K.I. SGLT2 Inhibitors May Predispose to Ketoacidosis. J. Clin. Endocrinol. Metab. 2015, 100, 2849–2852. [Google Scholar] [CrossRef]
- Hanas, R.; Lindgren, F.; Lindblad, B. A 2-yr national population study of pediatric ketoacidosis in Sweden: Predisposing conditions and insulin pump use. Pediatr. Diabetes 2009, 10, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Realsen, J.; Goettle, H.; Chase, H.P. Morbidity and mortality of diabetic ketoacidosis with and without insulin pump care. Diabetes Technol. Ther. 2012, 14, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Danne, T.; Garg, S.; Peters, A.L.; Buse, J.B.; Mathieu, C.; Pettus, J.H.; Alexander, C.M.; Battelino, T.; Ampudia-Blasco, F.J.; Bode, B.W.; et al. International Consensus on Risk Management of Diabetic Ketoacidosis in Patients with Type 1 Diabetes Treated with Sodium–Glucose Cotransporter (SGLT) Inhibitors. Diabetes Care 2019, 42, 1147–1154. [Google Scholar] [CrossRef]
- Tehrani, F.; Teymourian, H.; Wuerstle, B.; Kavner, J.; Patel, R.; Furmidge, A.; Aghavali, R.; Hosseini-Toudeshki, H.; Brown, C.; Zhang, F.; et al. An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 2022, 6, 1214–1224. [Google Scholar] [CrossRef]
- Goldenberg, R.M.; Gilbert, J.D.; Hramiak, I.M.; Woo, V.C.; Zinman, B. Sodium-glucose co-transporter inhibitors, their role in type 1 diabetes treatment and a risk mitigation strategy for preventing diabetic ketoacidosis: The STOP DKA Protocol. Diabetes Obes. Metab. 2019, 21, 2192–2202. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Peters, A.L.; Buse, J.B.; Danne, T. Strategy for Mitigating DKA Risk in Patients with Type 1 Diabetes on Adjunctive Treatment with SGLT Inhibitors: A STICH Protocol. Diabetes Technol. Ther. 2018, 20, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.Y.; Shang, T.; Koliwad, S.K.; Klonoff, D.C. Continuous Ketone Monitoring: A New Paradigm for Physiologic Monitoring. J. Diabetes Sci. Technol. 2021, 15, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Abbott. Abbott’s Biowearable: One Sensor for Glucose, Ketones. 2022. Available online: https://www.abbott.com/corpnewsroom/strategy-and-strength/abbotts-biowearable-one-sensor-for-glucose-ketones.html (accessed on 1 January 2024).
- Misra, S.; Oliver, N.S. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Diabet. Med. 2015, 32, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, C.A.; Nakhla, M.; Derraik, J.G.; Gunn, A.J.; Daneman, D.; Cutfield, W.S. Preventing Diabetic Ketoacidosis. Pediatr. Clin. N. Am. 2015, 62, 857–871. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tecce, N.; de Alteriis, G.; de Alteriis, G.; Verde, L.; Tecce, M.F.; Colao, A.; Muscogiuri, G. Harnessing the Synergy of SGLT2 Inhibitors and Continuous Ketone Monitoring (CKM) in Managing Heart Failure among Patients with Type 1 Diabetes. Healthcare 2024, 12, 753. https://doi.org/10.3390/healthcare12070753
Tecce N, de Alteriis G, de Alteriis G, Verde L, Tecce MF, Colao A, Muscogiuri G. Harnessing the Synergy of SGLT2 Inhibitors and Continuous Ketone Monitoring (CKM) in Managing Heart Failure among Patients with Type 1 Diabetes. Healthcare. 2024; 12(7):753. https://doi.org/10.3390/healthcare12070753
Chicago/Turabian StyleTecce, Nicola, Giorgio de Alteriis, Giulia de Alteriis, Ludovica Verde, Mario Felice Tecce, Annamaria Colao, and Giovanna Muscogiuri. 2024. "Harnessing the Synergy of SGLT2 Inhibitors and Continuous Ketone Monitoring (CKM) in Managing Heart Failure among Patients with Type 1 Diabetes" Healthcare 12, no. 7: 753. https://doi.org/10.3390/healthcare12070753
APA StyleTecce, N., de Alteriis, G., de Alteriis, G., Verde, L., Tecce, M. F., Colao, A., & Muscogiuri, G. (2024). Harnessing the Synergy of SGLT2 Inhibitors and Continuous Ketone Monitoring (CKM) in Managing Heart Failure among Patients with Type 1 Diabetes. Healthcare, 12(7), 753. https://doi.org/10.3390/healthcare12070753







