Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance
Abstract
1. Introduction
1.1. New Contribution
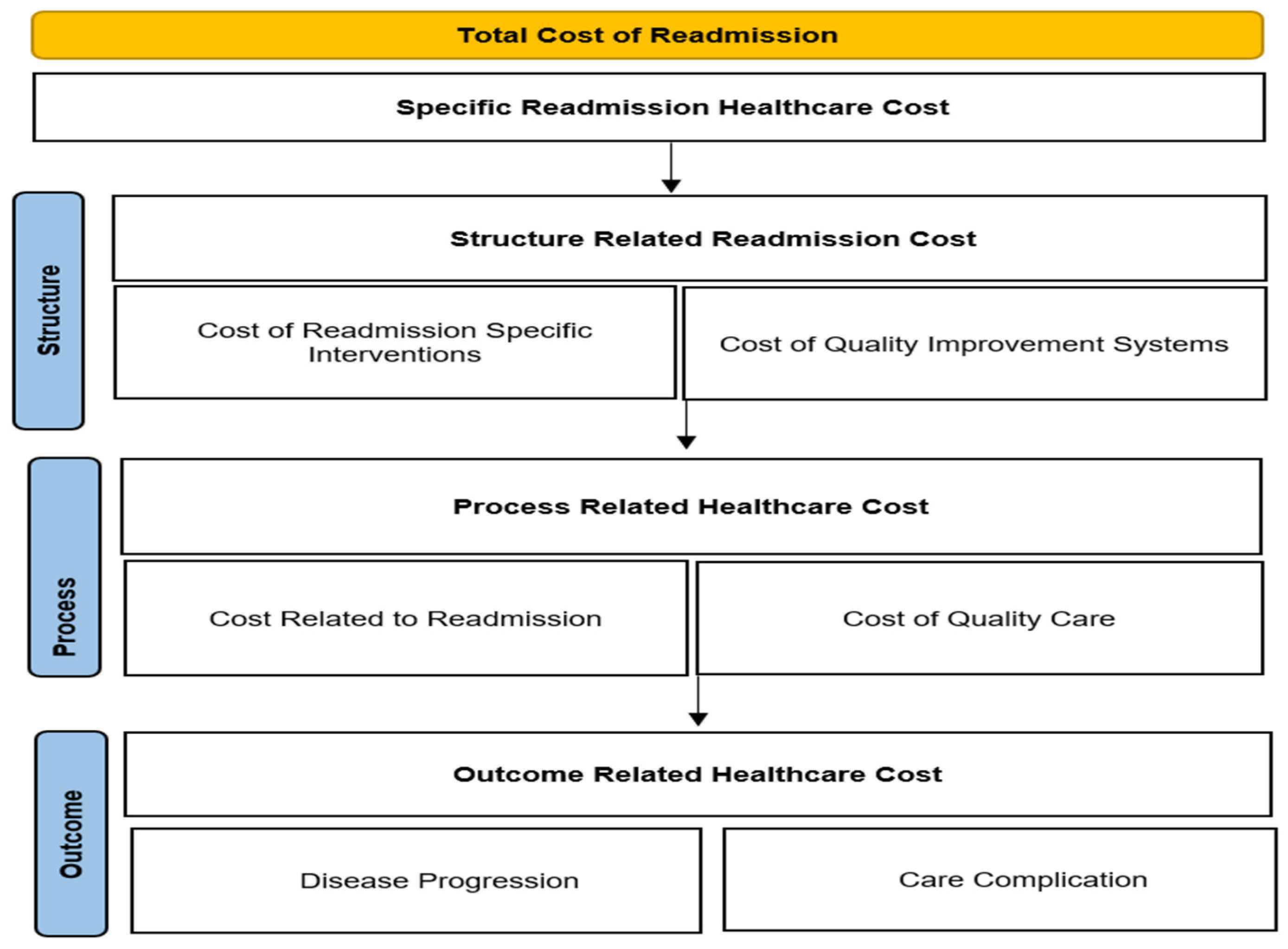
1.2. Conceptual Framework
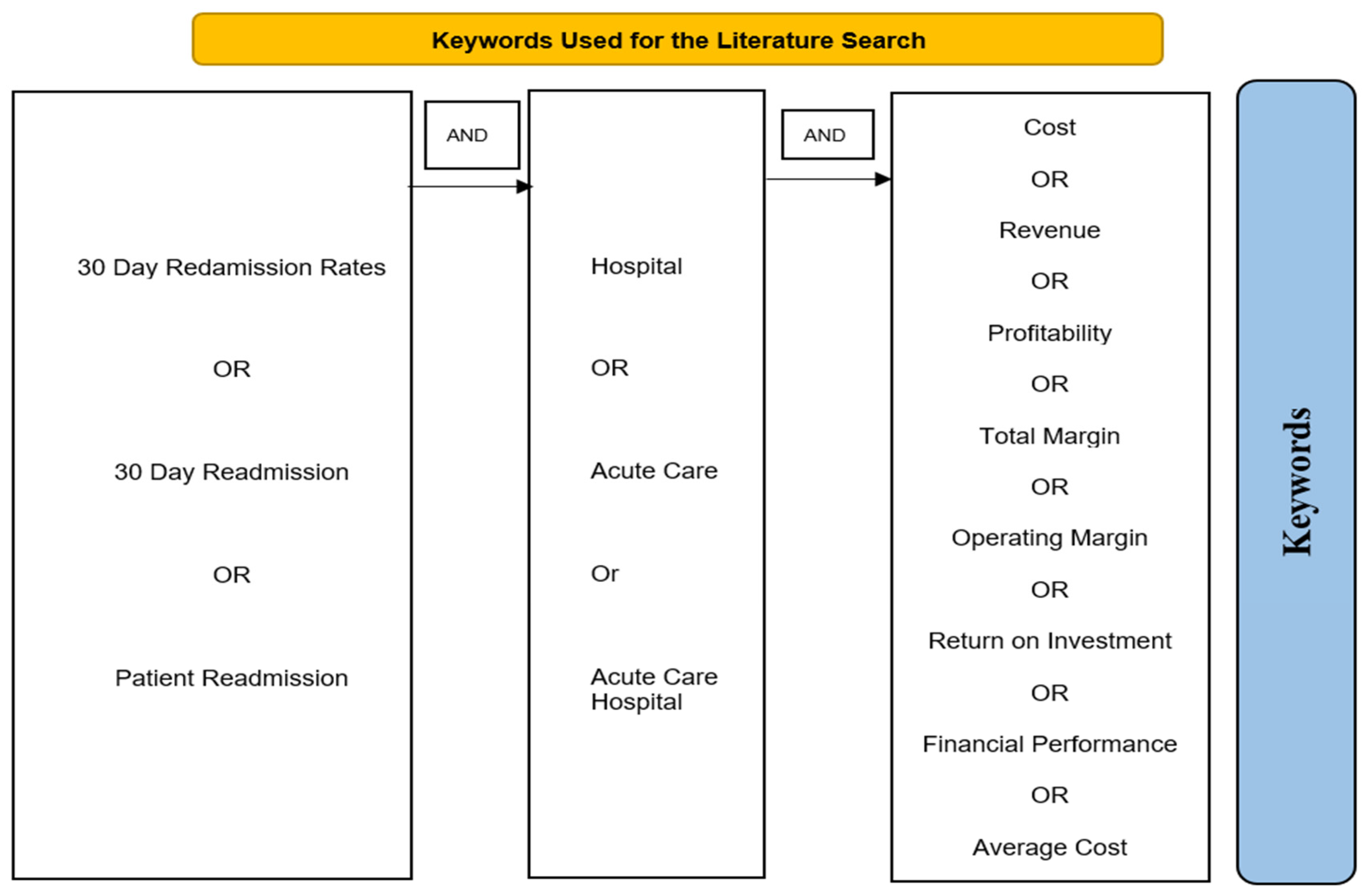
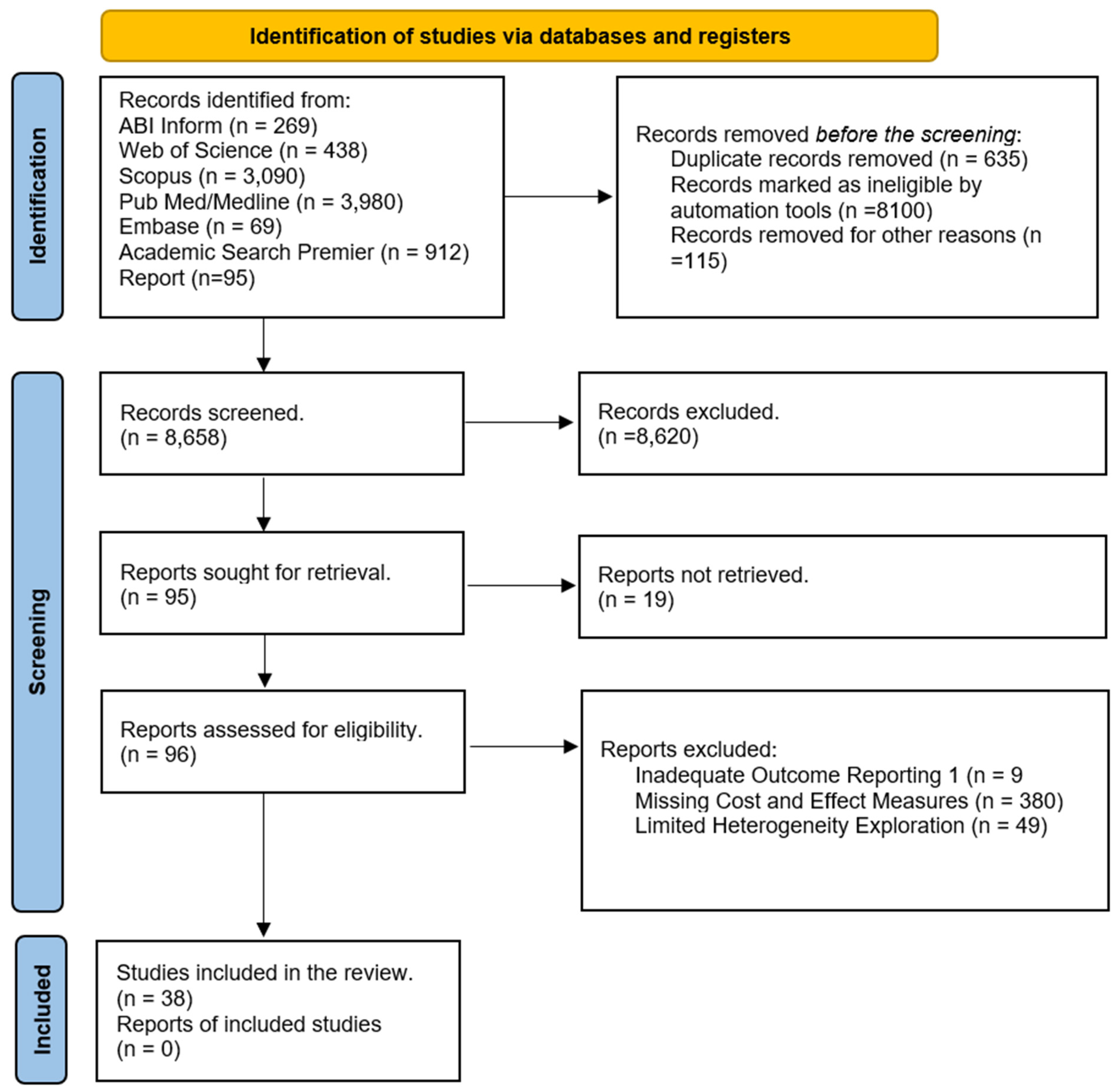
2. Methods
2.1. Outcomes
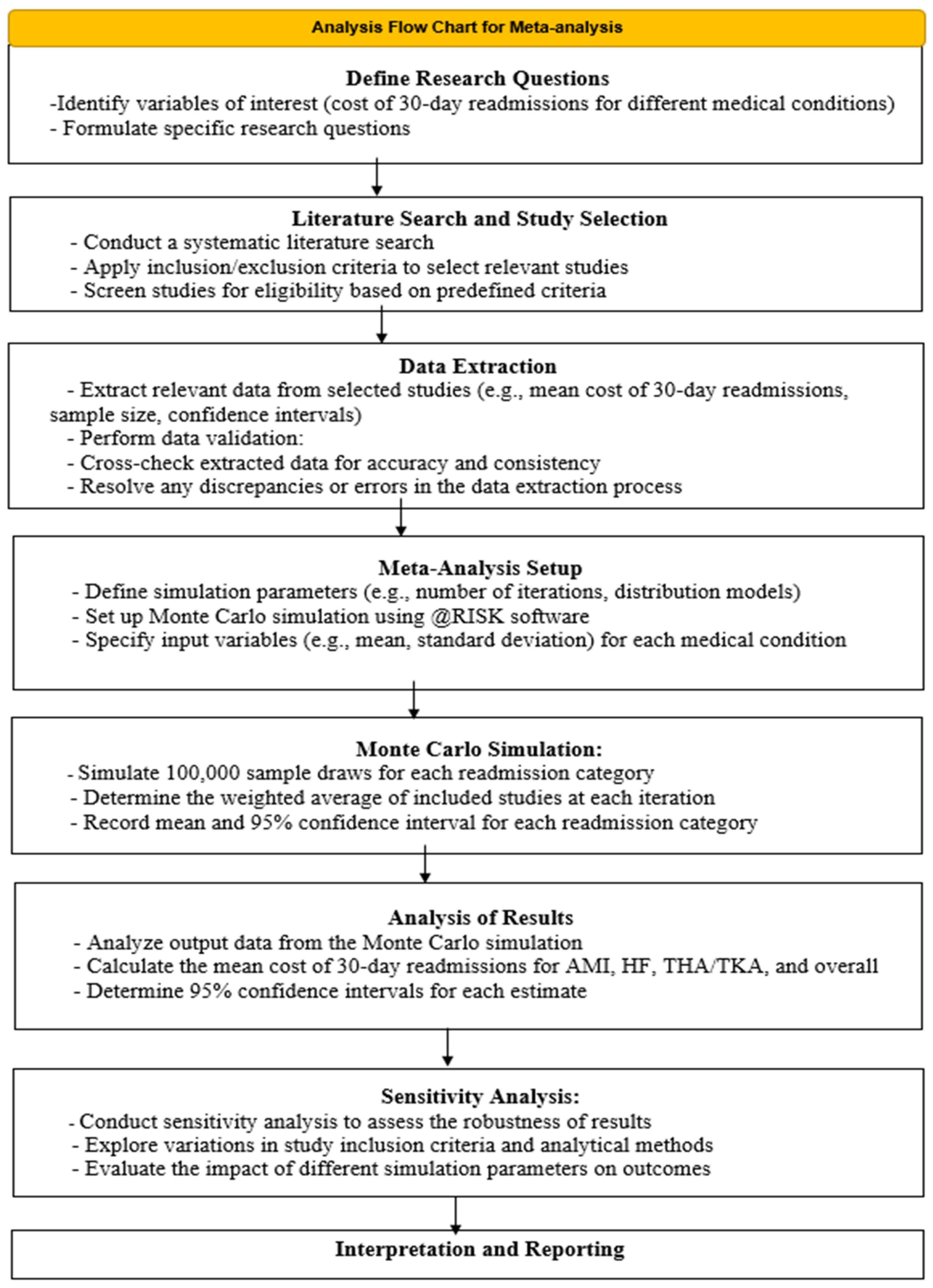
2.2. Statistical Analysis
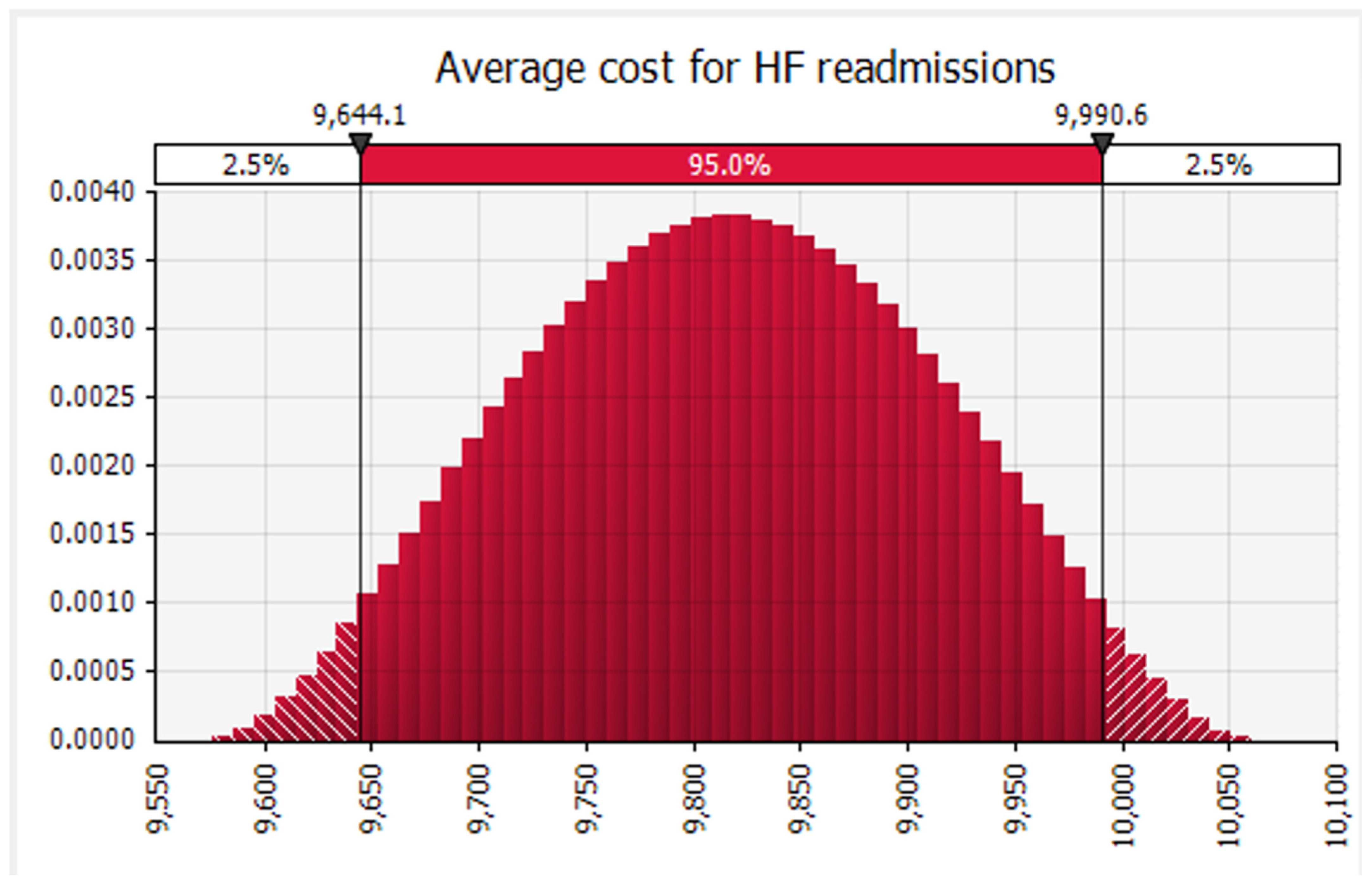
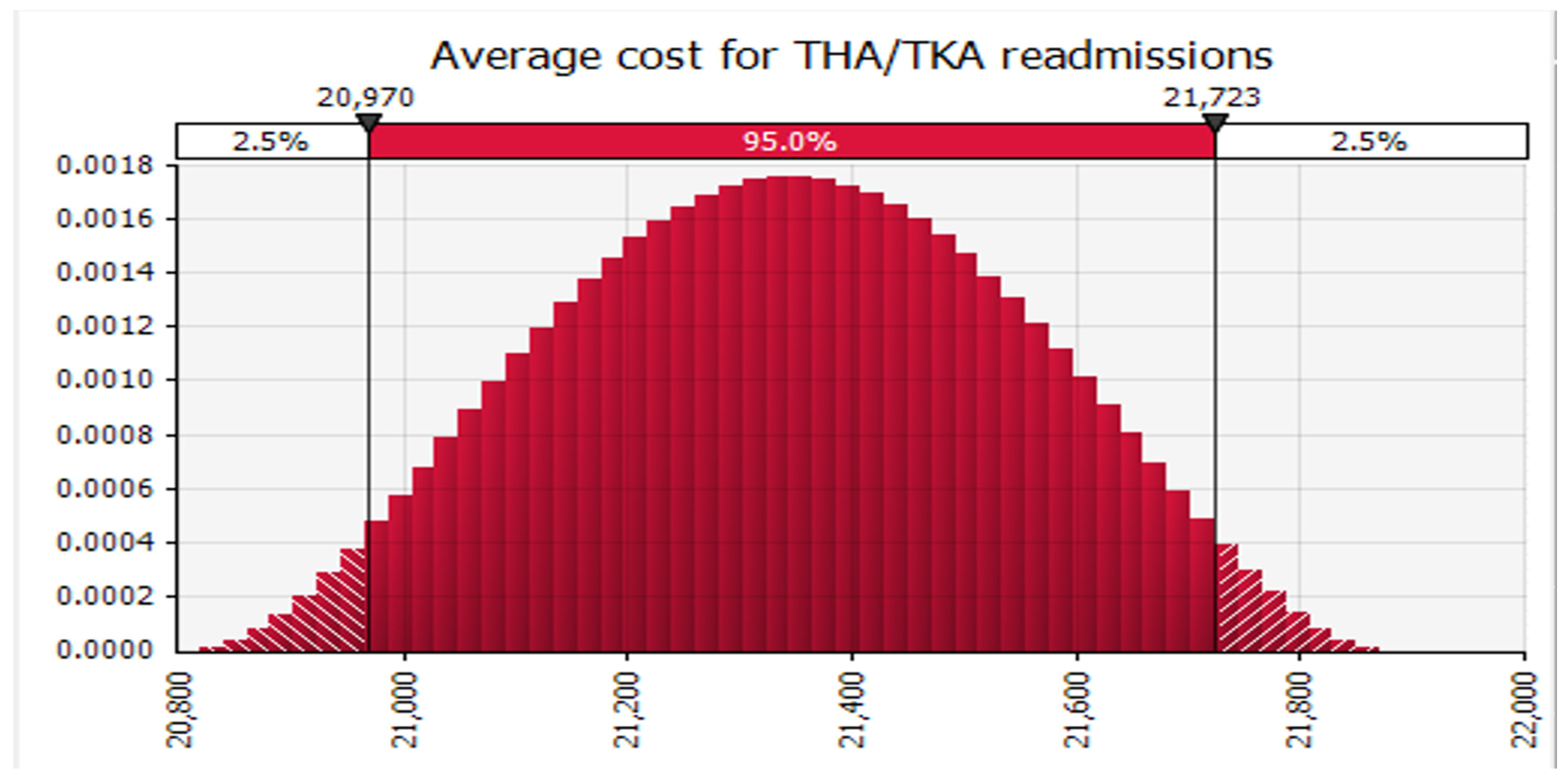
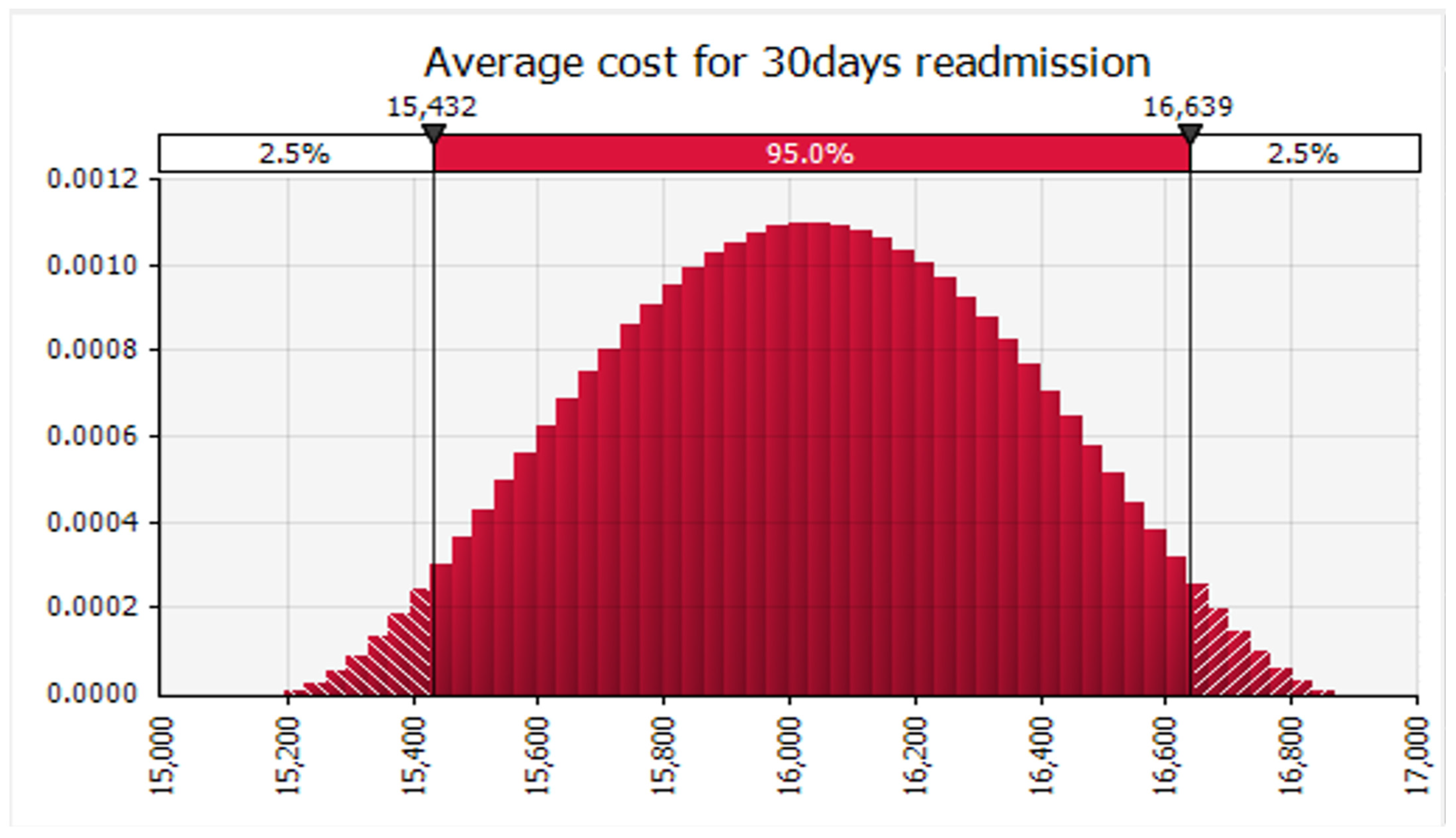
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Article | Author | Study Period/Sample/Design/Location | Independent Variables (IVs) | Dependent Variables | Data Source | Results |
|---|---|---|---|---|---|---|
| Costs associated with unplanned readmissions among patients with heart failure with and without hyponatremia | [35] | 2014–2016/national sample of over 1000 hospitals/retrospective cohort | 30-day readmission rate | Incremental cost | Premier healthcare, HCUP | Readmission cost when using HCUP was USD 547 and USD 569 for patients using premier database |
| Return-on-Investment (ROI) Analyses of an Inpatient Lay Health Worker Model on 30-Day Readmission Rates in a Rural Community Hospital | [36] | 2010–2015/single hospital/cross-sectional | 30-day readmission rate | Cost, return on investment | The hospital’s utilization and financial data | If the hospital was an ACO, as was the case for this study’s community hospital, the ROI significantly increased to USD 38.48 for every USD 1 spent on the BTH program |
| Measuring the Hospital Length of Stay/Readmission Cost Trade-Off Under a Bundled Payment Mechanism | [37] | 1/2/08 and 31/12/08/acute care hospitals in New York/longitudinal | 30-day readmission rate | Marginal cost | State inpatient databases (SID) and HCUP, AHA | The mean MC cost was USD 1857, and the mean MECR is USD 316; the mean difference between MC and MECR is USD 1541 |
| The cost of hospital readmissions: evidence from the VA | [38] | 2011/National/619,479 patients/cross-sectional | 30-day readmission rate | Direct patient cost: fixed and variable | VA administrative sources | The variable cost among sub-groups was lower for readmission rates, ranging from USD 6077 for pneumonia to USD 8345 for heart attack |
| Sex-based differences in outcomes, 30-day readmissions, and costs following catheter ablation of atrial fibrillation: the United States Nationwide Readmissions Database 2010–14 | [39] | 2010–2014/National/54,597 admissions/retrospective cohort | 30-day readmission rate | Cost | United States Agency for Healthcare Research and Quality (AHRQ) NRD | Among patients readmitted within 30 days, the median costs of readmission trended higher for females compared to males [USD 5774 (IQR USD 3286–10,661) vs. USD 5519 (IQR USD 3263–10,071); p = 0.076] |
| Outcomes, Costs, and 30-Day Readmissions After Catheter Ablation of Myocardial Infarct–Associated Ventricular Tachycardia in the Real World | [40] | 2010–2015/4109 admissions/retrospective cohort/national | 30-day readmission rate | Cost | HCUP state inpatient databases, the NRD | The median cost of readmission was USD 7932 (IQR, USD 4146–25,009) |
| Hospital Readmission and Costs of Total Knee Replacement Surgery in 2009 and 2014: Potential Implications for Healthcare Managers | [41] | 2009–2014/30,000 patients/national sample/retrospective cohort | 30-day readmission rate | Cost | HCUP state inpatient databases, the NRD | Costs per stay increased from USD 9929 to USD 11,904 over the four-year period, up a total of 20% |
| Risk Factors, Causes, and Costs of Hospital Readmission After Head and Neck Cancer Surgery | [42] | 2010–2014/nationwide/retrospective cohort/9487patients | 30-day readmission rate | Cost | HCUP state inpatient databases, the NRD | Mean cost per readmission was USD 15,916 standard error of the mean was USD 785; lower value was about USD 9000–USD 36,000 |
| Causes, Risk Factors, and Costs of 30-Day Readmissions After Mitral Valve Repair and Replacement | [43] | 2010–2014/national/retrospective cohort/76,342 patients | 30-day readmission rate | Cost | HCUP state inpatient databases, the NRD | The mean cost for readmission was USD 15,397; lower value for readmission was USD 10,164 for arrythmia and USD 24,739 for infection |
| Nationwide Analysis of 30-Day Readmissions After Esophagectomy: Causes, Costs, and Risk Factors | [44] | 2010–2014/national/retrospective cohort/76,342 patients | 30-day readmission rate | Cost | HCUP state inpatient databases, the NRD | Median cost of readmission was USD 9660 (interquartile range, USD 5392 to USD 20,447) |
| Contribution of 30-day readmissions to the increasing costs of care for the diabetic foot | [45] | 2012–2016/single hospital/prospective cohort/150 patients | 30-day readmission rate | Cost | Primary data collection | The median hospital cost per admission was USD 20,111 (interquartile range, USD 12,589–33,254); attributable cost was cost USD 7.9 million over 4 years, of which USD 1.2 million (16%) was attributable to readmission costs |
| The Relative Importance of Post-Acute Care and Readmissions for Post-Discharge Spending | [46] | 2007–2008/national/critical access hospitals/3217 patients/retrospective cohort | 30-day readmission rate | Cost | Medicare fee-for service data | Average spending ranging from USD 1768 for MS-DRG 379 (GI hemorrhage) to USD 12,369 for MS-DRG 480 (hip and femur procedures); the interquartile range varied from USD 1245 for MS-DRG 192 (COPD) to USD 4393 for MS-DRG 281 and USD 7874 for MS-DRG 282 (both AMI) |
| Readmission after pancreatic resection: causes, costs and cost-effectiveness analysis of high versus low quality hospitals using the Nationwide Readmission Database | [47] | 2010–2014/national/53,572 cases/retrospective cohort/ | 30-day readmission rate | Cost | HCUP national readmission databases, the NRD | The average cost of readmission was USD 15,563, the incremental adjusted cost of a major complication during the readmission was USD 38,028 ± 456 |
| The Effects of Multiple Chronic Conditions on Adult Patient Readmissions and Hospital Finances: A Management Case Study | [48] | 2010–2015/single hospital/retrospective cohort/2659 | 30-day readmission rate | Cost | Hospital data | Patients with 1 selected clinical condition present had the highest margin per admission (USD 2912); patients with 5 or more clinical conditions, on average, a total loss of USD 865 per admission |
| Relationship Between Hospital Financial Performance and Publicly Reported Outcomes | [49] | 2008–2012/statewide/retrospective cohort/279 hospitals | 30-day readmission rate | Revenue | Hospital annual financial data files from the Office of Statewide Health Planning and Development (OSHPD), CMS via the hospital comparison | Net revenue from operations from 2008 to 2012 (difference-in-differences estimates ranged from USD 8.61 to USD 6.77 million, p > 0.3 for all) |
| Costs And Clinical Factors Associated With 30- And 60-Day Hospital Readmission After Ventricular Tachycardia Ablation | [50] | 2013/nationwide/cross-sectional/529 patients | 30-day readmission rate | Cost (standard charge to cost calculations) | HCUP National Readmission Databases, the NRD | Costs for subsequent readmissions within 30- and 60 days post-ablation were USD 6973 and USD 7620 |
| Treatment outcomes, 30-day readmission and healthcare resource utilization after pancreatoduodenectomy for pancreatic malignancies | [51] | 2014/nationwide/cross-sectional/4445 patients | 30-day readmission rate | Cost, charges | HCUP National Readmission Databases, the NRD | The number of hospital days associated with readmission was 5548, with an in-hospital economic burden of USD 12.9 million (costs) and USD 43.7 million (charges) |
| Impact of Bipolar Disorder on Readmission Rates and Costs After Coronary Artery Bypass Grafting | [52] | 2010–2014/412,949/retrospective cohort/nationwide | 30-day readmission rate | Cost | National Readmission Database | Bipolar diagnosis did not significantly impact total hospital costs or length of stay of the index visit |
| Incidence, Cost, and Risk Factors for Readmission After Coronary Artery Bypass Grafting | [53] | 2013–2014/288,059/retrospective cohort/national | 30-day readmission rate | Cost | 2013 and 2014 Nationwide Readmissions Database (NRD) | Readmitted patients had a significantly cost (USD 49,528 USD 544.40 versus USD 41,014 USD 406.10) (all p < 0.001) compared with no readmissions |
| Inpatient costs, mortality and 30-day readmission in patients with central-line-associated bloodstream infections | [54] | 2008–2010/398/single-hospital/prospective study | 30-day readmission rate | Total cost and variable cost | Survey data | CLABSI was associated with c. USD 49,600 in excess total costs and USD 32,400 in excess variable costs |
| Readmission Rates and Their Impact on Hospital Financial Performance: A Study of Washington Hospitals | [25] | 2012–2014/98 hospitals/retrospective cohort/statewide | 30-day readmission rate | Operating revenues, operating expenses, operating margin | CMS hospital comparisons | The average operating revenues per patient is higher in 2014 than in 2013 by USD 9602 and in 2012 by USD 10,511; similarly, the mean operating expenses per patient is higher in 2014 than in 2013 by USD 9508 and in 2012 by USD 9436; the average operating margin in 2014 is higher by 2.56 percent points in 2013 and by 3.95 percentage points in 2012 |
| Predictors and Costs of 30-Day Readmissions After Index Hospitalizations for Alcohol-Related Disorders in US Adults | [32] | 2014/285,767 hospitalizations/cross-sectional/nationwide | 30-day readmission rate | Cost | NRD | Index hospitalization costs were higher among readmitted patients (USD 8840 vs. USD 8036, p < 0.01) |
| Predictors of Cost and Incidence of 30-Day Readmissions Following Hospitalizations for Schizophrenia and Psychotic Disorders | [55] | 2014/77,625 discharges/cross-sectional/nation-wide | 30-day readmission rate | Cost | Nation-wide readmission database | The average index and readmission costs were USD 9285 and USD 8593, respectively |
| Does a reduction in readmissions result in net savings for most hospitals? an examination of Medicare’s Hospital Readmissions Reduction Program | [4] | 2016/2465 hospitals/cross-sectional/Nation-wide | 30-day readmission rate | Reimbursement gains | Hospital comparison dataset | For an average hospital, avoiding one excess readmission would result in reimbursement gains of USD 10,000–USD 58,000 for Medicare discharges |
| One-year costs of medical admissions with and without a 30-day readmission and enhanced risk adjustment | [56] | 2000–2011/retrospective cohort/national/4684 hospitalizations | 30-day readmission rate | One-year subsequent Medicare spending (USD) | MCBS cost and use files | The unadjusted subsequent one-year Medicare spending among those readmitted (USD 56,856) was 60% higher than that among the non-readmitted (USD 35,465) |
| Hospital readmission with Clostridium difficile infection as a secondary diagnosis is associated with worsened outcomes and greater revenue loss relative to principal diagnosis: a retrospective cohort study | [57] | 2009–2013/retrospective cohort/4 states/5468 hospitalizations | 30-day readmission rate | Cost | State Inpatient Databases (SID), a part of the Health Care Utilization Project (HCUP) | Adjusted 30-day readmission cost and risk was lower in PrCDI (OR = 0.84; 95% CI 0.80, 0.88) and SrCDI (OR = 0.97; 95% CI 0.94, 1.01) than non-CDI |
| Comparison of Causes and Associated Costs of 30-Day Readmission of Transcatheter Implantation Versus Surgical Aortic Valve Replacement in the United States (A National Readmission Database Study) | [58] | 2013/retrospective cohort/national/5468 hospitalizations | 30-day readmission rate | Cost | NAD, HCUP | The 30-day cumulative costs were higher for the 2 endovascular TAVI (USD 51,025 vs. USD 46,228; p = 0.03) and transapical TAVI (USD 59,575 vs. USD 45,792; p < 0.01) |
| The cost of preventing readmissions: why surgeons should lead the effort. | [59] | 2012/single-hospital/cross-sectional/576 | 30-day readmission rate | Cost | United University Health Consortium | Calculated net profit for readmission was USD 144 |
| Effects of an Acute Care for Elders Unit on Costs and 30-Day Readmissions | [60] | 2010/single-hospital/cross-sectional | CMI | Cost | UAB hospital administrative database, | Adjusted cost ratios revealed significant cost savings for patients with low (0.82; 95% CI, 0.72–0.94) or moderate (0.74; 95% CI, 0.62–0.89) CMI scores; care was cost neutral for patients with high CMI scores (1.13; 95% CI, 0.93–1.37) |
| How Much Does a Readmission Cost the Bundle Following Primary Hip and Knee Arthroplasty? | [30] | Retrospective cohort | 30-day readmission rate | Cost | CMS claims | Readmitted patients had an average 90-day episode-of-care cost of USD 42,923 compared to USD 18,514 for no readmitted patients (p < 0.001; Table A1);patients who were readmitted generated significantly higher subacute care costs (USD 5201 vs. USD 3707, p < 0.001), home health aide costs (USD 1796 vs. USD 808, p < 0.001), and overall post-acute care costs (USD 28,064 vs. USD 4021, (p < 0.001) |
| Incidence, Cost, and Risk Factors for Readmission After Coronary Artery Bypass Grafting | [53] | Retrospective cohort | 30-day readmission rate | Cost | HCUP | Readmitted patients had a significantly higher cost (USD 49,528 USD 544.40 versus USD 41,014 USD 406.10) (p < 0.00) |
| Length of Stay and Cost of Pediatric Readmissions | [61] | Retrospective cohort | 30-day readmission rate | Cost | administrative database that contains information on | Readmission cost USD 6328 (95% CI: USD 6184–6475), respectively |
| Institutional Cost of Unplanned 30-Day Readmission Following Open and Endovascular Surgery | [62] | Retrospective cohort | 30-day readmission rate | Cost | The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) | The mean costs for 30-day unplanned readmission for open and endovascular procedures were USD 19,117 and USD 17,887, respectively (p = 0.635) |
| Frequency, Cost and Risk Factors of Readmissions among Severe Sepsis Survivors | [63] | Observational cohort | 30-day readmission rate | Cost | HCUP | The mean cost of each readmission was USD 25,505 (standard deviation USD 38,765) |
| The Readmission Event after Vascular Surgery: Causes and Costs | [64] | Retrospective cohort | 30-day readmission rate | Cost | Hospital data | The median hospital cost for readmission for wound complications was 29,723 USD (interquartile range 23,841–36,878), and for cardiac complications was 39,784 USD (26,305–46,918); the median cost of readmission for bypass graft occlusion was 33,366 USD (20,530–43,170) |
| Costs and Risk Factors for Hospital Readmission After Periprosthetic Knee Fractures in the United States | [65] | Retrospective cohort | 30-day readmission rate | Cost | HCUP | ORIF cost USD 25,539 and revision THA cost USD 37,680, with associated readmissions costing 15,269 and 16,806, respectively |
| Proportion and Cost of Unplanned 30-Day Readmissions After Sepsis Compared with Other Medical Conditions | [66] | Retrospective cohort | 30-day readmission rate | Index admissions, length of stay | CMS cost reports | The estimated mean cost per readmission was highest for sepsis compared with the other diagnoses (USD 10,070 [95% CI, USD 10,021–10,119] for sepsis, USD 8417 [95% CI, USD 8355–8480] for COPD, USD 9051 [95% CI, USD 8990–9113] for heart failure, USD 9424 [95% CI, USD 9279–9571] for AMI, and USD 9533 [95% CI, USD 9466–9600] for pneumonia; p < 0.005 for all pairwise comparisons) |
| Predictors and Cost of Readmission in Total Knee Arthroplasty | [31] | Retrospective cohort | 30-day readmission rate | Cost | HCUP | The overall median cost for each readmission was USD 6753 ± 175 |
References
- Fonarow, G.C. Unintended Harm Associated with the Hospital Readmissions Reduction Program. JAMA 2018, 320, 2539–2541. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Koenig, L.; Faerberg, J.; Steinberg, C.R.; Vaz, C.; Wheatley, M.P. The medicare hospital readmissions reduction program: Potential unintended consequences for hospitals serving vulnerable populations. Health Serv. Res. 2014, 49, 818–837. [Google Scholar] [CrossRef] [PubMed]
- Jweinat, J.J. Hospital Readmissions Under the Spotlight. J. Healthc. Manag. 2010, 55, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Yakusheva, O.; Hoffman, G.J. Does a reduction in readmissions result in net savings for most hospitals? an examination of Medicare’s Hospital Readmissions Reduction Program. Med. Care Res. Rev. 2020, 77, 334–344. [Google Scholar] [CrossRef]
- Hoffman, J.; Cronin, M. The true financial impact of hospital readmissions. Healthc. Financ. Manag. 2015, 69, 68–75. [Google Scholar]
- Hoyer, E.H.; Padula, W.V.; Brotman, D.J.; Reid, N.; Leung, C.; Lepley, D.; Deutschendorf, A. Patterns of Hospital Performance on the Hospital-Wide 30-Day Readmission Metric: Is the Playing Field Level? J. Gen. Intern. Med. 2018, 33, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Basch, E.; Rogak, L.J.; Dueck, A.C. Methods for Implementing and Reporting Patient-reported Outcome (PRO) Measures of Symptomatic Adverse Events in Cancer Clinical Trials. Clin. Ther. 2016, 38, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The methods and findings of quality assessment and monitoring: An illustrated analysis. J. Healthc. Qual. 1985, 7, 15. Available online: https://journals.lww.com/jhqonline/Citation/1985/07000/THE_METHODS_AND_FINDINGS_OF_QUALITY_ASSESSMENT_AND.11.aspx (accessed on 20 April 2021). [CrossRef]
- Brook, R.H.; Davies-Avery, A.; Greenfield, S.; Harris, L.J.; Lelah, T.; Solomon, N.E.; Ware, J.E. Assessing the Quality of Medical Care Using Outcome Measures: An Overview of the Method; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1977; Available online: https://www.jstor.org/stable/3763313?casa_token=vTBkCJT-2zsAAAAA:34nu7BiBI5DZYT0wNQb5yQhLO-b6bIiCo3XPxvQ0tO6RXDhCMDpU5DcRfUcGHCihJahEb0JBywFHGHJjFAXjVvr4eWMpJqfqw2gAbT4k7POrRk-JGjc (accessed on 20 April 2021).
- Donabedian, A. Evaluating the quality of medical care. Milbank Mem. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef]
- Donabedian, A. Exploratings in Quality Assessment and Monitoring Definition of Quality and Approaches to Its Assessment; Health Administration Press: Ann Arbor, MI, USA, 1980; Available online: https://ci.nii.ac.jp/naid/10010151458/ (accessed on 20 April 2021).
- Nuckols, T.K.; Escarce, J.J.; Asch, S.M. The Effects of Quality of Care on Costs: A Conceptual Framework. Milbank Q. 2013, 91, 316–353. [Google Scholar] [CrossRef]
- Brook, R.H.; Lohr, K.N. Efficacy, Effectiveness, Variations, and Quality: Boundary-Crossing Research; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1985; Available online: https://www.jstor.org/stable/3765001?casa_token=_VzVplcW8bYAAAAA:b6-PGUH5xwDZUyUPW8I6pbMYihCVRVIAOZ32Nr-LmKVoLVVaOyj6AxbfCeoGMu0t_HfniFl6s5rEmJPD-R7nb2stpGLKGoI3qyW6qrlhcIDW90bLzQ0 (accessed on 20 April 2021).
- Donabedian, A. Criteria and standards for quality assessment and monitoring. Qual. Rev. Bull. 1986, 12, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Ayanian, J.Z.; Markel, H. Donabedian’s Lasting Framework for Health Care Quality. N. Engl. J. Med. 2016, 375, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.; Lavoie, A.; Bourgeois, G.; Lapointe, J. Donabedian’s structure-process-outcome quality of care model. J. Trauma Acute Care Surg. 2015, 78, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Joynt, K.E.; Figueroa, J.F.; Orav, E.J.; Jha, A.K. Opinions on the HRRP: Results of a national survey of hospital leaders. Am. J. Manag. Care 2016, 22, e287–e294. Available online: https://www.ajmc.com/printer?url=/journals/issue/ (accessed on 20 April 2021). [PubMed]
- Beauvais, B.; Wells, R. Does money really matter? A review of the literature on the relationships between healthcare organization finances and quality. Hosp. Top. 2006, 84, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.; Oner, N.; Ray, M.N.; Zengul, F.D. Exploring the association between quality and financial performance in US hospitals: A systematic review. J. Health Care Financ. 2018, 44, 1–20. [Google Scholar]
- Jha, A.K.; Chan, D.C.; Ridgway, A.B.; Franz, C.; Bates, D.W. MarketWatch—Improving safety and eliminating redundant tests: Cutting costs in U.S. hospitals. Health Aff. 2009, 28, 1475–1484. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.; Yamin, C.K.; Keohane, C.; Denham, C.R.; Bates, D.W. Health care-associated infections: A Meta-analysis of costs and financial impact on the US health care system. JAMA Intern. Med. 2013, 173, 2039–2046. [Google Scholar] [CrossRef]
- Jha, A.K.; Desroches, C.M.; Campbell, E.G.; Donelan, K.; Rao, S.R.; Ferris, T.G.; Shields, A.; Rosenbaum, S.; Blumenthal, D. Use of electronic health records in U.S. Hospitals. N. Engl. J. Med. 2009, 360, 1628–1638. [Google Scholar] [CrossRef]
- Jang, S.J.; Yeo, I.; Feldman, D.N.; Cheung, J.W.; Minutello, R.M.; Singh, H.S.; Bergman, G.; Wong, S.C.; Kim, L.K. Associations Between Hospital Length of Stay, 30-Day Readmission, and Costs in ST-Segment-Elevation Myocardial Infarction After Primary Percutaneous Coronary Intervention: A Nationwide Readmissions Database Analysis. J. Am. Heart Assoc. 2020, 9, e015503. [Google Scholar] [CrossRef]
- Horwitz, L.; Chohreh Partovian, M.; Lin, Z.; Herrin, J.; Grady, J.; Mitchell Conover, M.; Julia Montague, B.; Chloe Dillaway, M.; Kathleen Bartczak, B.; Joseph Ross, B.; et al. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure DRAFT Measure Methodology Report Submitted by Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). 2011. Available online: https://sites.dartmouth.edu/dac/files/2018/08/mmshospital-wideall-conditionreadmissionrate-z6qxhh.pdf (accessed on 20 April 2021).
- Upadhyay, S.; Stephenson, A.L.; Smith, D.G. Readmission Rates and Their Impact on Hospital Financial Performance: A Study of Washington Hospitals. Inq. J. Health Care Organ. Provis. Financ. 2019, 56, 004695801986038. [Google Scholar] [CrossRef]
- Al Ahmad, Y.; Ali, M.T. Non-ST Elevation Myocardial Infarction: Diagnosis and Management. In Myocardial Infarction; IntechOpen: London, UK, 2019. [Google Scholar]
- Sood, N.; Weissblum, L.; Karaca-Mandic, P.; Huckfeldt, P.; Escarce, J. Skilled Nursing Facility Participation in Medicare’s Bundled Payments for Care Improvement Initiative: A Retrospective Study. Arch. Phys. Med. Rehabil. 2018, 100, 307–314. [Google Scholar] [CrossRef]
- Wang, Y.; Ghislandi, S.; Torbica, A. Investigating the geographic disparity in quality of care: The case of hospital readmission after acute myocardial infarction in Italy. Eur. J. Health Econ. 2020, 21, 1149–1168. [Google Scholar] [CrossRef]
- Fetterolf, D. Hispanics and Health Care in the United States: Access, Information and Knowledge; Pew Research Center: Washington, DC, USA, 2008; pp. 1–81. [Google Scholar]
- Fillingham, Y.A.; Austin, M.S.; Vannello, C.; Phillips, J.L.H.; Rondon, A.J.; Courtney, P.M. How Much Does a Readmission Cost the Bundle Following Primary Hip and Knee Arthroplasty? J. Arthroplasty 2019, 34, 819–823. [Google Scholar] [CrossRef]
- Urish, K.L.; Qin, Y.; Li, B.Y.; Borza, T.; Sessine, M.; Kirk, P.; Hollenbeck, B.K.; Helm, J.E.; Lavieri, M.S.; Skolarus, T.A.; et al. Predictors and Cost of Readmission in Total Knee Arthroplasty. J. Arthroplasty 2018, 33, 2759–2763. [Google Scholar] [CrossRef] [PubMed]
- Wani, R.J.; Tak, H.J.; Watanabe-Galloway, S.; Klepser, D.G.; Wehbi, N.K.; Chen, L.W.; Wilson, F.A. Predictors and Costs of 30-Day Readmissions after Index Hospitalizations for Alcohol-Related Disorders in US Adults. Alcohol. Exp. Res. 2019, 43, 857–868. [Google Scholar] [CrossRef]
- Ramaswamy, A.; Marchese, M.; Cole, A.P.; Harmouch, S.; Friedlander, D.; Weissman, J.S.; Lipsitz, S.R.; Haider, A.H.; Kibel, A.S.; Schoenfeld, A.J.; et al. Comparison of hospital readmission after total hip and total knee arthroplasty vs spinal surgery after implementation of the hospital Readmissions Reduction Program. JAMA Netw. Open 2019, 2, 194634. [Google Scholar] [CrossRef]
- Mcilvennan, C.K.; Eapen, Z.J.; Allen, L.A. Hospital Readmissions Reduction Program. Circulation 2015, 131, 1796–1803. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.N.; Ortendahl, J.D.; Harmon, A.L.; Kamat, S.A.; Stellhorn, R.A.; Chase, S.L.; Sundar, S.V. Costs associated with unplanned readmissions among patients with heart failure with and without hyponatremia. Am. J. Health Pharm. 2019, 76, 374–380. [Google Scholar] [CrossRef]
- Cardarelli, R.; Bausch, G.; Murdock, J.; Chyatte, M.R. Return-on-Investment (ROI) Analyses of an Inpatient Lay Health Worker Model on 30-Day Readmission Rates in a Rural Community Hospital. J. Rural Health 2018, 34, 411–422. [Google Scholar] [CrossRef]
- Carey, K. Measuring the Hospital Length of Stay/Readmission Cost Trade-Off Under a Bundled Payment Mechanism. Health Econ. 2015, 24, 790. [Google Scholar] [CrossRef]
- Carey, K.; Stefos, T. The cost of hospital readmissions: Evidence from the VA. Health Care Manag. Sci. 2016, 19, 241–248. [Google Scholar] [CrossRef]
- Cheung, J.W.; Cheng, E.P.; Wu, X.; Yeo, I.; Christos, P.J.; Kamel, H.; Markowitz, S.M.; Liu, C.F.; Thomas, G.; Ip, J.E.; et al. Sex-based differences in outcomes, 30-day readmissions, and costs following catheter ablation of atrial fibrillation: The United States Nationwide Readmissions Database 2010–2014. Eur. Heart J. 2019, 40, 3035–3043. [Google Scholar] [CrossRef]
- Cheung, J.W.; Yeo, I.; Ip, J.E.; Thomas, G.; Liu, C.F.; Markowitz, S.M.; Lerman, B.B.; Kim, L.K. Outcomes, Costs, and 30-Day Readmissions after Catheter Ablation of Myocardial Infarct-Associated Ventricular Tachycardia in the Real World. Circ. Electrophysiol. 2018, 11, e006754. [Google Scholar] [CrossRef]
- Cary, M.P.; Goode, V.; Crego, N.; Thornlow, D.; Colon-Emeric, C.; van Houtven, C.; Merwin, E.I. Hospital Readmission and Costs of Total Knee Replacement Surgery in 2009 and 2014 Potential Implications for Health Care Managers. Health Care Manag. 2019, 38, 24–28. [Google Scholar] [CrossRef]
- Goel, A.N.; Raghavan, G.; St John, M.A.; Long, J.L. Risk Factors, Causes, and Costs of Hospital Readmission after Head and Neck Cancer Surgery Reconstruction. JAMA Facial Plast. Surg. 2019, 21, 137–145. [Google Scholar] [CrossRef]
- Goel, N.J.; Iyengar, A.; Kelly, J.J.; Brown, C.R.; Kurshan, F.; Atluri, P.; Acker, M.A.; Chen, Z.H.; Desai, N.D. Causes, Risk Factors, and Costs of 30-Day Readmissions after Mitral Valve Repair and Replacement. Ann. Thorac. Surg. 2019, 108, 1729–1737. [Google Scholar] [CrossRef]
- Goel, N.J.; Iyengar, A.; Kelly, J.J.; Mavroudis, C.; Lancaster, C.; Williams, N.N.; Dempsey, D.T.; Kucharczuk, J. Nationwide Analysis of 30-Day Readmissions after Esophagectomy: Causes, Costs, and Risk Factors. Ann. Thorac. Surg. 2020, 109, 185–193. [Google Scholar] [CrossRef]
- Hicks, C.W.; Canner, J.K.; Karagozlu, H.; Mathioudakis, N.; Sherman, R.L.; Black, J.H., III; Abularrage, C.J. Contribution of 30-day readmissions to the increasing costs of care for the diabetic foot. J. Vasc. Surg. 2019, 70, 1263–1270. [Google Scholar] [CrossRef]
- Huckfeldt, P.J.; Mehrotra, A.; Hussey, P.S. The Relative Importance of Post-Acute Care and Readmissions for Post-Discharge Spending. Health Serv. Res. 2016, 51, 1919–1938. [Google Scholar] [CrossRef]
- Idrees, J.J.; Rosinski, B.F.; Merath, K.; Chen, Q.; Bagante, F.; Pawlik, T.M. Readmission after pancreatic resection: Causes, costs and cost-effectiveness analysis of high versus low quality hospitals using the Nationwide Readmission Database. HPB 2019, 21, 291–300. [Google Scholar] [CrossRef]
- Mihailoff, M.; Deb, S.; Lee, J.A.; Lynn, J. The Effects of Multiple Chronic Conditions on Adult Patient Readmissions and Hospital Finances: A Management Case Study. Inquiry 2017, 54, 0046958017729597. [Google Scholar] [CrossRef]
- Nguyen, O.K.; Halm, E.A.; Makam, A.N. Relationship between hospital financial performance and publicly reported outcomes. J. Hosp. Med. 2016, 11, 481–488. [Google Scholar] [CrossRef]
- Nosova, K.; Sutton, B. Costs and clinical factors associated with 30- and 60-day hospital readmission after ventricular tachycardia ablation. J. Am. Coll. Cardiol. 2018, 71, A438. [Google Scholar] [CrossRef]
- Peluso, H.; Jones, W.B.; Parikh, A.A.; Abougergi, M.S. Treatment outcomes, 30-day readmission and healthcare resource utilization after pancreatoduodenectomy for pancreatic malignancies. J. Hepatobiliary Pancreat. Sci. 2019, 26, 187–194. [Google Scholar] [CrossRef]
- Sanaiha, Y.; Juo, Y.-Y.; Seo, Y.-J.; Benharash, P.; Ebrahimi, R. Impact of Bipolar Disorder on Readmission Rates and Costs After Coronary Artery Bypass Grafting. J. Am. Coll. Cardiol. 2018, 71, A189. [Google Scholar] [CrossRef]
- Shah, R.M.; Zhang, Q.; Chatterjee, S.; Cheema, F.; Loor, G.; Lemaire, S.A.; Wall, M.J.; Coselli, J.S.; Rosengart, T.K.; Ghanta, R.K. Incidence, Cost, and Risk Factors for Readmission after Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2019, 107, 1782–1789. [Google Scholar] [CrossRef]
- Stevens, V.; Geiger, K.; Concannon, C.; Nelson, R.E.; Brown, J.; Dumyati, G. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin. Microbiol. Infect. 2014, 20, O318–O324. [Google Scholar] [CrossRef]
- Wani, R.J.P.M.S.; Kathe, N.J.P.M.S.; Kathe, D.G.P.M.B.A. Predictors of Cost and Incidence of 30-Day Readmissions following Hospitalizations for Schizophrenia and Psychotic Disorders. Qual. Manag. Health Care 2019, 28, 130. [Google Scholar] [CrossRef]
- Zheng, S.; Hanchate, A.; Shwartz, M. One-year costs of medical admissions with and without a 30-day readmission and enhanced risk adjustment. BMC Health Serv. Res. 2019, 19, 155. [Google Scholar] [CrossRef]
- Zilberberg, M.D.; Nathanson, B.H.; Marcella, S.; Hawkshead, J.J., III; Shorr, A.F. Hospital readmission with Clostridium difficile infection as a secondary diagnosis is associated with worsened outcomes and greater revenue loss relative to principal diagnosis: A retrospective cohort study. Medicine 2018, 97, e12212. [Google Scholar] [CrossRef]
- Tripathi, A.; Flaherty, M.P.; Abbott, J.D.; Fonarow, G.C.; Khan, A.R.; Saraswat, A.; Chahil, H.; Kolte, D.; Elmariah, S.; Hirsch, G.A.; et al. Comparison of Causes and Associated Costs of 30-Day Readmission of Transcatheter Implantation Versus Surgical Aortic Valve Replacement in the United States (A National Readmission Database Study). Am. J. Cardiol. 2018, 122, 431–439. [Google Scholar] [CrossRef]
- Postel, M.; Frank, P.N.; Barry, T.; Satou, N.; Shemin, R.; Benharash, P. The cost of preventing readmissions: Why surgeons should lead the effort. Am. Surg. 2014, 80, 1003–1006. [Google Scholar] [CrossRef]
- Flood, K.L.; MacLennan, P.A.; McGrew, D.; Green, D.; Dodd, C.; Brown, C.J. Effects of an acute care for elders unit on costs and 30-day readmissions. JAMA Intern. Med. 2013, 173, 981–987. [Google Scholar] [CrossRef]
- Markham, J.L.; Hall, M.; Gay, J.C.; Bettenhausen, J.L.; Berry, J.G. Length of stay and cost of pediatric readmissions. Pediatrics 2018, 141, e20172934. [Google Scholar] [CrossRef]
- Gracon, A.S.A.; Liang, T.W.; Easterday, T.S.; Weber, D.J.; Butler, J.; Slaven, J.E.; Lemmon, G.W.; Motaganahalli, R.L. Institutional Cost of Unplanned 30-Day Readmission following Open and Endovascular Surgery. Vasc. Endovasc. Surg. 2016, 50, 398–404. [Google Scholar] [CrossRef]
- Goodwin, A.J.; Rice, D.A.; Simpson, K.N.; Ford, D.W. Frequency, cost, and risk factors of readmissions among severe sepsis survivors. Crit. Care Med. 2015, 43, 738–746. [Google Scholar] [CrossRef]
- Duwayri, Y.; Goss, J.; Knechtle, W.; Veeraswamy, R.K.; Arya, S.; Rajani, R.R.; Brewster, L.P.; Dodson, T.F.; Sweeney, J.F. The Readmission Event after Vascular Surgery: Causes and Costs. Ann. Vasc. Surg. 2016, 36, 7–12. [Google Scholar] [CrossRef]
- Reeves, R.A.; Schairer, W.W.; Jevsevar, D.S. Costs and Risk Factors for Hospital Readmission after Periprosthetic Knee Fractures in the United States. J. Arthroplast. 2018, 33, 324–330.e1. [Google Scholar] [CrossRef]
- Mayr, F.B.; Talisa, V.B.; Balakumar, V.; Chang, C.C.H.; Fine, M.; Yende, S. Proportion and cost of unplanned 30-day readmissions after sepsis compared with other medical conditions. JAMA 2017, 317, 530–531. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kum Ghabowen, I.; Epane, J.P.; Shen, J.J.; Goodman, X.; Ramamonjiarivelo, Z.; Zengul, F.D. Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance. Healthcare 2024, 12, 750. https://doi.org/10.3390/healthcare12070750
Kum Ghabowen I, Epane JP, Shen JJ, Goodman X, Ramamonjiarivelo Z, Zengul FD. Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance. Healthcare. 2024; 12(7):750. https://doi.org/10.3390/healthcare12070750
Chicago/Turabian StyleKum Ghabowen, Iwimbong, Josue Patien Epane, Jay J. Shen, Xan Goodman, Zo Ramamonjiarivelo, and Ferhat Devrim Zengul. 2024. "Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance" Healthcare 12, no. 7: 750. https://doi.org/10.3390/healthcare12070750
APA StyleKum Ghabowen, I., Epane, J. P., Shen, J. J., Goodman, X., Ramamonjiarivelo, Z., & Zengul, F. D. (2024). Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance. Healthcare, 12(7), 750. https://doi.org/10.3390/healthcare12070750






