Factors Facilitating and Inhibiting the Implementation of Telerehabilitation—A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategy
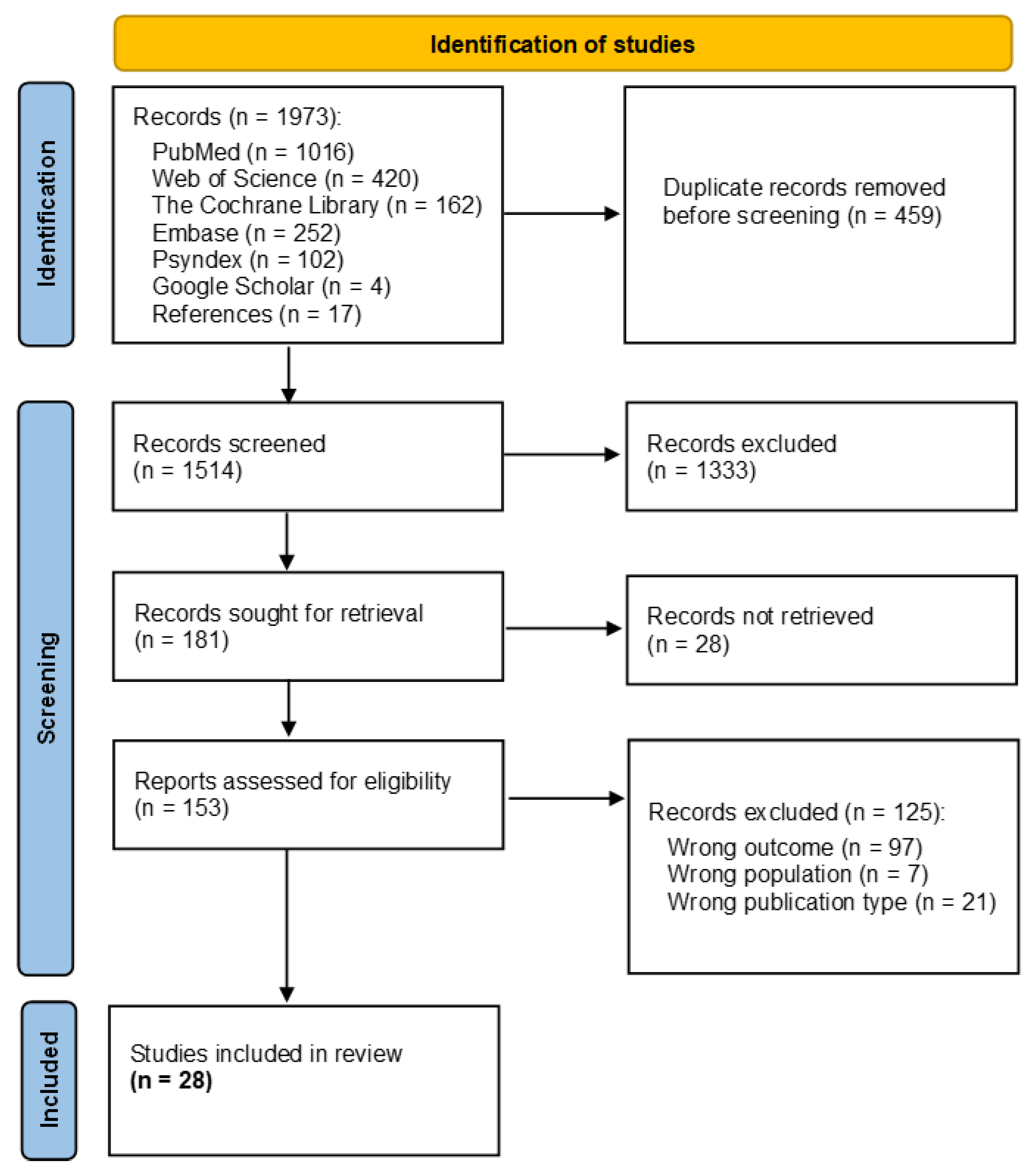
2.3. Study Selection
2.4. Analysing the Data
3. Results
3.1. Study Characeristics
3.2. TR Technologies
3.3. Population and Indication Groups
3.4. Status of Implementation
3.5. Implementation Frameworks
3.6. Barriers and Facilitators for Implementation of TR
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valle, C.; Schmitt-Sody, M. Digitalization in rehabilitation. Orthopadie 2023, 52, 869–875. [Google Scholar]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy during the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys. Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Bayly, J.; Bradshaw, A.; Fettes, L.; Omarjee, M.; Talbot-Rice, H.; Walshe, C.; Sleeman, K.E.; Bajwah, S.; Dunleavy, L.; Hocaoglu, M.; et al. Understanding the impact of the COVID-19 pandemic on delivery of rehabilitation in specialist palliative care services: An analysis of the CovPall-Rehab survey data. Palliat. Med. 2022, 36, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Meyding-Lamadé, U.; Bassa, B.; Tibitanzl, P.; Davtyan, A.; Lamadé, E.K.; Craemer, E.M. Telerehabilitation: Von der virtuellen Welt zur Realität—Medizin im 21. Jahrhundert: Videogestützte Therapie in Zeiten von COVID-19. Der Nervenarzt 2021, 92, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Fiani, B.; Siddiqi, I.; Lee, S.C.; Dhillon, L. Telerehabilitation: Development, Application, and Need for Increased Usage in the COVID-19 Era for Patients with Spinal Pathology. Cureus 2020, 12, e10563. [Google Scholar] [CrossRef] [PubMed]
- John, M. Telemedizinische Assistenzsysteme in der Rehabilitation und Nachsorge—Projekte, Technologien und Funktionen. B&G 2017, 33, 197–207. [Google Scholar]
- Brennan, D.; Tindall, L.; Theodoros, D.; Brown, J.; Campbell, M.; Christiana, D.; Smith, D.; Cason, J.; Lee, A. A Blueprint for Telerehabilitation Guidelines. Int. J. Telerehabil. 2010, 2, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Latifi, R. (Ed.) Telerehabilitation: Current Perspectives; IOS: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef] [PubMed]
- Cox, N.S.; Dal Corso, S.; Hansen, H.; McDonald, C.F.; Hill, C.J.; Zanaboni, P.; Alison, J.A.; O’Halloran, P.; Macdonald, H.; Holland, A.E. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst. Rev. 2021, 1, CD013040. [Google Scholar] [CrossRef]
- Velayati, F.; Ayatollahi, H.; Hemmat, M. A Systematic Review of the Effectiveness of Telerehabilitation Interventions for Therapeutic Purposes in the Elderly. Methods Inf. Med. 2020, 59, 104–109. [Google Scholar] [CrossRef]
- Carlbring, P.; Andersson, G.; Cuijpers, P.; Riper, H.; Hedman-Lagerlöf, E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018, 47, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Bican, R.; Christensen, C.; Fallieras, K.; Sagester, G.; O’Rourke, S.; Byars, M.; Tanner, K. Rapid Implementation of Telerehabilitation for Pediatric Patients during COVID-19. Int. J. Telerehabil. 2021, 13, e6371. [Google Scholar] [CrossRef] [PubMed]
- Pearce, L.; Costa, N.; Sherrington, C.; Hassett, L. Implementation of digital health interventions in rehabilitation: A scoping review. Clin. Rehabil. 2023, 37, 1533–1551. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Glegg, S.M.N.; Levac, D.E. Barriers, Facilitators and Interventions to Support Virtual Reality Implementation in Rehabilitation: A Scoping Review. Phys. Med. Rehabil. 2018, 10, 1237–1251.e1. [Google Scholar] [CrossRef] [PubMed]
- Nizeyimana, E.; Joseph, C.; Plastow, N.; Dawood, G.; Louw, Q.A. A scoping review of feasibility, cost, access to rehabilitation services and implementation of telerehabilitation: Implications for low- and middle-income countries. Digit. Health 2022, 8, 20552076221131670. [Google Scholar] [CrossRef] [PubMed]
- Subedi, N.; Rawstorn, J.C.; Gao, L.; Koorts, H.; Maddison, R. Implementation of Telerehabilitation Interventions for the Self-Management of Cardiovascular Disease: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e17957. [Google Scholar] [CrossRef]
- Rabanifar, N.; Abdi, K. Barriers and Challenges of Implementing Telerehabilitation: A Systematic Review. IRJ 2021, 19, 121–128. [Google Scholar] [CrossRef]
- Stampa, S.; Thienel, C.; Tokgöz, P.; Razum, O.; Dockweiler, C. OSF Registries. Protocol for a Scoping Review on Implementation Conditions of Telerehabilitation. Available online: https://osf.io/saqyu (accessed on 11 January 2024).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Von Elm, E.; Schreiber, G.; Haupt, C.C. Methodische Anleitung für Scoping Reviews (JBI-Methodologie). Z. Evid. Fortbild. Qual. Gesundheitswes. 2019, 143, 1–7. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bairapareddy, K.C.; Alaparthi, G.K.; Jitendra, R.S.; Prathiksha; Rao, P.P.; Shetty, V.; Chrasekaran, B. We are so close; yet too far: Perceived barriers to smartphone-based telerehabilitation among healthcare providers and patients with Chronic Obstructive Pulmonary Disease in India. Heliyon 2021, 7, e07857. [Google Scholar] [CrossRef]
- Rabanifar, N.; Hoseini, M.A.; Abdi, K. Exploring Barriers to Implementing Telerehabilitation from experiences of managers, policymakers, and providers of rehabilitation services in Iran: A Qualitative Study. Med. J. Islam. Repub. Iran 2022, 36, 157. [Google Scholar] [CrossRef]
- Teriö, M.; Eriksson, G.; Kamwesiga, J.T.; Guidetti, S. What’s in it for me? A process evaluation of the implementation of a mobile phone-supported intervention after stroke in Uganda. BMC Public Health 2019, 19, 562. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. The World by Income and Region. Available online: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (accessed on 17 January 2024).
- Auger, L.-P.; Moreau, E.; Côté, O.; Guerrera, R.; Rochette, A.; Kairy, D. Implementation of Telerehabilitation in an Early Supported Discharge Stroke Rehabilitation Program before and during COVID-19: An Exploration of Influencing Factors. Disabilities 2023, 3, 87–104. [Google Scholar] [CrossRef]
- Banerjee-Guenette, P.; Bigford, S.; Glegg, S.M.N. Facilitating the Implementation of Virtual Reality-Based Therapies in Pediatric Rehabilitation. Phys. Occup. Ther. Pediatr. 2020, 40, 201–216. [Google Scholar] [CrossRef]
- Caughlin, S.; Mehta, S.; Corriveau, H.; Eng, J.J.; Eskes, G.; Kairy, D.; Meltzer, J.; Sakakibara, B.M.; Teasell, R. Implementing Telerehabilitation After Stroke: Lessons Learned from Canadian Trials. Telemed. J. E-Health 2020, 26, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Farzad, M.; MacDermid, J.; Ferreira, L.; Szekeres, M.; Cuypers, S.; Shafiee, E. A description of the barriers, facilitators, and experiences of hand therapists in providing remote (tele) rehabilitation: An interpretive description approach. J. Hand Ther. 2023, 36, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Hurtubise, K.; Pratte, G.; Hamel, C.; Clapperton, I.; Camden, C. Rethinking early intervention rehabilitation services for children with motor difficulties: Engaging stakeholders in the conceptualization of telerehabilitation primary care. Disabil. Rehabil. 2022, 44, 6749–6758. [Google Scholar] [CrossRef]
- Jiancaro, T.; Bayoumi, A.M.; Ibáñez-Carrasco, F.; Torres, B.; McDuff, K.; Brown, D.A.; Chan Carusone, S.; Tang, A.; Loutfy, M.; Cobbing, S.; et al. Factors influencing initial implementation of an online community-based exercise intervention with adults living with HIV: A systems approach. Front. Rehabil. Sci. 2023, 4, 1176960. [Google Scholar] [CrossRef] [PubMed]
- Kairy, D.; Lehoux, P.; Vincent, C. Exploring routine use of telemedicine through a case study in rehabilitation. Rev. Panam. Salud Publica. 2014, 35, 337–344. [Google Scholar] [PubMed]
- Munce, S.; Andreoli, A.; Bayley, M.; Guo, M.; Inness, E.L.; Kua, A.; McIntyre, M. Clinicians’ Experiences of Implementing a Telerehabilitation Toolkit During the COVID-19 Pandemic: Qualitative Descriptive Study. JMIR Rehabil. Assist. Technol. 2023, 10, e44591. [Google Scholar] [CrossRef] [PubMed]
- Pol, M.; Qadeer, A.; van Hartingsveldt, M.; Choukou, M.-A. Perspectives of Rehabilitation Professionals on Implementing a Validated Home Telerehabilitation Intervention for Older Adults in Geriatric Rehabilitation: Multisite Focus Group Study. JMIR Rehabil. Assist. Technol. 2023, 10, e44498. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-L.; Waterson, S.; Eng, J.J. Implementation and Evaluation of the Virtual Graded Repetitive Arm Supplementary Program (GRASP) for Individuals with Stroke during the COVID-19 Pandemic and Beyond. Phys. Ther. 2021, 101, pzab083. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Hill, A.J.; O’Leary, S.P.; Raymer, M.E.; Russell, T.G. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: A qualitative study. Musculoskelet. Sci. Pract. 2017, 32, 7–16. [Google Scholar] [CrossRef]
- Cox, N.S.; Scrivener, K.; Holl, A.E.; Jolliffe, L.; Wighton, A.; Nelson, S.; McCredie, L.; Lannin, N.A. A Brief Intervention to Support Implementation of Telerehabilitation by Community Rehabilitation Services During COVID-19: A Feasibility Study. Arch. Phys. Med. Rehabil. 2021, 102, 789–795. [Google Scholar] [CrossRef]
- Lau, A.Y.; Piper, K.; Bokor, D.; Martin, P.; Lau, V.S.; Coiera, E. Challenges During Implementation of a Patient-Facing Mobile App for Surgical Rehabilitation: Feasibility Study. JMIR Hum. Factors 2017, 4, e8096. [Google Scholar] [CrossRef]
- Pitt, R.; Hill, A.J.; Theodoros, D.; Russell, T. “I definitely think it’s a feasible and worthwhile option”: Perspectives of speech-language pathologists providing online aphasia group therapy. Aphasiology 2018, 32, 1031–1053. [Google Scholar] [CrossRef]
- Ross, M.H.; Nelson, M.; Parravicini, V.; Weight, M.; Tyrrell, R.; Hartley, N.; Russell, T. Staff perspectives on the key elements to successful rapid uptake of telerehabilitation in medium-sized public hospital physiotherapy departments. Physiother. Res. Int. 2023, 28, e1991. [Google Scholar] [CrossRef]
- Ahonle, Z.J.; Kreider, C.M.; Hale-Gallardo, J.; Castaneda, G.; Findley, K.; Ottomanelli, L.; Romero, S. Implementation and use of video tele-technologies in delivery of individualized community-based vocational rehabilitation services to rural veterans. J. Vocat. Rehabil. 2021, 55, 227–233. [Google Scholar] [CrossRef]
- Duran, A.T.; Keener-DeNoia, A.; Stavrolakes, K.; Fraser, A.; Blanco, L.V.; Fleisch, E.; Pieszchata, N.; Cannone, D.; Keys McKay, C.; Whittman, E.; et al. Applying User-Centered Design and Implementation Science to the Early-Stage Development of a Telehealth-Enhanced Hybrid Cardiac Rehabilitation Program: Quality Improvement Study. JMIR Form. Res. 2023, 7, e47264. [Google Scholar] [CrossRef] [PubMed]
- Gorzelitz, J.S.; Bouji, N.; Stout, N.L. Program Barriers and Facilitators in Virtual Cancer Exercise Implementation: A Qualitative Analysis. Transl. J. Am. Coll. Sports Med. 2022, 7, e000199. [Google Scholar] [CrossRef] [PubMed]
- Hale-Gallardo, J.L.; Kreider, C.M.; Jia, H.; Castaneda, G.; Freytes, I.M.; Ripley, D.C.C.; Ahonle, Z.J.; Findley, K.; Romero, S. Telerehabilitation for rural veterans: A qualitative assessment of barriers and facilitators to implementation. J. Multidiscip. Healthc. 2020, 13, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Damhus, C.S.; Emme, C.; Hansen, H. Barriers and enablers of COPD telerehabilitation—A frontline staff perspective. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 2473–2482. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Correia, A.; Barberis, T.; Msimanga, L. Barriers to the implementation of a computer-based rehabilitation programme in two public psychiatric settings. S. Afr. J. Psychiatr. 2018, 24, 1163. [Google Scholar]
- Aloyuni, S.; Alharbi, R.; Kashoo, F.; Alqahtani, M.; Alanazi, A.; Alzhrani, M.; Ahmad, M. Knowledge, Attitude, and Barriers to Telerehabilitation-Based Physical Therapy Practice in Saudi Arabia. Healthcare 2020, 8, 460. [Google Scholar] [CrossRef]
- Brouns, B.; van Bodegom-Vos, L.; de Kloet, A.J.; Vlieland Vliet, T.P.; Gil, I.L.C.; Souza, L.M.N.; Braga, L.W.; Meesters, J.J.L. Differences in factors influencing the use of eRehabilitation after stroke; a cross-sectional comparison between Brazilian and Dutch healthcare professionals. BMC Health Serv. Res. 2020, 20, 488. [Google Scholar]
- Kraaijkamp, J.J.M.; Persoon, A.; Aurelian, S.; Bachmann, S.; Cameron, I.D.; Choukou, M.-A.; Dockery, F.; Eruslanova, K.; Gordon, A.L.; Grund, S.; et al. eHealth in Geriatric Rehabilitation: An International Survey of the Experiences and Needs of Healthcare Professionals. J. Clin. Med. 2023, 12, 4504. [Google Scholar] [CrossRef]
- Yosef, A.B.; Maeir, T.; Khalailh, F.; Gilboa, Y. Perceived feasibility of an occupation-based telerehabilitation intervention for older adults with chronic health conditions in Israel. Hong Kong J. Occup. Ther. 2022, 35, 62–70. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Reardon, C.M.; Opra Widerquist, M.A.; Lowery, J. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): The CFIR Outcomes Addendum. Implement. Sci. 2022, 17, 7. [Google Scholar] [CrossRef] [PubMed]
- Bouabida, K.; Lebouché, B.; Pomey, M.-P. Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare 2022, 10, 2293. [Google Scholar] [CrossRef] [PubMed]
- Bassa, B.; Hahner, F.; Braun, S.; Meyding-Lamadé, U. Telemedizin und internationale Projekte: Von Asien nach Afrika—Chancen der Zukunft? Der Nervenarzt 2024. ahead of print. [Google Scholar] [CrossRef] [PubMed]
| Number | Type of Search Term | Search Term |
|---|---|---|
| #1 | MeSH | telerehabilitation |
| #2 | ti,ab,kw | telerehab* |
| #3 | ti,ab,kw | tele-rehab* |
| #4 | ti,ab,kw | erehab* |
| #5 | ti,ab,kw | e-rehab* |
| #6 | ti,ab,kw | virtual* NEAR/5 rehab* |
| #7 | ti,ab,kw | remote* NEAR/5 rehab* |
| #8 | ti,ab,kw | digital* NEAR/5 rehab* |
| #9 | ti,ab,kw | online NEAR/5 rehab* |
| #10 | ti,ab,kw | mobile NEAR/5 rehab* |
| #11 | ti,ab,kw | web-based NEAR/5 rehab* |
| #12 | ti,ab,kw | computer-based NEAR/5 rehab* |
| #13 | ti,ab,kw | internet-based NEAR/5 rehab* |
| #14 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 | |
| #15 | ti,ab,kw | influenc* |
| #16 | ti,ab,kw | barrier* |
| #17 | ti,ab,kw | inhibit* |
| #18 | ti,ab,kw | imped* |
| #19 | ti,ab,kw | hinder* |
| #20 | ti,ab,kw | hindrance* |
| #21 | ti,ab,kw | facilitat* |
| #22 | ti,ab,kw | promot* |
| #23 | #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 | |
| #24 | MeSH | diffusion of innovation |
| #25 | ti,ab,kw | diffusion of innovation |
| #26 | ti,ab,kw | implement* |
| #27 | ti,ab,kw | adopt* |
| #28 | ti,ab,kw | realis* |
| #29 | ti,ab,kw | realiz* |
| #30 | #24 OR #25 OR #26 OR #27 OR #28 OR #29 | |
| #31 | (#14 AND #23 AND #30) AND (publication date between May 2012 and October 2023) | |
| CFIR Domain | Construct | Facilitators | Barriers |
|---|---|---|---|
| Innovation | Innovation Evidence Base | Quality and validity of TR programme [29,33,41,46] | |
| Less objectivity and specificity [29] | |||
| Innovation Relative Advantage | Attractiveness for patients: less travelling and shorter waiting time, personalised interventions, independent continuation of therapy [25,31,32,46,47,48,51] | ||
| Error-free functioning of the innovation [38] | |||
| Access for more patients [46] | |||
| Greater flexibility (for both sides) [46] | |||
| Similar interfaces to other well-known systems [33] | |||
| Consistency of schedule and programme components [46] | |||
| Efficiency of the innovation [42] | |||
| Limited treatment methods, e.g., inability of palpation [26,29,32,43,46,47,48] | |||
| Reduction in patient interaction through TR [26] | |||
| Innovation Adaptability | Adaptability with existing programmes [33,37,46] | Platform flexibility and adaptability [29,33,41,46,52] | |
| Innovation Complexity | Ease of use [29,31,42,43,51,52] | Usability [27,32] | |
| Availability of FAQs [51] | |||
| Availability of video instructions [51] | |||
| Innovation Design | Unrealistic treatment environment [26] | ||
| Innovation Cost | See “resources” | ||
| Inner Setting | Structural Characteristics: Physical Infrastructure | Use of existing infrastructure [45,46] | |
| Adequate space, consultation rooms and equipment [36,38,43] | Limited space [36,39,47] | ||
| Lack of specialised therapy equipment at patients’ home [26,32,36] | |||
| Structural Characteristics: Information Technology Infrastructure | Internet failure [26,31,42,46] | ||
| Technological issues like server breakdowns, poor video quality and initial implementation (clinicians) [26,27,30,34,38,41,42,43,44,46,48,50] | |||
| Structural Characteristics: Work Infrastructure | Clearly defined roles and responsibilities [31] | ||
| Flexibility of clinical regulations, organisational policies and procedures [33] | High level of bureaucracy [26] | ||
| Development of policies and procedures [46] | Ineffectiveness of organisational policies [25] | ||
| Technological support [36,42,43,44,46,51,52] | Slowness of technical support [31] | ||
| High workload [41] | |||
| Relational Connections | Embedding in interdisciplinary care [44] | ||
| Positive reinforcement [25] | |||
| Counselling [25] | |||
| Communication | Supportive and effective communication strategies [30,42,43,46] | No clear communication pathways were established [46] | |
| Information provision about the application and processes [25,32,52] | Lack of information about the innovation and its implementation (staff) [46] | ||
| Common language [33] | Lack of common language between patient, therapist, and technologist [26] | ||
| Intervention not available in local language [25,27] | |||
| Challenges in virtual communication [32,46,48] | |||
| Maintenance of platform information [33] | |||
| Culture: Human-Equality-Centredness | Right of co-determination (staff) [48] | ||
| Culture: Recipient-Centredness | Participants support and connectedness [46,47] | Safety of the patients, e.g., dysphagia or risk of falling [26,29,45,46] | |
| Relationship building with participants [38,46] | Unreachability of patients/relatives in vulnerable or risky situation [33] | ||
| Patients are pushed less [48] | |||
| Privacy concerns (patients) [26,41] | |||
| Culture: Learning-Centredness | Exchange and problem solving of challenges [46] | ||
| Compatibility | Incompatibility with existing technology [42] | ||
| Incompatibility with existing workflows [46] | |||
| Incompatibility with psychosocial components of clinical practice [35] | |||
| Inability to conduct group-based sessions [45] | |||
| Lack of appropriate patients (lack of experience) [27,30] | |||
| Relative Priority | Prioritisation of the innovation [36] | Lack of priority for TR [26] | |
| Incentive System | Lack of tangible or intangible benefits or incentives [46] | ||
| Available Resources | Financial resources [52] | Lack of financial resources/financing for the programme [25,33,34,38,39,42,46,50,52] | |
| Time to learn [51,52] | Lack of time resources [25,29,30,33,34,37,38,41,52] | ||
| Adequate technical resources in TR centres [29,36,43,44,46,52] | Lack of adequate technology and software in rehab centres [46,47] | ||
| Well-trained staff [38,46] | Lack of human resources, e.g., trained staff [25,26,33,34,35,50] | ||
| Lack of technical equipment and internet access in patients’ home [25,29,32,33,36,39,42,46,48,49] | |||
| Insufficiency of available resources to support the innovation [26,46] | |||
| Access to knowledge | Staff training [31,36,39,42,43,46,48] | ||
| Outer Setting | Local Conditions | Good infrastructure to attract technical staff [47] | Lack of infrastructure [36,41,47,53] |
| Location of healthcare institute [50] | |||
| Limited internet service in rural areas [33] | |||
| Partnership and Connections | Feedbacks from audits [38] | ||
| Broad stakeholder involvement [33] | Not existing networks [35,46] | ||
| Collaboration with patients’ caregivers [53] | Poor cooperation with other stakeholders [26] | ||
| Policies and Laws | Ministry support and guidelines [33] | External policies [25,45,46,47,50] | |
| Integration of the providers’ professional knowledge/mentorship [33,46,47] | Providers willingness [33,50] | ||
| Lack of government initiatives and support [25,26] | |||
| Financing | Insurer buy-in and payment [46] | Insurance coverage/cost assumption [25,32,46] | |
| Lower costs for internet providers [33] | |||
| External Pressure | Marketing and advertising [46] | ||
| Individuals | High-level Leaders | Managers and programme leaders’ involvement [29,33,35,36,43,45,46,47] | Non-involvement of managers and programme leaders [33,46] |
| Implementation Team Members | Structure of the team [29] | Change in team structure [29] | |
| Role of therapists in providing troubleshooting support for technology breakdowns [42,46] | |||
| Other Implementation Support | Family/peer support for patients [25,33,37] | Lack of social support [25,37,40] | |
| Capability | Familiarity with the innovation [46] | Limited knowledge (staff) [25,26,31,32,33,37,39,40,41,45,46,50,52] | |
| Experiences with TR in general [35] | Bad experiences with TR/Feeling inexperienced (staff) [29,42] | ||
| Insecurity (therapists) [48] | |||
| Lack of awareness among health professionals [25] | |||
| Technology competence/lack of technical skills (patients) [25,29,32,34,36,39,45,46,53] | |||
| Lack of (digital) health literacy (patients) [25,41,45] | |||
| Poor health status of patients [26,29,37,38,41,49] | |||
| Opportunity | Interruptions at home (patients) [49] | ||
| Challenges in incorporating the programme in daily routine (patients) [49] | |||
| Motivation | Comfortability using the TR technology (staff) [38] | Negative perception of TR by therapist [42,46] | |
| Willingness/acceptance of therapists [43] | Lack of willingness and professional motivation (staff, provider) [33,46] | ||
| Patients’ motivation, willingness and compliance [27,30,31,37,39,43,51,53] | Non-compliance and demotivation (patients) [25,27,32,35] | ||
| Self-efficacy/determination (patients) [25] | Acceptance/hesitation of patients [25,26,32,37,46,47] | ||
| Concerns (of patients) having fewer direct interactions [31] | |||
| Negative emotional experiences of patients [49] | |||
| Implementation Process | Teaming | Interdisciplinary collaboration in teams [29,44,45,48,52] | |
| Learning from each other [43] | |||
| Planning | Definition of clear service objectives, expectations and limits [33] | Unclear pathways, policies and procedures [27,33,46] | |
| Providers’ autonomy and flexibility in implementing TR into practice [47] | Changes in role and responsibilities/disruption in existing workflows [31] | ||
| Well-planned implementation [38] | Lack of coordination among multidisciplinary clinicians [41] | ||
| Uncertainty in the implementation process [26] | |||
| Pre- and postimplementation support/Leadership support [36,41] | |||
| High expectations (both sides) [26] | |||
| Engaging | Consistent use [46] | Underuse and undervalue TR [42] | |
| Staff engagement [27] | Staff are more comfortable with face-to-face therapy [42] | ||
| Innovation culture and enthusiasm among teams and organisations [29,46,52] | Resistance to change [39] | ||
| Reflecting and Evaluation | Systematically sharing of lessons learned during implementation [46] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stampa, S.; Thienel, C.; Tokgöz, P.; Razum, O.; Dockweiler, C. Factors Facilitating and Inhibiting the Implementation of Telerehabilitation—A Scoping Review. Healthcare 2024, 12, 619. https://doi.org/10.3390/healthcare12060619
Stampa S, Thienel C, Tokgöz P, Razum O, Dockweiler C. Factors Facilitating and Inhibiting the Implementation of Telerehabilitation—A Scoping Review. Healthcare. 2024; 12(6):619. https://doi.org/10.3390/healthcare12060619
Chicago/Turabian StyleStampa, Susanne, Christine Thienel, Pinar Tokgöz, Oliver Razum, and Christoph Dockweiler. 2024. "Factors Facilitating and Inhibiting the Implementation of Telerehabilitation—A Scoping Review" Healthcare 12, no. 6: 619. https://doi.org/10.3390/healthcare12060619
APA StyleStampa, S., Thienel, C., Tokgöz, P., Razum, O., & Dockweiler, C. (2024). Factors Facilitating and Inhibiting the Implementation of Telerehabilitation—A Scoping Review. Healthcare, 12(6), 619. https://doi.org/10.3390/healthcare12060619






