Development of Field Tests for Cardiovascular Fitness Assessment in Wheelchair
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Subjects
2.2. Procedure
2.2.1. Familiarization Session
2.2.2. Incremental Arm Ergometer Test
2.2.3. Experiment 1 Procedure
2.2.4. Experiment 2 Procedure
2.2.5. Instrumentation
2.3. Statistical Analyses
3. Results
3.1. Inter-Sport Comparison of Cardiorespiratory Fitness with Arm Ergometer
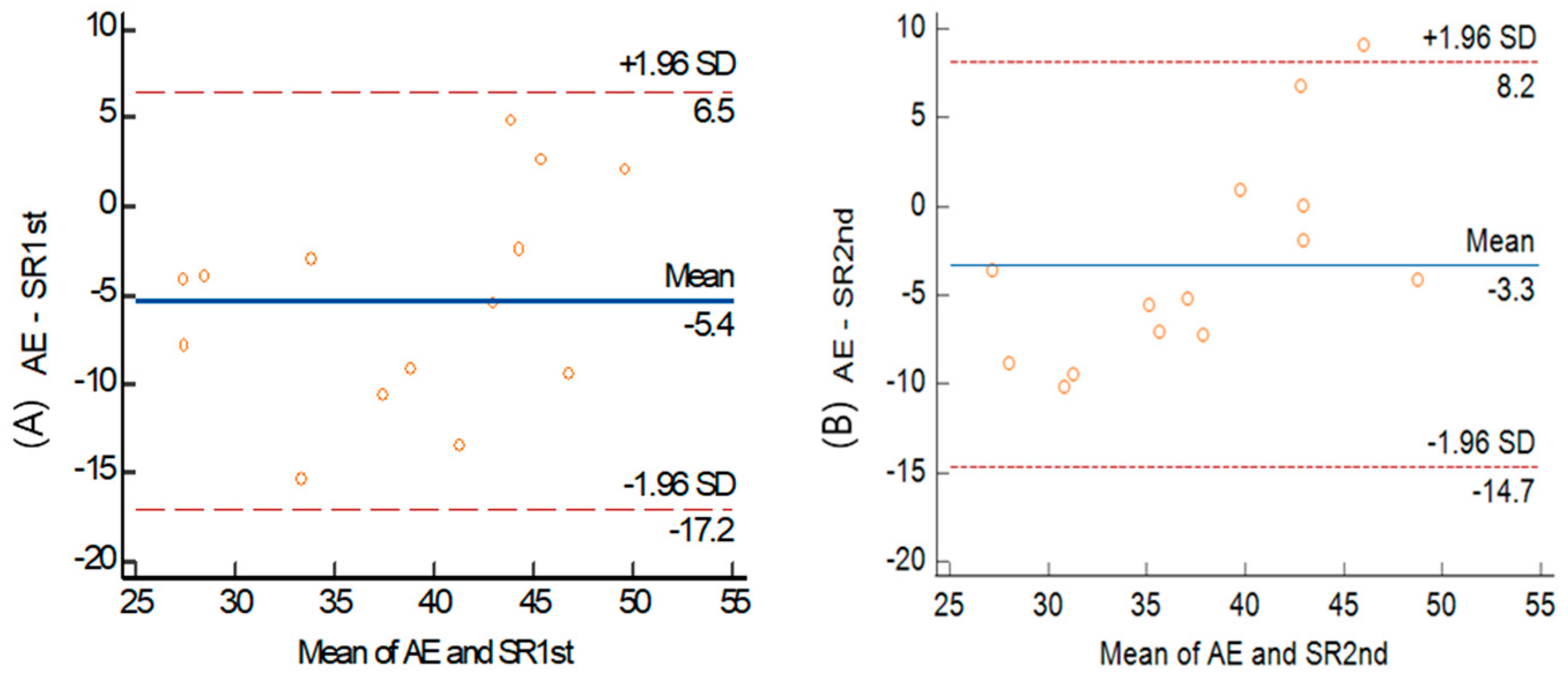
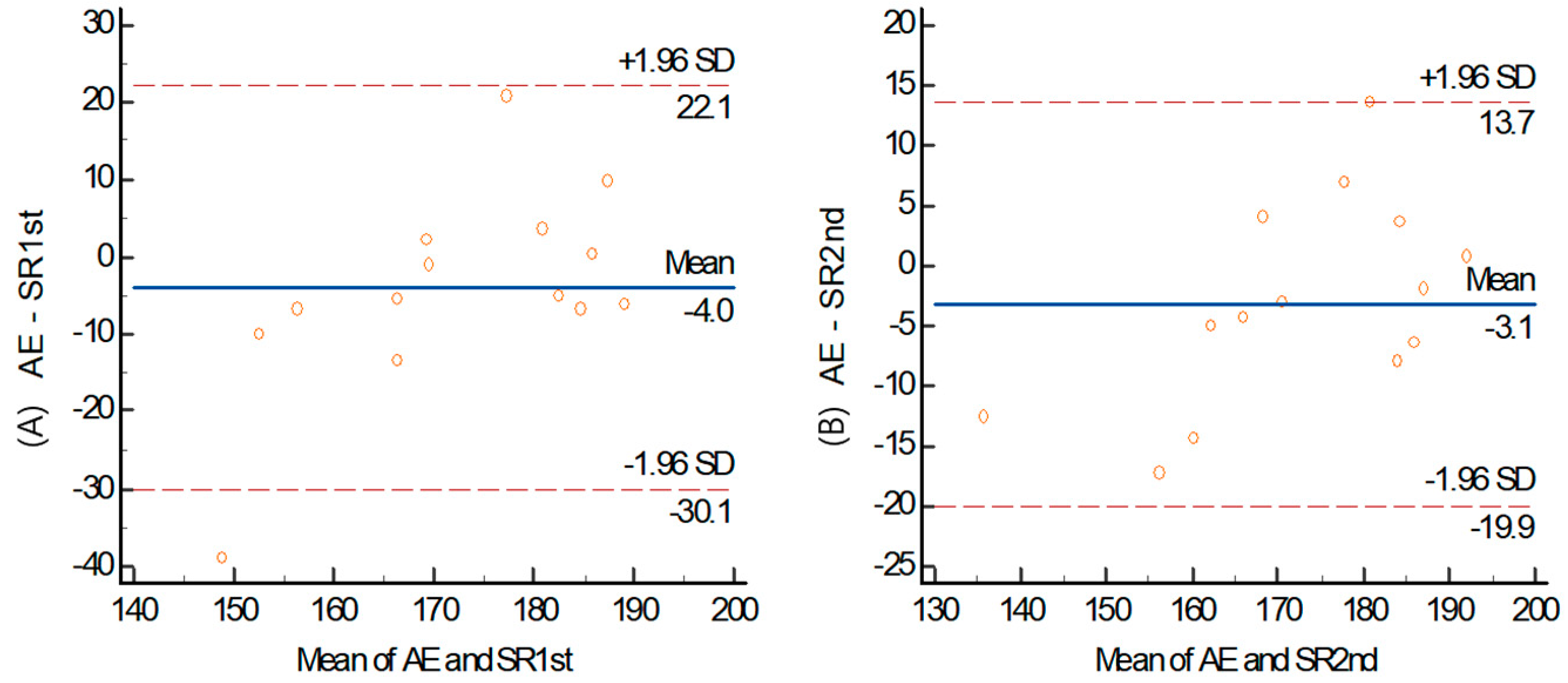
3.2. Validity of Shuttle Ride
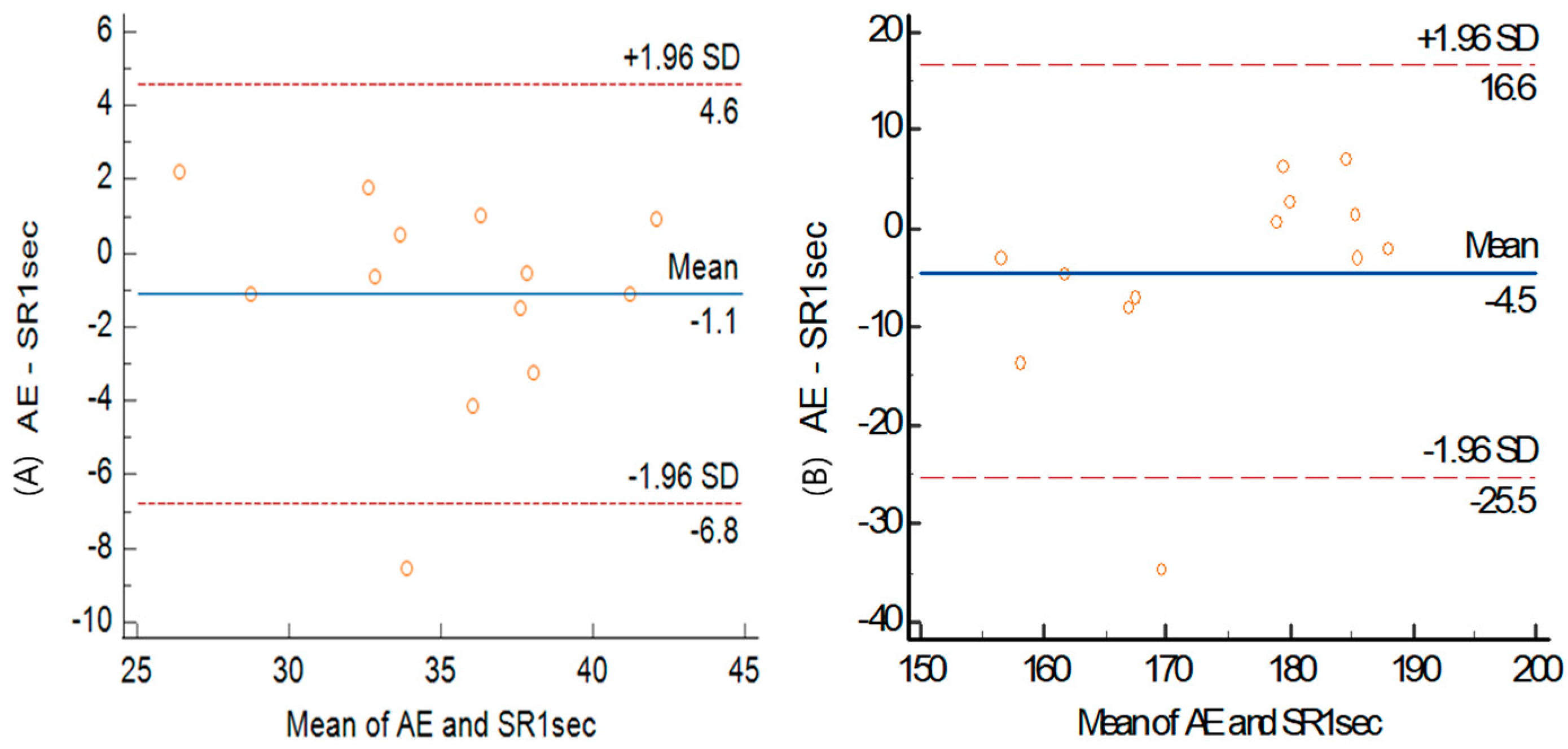
3.3. Correlation between Modified Shuttle Ride and Arm Ergometer
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Myer, G.D.; Jayanthi, N.; DiFiori, J.P.; Faigenbaum, A.D.; Kiefer, A.W.; Logerstedt, D.; Micheli, L.J. Sports Specialization, Part II: Alternative Solutions to Early Sport Specialization in Youth Athletes. Sports Health 2016, 8, 65–73. [Google Scholar] [CrossRef]
- Müller, E.; Benko, U.; Raschner, C.; Schwameder, H. Specific fitness training and testing in competitive sports. Med. Sci. Sports Exerc. 2000, 32, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Fentem, P.H. Physical activity among persons with disabilities—A public health perspective. Exerc. Sport Sci. Rev. 1997, 25, 195–234. [Google Scholar] [CrossRef]
- Bernardi, M.; Guerra, E.; Di Giacinto, B.; Di Cesare, A.; Castellano, V.; Bhambhani, Y. Field evaluation of paralympic athletes in selected sports: Implications for training. Med. Sci. Sport Exer. 2010, 42, 1200–1208. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J. A conceptual model for integrating athletes’ needs and sport demands in the development of competitive mental preparation strategies. Sport Psychol. 1995, 9, 339–357. [Google Scholar] [CrossRef]
- Vinet, A.; Bernard, P.L.; Poulain, M.; Varray, A.; Le Gallais, D.; Micallef, J.P. Validation of an incremental field test for the direct assessment of peak oxygen uptake in wheelchair-dependent athletes. Spinal Cord 1996, 34, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Veeger, H.E.; Hadj Yahmed, M.; van der Woude, L.H.; Charpentier, P. Peak oxygen uptake and maximal power output of Olympic wheelchair-dependent athletes. Med. Sci. Sports Exerc. 1991, 23, 1201–1209. [Google Scholar] [CrossRef]
- Nightingale, T.E.; Rouse, P.C.; Thompson, D.; Bilzon, J.L.J. Measurement of Physical Activity and Energy Expenditure in Wheelchair Users: Methods, Considerations and Future Directions. Sports Med. Open 2017, 3, 10. [Google Scholar] [CrossRef]
- Franklin, B.A.; Swantek, K.I.; Grais, S.L.; Johnstone, K.S.; Gordon, S.; Timmis, G.C. Field test estimation of maximal oxygen consumption in wheelchair users. Arch. Phys. Med. Rehabil. 1990, 71, 574–578. [Google Scholar]
- Vanderthommen, M.; Francaux, M.; Colinet, C.; Lehance, C.; Lhermerout, C.; Crielaard, J.M.; Theisen, D. A multistage field test of wheelchair users for evaluation of fitness and prediction of peak oxygen consumption. J. Rehabil. Res. Dev. 2002, 39, 685–692. [Google Scholar]
- Verschuren, O.; Zwinkels, M.; Ketelaar, M.; Reijnders-van Son, F.; Takken, T. Reproducibility and validity of the 10-m shuttle ride test in wheelchair-using children and adolescents with cerebral palsy. Phys. Ther. 2013, 93, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Léger, L.; Boucher, R. An indirect continuous running multistage field test: The Université de Montréal track test. Can. J. Appl. Sport Sci. 1980, 5, 77–84. [Google Scholar] [PubMed]
- Poulain, M.; Vinet, A.; Bernard, P.L.; Varray, A. Reproducibility of the Adapted Leger and Boucher Test for wheelchair-dependent athletes. Spinal Cord 1999, 37, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Vinet, A.; Le Gallais, D.; Bouges, S.; Bernard, P.L.; Poulain, M.; Varray, A.; Micallef, J.P. Prediction of VO(2peak) in wheelchair-dependent athletes from the adapted Léger and Boucher test. Spinal Cord 2002, 40, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Vanlandewijck, Y.; Spaepen, A.; Theisen, D.; Van de Vliet, P.; Pétré, L.; van der Woude, L.; Hopman, M.; van Kemenade, C. Determination of Work Capacity in Wheelchair Sportsmen in a Sport Specific Environment; IOS Press: Amsterdam, The Netherlands, 1999. [Google Scholar]
- Dupitier, E.; Voisin, M.; Stalens, C.; Laforet, P.; Pouplin, S. Identification of wheelchair seating criteria in adults with neuromuscular diseases: A Delphi study. PLoS ONE 2023, 18, e0290627. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, NY, USA, 2013. [Google Scholar]
- Churton, E.; Keogh, J.W. Constraints influencing sports wheelchair propulsion performance and injury risk. BMC Sports Sci. Med. Rehabil. 2013, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Gee, C.M.; Lacroix, M.A.; Stellingwerff, T.; Gavel, E.H.; Logan-Sprenger, H.M.; West, C.R. Physiological Considerations to Support Podium Performance in Para-Athletes. Front. Rehabil. Sci. 2021, 2, 732342. [Google Scholar] [CrossRef] [PubMed]
- Goosey-Tolfrey, V.L.; Leicht, C.A. Field-based physiological testing of wheelchair athletes. Sports Med. 2013, 43, 77–91. [Google Scholar] [CrossRef]
- Chang, S.C.; Adami, A.; Lin, H.C.; Lin, Y.C.; Chen, C.P.C.; Fu, T.C.; Hsu, C.C.; Huang, S.C. Relationship between maximal incremental and high-intensity interval exercise performance in elite athletes. PLoS ONE 2020, 15, e0226313. [Google Scholar] [CrossRef]
- Gil, S.M.; Yanci, J.; Otero, M.; Olasagasti, J.; Badiola, A.; Bidaurrazaga-Letona, I.; Iturricastillo, A.; Granados, C. The Functional Classification and Field Test Performance in Wheelchair Basketball Players. J. Hum. Kinet. 2015, 46, 219–230. [Google Scholar] [CrossRef]
- Yanci, J.; Granados, C.; Otero, M.; Badiola, A.; Olasagasti, J.; Bidaurrazaga-Letona, I.; Iturricastillo, A.; Gil, S. Sprint, agility, strength and endurance capacity in wheelchair basketball players. Biol. Sport 2015, 32, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.; Choi, S. Development of Estimation Equation for Peak Oxygen Uptake Using Shuttle Run in Wheelchair Basketball Players. Korean J. Adapt. Phys. Act. 2020, 28, 93–102. [Google Scholar]
- Verschuren, O.; Bosma, L.; Takken, T. Reliability of a shuttle run test for children with cerebral palsy who are classified at Gross Motor Function Classification System level III. Dev. Med. Child Neurol. 2011, 53, 470–472. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Takken, T.; Ketelaar, M.; Gorter, J.W.; Helders, P.J. Reliability and validity of data for 2 newly developed shuttle run tests in children with cerebral palsy. Phys. Ther. 2006, 86, 1107–1117. [Google Scholar] [CrossRef]
- Vanlandewijck, Y.C.; Daly, D.J.; Theisen, D.M. Field test evaluation of aerobic, anaerobic, and wheelchair basketball skill performances. Int. J. Sports Med. 1999, 20, 548–554. [Google Scholar] [CrossRef]
- Monteiro, E.R.; Vingren, J.L.; Corrêa Neto, V.G.; Neves, E.B.; Steele, J.; Novaes, J.S. Effects of Different Between Test Rest Intervals in Reproducibility of the 10-Repetition Maximum Load Test: A Pilot Study with Recreationally Resistance Trained Men. Int. J. Exerc. Sci. 2019, 12, 932–940. [Google Scholar]
- Requejo, P.S.; Furumasu, J.; Mulroy, S.J. Evidence-Based Strategies for Preserving Mobility for Elderly and Aging Manual Wheelchair Users. Top. Geriatr. Rehabil. 2015, 31, 26–41. [Google Scholar] [CrossRef]


| Types of Disabilities | Causes of Disabilities | ||
|---|---|---|---|
| Cerebral palsy | Locomotor disability | Congenital disability | Acquired disability |
| 1 | 13 | 2 | 12 |
| Sports | Variables | M ± SD |
|---|---|---|
| Para ice hockey (Experiment 1) (n = 14) | Experience (year) | 12.1 ± 5.8 |
| Period of disability (year) | 22.7 ± 11.6 | |
| Disability classification | 2.5 ± 1.16 | |
| VO2max with AE (mL/kg/min) | 35.9 ± 8.9 | |
| HRmax with AE (beats/min) | 170.6 ± 18.2 | |
| Wheelchair basketball (Experiment 2) (n = 13) | Experience (year) | 10 ± 6 |
| Period of disability (year) | 15.6 ± 7.5 | |
| Disability classification | 1.8 ± 1.0 | |
| VO2max with AE (mL/kg/min) | 34.6 ± 4.5 | |
| HRmax with AE (beats/min) | 171.8 ± 14.4 |
| Level | Shuttle Count | Distance (m) | Standard Audio Cue | +1 s | 1.5 s | |||
|---|---|---|---|---|---|---|---|---|
| Time (s) | Speed (km/h) | Time (s) | Speed (km/h) | Time (s) | Speed (km/h) | |||
| 1 | 7 | 15 | 8.5 | 6.4 | 9.5 | 5.7 | 10 | 5.4 |
| 2 | 8 | 15 | 8 | 6.8 | 9 | 6.0 | 9.5 | 5.7 |
| 3 | 8 | 15 | 7.6 | 7.1 | 8.6 | 6.3 | 9.1 | 5.9 |
| 4 | 9 | 15 | 7.2 | 7.5 | 8.2 | 6.6 | 8.7 | 6.2 |
| 5 | 9 | 15 | 6.9 | 7.8 | 7.9 | 6.8 | 8.4 | 6.4 |
| 6 | 10 | 15 | 6.5 | 8.3 | 7.5 | 7.2 | 8 | 6.8 |
| 7 | 10 | 15 | 6.3 | 8.6 | 7.3 | 7.4 | 7.8 | 6.9 |
| 8 | 11 | 15 | 6 | 9.0 | 7 | 7.7 | 7.5 | 7.2 |
| 9 | 11 | 15 | 5.8 | 9.3 | 6.8 | 7.9 | 7.3 | 7.4 |
| 10 | 11 | 15 | 5.5 | 9.8 | 6.5 | 8.3 | 7 | 7.7 |
| 11 | 12 | 15 | 5.3 | 10.2 | 6.3 | 8.6 | 6.8 | 7.9 |
| 12 | 12 | 15 | 5.1 | 10.6 | 6.1 | 8.9 | 6.6 | 8.2 |
| 13 | 13 | 15 | 5 | 10.8 | 6 | 9.0 | 6.5 | 8.3 |
| 14 | 13 | 15 | 4.8 | 11.3 | 5.8 | 9.3 | 6.3 | 8.6 |
| 15 | 13 | 15 | 4.6 | 11.7 | 5.6 | 9.6 | 6.1 | 8.9 |
| 16 | 14 | 15 | 4.5 | 12.0 | 5.5 | 9.8 | 6 | 9.0 |
| 17 | 14 | 15 | 4.4 | 12.3 | 5.4 | 10.0 | 5.9 | 9.2 |
| 18 | 15 | 15 | 4.2 | 12.9 | 5.2 | 10.4 | 5.7 | 9.5 |
| 19 | 15 | 15 | 4.1 | 13.2 | 5.1 | 10.6 | 5.6 | 9.6 |
| 20 | 16 | 15 | 1 | 13.5 | 5 | 10.8 | 5.5 | 9.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, E.H.; Choi, B.-A.; Seo, Y. Development of Field Tests for Cardiovascular Fitness Assessment in Wheelchair. Healthcare 2024, 12, 580. https://doi.org/10.3390/healthcare12050580
Cho EH, Choi B-A, Seo Y. Development of Field Tests for Cardiovascular Fitness Assessment in Wheelchair. Healthcare. 2024; 12(5):580. https://doi.org/10.3390/healthcare12050580
Chicago/Turabian StyleCho, Eun Hyung, Bong-Arm Choi, and Yongsuk Seo. 2024. "Development of Field Tests for Cardiovascular Fitness Assessment in Wheelchair" Healthcare 12, no. 5: 580. https://doi.org/10.3390/healthcare12050580
APA StyleCho, E. H., Choi, B.-A., & Seo, Y. (2024). Development of Field Tests for Cardiovascular Fitness Assessment in Wheelchair. Healthcare, 12(5), 580. https://doi.org/10.3390/healthcare12050580








