Abstract
Background: Gaining knowledge of the various reasons behind people’s consumption of highly processed foods has the potential to enhance obesity prevention initiatives and open avenues to tailor treatment approaches for obesity and binge eating at a more personalized level. This contribution aimed to test the psychometric properties and factor structure of the Palatable Eating Motives Scale (PEMS-IT) in a community sample of Italian adults. Methods: A confirmatory factor analysis was performed to test the factor structure of the Italian version of the PEMS (PEMS-IT) on a total of 616 respondents. Furthermore, the reliability and convergent validity analysis of the tool were evaluated. Results: The analysis confirmed the four-factor structure of PEMS-IT [(YBχ2 (164) = 537.901; p < 0.001, the CFI = 0.918, RMSEA = 0.072; 90%CI [0.065–0.078]; p(RMSEA < 0.05) < 0.001, and SRMR = 0.080] and satisfactory reliability on its subscales (Cronbach’s α: 0.745–0.917). Positive correlations were also found with food addiction and binge-eating symptoms, compulsive eating behavior, and uncontrolled and emotional eating. Conclusions: The PEMS-IT appears to be an instrument with promising psychometric properties and potential applications in clinical settings. However, it also has some limitations, and future studies could focus on improving the semantic content of the elements to increase the overall utility and precision of the instrument.
1. Introduction
Although there has been progress in understanding the environmental, genetic, and physiological factors that contribute to obesity, the global prevalence of this chronic disease remains elevated and is expected to increase [1,2]—as the challenge of maintaining weight loss is common even after initial success [3,4,5,6,7].
One potential factor contributing to the increase in overweight and obesity, as well as to the development of binge-eating disorders (BEDs), is the proliferation of highly processed foods (HPFs) [8]. These foods are typically characterized by high levels of fat, sugar, and salt, coupled with small amounts of vitamins, minerals, and fiber. Examples of highly processed foods are fizzy drinks, packaged snacks, cakes, and certain types of ready-to-eat foods. In addition, the abundance of food additives, including artificial colors, flavors, or preservatives, makes HPFs hyperpalatable and attractive.
Consumption of foods considered palatable is notoriously driven by pleasure rather than hunger or metabolic need [9,10]. Eating too much of them causes a profound state of reward hyposensitivity, similar to that of drug abuse, that can lead to the development of compulsive-like eating [11]. Therefore, high-carbohydrate and high-fat foods could be considered palatable. They are widely available to adults and children, both in terms of convenience and economic cost [12].
But people may differ in the reasons or motivations behind the consumption of hyperpalatable processed foods [13].
Some people may indulge in tasty foods for conventional or adaptive reasons, such as to celebrate an occasion, while others may do so for less adaptive reasons, including coping with negative emotions and stress.
Understanding what drives the consumption of hyper-processed palatable foods in the community could inform obesity prevention efforts and pave the way for more personalized treatment strategies for obesity and binge eating [14]. Furthermore, it could contribute to efforts to improve the nutritional quality of individuals’ diets [15].
A motivational model that has robust evidence supporting its validity in the context of alcohol use and has recently been extended to the consumption of hyper-processed palatable foods could offer a unified framework for understanding various motives that might drive hedonic eating [16].
Indeed, evidence suggests the rewarding effect of both alcohol and HPFs [17,18] and that energy overconsumption may be driven by the same motives across behaviors.
Among young adults, alcohol consumption for reward enhancement and social reasons is positively correlated with the level of alcohol consumption, while drinking to cope with negative emotions is directly associated with alcohol-related problems [19]. Similarly, eating to cope with negative emotions is related to binge-eating tendencies in studies conducted on college students [20,21] and motives such as reward enhancement, social reinforcement, and conformity also demonstrate significant associations with binge eating [17].
Hyper-processed palatable foods constitute the vast majority of energy intake during binge-eating episodes, and higher scores of hyper-processed food consumption are strongly correlated with increased chances of developing BEDs [22]. As for BEDs, food addiction is linked to greater reward sensitivity, greater food cravings, and hyper-responsiveness to HPFs [23,24,25].
Therefore, to deepen the knowledge of the motivations for consuming hyper-processed palatable foods, Burgess and colleagues (2014) created the Palatable Eating Motives Scale (PEMS) [17], a self-report scale derived from the revised Drinking Motives Questionnaire (DMQ-R) [26,27].
This questionnaire categorizes four reasons for eating palatable foods and beverages when not driven by hunger: coping, reward enhancement, social, and conformity motives.
Motives for coping encompass items that pertain to the consumption of palatable foods or drinks as a means of addressing negative emotions such as anxiety, sadness, frustration, or anger. The reward enhancement motive involves questions about the consumption of delicious foods or beverages to amplify positive experiences, emotions, or inherent satisfactory qualities that are not related to social contexts. For example, this may include eating certain foods that bring pleasure or contribute to personal happiness.
Social motives include inquiries about the consumption of palatable foods or beverages for social purposes, such as enjoying them at a party or participating in eating behaviors to socialize more with friends. On the other hand, the conformity motive involves questions about consuming tasty foods in response to external pressures, such as conforming to social expectations within a group of friends or adopting eating behaviors to avoid exclusion.
Since the PEMS is currently unavailable for implementation within the Italian population, this study aimed to adapt and test the psychometric properties of the Italian version of the PEMS (PEMS-IT) in a sample of Italian respondents from the general population and to examine its factor structure.
2. Materials and Methods
This research used a cross-sectional research study design to investigate the factor structure and psychometric properties of PEMS-IT among a sample of Italian adults from the community.
2.1. Translation and Cultural Adaptation
Translation and cross-cultural adaptation were carried out according to the cross-cultural adaptation guidelines of self-report measures proposed by Beaton et al. (2000), which included the following steps: 1. independent translations; 2. synthesis of these translations; 3. back-translations; 4. expert committee evaluation; and 5. pre-test of the pre-final version [28]. All translators involved in the process were bilingual and had a special professional background in psychology or other relevant areas.
- Step 1: Translation
First, the PEMS was translated from English into Italian by two natural multilingual translators from Italy. Along with clear directions, each translator independently translated the original content and response options. Neither the conceptual content of the questionnaire nor its concepts were known to either of the translators.
- Step 2: Synthesis of the translations
Subsequently, a synthesis of both translations was produced through discussion between the translators until a consensus was reached. Thus, a theoretically equivalent translation of the original questionnaire was obtained.
- Step 3: Back-translation
This reconciled version was then provided to a professional back-translator who was also bilingual and blind to the original English versions of the tool. The back-translated questionnaire was further compared with the original to detect any misinterpretation or imprecisions in the translation process.
- Step 4: Expert committee evaluation
Then, both the translation synthesis and the back-translated version of the PEMS were discussed between all translators and professionals involved in this study. These comprised two health professionals (psychotherapists) with many years of experience in the field of obesity and eating disorder treatment (authors G.C. and G.P.) and an expert in the validation of psychiatric questionnaires (author A.A.R.). Discussion and feedback were recorded and considered in the harmonization process. Once a consensus was reached on the identified differences in the proceeding, the PEMS-IT was proofread for grammar, spelling, and content errors, generating a pre-final version of the tool.
- Step 5: Pre-test of the pre-final version
Finally, the resulting version of the PEMS-IT was administered to a representative sample of 15 persons from the general population to assess the comprehensibility of the items. No further adjustments were made. The final version of the PEMS-IT is reported in Supplementary Materials S1.
2.2. Sample Size Calculation
The size of the sample was chosen a priori, and the ‘n:q’ criterion, which denotes the relationship between individuals and parameters, was used [29]. A requirement of 10 participants per parameter (=46) was established, culminating in a sample size of no fewer than 460 participants being determined.
2.3. Procedure
Based on the methodology employed in prior research [30,31,32,33], an online survey was conducted using Qualtrics software//February 2023 and distributed using the snowball sampling method on social networks (e.g., Facebook, Twitter, and Instagram). The recruitment materials provided detailed information on eligibility criteria and additional specifics to ensure that participants could make informed decisions, including assurances of anonymity for their responses. Those who agreed to participate completed the survey online.
Each participant was requested to provide sociodemographic (i.e., sex and age) and clinical information (weight and height, utilized for body mass index (BMI) calculation). Together with PEMS-IT, respondents were also asked to complete the Italian version of the following self-report questionnaires: the modified version of the Yale Food Addiction Scale 2.0 (mYFAS 2.0), the Binge Eating Scale (BES), the Measure of Eating Compulsivity 10-Italian version (MEC10-IT), the Three Factor Eating Questionnaire-18 (TFEQ-R-18), and the Repetitive Eating Questionnaire (Rep(Eat)-Q).
Ethical approval for the study was obtained from the Ethics Committee of the I.R.C.C.S. Istituto Auxologico Italiano, under protocol number 2020_02_18_04. All procedures adhered to the ethical standards set by the institutional and/or national research committee and were in accordance with the Declaration of Helsinki of 1964 and its subsequent amendments or equivalent ethical standards.
2.4. Participants
The inclusion criteria for the study participants were (A) being a native Italian speaker; (B) being 18 years or older; and (C) providing online consent to participate. Individuals were excluded if they (A) had visual and/or cognitive impairments that hindered the completion of the survey and (B) failed to respond to all the survey items.
The sample was made up of 616 respondents from the general population. The sample consisted of 474 women (76.9%) and 142 men (23.1%), between 18 and 84 years old (mean = 29.21, SD = 11.69) and with a BMI ranging from 14.84 to 55.74 kg/m2 (mean = 22.17, SD = 4.22, median = 21.30, skewness = 2.58, kurtosis = 11.84). More specifically, most of the sample was of normal weight (BMI of 18.5 to 24.9 kg/m2; n = 443; 71.9%), followed by underweight (BMI of 16 to 18.4 kg/m2; n = 70; 11.4%) and overweight (BMI of 25 to 29.9 kg/m2; n = 70; 11.4). The remaining part of the sample included class I obesity (BMI of 30 to 34.9 kg/m2; n = 13; 2.1%), class II obesity (BMI of 35 to 39.9 kg/m2; n = 9; 1.5%), class III obesity (BMI ≥ 40 kg/m2; n = 6; 1%), and severely underweight (BMI < 16 kg/m2; n = 5; 0.8%) [34].
2.5. Measures
The Palatable Eating Motives Scale (PEMS) [17] consists of 20 items answered on a 5-point Likert scale ranging from 1 that measures motivations for eating a variety of palatable foods and beverages across four main dimensions: social motives (Items 3, 5, 11, 14, 16); coping motives (Items 4, 6, 15, 17); reward enhancement motives (Items 7, 9, 10, 13, 18); and conformity motives (Items 2, 8, 12, 19, 20). Scores are obtained by the sum of these items.
The Modified Yale Food Addiction Scale 2.0 (mYFAS2.0) [30,35] comprises 11 diagnostic items from the original YFAS 2.0, along with two questions that assess impairment/distress. The scale retains the key characteristics of the original YFAS 2.0, including two scoring options (symptom count and diagnostic scores) and a diagnostic continuum indicating severity. All items are evaluated on an eight-point Likert scale, ranging from 0 (never) to 7 (every day). In the present sample, the internal consistency of mYFAS2.0 was KR20 = 0.852.
The Binge Eating Scale (BES) [36] consists of 16 items designed to assess prominent behavioral aspects (such as rapid eating or consuming large amounts of food) and affective/cognitive symptoms (such as guilt, a sense of being out of control, or an inability to stop eating) associated with episodes of binge eating. Each item presents 3 to 4 statements representing varying degrees of severity for the measured characteristics. Participants are asked to choose the statement that captures their personal experience. In the present study, BES showed acceptable internal consistency, with Cronbach’s alpha equal to 0.908.
The Italian version of the Measure of Eating Compulsivity (MEC10-IT) [32] is a brief, feasible, solid, and extremely reliable tool consisting of 10 items answered on a 5-point Likert-type scale ranging from 0 (very untrue) to 4 (very true) aimed at measuring compulsive eating behaviors and binge eating behaviors. High scores correspond to a high degree of eating compulsivity. The internal consistency of MEC10-IT in the present study was equal to 0.923.
The Three Factor Eating Questionnaire Revised–18 (IT-TFEQ-R-18) [37] is a reliable, solid, and psychometrically sound questionnaire that consists of 18 items measured on a 4-point Likert scale ranging from 1 (definitely false) to 4 (definitely true) designed to assess three main cognitive and behavioral domains of eating disorders: cognitive restraint (CR-6 items), uncontrolled eating (UE-9 items), and emotional eating (EE-3 items). High scores reflect a higher level of each dimension. In this study, the internal consistency of the IT-TFEQ-R-18 scales was 0.818 for the CR scale, 0.872 for the UE scale, and 0.884 for the EE scale.
The Repetitive Eating Questionnaire (Rep(Eat)-Q) [38] is a reliable, promising, and psychometrically based questionnaire that aims to measure a peculiar form of food addiction: grazing. It comprises 12 items answered on a 7-point Likert scale ranging from 0 (never) to 6 (every day) measuring the frequency of the attitudinal and behavioral characteristics of grazing during the past 28 days. It is made up of two dimensions: compulsive grazing (CG) and repetitive eating (RE), and a total score. The internal consistency of the Rep(Eat)-Q was equal to 0.910 for the total score, 0.887 for the RE scale, and 0.857 for the CG scale.
2.6. Statistical Analysis
Statistical analyses were performed with the R software—version 4.3.2 [39,40] and the following packages: lavaan [41,42], psych [43], psychTools [44], and tidyverse [45]. Graphical representations were made with the semPlot package [46].
According to its original validation study [17], a first-order model was specified comprising four correlated factors (Figure 1). Since the original validation study did not assume a ‘general factor’ (total score), no alternative models were tested. The MLR estimator (namely, robust maximum likelihood) was used to evaluate the factor structure of the PEMS-IT [47,48]—as some items were not normally distributed. Model fit was assessed using (A) the Yuan–Bentler Chi-square statistic (YBχ2), (B) the Root-Mean Square Error of Approximation (RMSEA), (C) the Comparative Fit Index (CFI), and (D) the Standardized Root Mean Residual (SRMR) [29,47,48]. To evaluate the goodness of fit, the following cut-off criteria were used: (A) statistical non-significance of the YBχ2, (B) an RMSEA less than 0.08, (C) a CFI higher than 0.95, and (D) an SRMR lower than 0.08 [29,49,50].
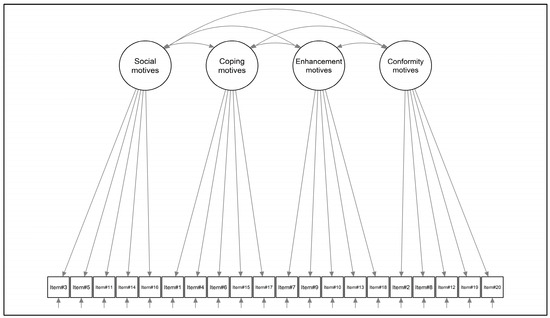
Figure 1.
Structural model of the PEMS-IT.
Once the factor structure of PEMS-IT was tested, its internal consistency was evaluated with Cronbach’s alpha (α) and McDonald’s omega (ω) [51]; for categorical/dichotomous items, the Kuder–Richardson20 (KR20) coefficient was used. Additionally, adjusted item–total correlation was calculated [52,53].
Convergence validity was performed using the Pearson correlation coefficient [52], with interpretations guided by Cohen’s standards: r < 0.10, negligible; r ranging from 0.10 to 0.30, minimal; r from 0.30 to 0.50, moderate; and r > 0.50, substantial [54].
3. Results
3.1. Structural Validity
The four-factor model (Figure 1) showed a good fit to the data: YBχ2 (164) = 537.901; p < 0.001, the CFI = 0.918, RMSEA = 0.072; 90%CI [0.065–0.078]; p(RMSEA < 0.05) < 0.001, and SRMR = 0.080. Social motive was weakly correlated with coping strategies (ϕ = 0.227), and moderately correlated with both reward enhancement (ϕ = 0.489) and conformity (ϕ = 0.541) motives. In addition, coping strategies were moderately correlated with reward enhancement motives (ϕ = 0.447) and weakly correlated with conformity motives (ϕ = 0.118). Last, reward enhancement motives did not correlate with conformity (ϕ = 0.045). The standardized factor loadings ranged from 0.317 (item#10; conformity) to 0.921 (item#4; coping). All statistics are shown in Table 1 below.

Table 1.
Items’ descriptive statistics and confirmatory factor analysis (CFA) results.
3.2. Internal Consistency
Internal consistency analysis revealed satisfactory results. Indeed, for the social motives scale, McDonald’s ω was equal to 0.845 and Cronbach’s α was equal to 0.840. For the coping motive scale, McDonald’s ω was equal to 0.922 and Cronbach’s α was equal to 0.917. In addition, for the reward enhancement motive scale, McDonald’s ω was equal to 0.844 and Cronbach’s α was equal to 0.804. Last, for the social motive scale, McDonald’s ω was equal to 0.749 and Cronbach’s α was equal to 0.745.
3.3. Convergent Validity
As shown in Table 2, small-to-moderate correlations were found between the PEMS-IT scales. Furthermore, considering the social motive scale, moderate associations were found with the PEMS-IT conformity motive scale (r = 0.546, p < 0.001) and the PEMS-IT reward enhancement motive scale (r = 0.447, p < 0.001). Still, only a few (small) correlations were found with other selected convergent measures. Indeed, small associations were found between the total score (r = 0.153, p < 0.001) and the Rep(Eat)-Q CG scale (r = 0.172, p < 0.001).

Table 2.
Correlation analysis.
Regarding the coping motives scale, a moderate association was found with the PEMS-IT reward enhancement motive scale (r = 0.436, p < 0.001). Furthermore, moderate-to-large correlations were found with other convergent measures, particularly with scales that refer to excessive food intake. Indeed, moderate associations were found between the dimensions of the PEMS-IT coping motives and the mYFAS2.0 symptom count of mYFAS2.0 (r = 0.426, p < 0.001), the total score of BES (r = 0.587, p < 0.001), the total score of MEC10-IT (r = 0.554, p < 0.001), the TFEQ-R-18-uncontrolled eating scale (r = 0.498, p < 0.001), and the Rep(Eat)-Q total score (r = 0.528, p < 0.001). Furthermore, a large correlation was found with the TFEQ-R-18-emotional eating scale (r = 0.772, p < 0.001).
Taking into account the reward enhancement motive scale, small associations were found with other convergent measures: the highest association was with the TFEQ-R-18 uncontrolled eating scale (r = 0.343, p < 0.001), followed by the Rep(Eat)-Q total score (r = 0.282, p < 0.001) and the MEC10-IT total score (r = 0.248, p < 0.001).
Finally, small associations were found between the conformity motive scale and other convergent measures: the highest association was with the Rep(Eat)-Q CG scale (r = 0.167, p < 0.001), followed by the BES total score (r = 0.163, p < 0.001) and the TFEQ-R-18-emotional eating scale (r = 0.157, p < 0.001).
4. Discussion
Highly palatable foods play a relevant role in obesity and binge eating. A better understanding of whether individuals eat palatable foods primarily to cope, enhance reward, be social, or conform, measured by the PEMS, would inform the development of personalized treatment strategies for people suffering from eating and weight problems. For this reason, and since the tool is not yet available for use in Italy, the present contribution aimed to explore the psychometric proprieties of the PEMS and to test its factor structure in a sample of Italian adults from the general population.
The results of the confirmatory factor analysis (CFA) supported the structural validity of the PEMS-IT by confirming a four-factor structure: social, coping, reward enhancement, and conformity motives. Indeed, each of the 20 items loaded onto the theoretically hypothesized dimension with good fit indexes—thus demonstrating their successful portrayal of the underlying constructs [29,47].
Furthermore, considering the psychometric characteristics of the tool, reliability analyses revealed satisfactory results on all subscales.
Convergence validity analyses also showed small-to-large associations between the PEMS-IT subscales, as well as between the PEMS-IT subscales with other relevant measures. In particular, moderate-to-large correlations were found between the dimension of coping motives of the PEMS-IT and measures of excessive food intake, including the mYFAS2.0 symptom count (r = 0.426, p < 0.001), the BES score (r = 0.587, p < 0.001), the total MEC10-IT total score (r = 0.554, p < 0.001), the TFEQ-R-18-uncontrolled eating scale (r = 0.498, p < 0.001) and the emotional eating scale (r = 0.772, p < 0.001), and the Rep(Eat)-Q total score (r = 0.528, p < 0.001).
This suggests a tendency to eat HPFs in response to emotional urges. In fact, several systematic reviews and meta-analyses conclude that emotional states significantly impact individual diet choices and can result in the development of disordered eating behaviors and weight problems [55,56,57,58,59,60,61]. In particular, when individuals are under stress, a preference for highly palatable “snack-type” foods over “meal-type” foods has been observed. For example, Baumeister et al. (2002) noted that emotional eating tends to manifest more prominently in snacking behaviors [62]. Furthermore, a study by Boggiano et al. (2017) employing a sample of university students revealed significant positive correlations between the dimensions and the three subscales of the Emotional Eating Scale (EES) [63], namely anger/frustration, anxiety, and depression [21]. In particular, the PEMS coping and reward enhancement subscales (internal motives) correlated with higher BMI and were associated with increased eating concerns and emotion-triggered eating in both sexes, along with binge eating in females [8].
However, the results of this study should be interpreted in light of a few limitations. First, the cross-sectional nature of the sample and its testing only in a community sample, respectively, limit the evaluation of the temporal stability of the PEMS-IT and its external validity. Future research should evaluate the test–retest reliability of the tool and its measurement invariance between non-clinical and clinical samples. Another weakness of this research is that a limited number of emotional eating scales, such as the EES [63], were used to test convergence and incremental validity. Another limitation of this study was the lack of investigation into the divergent validity of the instrument. Future studies should consider evaluating this aspect using modern statistical approaches [64]. Furthermore, from a psychometric point of view, it is important to note that some items (Item#2 and Item#10), distributed on all questionnaire scales, exhibit factor loadings below 0.5. This suggests that although the model fits the data well (fit indices are good), these items do not optimally saturate the latent construct they are measuring. Future studies should consider developing a new version of the instrument by retaining the best items and replacing those that less accurately reflect the investigated construct. Furthermore, another limitation of this study is that the sample is mainly composed of women and that the age and BMI of the respondents vary a great deal, and this could impact the metabolic regulation and eating habits of the individuals. Future research should test possible explanatory models of motives that drive eating behaviors by considering the variables as possible intervening factors.
Despite the constraints mentioned above, this study marks the initial effort to assess the psychometric qualities of PEMS-IT within the broader population of Italy, supporting the validity and reliability of the tool. Importantly, these conclusions are based on robust statistical measures widely recognized throughout the world. Consequently, PEMS-IT emerges as a reliable option for clinical and research applications, as it proficiently detects the primary motivations for eating HPFs that are not related to hunger with precision and efficiency.
5. Conclusions
PEMS-IT is a useful measure for a rapid assessment of the baseline reasons for HPF consumption, which contribute greatly to obesity and eating-related disorders and influence individuals’ ability to adhere to weight reduction and rehabilitation programs [8]. In the present study, PEMS-IT shows promise for clinical applications; a thorough understanding of its psychometric properties, limitations, and potential areas for improvement is crucial to maximize its utility and precision in assessing motivations related to palatable food consumption. Indeed, this self-report tool could complement existing measures of compulsive or emotional eating, helping to predict the clinical risk of obesity and supporting the development of customized prevention and treatment strategies against obesity, binge eating, and food addiction.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/healthcare12050574/s1, Supplementary Materials S1: The Palatable Eating Motives Scale–Italian version (PEMS-IT).
Author Contributions
Conceptualization, A.A.R.; methodology, A.A.R.; formal analysis, A.A.R.; writing—original draft preparation, G.P. and A.A.R.; writing—review and editing, M.S.; supervision, S.M. and G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board (IRB) at the I.R.C.C.S. Istituto Auxologico Italiano (protocol no. 2020_02_18_04).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Popov, V.B.; Aytaman, A.; Aleman, J.O. Obesity: The Forgotten Pandemic. Am. J. Gastroenterol. 2022, 117, 7–10. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Manzoni, G.M.; Corti, S.; Vegliante, N.; Molinari, E.; Castelnuovo, G. Addressing motivation in globesity treatment: A new challenge for clinical psychology. Front. Psychol. 2012, 3, 317. [Google Scholar] [CrossRef]
- Greaves, C.; Poltawski, L.; Garside, R.; Briscoe, S. Understanding the challenge of weight loss maintenance: A systematic review and synthesis of qualitative research on weight loss maintenance. Health Psychol. Rev. 2017, 11, 145–163. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Manzoni, G.M.; Villa, V.; Cesa, G.L.; Pietrabissa, G.; Molinari, E. The STRATOB study: Design of a randomized controlled clinical trial of Cognitive Behavioral Therapy and Brief Strategic Therapy with telecare in patients with obesity and binge-eating disorder referred to residential nutritional rehabilitation. Trials 2011, 12, 114. [Google Scholar] [CrossRef] [PubMed]
- Evert, A.B.; Franz, M.J. Why Weight Loss Maintenance Is Difficult. Diabetes Spectr. 2017, 30, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Kahan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef]
- Jackson, J.B.; Pietrabissa, G.; Rossi, A.; Manzoni, G.M.; Castelnuovo, G. Brief strategic therapy and cognitive behavioral therapy for women with binge eating disorder and comorbid obesity: A randomized clinical trial one-year follow-up. J. Consult. Clin. Psychol. 2018, 86, 688–701. [Google Scholar] [CrossRef]
- Harb, A.A.; Shechter, A.; Koch, P.A.; St-Onge, M.P. Ultra-processed foods and the development of obesity in adults. Eur. J. Clin. Nutr. 2023, 77, 619–627. [Google Scholar] [CrossRef]
- Fox, C.K.; Northrop, E.F.; Rudser, K.D.; Ryder, J.R.; Kelly, A.S.; Bensignor, M.O.; Bomberg, E.M.; Bramante, C.T.; Gross, A.C. Contribution of Hedonic Hunger and Binge Eating to Childhood Obesity. Child. Obes. 2021, 17, 257–262. [Google Scholar] [CrossRef]
- Burdette, J.H.; Laurienti, P.J.; Miron, L.L.; Bahrami, M.; Simpson, S.L.; Nicklas, B.J.; Fanning, J.; Rejeski, W.J. Functional Brain Networks: Unique Patterns with Hedonic Appetite and Confidence to Resist Eating in Older Adults with Obesity. Obesity 2020, 28, 2379–2388. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; DiFeliceantonio, A.G. Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction 2023, 118, 589–598. [Google Scholar] [CrossRef]
- Lowe, M.R.; Butryn, M.L. Hedonic hunger: A new dimension of appetite? Physiol. Behav. 2007, 91, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Ferriter, C.; Ray, L.A. Binge eating and binge drinking: An integrative review. Eat. Behav. 2011, 12, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Cattivelli, R.; Castelnuovo, G.; Musetti, A.; Varallo, G.; Spatola, C.A.M.; Riboni, F.V.; Usubini, A.G.; Tosolin, F.; Manzoni, G.M.; Capodaglio, P.; et al. ACTonHEALTH study protocol: Promoting psychological flexibility with activity tracker and mHealth tools to foster healthful lifestyle for obesity and other chronic health conditions. Trials 2018, 19, 659. [Google Scholar] [CrossRef]
- Boggiano, M.M. Palatable Eating Motives Scale in a college population: Distribution of scores and scores associated with greater BMI and binge-eating. Eat. Behav. 2016, 21, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Fazzino, T.L.; Raheel, A.; Peppercorn, N.; Forbush, K.; Kirby, T.; Sher, K.J.; Befort, C. Motives for drinking alcohol and eating palatable foods: An evaluation of shared mechanisms and associations with drinking and binge eating. Addict. Behav. 2018, 85, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Burgess, E.E.; Turan, B.; Lokken, K.L.; Morse, A.; Boggiano, M.M. Profiling motives behind hedonic eating. Preliminary validation of the Palatable Eating Motives Scale. Appetite 2014, 72, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Rogers, P.J. Determinants of food reward and some parallels with vehicles for self-administration of nicotine, caffeine and alcohol. Addiction 2023, 118, 601–602. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.L.; Kuntsche, E.; Levitt, A.; Barber, L.L.; Wolf, S. Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In The Oxford Handbook of Substance Use and Substance Use Disorders; Oxford University Press: New York, NY, USA, 2016; Volume 1. [Google Scholar]
- Boggiano, M.M.; Burgess, E.E.; Turan, B.; Soleymani, T.; Daniel, S.; Vinson, L.D.; Lokken, K.L.; Wingo, B.C.; Morse, A. Motives for eating tasty foods associated with binge-eating. Results from a student and a weight-loss seeking population. Appetite 2014, 83, 160–166. [Google Scholar] [CrossRef]
- Boggiano, M.M.; Wenger, L.E.; Burgess, E.E.; Tatum, M.M.; Sylvester, M.D.; Morgan, P.R.; Morse, K.E. Eating tasty foods to cope, enhance reward, socialize or conform: What other psychological characteristics describe each of these motives? J. Health Psychol. 2017, 22, 280–289. [Google Scholar] [CrossRef]
- Bjorlie, K.; Forbush, K.T.; Chapa, D.A.N.; Richson, B.N.; Johnson, S.N.; Fazzino, T.L. Hyper-palatable food consumption during binge-eating episodes: A comparison of intake during binge eating and restricting. Int. J. Eat. Disord. 2022, 55, 688–696. [Google Scholar] [CrossRef]
- Carbone, E.A.; Aloi, M.; Rania, M.; de Filippis, R.; Quirino, D.; Fiorentino, T.V.; Segura-Garcia, C. The relationship of food addiction with binge eating disorder and obesity: A network analysis study. Appetite 2023, 190, 107037. [Google Scholar] [CrossRef]
- Ratkovic, D.; Knezevic, V.; Dickov, A.; Fedrigolli, E.; Comic, M. Comparison of binge-eating disorder and food addiction. J. Int. Med. Res. 2023, 51, 3000605231171016. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; White, M.A.; Potenza, M.N. Binge eating disorder and food addiction. Curr. Drug Abus. Rev. 2011, 4, 201–207. [Google Scholar] [CrossRef]
- Cooper, M.L.; Russell, M.; Skinner, J.B.; Windle, M. Development and validation of a three-dimensional measure of drinking motive. Psychol. Assess. 1992, 4, 123–132. [Google Scholar] [CrossRef]
- Cooper, M.L. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol. Assess. 1994, 6, 117–128. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2023. [Google Scholar]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Mannarini, S.; Fabbricatore, M.; Imperatori, C.; Innamorati, M.; Gearhardt, A.N.; Castelnuovo, G. Structural validity, measurement invariance, reliability and diagnostic accuracy of the Italian version of the Yale Food Addiction Scale 2.0 in patients with severe obesity and the general population. Eat. Weight. Disord. 2021, 26, 345–366. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2022, 15, 104. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Gearhardt, A.N.; Musetti, A.; Castelnuovo, G.; Mannarini, S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients 2023, 15, 1378. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Tagliagambe, A.; Scuderi, A.; Montecchiani, L.; Castelnuovo, G.; Mannarini, S.; Dalla Ragione, L. Many Facets of Eating Disorders: Profiling Key Psychological Features of Anorexia Nervosa and Binge Eating Disorder. Behav. Sci. 2023, 13, 276. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry, Report of a WHO Expert Committee; WHO Technical Report Series 854; World Health Organization: Geneva, Switzerland, 1995.
- Imperatori, C.; Fabbricatore, M.; Lester, D.; Manzoni, G.M.; Castelnuovo, G.; Raimondi, G.; Innamorati, M. Psychometric properties of the modified Yale Food Addiction Scale Version 2.0 in an Italian non-clinical sample. Eat. Weight Disord. 2019, 24, 37–45. [Google Scholar] [CrossRef]
- Ricca, V.; Mannucci, E.; Moretti, S.; Di Bernardo, M.; Zucchi, T.; Cabras, P.L.; Rotella, C.M. Screening for binge eating disorder in obese outpatients. Compr. Psychiatry 2000, 41, 111–115. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Castelnuovo, G.; Mannarini, S. Cognitive Restraint, Uncontrolled Eating, and Emotional Eating. The Italian Version of the Three Factor Eating Questionnaire—Revised 18 (TFEQ-R-18): A Three-step Validation Study. Eat. Weight. Disord. 2024, 29, 16. [Google Scholar] [CrossRef]
- Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Grazing: A different form of food addiction. The Italian version of the Repetitive Eating Questionnaire (Rept(Eat)-Q). Nutrients 2023, in press. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- R Core Team. The R Project for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. [Google Scholar]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Rosseel, Y.; Oberski, D.L.; Byrnes, J.; Vanbrabant, L.; Savalei, V.; Merkle, E.; Hallquist, M.; Rhemtulla, M.; Katsikatsou, M.; Barendse, M.; et al. Package ‘lavaan’; 2017; pp. 1–89. Available online: http://cran.nexr.com/web/packages/lavaan/lavaan.pdf (accessed on 11 January 2024).
- Revelle, W. psych: Procedures for Personality and Psychological Research; Northwestern University: Evanston, IL, USA, 2018. [Google Scholar]
- Revelle, W. psychTools:Tools to Accompany the ‘psych’ Package for Psychological Research; Northwestern University: Evanston, IL, USA, 2020. [Google Scholar]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Epskamp, S. semPlot: Unified Visualizations of Structural Equation Models. Struct. Equ. Model. Multidiscip. J. 2015, 22, 474–483. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Hoyle, R.H. Handbook of Structural Equation Modeling, 2nd ed.; The Guilford Press: New York, NY, USA, 2023. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Yu, C.-Y. Evaluating Cutoff Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes. Doctoral Dissertation, University of California, Los Angeles, CA, USA, 2002. [Google Scholar]
- McDonald, R.P. Test Theory: A Unified Treatment; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1999. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: Harlow, UK, 2014. [Google Scholar]
- Howell, D.C. Statistical Methods for Psychology; Wadsworth, Cengage Learning: Belmont, CA, USA, 2013. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Arexis, M.; Feron, G.; Brindisi, M.C.; Billot, P.E.; Chambaron, S. A scoping review of emotion regulation and inhibition in emotional eating and binge-eating disorder: What about a continuum? J. Eat. Disord. 2023, 11, 197. [Google Scholar] [CrossRef]
- Tonelli, H.; de Siqueira Rotenberg, L. Emotion perception and theory of mind in obesity: A systematic review on the impact of social cognitive deficits on dysfunctional eating behaviors. Surg. Obes. Relat. Dis. 2021, 17, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K.A.; Haynos, A.F. A theoretical review of interpersonal emotion regulation in eating disorders: Enhancing knowledge by bridging interpersonal and affective dysfunction. J. Eat. Disord. 2020, 8, 21. [Google Scholar] [CrossRef]
- Leehr, E.J.; Krohmer, K.; Schag, K.; Dresler, T.; Zipfel, S.; Giel, K.E. Emotion regulation model in binge eating disorder and obesity--a systematic review. Neurosci. Biobehav. Rev. 2015, 49, 125–134. [Google Scholar] [CrossRef]
- Leppanen, J.; Brown, D.; McLinden, H.; Williams, S.; Tchanturia, K. The Role of Emotion Regulation in Eating Disorders: A Network Meta-Analysis Approach. Front. Psychiatry 2022, 13, 793094. [Google Scholar] [CrossRef]
- Prefit, A.B.; Candea, D.M.; Szentagotai-Tatar, A. Emotion regulation across eating pathology: A meta-analysis. Appetite 2019, 143, 104438. [Google Scholar] [CrossRef] [PubMed]
- Giusti, E.M.; Manna, C.; Scolari, A.; Mestre, J.M.; Prevendar, T.; Castelnuovo, G.; Pietrabissa, G. The Relationship between Emotional Intelligence, Obesity and Eating Disorder in Children and Adolescents: A Systematic Mapping Review. Int. J. Environ. Res. Public Health 2021, 18, 2054. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Heatherton, T.F.; Tice, D.M.; Boekaerts, M.; Pintrich, P.R.; Zeidner, M. Losing control: How & why people fail at self-regulation and Handbook of selfregulation. J. Psychiatry Law 2002, 30, 283–284. [Google Scholar]
- Arnow, B.; Kenardy, J.; Agras, W.S. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 1995, 18, 79–90. [Google Scholar] [CrossRef]
- Panzeri, A.; Bettinardi, O.; Bottesi, G.; Bertolotti, G.; Brambatti, L.; Monfredo, M.; Mignemi, G.; Bruno, G.; Vidotto, G.; Spoto, A.; et al. Assessment of perceived support in the context of emergency: Development and validation of the psycho-social support scale. Curr. Psychol. 2023, 42, 22514–22525. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).