Associations between COVID-19 Pandemic-Related Overtime, Perceived Chronic Stress and Burnout Symptoms in German General Practitioners and Practice Personnel—A Prospective Study
Abstract
1. Introduction
1.1. Chronic Stress in General Practice
1.2. Burnout in General Practice
1.3. Sources for Chronic Stress and Burnout
1.4. Mental Health Impact of the COVID-19 Pandemic
1.5. The IMPROVEjob Trial
1.6. Theory, Hypothesis, and Research Question
2. Materials and Methods
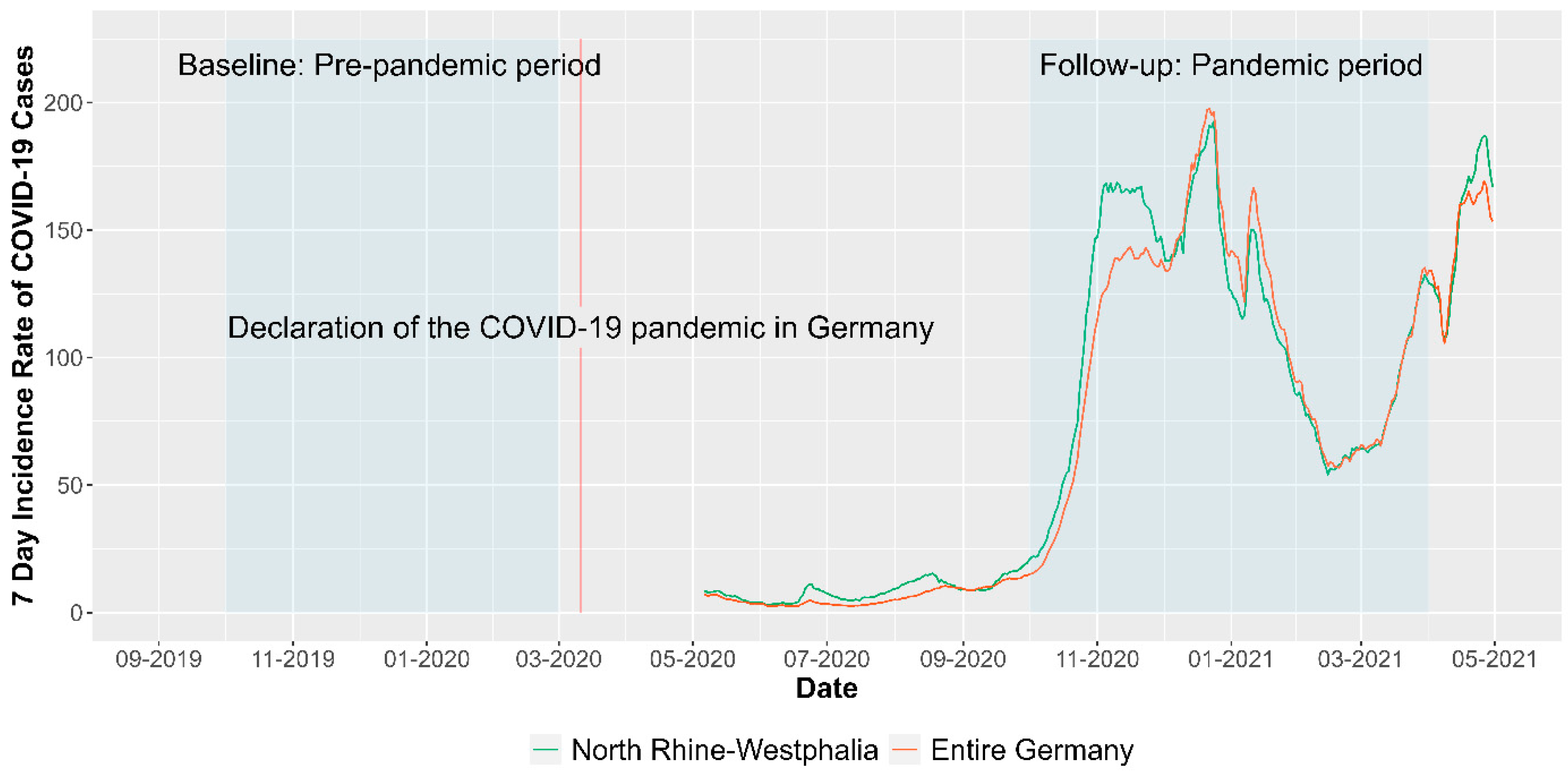
2.1. Study Design and Setting
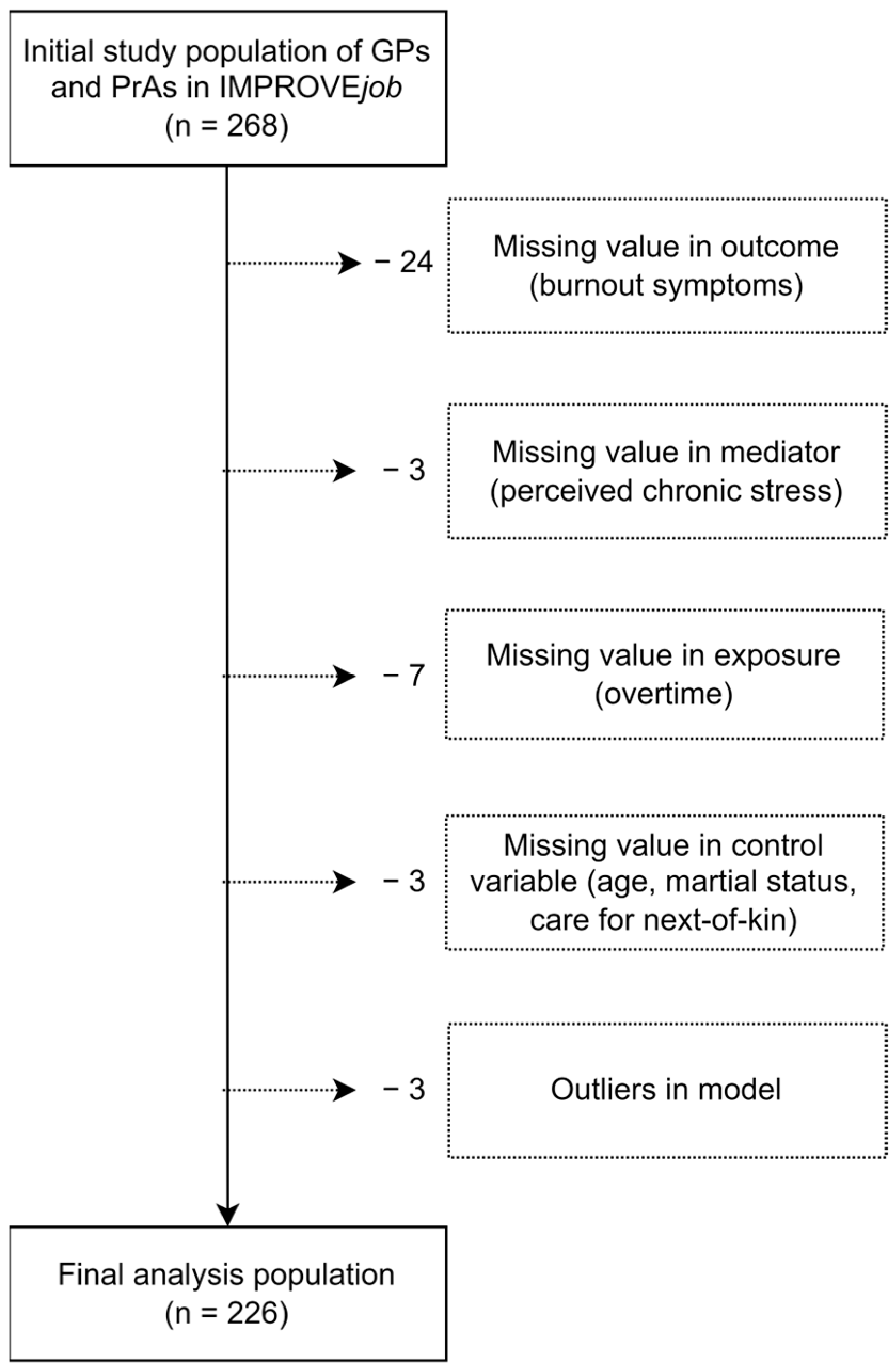
2.2. Recruitment and Analysis Population
2.3. Outcome Variable: Pandemic-Related Changes in Burnout Symptoms
2.4. Independent Variable: Pandemic-Related Changes in Overtime
2.5. Mediator Variable: Pandemic-Related Changes in Perceived Chronic Stress
2.6. Control Variables
| Total Sample (n = 226) | ||
|---|---|---|
| Variable | Mean (SD) | t-Test (p-Value) |
| Overtime (BL) | 1.34 (2.16) | |
| Overtime (FU) | 1.42 (2.16) | |
| Overtime (Δ) | 0.08 (2.26) | 0.5 (0.62) |
| TICS-SSCS (BL) | 19.11 (8) | |
| TICS-SSCS (FU) | 18 (8.42) | |
| TICS-SSCS (Δ) | −1.11 (7.04) | −2.36 (0.02) |
| MBI (BL) | 5.56 (1.99) | |
| MBI (FU) | 5.92 (2.02) | |
| MBI (Δ) | 0.36 (1.79) | 3.04 (0.003) |
2.7. Statistical Analysis
3. Results
3.1. Descriptive Results
3.2. Mediation Analysis of Pandemic-Related Changes in Overtime, Perceived Chronic Stress and Burnout Symptoms
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vancampfort, D.; Koyanagi, A.; Ward, P.B.; Veronese, N.; Carvalho, A.F.; Solmi, M.; Mugisha, J.; Rosenbaum, S.; De Hert, M.; Stubbs, B. Perceived Stress and Its Relationship With Chronic Medical Conditions and Multimorbidity Among 229,293 Community-Dwelling Adults in 44 Low- and Middle-Income Countries. Am. J. Epidemiology 2017, 186, 979–989. [Google Scholar] [CrossRef]
- Hapke, U.; Maske, U.; Scheidt-Nave, C.; Bode, L.; Schlack, R.; Busch, M. Chronischer Stress bei Erwachsenen in Deutschland. Bundesgesundheitsblatt—Gesundheitsforschung—Gesundheitsschutz 2013, 56, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Hussenoeder, F.S.; Conrad, I.; Pabst, A.; Luppa, M.; Stein, J.; Engel, C.; Zachariae, S.; Zeynalova, S.; Yahiaoui-Doktor, M.; Glaesmer, H.; et al. Different Areas of Chronic Stress and Their Associations with Depression. Int. J. Environ. Res. Public Health 2022, 19, 8773. [Google Scholar] [CrossRef]
- Fishta, A.; Backé, E.-M. Psychosocial stress at work and cardiovascular diseases: An overview of systematic reviews. Int. Arch. Occup. Environ. Health 2015, 88, 997–1014. [Google Scholar] [CrossRef] [PubMed]
- Lukan, J.; Bolliger, L.; Pauwels, N.S.; Luštrek, M.; De Bacquer, D.; Clays, E. Work environment risk factors causing day-to-day stress in occupational settings: A systematic review. BMC Public Health 2022, 22, 240. [Google Scholar] [CrossRef] [PubMed]
- Viehmann, A.; Kersting, C.; Thielmann, A.; Weltermann, B. Prevalence of chronic stress in general practitioners and practice assistants: Personal, practice and regional characteristics. PLoS ONE 2017, 12, e0176658. [Google Scholar] [CrossRef]
- Beech, J.; Fraser, C.; Gardner, T.; Buzelli, L.; Williamson, S.; Alderwick, H. Stressed and overworked: What the Commonwealth Fund’s 2022 International Health Policy Survey of Primary Care Physicians in 10 Countries means for the UK; The Health Foundation: London, UK, 2023. [Google Scholar]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- Rosta, J.; Bååthe, F.; Aasland, O.G.; Rø, K.I. Changes in work stress among doctors in Norway from 2010 to 2019: A study based on repeated surveys. BMJ Open 2020, 10, e037474. [Google Scholar] [CrossRef]
- Riley, R.; Spiers, J.; Buszewicz, M.; Taylor, A.K.; Thornton, G.; Chew-Graham, C.A. What are the sources of stress and distress for general practitioners working in England? A qualitative study. BMJ Open 2017, 8, e017361. [Google Scholar] [CrossRef]
- Lee, F.J.; Brown, J.B.; Stewart, M. Exploring family physician stress: Helpful strategies. Can. Fam. Physician 2009, 55, 288–289.e6. [Google Scholar]
- McManus, I.; Winder, B.; Gordon, D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002, 359, 2089–2090. [Google Scholar] [CrossRef]
- WHO News. Burn-Out An “Occupational Phenomenon”: International Classification of Diseases. 2019. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 5 September 2021).
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Karuna, C.; Palmer, V.J.; Scott, A.; Gunn, J. Prevalence of burnout among GPs: A systematic review and meta-analysis. Br. J. Gen. Pract. 2022, 72, e316–e324. [Google Scholar] [CrossRef]
- Soler, J.K.; Yaman, H.; Esteva, M.; Dobbs, F.; Asenova, R.S.; Katić, M.; OžVačIć, Z.; Desgranges, J.P.; Moreau, A.; Lionis, C.; et al. Burnout in European family doctors: The EGPRN study. Fam. Pract. 2008, 25, 245–265. [Google Scholar] [CrossRef]
- Degen, L.; Linden, K.; Seifried-Dübon, T.; Werners, B.; Grot, M.; Rind, E.; Pieper, C.; Eilerts, A.-L.; Schroeder, V.; Kasten, S.; et al. Job Satisfaction and Chronic Stress of General Practitioners and Their Teams: Baseline Data of a Cluster-Randomised Trial (IMPROVEjob). Int. J. Environ. Res. Public Health 2021, 18, 9458. [Google Scholar] [CrossRef]
- Monsalve-Reyes, C.S.; Luis-Costas, C.S.; Gómez-Urquiza, J.L.; Albendín-García, L.; Aguayo, R.; la Fuente, G.A.C.-D. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018, 19, 59. [Google Scholar] [CrossRef]
- Bozorgmehr, A.; Thielmann, A.; Weltermann, B. Chronic stress in practice assistants: An analytic approach comparing four machine learning classifiers with a standard logistic regression model. PLoS ONE 2021, 16, e0250842. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. Journal of applied psychology 2001, 86, 499. [Google Scholar] [CrossRef]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Goetz, K.; Campbell, S.M.; Steinhaeuser, J.; Broge, B.; Willms, S.; Szecsenyi, J. Evaluation of job satisfaction of practice staff and general practitioners: An exploratory study. BMC Fam. Pract. 2011, 12, 137. [Google Scholar] [CrossRef] [PubMed]
- Tuxford, L.M.; Bradley, G.L. Emotional job demands and emotional exhaustion in teachers. Educ. Psychol. 2013, 35, 1006–1024. [Google Scholar] [CrossRef]
- Burr, H.; Berthelsen, H.; Moncada, S.; Nübling, M.; Dupret, E.; Demiral, Y.; Oudyk, J.; Kristensen, T.S.; Llorens, C.; Navarro, A.; et al. The Third Version of the Copenhagen Psychosocial Questionnaire. Saf. Health Work. 2019, 10, 482–503. [Google Scholar] [CrossRef]
- Le Huu, P.; Bellagamba, G.; Bouhadfane, M.; Villa, A.; Lehucher, M.-P. Meta-analysis of effort–reward imbalance prevalence among physicians. Int. Arch. Occup. Environ. Health 2022, 95, 559–571. [Google Scholar] [CrossRef]
- Kersting, C.; Zimmer, L.; Thielmann, A.; Weltermann, B. Chronic stress, work-related daily challenges and medicolegal investigations: A cross-sectional study among German general practitioners. BMC Fam. Pract. 2019, 20, 143. [Google Scholar] [CrossRef]
- Gardner, R.L.; Cooper, E.; Haskell, J.; A Harris, D.; Poplau, S.; Kroth, P.J.; Linzer, M. Physician stress and burnout: The impact of health information technology. J. Am. Med. Inform. Assoc. 2018, 26, 106–114. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General US Population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- Jefferson, L.; Golder, S.; Heathcote, C.; Avila, A.C.; Dale, V.; Essex, H.; Cornelis, C.v.d.F.; McHugh, E.; Moe-Byrne, T.; Bloor, K. GP wellbeing during the COVID-19 pandemic: A systematic review. Br. J. Gen. Pract. 2022, 72, e325–e333. [Google Scholar] [CrossRef]
- Chutiyami, M.; Cheong, A.M.Y.; Salihu, D.; Bello, U.M.; Ndwiga, D.; Maharaj, R.; Naidoo, K.; Kolo, M.A.; Jacob, P.; Chhina, N.; et al. COVID-19 Pandemic and Overall Mental Health of Healthcare Professionals Globally: A Meta-Review of Systematic Reviews. Front. Psychiatry 2022, 12, 804525. [Google Scholar] [CrossRef] [PubMed]
- Phiri, P.; Ramakrishnan, R.; Rathod, S.; Elliot, K.; Thayanandan, T.; Sandle, N.; Haque, N.; Chau, S.W.; Wong, O.W.; Chan, S.S.; et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine 2021, 34, 100806. [Google Scholar] [CrossRef] [PubMed]
- Moro, M.F.; Calamandrei, G.; Poli, R.; Di Mattei, V.; Perra, A.; Kurotschka, P.K.; Restrepo, A.; Romano, F.; La Torre, G.; Preti, E.; et al. The Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Workers in Italy: Analyzing the Role of Individual and Workplace-Level Factors in the Reopening Phase After Lockdown. Front. Psychiatry 2022, 13, 867080. [Google Scholar] [CrossRef] [PubMed]
- KBV Kassenärztliche Bundesvereinigung. CORONA-REPORT/25.11.2020 2020. Available online: https://www.kbv.de/html/corona-report.php (accessed on 9 September 2023).
- Doleman, G.; De Leo, A.; Bloxsome, D. The impact of pandemics on healthcare providers’ workloads: A scoping review. J. Adv. Nurs. 2023, 79, 4434–4454. [Google Scholar] [CrossRef]
- Mause, L.; Hoffmann, J.; Ohnhäuser, T.; Gunkel, S.; Stöcker, A.; Scholten, N. Work climate in pandemic times: Which burdens do German physicians in primary care report? Fam. Pract. 2021, 39, 46–51. [Google Scholar] [CrossRef]
- Werdecker, L.; Esch, T. Burnout, satisfaction and happiness among German general practitioners (GPs): A cross-sectional survey on health resources and stressors. PLoS ONE 2021, 16, e0253447. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Erwin, P.J.; Shanafelt, T.D. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet 2016, 388, 2272–2281. [Google Scholar] [CrossRef]
- Asuero, A.M.; Queraltó, J.M.; Pujol-Ribera, E.; Berenguera, A.; Rodriguez-Blanco, T.; Epstein, R.M. Effectiveness of a Mindfulness Education Program in Primary Health Care Professionals: A Pragmatic Controlled Trial. J. Contin. Educ. Health Prof. 2014, 34, 4–12. [Google Scholar] [CrossRef]
- Council of European Union. Council Directive 89/391/EEC of 12 June 1989 on the introduction of measures to encourage improvements in the safety and health of workers at work, 1989; Council of European Union: Brussel, Belgium, 1989. [Google Scholar]
- Montano, D.; Hoven, H.; Siegrist, J. Effects of organisational-level interventions at work on employees’ health: A systematic review. BMC Public Health. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Nikunlaakso, R.; Laitinen, J. Effectiveness of Workplace Interventions to Improve Health and Well-Being of Health and Social Service Workers: A Narrative Review of Randomised Controlled Trials. Healthcare 2023, 11, 1792. [Google Scholar] [CrossRef]
- Weltermann, B.M.; Kersting, C.; Pieper, C.; Seifried-Dübon, T.; Dreher, A.; Linden, K.; Rind, E.; Ose, C.; Jöckel, K.-H.; Junne, F.; et al. IMPROVEjob—Participatory intervention to improve job satisfaction of general practice teams: A model for structural and behavioural prevention in small and medium-sized enterprises—A study protocol of a cluster-randomised controlled trial. Trials 2020, 21, 532. [Google Scholar] [CrossRef] [PubMed]
- Degen, L.; Göbel, J.; Minder, K.; Seifried-Dübon, T.; Werners, B.; Grot, M.; Rind, E.; Pieper, C.; Eilerts, A.-L.; Schröder, V.; et al. Leadership program with skills training for general practitioners was highly accepted without improving job satisfaction: The cluster randomized IMPROVEjob study. Sci. Rep. 2022, 12, 17869. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch-Institut. 7-Tage-Inzidenz der COVID-19-Fälle in Deutschland: Zenodo 2023; Robert Koch-Institut: Berlin, Germany, 2023. [Google Scholar]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory. In Evaluating Stress: A Book of Resources; Zalaquett, C.P., Wood, R.J., Eds.; Scarecrow Education: Lanham, MI, USA, 1997. [Google Scholar]
- Kotsopoulos, D.; Bardaki, C.; Papaioannou, T.G. Determinants of Employees’ Personal and Collective Energy Consumption and Conservation at Work. Sustainability 2023, 15, 4913. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Sloan, J.A.; Shanafelt, T.D. Single Item Measures of Emotional Exhaustion and Depersonalization Are Useful for Assessing Burnout in Medical Professionals. J. Gen. Intern. Med. 2009, 24, 1318–1321. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Satele, D.V.; Sloan, J.A.; Shanafelt, T.D. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J. Gen. Intern. Med. 2012, 27, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Schulz, P.; Schlotz, W. Trierer Inventar zur Erfassung von chronischem Streß (TICS): Skalenkonstruktion, teststatistische Überprüfung und Validierung der Skala Arbeitsüberlastung. Diagnostica 1999, 45, 8–19. [Google Scholar] [CrossRef]
- Schulz, P.; Schlotz, W.; Becker, P. Trierer Inventar zum Chronischen Stress (TICS) [Trier Inventory for Chronic Stress (TICS)]; Hogrefe: Göttingen, Germany, 2004. [Google Scholar]
- Göbel, J.; Schmidt, M.; Seifried-Dübon, T.; Linden, K.; Degen, L.; Rind, E.; Eilerts, A.-L.; Pieper, C.; Grot, M.; Werners, B.; et al. Higher Work-Privacy Conflict and Lower Job Satisfaction in GP Leaders and Practice Assistants Working Full-Time Compared to Part-Time: Results of the IMPROVEjob Study. Int. J. Environ. Res. Public Health 2022, 19, 2618. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, A.V.; White, H.R.; Howell-White, S. Becoming Married and Mental Health: A Longitudinal Study of a Cohort of Young Adults. J. Marriage Fam. 1996, 58, 895. [Google Scholar] [CrossRef]
- Alves, L.C.d.S.; Monteiro, D.Q.; Bento, S.R.; Hayashi, V.D.; Pelegrini, L.N.d.C.; Vale, F.A.C. Burnout syndrome in informal caregivers of older adults with dementia: A systematic review. Dement. Neuropsychol. 2019, 13, 415–421. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013; ISBN 1609182308. [Google Scholar]
- Davidson, R.; MacKinnon, J.G. Estimation and Inference in Econometrics; Oxford University Press: New York, NY, Oxford, 1993; ISBN 9780195060119. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Feng, J.; Jiang, H.; Shen, X.; Lei, Z.; Li, L.; Zhu, Y.; Zhang, M.; Yang, T.; Meng, X.; Di, H.; et al. Occupational stress and associated factors among general practitioners in China: A national cross-sectional study. BMC Public Health 2022, 22, 1061. [Google Scholar] [CrossRef]
- Núñez-Elvira, A. Trends and determinants of GPs’ work hours in the UK: A quantitative study. BJGP Open 2023, 7. [Google Scholar] [CrossRef]
- Leutgeb, R.; Frankenhauser-Mannuß, J.; Scheuer, M.; Szecsenyi, J.; Goetz, K. Job satisfaction and stressors for working in out-of-hours care—A pilot study with general practitioners in a rural area of Germany. BMC Fam. Pract. 2018, 19, 95. [Google Scholar] [CrossRef]
- Koch, K.; Miksch, A.; Schürmann, C.; Joos, S.; Sawicki, P.T. The German Health Care System in International Comparison. Dtsch. Aerzteblatt Online 2011, 108, 255–261. [Google Scholar] [CrossRef]
- Kramer, V.; Papazova, I.; Thoma, A.; Kunz, M.; Falkai, P.; Schneider-Axmann, T.; Hierundar, A.; Wagner, E.; Hasan, A. Subjective burden and perspectives of German healthcare workers during the COVID-19 pandemic. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 271, 271–281. [Google Scholar] [CrossRef]
- Linzer, M.; Poplau, S.; Babbott, S.; Collins, T.; Guzman-Corrales, L.; Menk, J.; Murphy, M.L.; Ovington, K. Worklife and Wellness in Academic General Internal Medicine: Results from a National Survey. J. Gen. Intern. Med. 2016, 31, 1004–1010. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; West, C.P.; Dyrbye, L.N.; Trockel, M.; Tutty, M.; Wang, H.; Carlasare, L.E.; Sinsky, C. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic. Mayo Clin. Proc. 2022, 97, 2248–2258. [Google Scholar] [CrossRef] [PubMed]
- Sinsky, C.A.; Shanafelt, T.D.; Dyrbye, L.N.; Sabety, A.H.; Carlasare, L.E.; West, C.P. Health Care Expenditures Attributable to Primary Care Physician Overall and Burnout-Related Turnover: A Cross-sectional Analysis. Mayo Clin. Proc. 2022, 97, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Jiang, H.; Xu, H.; Ye, J.; Lv, C.; Lu, Z.; Gan, Y. The global prevalence of turnover intention among general practitioners: A systematic review and meta-analysis. BMC Fam. Pract. 2020, 21, 246. [Google Scholar] [CrossRef] [PubMed]
- Amanullah, S.; Shankar, R.R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthcare 2020, 8, 421. [Google Scholar] [CrossRef] [PubMed]
- Macaron, M.M.; Segun-Omosehin, O.A.; Matar, R.H.; Beran, A.; Nakanishi, H.; Than, C.A.; Abulseoud, O.A. A systematic review and meta analysis on burnout in physicians during the COVID-19 pandemic: A hidden healthcare crisis. Front. Psychiatry 2023, 13, 1071397. [Google Scholar] [CrossRef] [PubMed]
- Alarcon, G.; Eschleman, K.J.; Bowling, N.A. Relationships between personality variables and burnout: A meta-analysis. Work. Stress 2009, 23, 244–263. [Google Scholar] [CrossRef]
- Jiménez-Fernández, R.; Corral-Liria, I.; Trevissón-Redondo, B.; Lopez-Lopez, D.; Losa-Iglesias, M.; Becerro-De-Bengoa-Vallejo, R. Burnout, resilience and psychological flexibility in frontline nurses during the acute phase of the COVID-19 pandemic (2020) in Madrid, Spain. J. Nurs. Manag. 2022, 30, 2549–2556. [Google Scholar] [CrossRef]
- M. Blanch, J.; Ochoa, P.; Fernanda Caballero, M. Over Engagement, Protective or Risk Factor of Burnout? In Sustainable Management Practices; Sarfraz, M., Ibrahim Adbullah, M., Rauf, A., Ghulam Meran Shah, S., Eds.; IntechOpen: London, UK, 2019; ISBN 978-1-78985-153-3. [Google Scholar]
- Mangory, K.Y.; Ali, L.Y.; Rø, K.I.; Tyssen, R. Effect of burnout among physicians on observed adverse patient outcomes: A literature review. BMC Health Serv. Res. 2021, 21, 369. [Google Scholar] [CrossRef]
- Han, S.; Shanafelt, T.D.; Sinsky, C.A.; Awad, K.M.; Dyrbye, L.N.; Fiscus, L.C.; Trockel, M.; Goh, J. Estimating the Attributable Cost of Physician Burnout in the United States. Ann. Intern. Med. 2019, 170, 784–790. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Noseworthy, J.H. Executive Leadership and Physician Well-being. Mayo Clin. Proc. 2016, 92, 129–146. [Google Scholar] [CrossRef]
- Papp, M.; Kőrösi, L.; Sándor, J.; Nagy, C.; Juhász, A.; Ádány, R. Workforce crisis in primary healthcare worldwide: Hungarian example in a longitudinal follow-up study. BMJ Open 2019, 9, e024957. [Google Scholar] [CrossRef]
- Bussche, H.v.D. The future problems of general practice in Germany: Current trends and necessary measures. Bundesgesundheitsblatt—Gesundheitsforschung—Gesundheitsschutz 2019, 62, 1129–1137. [Google Scholar] [CrossRef]
- Wangler, J.; Jansky, M. How can primary care be secured in the long term?—A qualitative study from the perspective of general practitioners in Germany. Eur. J. Gen. Pract. 2023, 29, 2223928. [Google Scholar] [CrossRef]
- Stierli, R.; Rozsnyai, Z.; Felber, R.; Jörg, R.; Kraft, E.; Exadaktylos, A.K.; Streit, S. Primary Care Physician Workforce 2020 to 2025—A cross-sectional study for the Canton of Bern. Swiss Med. Wkly. 2021, 151, w30024. [Google Scholar] [CrossRef] [PubMed]
- Le Floch, B.; Bastiaens, H.; Le Reste, J.Y.; Lingner, H.; Hoffman, R.; Czachowski, S.; Assenova, R.; Koskela, T.H.; Klemenc-Ketis, Z.; Nabbe, P.; et al. Which positive factors give general practitioners job satisfaction and make general practice a rewarding career? A European multicentric qualitative research by the European general practice research network. BMC Fam. Pract. 2019, 20, 96. [Google Scholar] [CrossRef] [PubMed]
- Van Ham, I.; Verhoeven, A.A.H.; Groenier, K.H.; Groothoff, J.W.; De Haan, J. Job satisfaction among general practitioners: A systematic literature review. Eur. J. Gen. Pract. 2006, 12, 174–180. [Google Scholar] [CrossRef] [PubMed]


| Total Sample (n = 226) | |
|---|---|
| Variable | |
| Female, n (%) | 196 (86.7) |
| Age in years, mean (SD) | 45 (12) |
| General practice assistants, n (%) | 158 (69.9) |
| Working full-time, n (%) | 123 (54.4) |
| Living in a relationship/married, n (%) | 183 (81.0) |
| Care for next-of-kin, n (%) | 48 (21.2) |
| Control group, n (%) | 119 (52.7) |
| Total Sample (n = 226) | GPs (n = 68) | PrAs (n = 158) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | |
| Total Effect | 0.13 | 0.03, 0.23 | 0.05 | −0.16, 0.26 | 0.34 | 0.12, 0.57 |
| Direct Effect | 0.02 | −0.08, 0.12 | −0.03 | −0.29, 0.23 | 0.17 | −0.05, 0.38 |
| Indirect Effect | 0.11 | 0.06, 0.19 | 0.08 | 0.01, 0.17 | 0.17 | 0.08, 0.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Küppers, L.; Göbel, J.; Aretz, B.; Rieger, M.A.; Weltermann, B. Associations between COVID-19 Pandemic-Related Overtime, Perceived Chronic Stress and Burnout Symptoms in German General Practitioners and Practice Personnel—A Prospective Study. Healthcare 2024, 12, 479. https://doi.org/10.3390/healthcare12040479
Küppers L, Göbel J, Aretz B, Rieger MA, Weltermann B. Associations between COVID-19 Pandemic-Related Overtime, Perceived Chronic Stress and Burnout Symptoms in German General Practitioners and Practice Personnel—A Prospective Study. Healthcare. 2024; 12(4):479. https://doi.org/10.3390/healthcare12040479
Chicago/Turabian StyleKüppers, Lucas, Julian Göbel, Benjamin Aretz, Monika A. Rieger, and Birgitta Weltermann. 2024. "Associations between COVID-19 Pandemic-Related Overtime, Perceived Chronic Stress and Burnout Symptoms in German General Practitioners and Practice Personnel—A Prospective Study" Healthcare 12, no. 4: 479. https://doi.org/10.3390/healthcare12040479
APA StyleKüppers, L., Göbel, J., Aretz, B., Rieger, M. A., & Weltermann, B. (2024). Associations between COVID-19 Pandemic-Related Overtime, Perceived Chronic Stress and Burnout Symptoms in German General Practitioners and Practice Personnel—A Prospective Study. Healthcare, 12(4), 479. https://doi.org/10.3390/healthcare12040479


_Rachiotis.png)



