Impact of the Italian Healthcare Outcomes Program (PNE) on the Care Quality of the Poorest Performing Hospitals
Abstract
1. Introduction
2. Materials and Methods
2.1. PNE Characteristics and Methodology
- RR > 1.00 and p < 0.05 (poor performance—the patients treated by this hospital had a higher likelihood of death than the average Italian patient, and the results are significant, indicating a low level of uncertainty);
- RR > 1.00 and p ≥ 0.05 (poor performance, uncertain—the patients treated by this hospital had a higher likelihood of death than the average Italian patient, but the results are not significant);
- RR ≤ 1.00 and p ≥ 0.05 (high performance, uncertain—the patients treated by this hospital had an equal or lower likelihood of death than the average Italian patient, but the results are not significant);
- RR ≤ 1.00 and p < 0.05 (high performance—the patients treated by this hospital had an equal or lower likelihood of death than the average Italian patient, and the results are significant).
2.2. Study Methods
- Acute myocardial infarction (AMI);
- Congestive heart failure (CHF);
- Stroke;
- Chronic obstructive pulmonary disease (COPD);
- Chronic kidney disease (CKD);
- Femur fracture;
- Lung cancer;
- Colon cancer.
- (a)
- The adjusted RR remained ≥ 1.30, with a p < 0.05;
- (b)
- The adjusted RR remained ≥ 1.30, but the p-value became equal or higher than 0.05;
- (c)
- The adjusted RR decreased below 1.30, but remained higher than 1.00, regardless of the p-value;
- (d)
- The adjusted RR decreased below (or was equal to) 1.00, but the p-value was ≥ 0.05;
- (e)
- The adjusted RR decreased below (or was equal to) 1.00, with a p < 0.05.
2.3. Data Analysis
3. Results
3.1. Overall Performance Variation
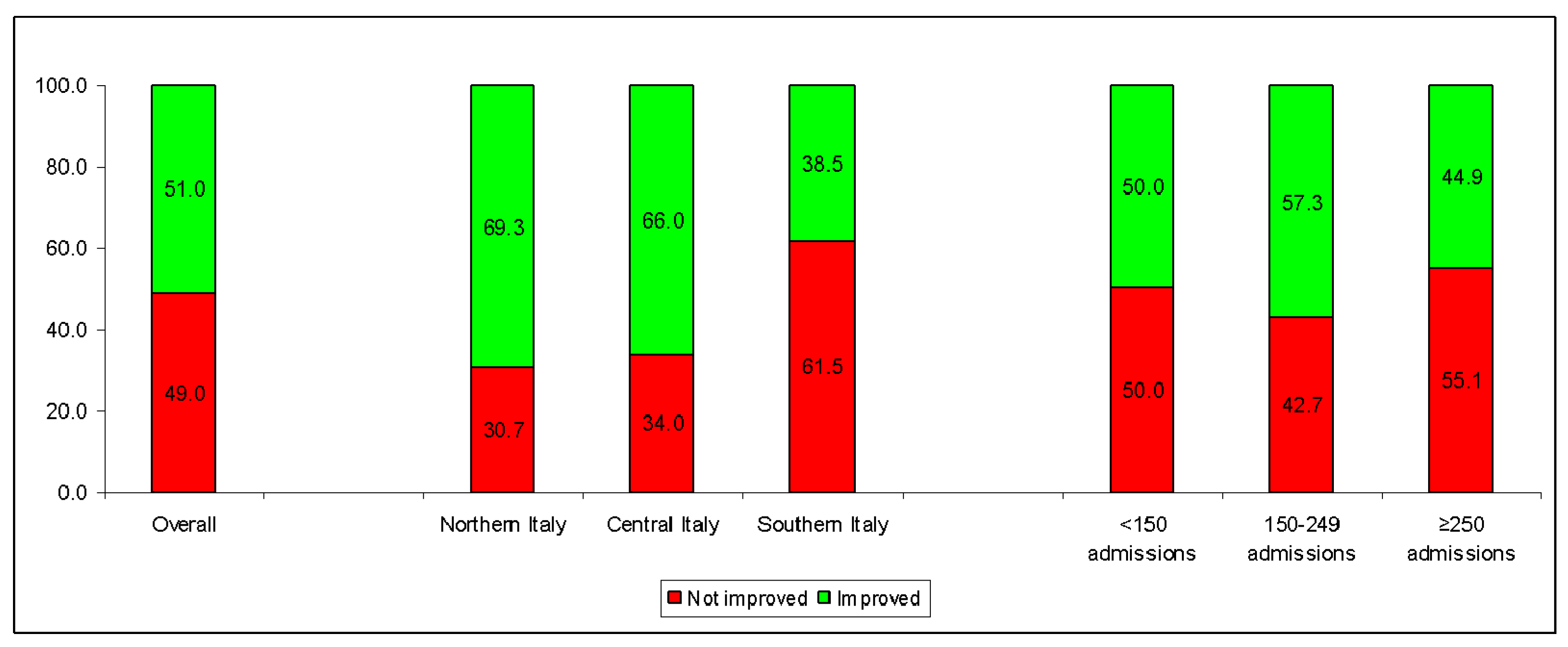
3.2. Performance by Disease, Geographical Area and Hospital Volumes
3.3. Multivariate and Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Health System Performance Assessment. Available online: https://www.who.int/publications-detail-redirect/9789240042476 (accessed on 26 November 2023).
- Braithwaite, J.; Hibbert, P.; Blakely, B.; Plumb, J.; Hannaford, N.; Long, J.C.; Marks, D. Health system frameworks and performance indicators in eight countries: A comparative international analysis. SAGE Open Med. 2017, 5, 2050312116686516. [Google Scholar] [CrossRef]
- Renee Rutter, S.; Park, S.H. Relationship between Hospital Characteristics and Value-Based Program Measure Performance: A Literature Review. West. J. Nurs. Res. 2020, 42, 1010–1021. [Google Scholar] [CrossRef] [PubMed]
- England NHS. Clinical Commissioning Group Outcomes Indicators Set—October 2020. 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/ccg-outcomes-indicator-set/october-2020 (accessed on 5 February 2024).
- Australian Institute of Health and Welfare. Australia’s Health Performance Framework. Available online: https://www.aihw.gov.au/reports-data/australias-health-performance/australias-health-performance-framework (accessed on 31 January 2024).
- Milstein, R.; Schreyoegg, J. Pay for performance in the inpatient sector: A review of 34 P4P programs in 14 OECD countries. Health Policy 2016, 120, 1125–1140. [Google Scholar] [CrossRef]
- AGENAS. PNE—Programma Nazionale Esiti. Available online: https://pne.agenas.it/home (accessed on 26 November 2023).
- AGENAS. Archivio Monitor ANNO 2018—Agenas.gov.it. Available online: https://www.agenas.gov.it/comunicazione/114-archivio-monitor/164-archivio-monitor-anno-2018 (accessed on 18 December 2023).
- AGENAS. Obiettivi PNE: Attivita’ di Audit. Available online: https://www.agenas.gov.it/aree-tematiche/qualita-e-sicurezza/accreditamento?view=article&id=1146:obiettivi-pne-attivita-di-audit&catid=90 (accessed on 26 November 2023).
- AGENAS. Programma Nazionale Esiti—Metodi Statistici. Available online: https://pne.agenas.it/assets/documentation/fonti_metodi/metodi.pdf (accessed on 26 November 2023).
- Pinnarelli, L.; Nuti, S.; Sorge, C.; Davoli, M.; Fusco, D.; Agabiti, N.; Vainieri, M.; Perucci, C.A. What drives hospital performance? The impact of comparative outcome evaluation of patients admitted for hip fracture in two Italian regions. BMJ Qual. Saf. 2012, 21, 127–134. [Google Scholar] [CrossRef]
- Colais, P.; Pinnarelli, L.; Mataloni, F.; Giordani, B.; Duranti, G.; D’Errigo, P.; Rosato, S.; Seccareccia, F.; Baglio, G.; Davoli, M. The National Outcomes Evaluation Programme in Italy: The Impact of Publication of Health Indicators. Int. J. Environ. Res. Public. Health 2022, 19, 1685. [Google Scholar] [CrossRef]
- AGENAS. PNE—Programma Nazionale Esiti. pne.agenas.it. Available online: https://pne.agenas.it/ospedaliera/indicatori (accessed on 19 December 2023).
- Italy’s Health Performance, 1990–2017: Findings from the Global Burden of Disease Study 2017. Lancet Public Health 2019, 4, e645–e657. [CrossRef] [PubMed]
- Øvretveit, J.; Gustafson, D. Evaluation of quality improvement programmes. Qual. Saf. Health Care 2002, 11, 270–275. [Google Scholar] [CrossRef]
- Italian Ministry of Health. The Clinical Audit. Available online: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?id=1552 (accessed on 31 January 2024).
- Italian Ministry of Health. Guidelines and Recommendations. Available online: https://www.salute.gov.it/portale/sicurezzaCure/menuContenutoSicurezzaCure.jsp?lingua=italiano&area=qualita&menu=lineeguida (accessed on 31 January 2024).
- Connor, L.; Dean, J.; McNett, M.; Tydings, D.M.; Shrout, A.; Gorsuch, P.F.; Hole, A.; Moore, L.; Brown, R.; Melnyk, B.M.; et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid. Based Nurs. 2023, 20, 6–15. [Google Scholar] [CrossRef]
- Withanachchi, N.; Uchida, Y.; Nanayakkara, S.; Samaranayake, D.; Okitsu, A. Resource allocation in public hospitals: Is it effective? Health Policy 2007, 80, 308–313. [Google Scholar] [CrossRef]
- Langiano, T.; Martin, S.J. Quality improvement measures adopted by the Italian National Health Service. Int. J. Artif. Organs 1998, 21, 726–729. [Google Scholar] [CrossRef]
- Salampessy, B.H.; Portrait, F.R.M.; van der Hijden, E.; Klink, A.; Koolman, X. On the correlation between outcome indicators and the structure and process indicators used to proxy them in public health care reporting. Eur. J. Health Econ. 2021, 22, 1239–1251. [Google Scholar] [CrossRef] [PubMed]
- Barclay, M.E.; Dixon-Woods, M.; Lyratzopoulos, G. Concordance of Hospital Ranks and Category Ratings Using the Current Technical Specification of US Hospital Star Ratings and Reasonable Alternative Specifications. JAMA Health Forum 2022, 3, e221006. [Google Scholar] [CrossRef]
- Eldridge, N.; Wang, Y.; Metersky, M.; Eckenrode, S.; Mathew, J.; Sonnenfeld, N.; Perdue-Puli, J.; Hunt, D.; Brady, P.J.; McGann, P.; et al. Trends in Adverse Event Rates in Hospitalized Patients, 2010–2019. JAMA 2022, 328, 173–183. [Google Scholar] [CrossRef]
- Kaye, D.R.; Norton, E.C.; Ellimoottil, C.; Ye, Z.; Dupree, J.M.; Herrel, L.A.; Miller, D.C. Understanding the relationship between the Centers for Medicare and Medicaid Services’ Hospital Compare star rating, surgical case volume, and short-term outcomes after major cancer surgery. Cancer 2017, 123, 4259–4267. [Google Scholar] [CrossRef]
- Wang, Y.; Eldridge, N.; Metersky, M.L.; Sonnenfeld, N.; Fine, J.M.; Pandolfi, M.M.; Eckenrode, S.; Bakullari, A.; Galusha, D.H.; Jaser, L.; et al. Association Between Hospital Performance on Patient Safety and 30-Day Mortality and Unplanned Readmission for Medicare Fee-for-Service Patients With Acute Myocardial Infarction. J. Am. Heart Assoc. 2016, 5, e003731. [Google Scholar] [CrossRef]
- Pross, C.; Busse, R.; Geissler, A. Hospital quality variation matters—A time-trend and cross-section analysis of outcomes in German hospitals from 2006 to 2014. Health Policy 2017, 121, 842–852. [Google Scholar] [CrossRef]
- Klein, S.; Rauh, J.; Pauletzki, J.; Klakow-Franck, R.; Zander-Jentsch, B. Introduction of quality indicators in German hospital capacity planning—Do results show an improvement in quality? Health Policy 2023, 133, 104830. [Google Scholar] [CrossRef]
- Chang, S.J.; Hsiao, H.C.; Huang, L.H.; Chang, H. Taiwan quality indicator project and hospital productivity growth. Omega 2011, 39, 14–22. [Google Scholar] [CrossRef]
- Aghaei Hashjin, A.; Kringos, D.S.; Manoochehri, J.; Aryankhesal, A.; Klazinga, N.S. Development and impact of the Iranian hospital performance measurement program. BMC Health Serv. Res. 2014, 14, 448. [Google Scholar] [CrossRef][Green Version]
- Waters, T.M.; Burns, N.; Kaplan, C.M.; Graetz, I.; Benitez, J.; Cardarelli, R.; Daniels, M.J. Combined impact of Medicare’s hospital pay for performance programs on quality and safety outcomes is mixed. BMC Health Serv. Res. 2022, 22, 958. [Google Scholar] [CrossRef]
- Kahn, C.N., 3rd; Rhodes, K.; Pal, S.; McBride, T.J.; May, D.; DaVanzo, J.E.; Dobson, A. CMS Hospital Value-Based Programs: Refinements Are Needed To Reduce Health Disparities And Improve Outcomes. Health Aff. 2023, 42, 928–936. [Google Scholar] [CrossRef]
- Cavalieri, M.; Gitto, L.; Guccio, C. Reimbursement systems and quality of hospital care: An empirical analysis for Italy. Health Policy 2013, 111, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Mathes, T.; Pieper, D.; Morche, J.; Polus, S.; Jaschinski, T.; Eikermann, M. Pay for performance for hospitals. Cochrane Database Syst. Rev. 2019, 7, Cd011156. [Google Scholar] [CrossRef]
- Garattini, L.; Zanetti, M.; Freemantle, N. The Italian NHS: What Lessons to Draw from COVID-19? Appl. Health Econ. Health Policy 2020, 18, 463–466. [Google Scholar] [CrossRef]
- Toth, F. How health care regionalisation in Italy is widening the North-South gap. Health Econ. Policy Law. 2014, 9, 231–249. [Google Scholar] [CrossRef] [PubMed]
- Franzini, L.; Giannoni, M. Determinants of health disparities between Italian regions. BMC Public Health 2010, 10, 296. [Google Scholar] [CrossRef]
- Maio, V.; Manzoli, L. The Italian Health Care System: WHO ranking versus public perception. P&T 2002, 27, 301–308. [Google Scholar]
- Mesman, R.; Westert, G.P.; Berden, B.J.; Faber, M.J. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume-outcome relationships. Health Policy 2015, 119, 1055–1067. [Google Scholar] [CrossRef]
- Amato, L.; Fusco, D.; Acampora, A.; Bontempi, K.; Rosa, A.C.; Colais, P.; Cruciani, F.; D’Ovidio, M.; Mataloni, F.; Minozzi, S.; et al. Volume and health outcomes: Evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol. Prev. 2017, 41 (Suppl. S2), 1–128. [Google Scholar] [CrossRef]
| All Outcomes | AMI | CHF | Stroke | COPD | CKD | Femur Fracture | Colon Cancer | Lung Cancer | |
|---|---|---|---|---|---|---|---|---|---|
| n = 288 | n = 28 | n = 72 | n = 32 | n = 36 | n = 68 | n = 30 | n = 16 | n = 6 | |
| % | % | % | % | % | % | % | % | % | |
| Overall performance | |||||||||
| Improved | 51.0 | 67.9 | 44.4 | 53.1 | 44.4 | 42.6 | 66.7 | 81.2 | 16.7 |
| 23.6 | 32.1 | 25.0 | 21.9 | 13.9 | 20.6 | 30.0 | 37.5 | 0.0 |
| 25.0 | 28.6 | 16.7 | 28.1 | 30.6 | 19.1 | 36.7 | 43.8 | 16.7 |
| 2.4 | 7.1 | 2.8 | 3.1 | 0.0 | 2.9 | 0.0 | 0.0 | 0.0 |
| Did not improve | 49.0 | 32.1 | 55.6 | 46.9 | 55.6 | 57.4 | 33.3 | 18.8 | 83.3 |
| 34.7 | 17.9 | 34.7 | 25.0 | 44.4 | 52.9 | 23.3 | 12.5 | 16.7 |
| 14.2 | 14.3 | 20.8 | 21.9 | 11.1 | 4.4 | 10.0 | 6.3 | 66.7 |
| aRR ≥ 1.30, p < 0.05 | aRR ≥ 1.30, p ≥ 0.05 | 1 < aRR < 1.30 | aRR ≤ 1.00, p ≥ 0.05 | aRR < 1.00, p < 0.05 | |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | % (n) | |
| Geographical area | |||||
| 17.3 (13) | 13.3 (10) | 28.0 (21) | 40.0 (30) | 1.3 (1) |
| 27.7 (13) | 6.4 (3) | 19.2 (9) | 36.2 (17) | 10.6 (5) |
| 44.6 (74) | 16.9 (28) | 22.9 (38) | 15.1 (25) | 0.6 (1) |
| N. of hospital admissions ** in 2016 | |||||
| <150 | 35.4 (34) | 14.6 (14) | 18.8 (18) | 29.2 (28) | 2.1 (2) |
| 150–249 | 26.2 (27) | 16.5 (17) | 25.2 (26) | 29.1 (30) | 2.9 (3) |
| ≥250 | 43.8 (39) | 11.2 (10) | 27.0 (24) | 15.7 (14) | 2.3 (2) |
| Regions | Not Improved | Total |
|---|---|---|
| % (n) | n | |
| Piemonte | 21.1 | 19 |
| Liguria | 0.0 | 8 |
| Lombardia | 36.8 | 19 |
| Veneto | 50.0 | 14 |
| Friuli Venezia Giulia | 50.0 | 4 |
| Emilia Romagna | 27.3 | 11 |
| Toscana | 21.4 | 14 |
| Umbria | - | - |
| Marche | 20.0 | 5 |
| Lazio | 42.9 | 28 |
| Abruzzo | 58.3 | 12 |
| Molise | 50.0 | 6 |
| Basilicata | 40.0 | 5 |
| Campania | 68.0 | 50 |
| Calabria | 58.8 | 17 |
| Puglia | 62.2 | 39 |
| Sicilia | 68.8 | 32 |
| Sardegna | 14.3 | 7 |
| Total (Italy) | 49.0 | 288 |
| OR | (95% CI) | p | |
|---|---|---|---|
| Geographical area | |||
| 1 (Ref. cat.) | -- | -- |
| 3.37 | (1.86–6.11) | <0.001 |
| 3.28 | (1.63–6.61) | 0.001 |
| N. of hospital admissions in the year 2016, 20-admission increase | 0.49 | (0.29–0.83) | 0.008 |
| Adjusted RR in the year 2016, 1-unit increase | 0.94 | (0.91–0.98) | 0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiore, M.; Bianconi, A.; Acuti Martellucci, C.; Rosso, A.; Zauli, E.; Flacco, M.E.; Manzoli, L. Impact of the Italian Healthcare Outcomes Program (PNE) on the Care Quality of the Poorest Performing Hospitals. Healthcare 2024, 12, 431. https://doi.org/10.3390/healthcare12040431
Fiore M, Bianconi A, Acuti Martellucci C, Rosso A, Zauli E, Flacco ME, Manzoli L. Impact of the Italian Healthcare Outcomes Program (PNE) on the Care Quality of the Poorest Performing Hospitals. Healthcare. 2024; 12(4):431. https://doi.org/10.3390/healthcare12040431
Chicago/Turabian StyleFiore, Matteo, Alessandro Bianconi, Cecilia Acuti Martellucci, Annalisa Rosso, Enrico Zauli, Maria Elena Flacco, and Lamberto Manzoli. 2024. "Impact of the Italian Healthcare Outcomes Program (PNE) on the Care Quality of the Poorest Performing Hospitals" Healthcare 12, no. 4: 431. https://doi.org/10.3390/healthcare12040431
APA StyleFiore, M., Bianconi, A., Acuti Martellucci, C., Rosso, A., Zauli, E., Flacco, M. E., & Manzoli, L. (2024). Impact of the Italian Healthcare Outcomes Program (PNE) on the Care Quality of the Poorest Performing Hospitals. Healthcare, 12(4), 431. https://doi.org/10.3390/healthcare12040431







