The Mental Wellbeing of Child and Adolescent Mental Health Service (CAMHS) Workers in England: A Cross-Sectional Descriptive Study Reporting Levels of Burnout, Wellbeing and Job Satisfaction
Abstract
1. Introduction
Objectives of the Current Study
- (1)
- Assess the levels of staff burnout, wellbeing, and job satisfaction experienced in one UK CAMH service and how these are interrelated.
- (2)
- Explore whether they differ by demographic and work-related factors (i.e., sex, age, clinical vs. non-clinical professional role, and working pattern).
2. Materials and Methods
2.1. Recruitment
2.2. Measures
2.2.1. The Copenhagen Burnout Inventory (CBI)
2.2.2. Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS)
2.2.3. Short Index of Job Satisfaction (SIJS)
2.3. Data Analysis
3. Results
3.1. Participants
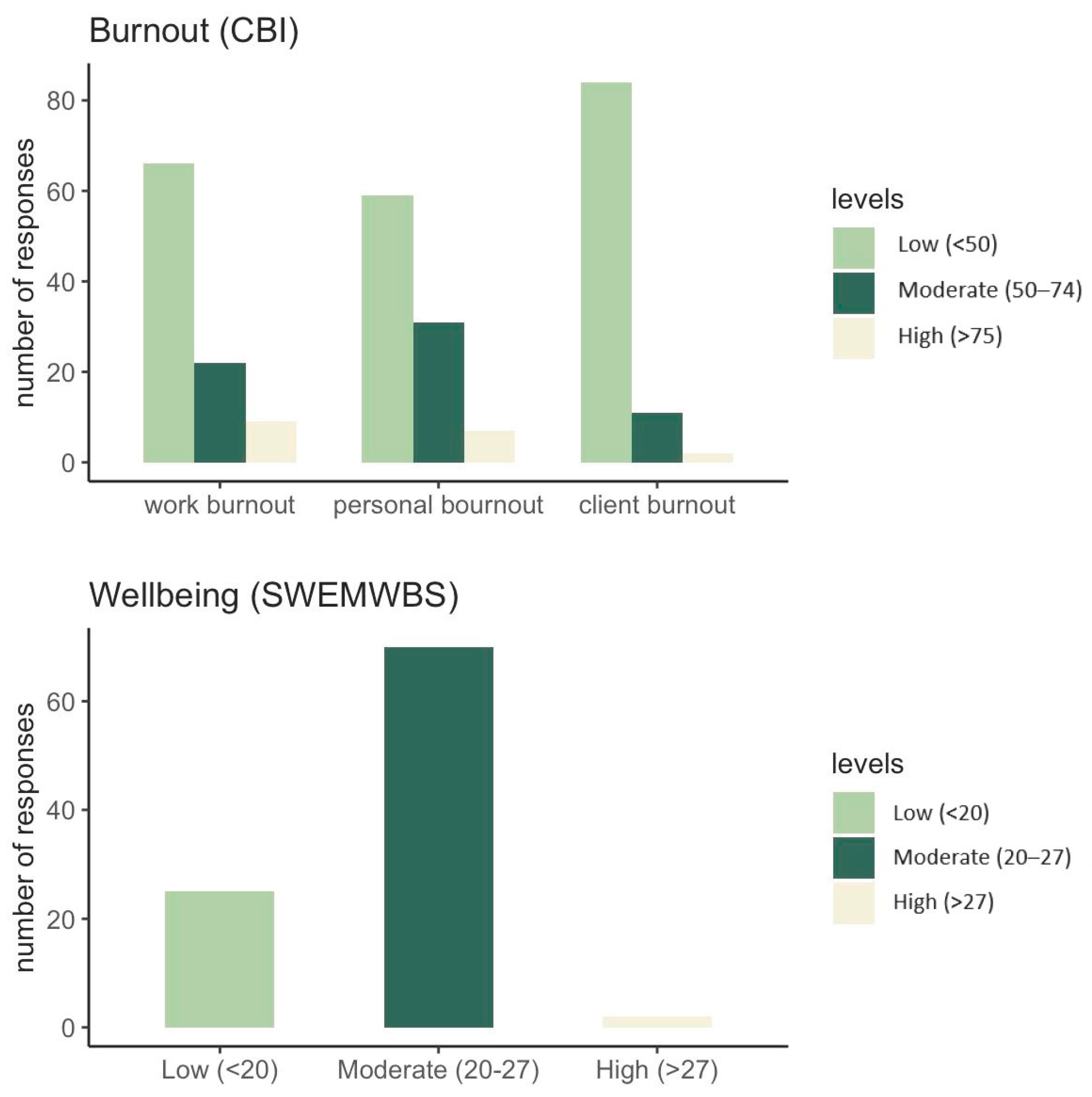
3.2. Copenhagen Burnout Inventory (CBI)
3.3. SWEMWBS
3.4. SIJS
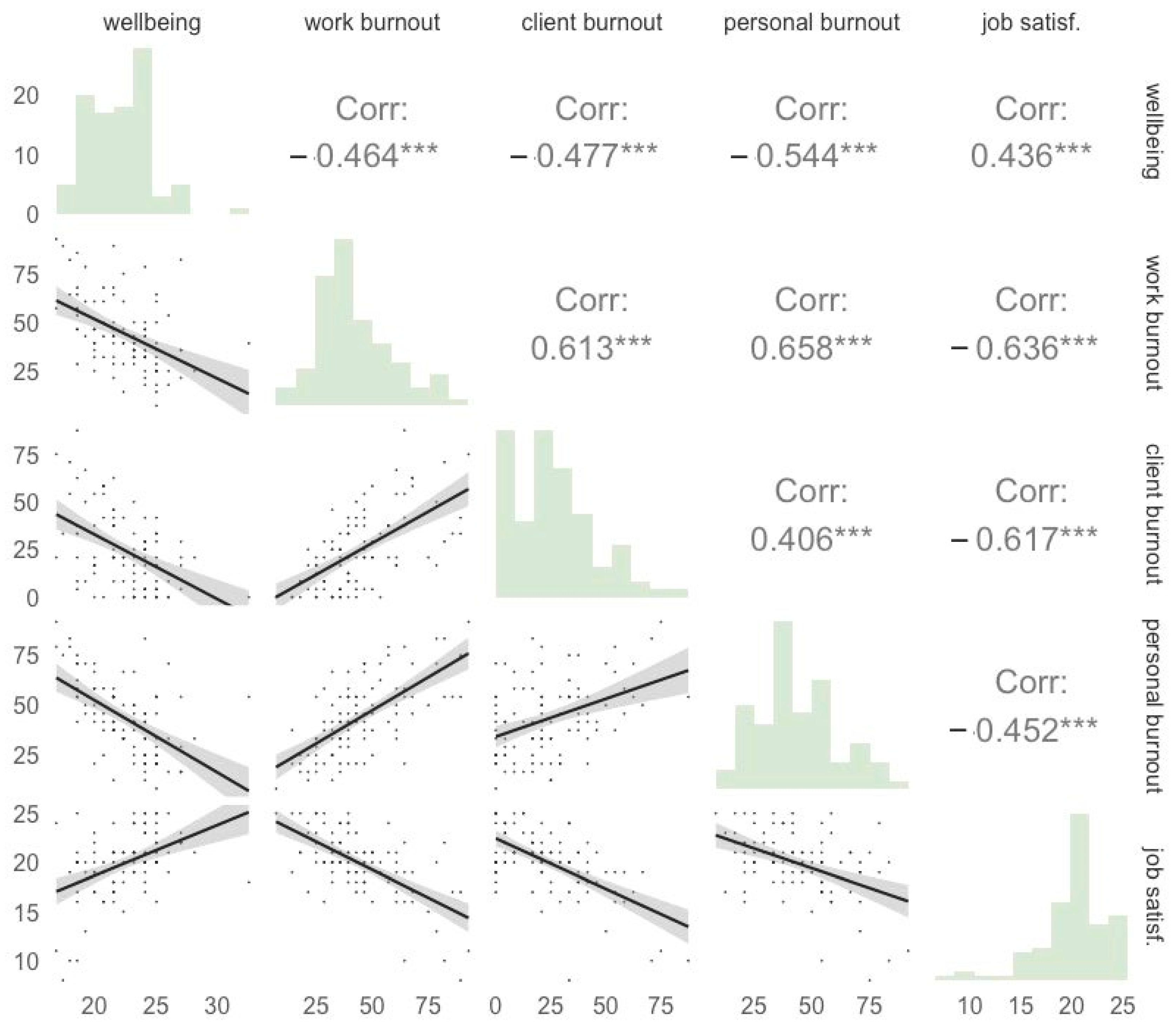
3.5. Relationship between Burnout, Wellbeing, and Job Satisfaction
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Newlove-Delgado, T.; Marcheselli, F.; Williams, T.; Mandalia, D.; Davis, J.; McManus, S.; Savic, M.; Treloar, W.; Ford, T. Mental Health of Children and Young People in England, 2023; NHS: Leeds, UK, 2023. [Google Scholar]
- Farmer, P.; Dyer, J. The Five Year Forward View for Mental Health; A report from the independent Mental Health Taskforce to the NHS in England; NHS England: London, UK, 2016. [Google Scholar]
- Anderson, J.K.; Howarth, E.; Vainre, M.; Jones, P.B.; Humphrey, A. A Scoping Literature Review of Service-Level Barriers for Access and Engagement with Mental Health Services for Children and Young People. Child. Youth Serv. Rev. 2017, 77, 164–176. [Google Scholar] [CrossRef]
- McNicholas, F.; Adamis, D.; Minihan, E.; Doody, N.; Gavin, B. Occupational Stress in Clinical and Non-Clinical Staff in Child and Adolescent Mental Health Services (CAMHS): A Cross-Sectional Study. Ir. J. Psychol. Med. 2022, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hunt, L.S. “You Absorb Trauma, without Noticing It”: A Qualitative Exploration of Staff Experiences and Subjective Well-Being Working in CAMHS Inpatient Services. Ph.D. Thesis, University of Essex, Colchester, UK, 2020. [Google Scholar]
- Doody, N.; O’Connor, C.; McNicholas, F. Consultant Psychiatrists’ Perspectives on Occupational Stress in Child and Adolescent Mental Health Services (CAMHS). Ir. J. Med. Sci. 2022, 191, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.; Hall, L.H.; Berzins, K.; Baker, J.; Melling, K.; Thompson, C. Mental Healthcare Staff Well-Being and Burnout: A Narrative Review of Trends, Causes, Implications, and Recommendations for Future Interventions. Int. J. Ment. Health Nurs. 2018, 27, 20–32. [Google Scholar] [CrossRef] [PubMed]
- McNicholas, F.; Sharma, S.; Oconnor, C.; Barrett, E. Burnout in Consultants in Child and Adolescent Mental Health Services (CAMHS) in Ireland: A Cross-Sectional Study. BMJ Open 2020, 10, e030354. [Google Scholar] [CrossRef] [PubMed]
- Aminihajibashi, S.; Skar, A.-M.S.; Jensen, T.K. Professional Wellbeing and Turnover Intention among Child Therapists: A Comparison between Therapists Trained and Untrained in Trauma-Focused Cognitive Behavioral Therapy. BMC Health Serv. Res. 2022, 22, 1328. [Google Scholar] [CrossRef] [PubMed]
- Bentham, C.; Driver, K.; Stark, D. Wellbeing of CAMHS Staff and Changes in Working Practices during the COVID-19 Pandemic. J. Child Adolesc. Psychiatr. Nurs. 2021, 34, 225–235. [Google Scholar] [CrossRef]
- Wintour, L. Experiences of Working in CAMHS Section A: A Narrative Overview of Literature Exploring Staff Experiences of Working in CAMHS. Ph.D. Thesis, Canterbury Christ Church University, Canterbury, UK, 2022. [Google Scholar]
- Parry, S.; Eve, Z.; Brockway, A.; Di Basilio, D.; Stamou, V. Exploring the Workplace Well-Being of Staff at a New Integrated Community Mental Health Service for Children and Young People. Ment. Health Pract. 2023, 26, 26–32. [Google Scholar] [CrossRef]
- Martin, L.; White, M.P.; Hunt, A.; Richardson, M.; Pahl, S.; Burt, J. Nature Contact, Nature Connectedness and Associations with Health, Wellbeing and pro-Environmental Behaviours. J. Environ. Psychol. 2020, 68, 101389. [Google Scholar] [CrossRef]
- Hunt, D.F.; Morgan, M.; Connors, M.; Mellor, C. Bringing Nature into CAMHS Inpatient Services: Reflections for the Implementation and Integration of Training into Practice. Int. Rev. Psychiatry 2022, 34, 546–552. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A New Tool for the Assessment of Burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Creedy, D.K.; Sidebotham, M.; Gamble, J.; Pallant, J.; Fenwick, J. Prevalence of Burnout, Depression, Anxiety and Stress in Australian Midwives: A Cross-Sectional Survey. BMC Pregnancy Childbirth 2017, 17, 13. [Google Scholar] [CrossRef]
- Agbobli, Y.A.; Konu, Y.R.; Gbeasor-Komlanvi, F.A.; Sadio, A.J.; Tchankoni, M.K.; Anani, J.; Akliku, N.; Bakoubayi, A.W.; Ekouevi, D.K. Prevalence and Factors Associated with Burnout among Healthcare Workers during the COVID-19 Pandemic in Togo, June 2021. Arch. Environ. Occup. Health 2022, 77, 828–837. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Knight, A. Questionnaire Survey of Burnout Amongst Dentists in Singapore. Int. Dent. J. 2022, 72, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Alameddine, M.; Bou-Karroum, K.; Hijazi, M.A. A National Study on the Resilience of Community Pharmacists in Lebanon: A Cross-Sectional Survey. J. Pharm. Policy Pract. 2022, 15, 8. [Google Scholar] [CrossRef] [PubMed]
- Borritz, M.; Rugulies, R.; Villadsen, E.; Mikkelsen, O.A.; Kristensen, T.S.; Bjorner, J.B. Burnout among Employees in Human Service Work: Design and Baseline Findings of the PUMA Study. Scand. J. Public Health 2006, 34, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Ng Fat, L.; Scholes, S.; Boniface, S.; Mindell, J.; Stewart-Brown, S. Evaluating and Establishing National Norms for Mental Wellbeing Using the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Findings from the Health Survey for England. Qual. Life Res. 2017, 26, 1129–1144. [Google Scholar] [CrossRef] [PubMed]
- Stewart-Brown, S.L.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal Construct Validity of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): A Rasch Analysis Using Data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef]
- Vaingankar, J.A.; Abdin, E.; Chong, S.A.; Sambasivam, R.; Seow, E.; Jeyagurunathan, A.; Picco, L.; Stewart-Brown, S.; Subramaniam, M. Psychometric Properties of the Short Warwick Edinburgh Mental Well-Being Scale (SWEMWBS) in Service Users with Schizophrenia, Depression and Anxiety Spectrum Disorders. Health Qual. Life Outcomes 2017, 15, 153. [Google Scholar] [CrossRef]
- Koushede, V.; Lasgaard, M.; Hinrichsen, C.; Meilstrup, C.; Nielsen, L.; Rayce, S.B.; Torres-Sahli, M.; Gudmundsdottir, D.G.; Stewart-Brown, S.; Santini, Z.I. Measuring Mental Well-Being in Denmark: Validation of the Original and Short Version of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS and SWEMWBS) and Cross-Cultural Comparison across Four European Settings. Psychiatry Res. 2019, 271, 502–509. [Google Scholar] [CrossRef]
- Melendez-Torres, G.J.; Hewitt, G.; Hallingberg, B.; Anthony, R.; Collishaw, S.; Hall, J.; Murphy, S.; Moore, G. Measurement Invariance Properties and External Construct Validity of the Short Warwick-Edinburgh Mental Wellbeing Scale in a Large National Sample of Secondary School Students in Wales. Health Qual. Life Outcomes 2019, 17, 139. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Luk, T.T.; Wang, M.P.; Shen, C.; Ho, S.Y.; Viswanath, K.; Chan, S.S.C.; Lam, T.H. The Reliability and Validity of the Chinese Short Warwick-Edinburgh Mental Well-Being Scale in the General Population of Hong Kong. Qual. Life Res. 2019, 28, 2813–2820. [Google Scholar] [CrossRef] [PubMed]
- The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS). Available online: https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs (accessed on 17 December 2023).
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Shah, N.; Cader, M.; Andrews, B.; McCabe, R.; Stewart-Brown, S.L. Short Warwick-Edinburgh Mental Well-Being Scale (SWEMWBS): Performance in a Clinical Sample in Relation to PHQ-9 and GAD-7. Health Qual. Life Outcomes 2021, 19, 260. [Google Scholar] [CrossRef]
- Sinval, J.; Marôco, J. Short Index of Job Satisfaction: Validity Evidence from Portugal and Brazil. PLoS ONE 2020, 15, e0231474. [Google Scholar] [CrossRef] [PubMed]
- Judge, T.A.; Erez, A.; Bono, J.E.; Thoresen, C.J. The core self-evaluations scale: Development of a measure. Pers. Psychol. 2003, 56, 303–331. [Google Scholar] [CrossRef]
- Judge, T.A.; Bono, J.E.; Locke, E.A.; Tippie, H.B.; Judge, T.A. Personality and Job Satisfaction: The Mediating Role of Job Characteristics. J. Appl. Psychol. 2000, 85, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Hunter, B.; Fenwick, J.; Sidebotham, D.M.; Henley, D.J. Midwives in the United Kingdom: Levels of Burnout, Depression, Anxiety and Stress and Associated Predictors. Midwifery 2019, 79, 102526. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; Albendín-García, L.; Gómez-Urquiza, J.L.; Vargas-Román, K.; Ramirez-Baena, L.; Ortega-Campos, E.; De La Fuente-Solana, E.I. Prevalence and Predictors of Burnout in Midwives: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 641. [Google Scholar] [CrossRef]
- NHS Staff Survey. 2022 National Results Briefing. 2023. Available online: https://www.nhsstaffsurveys.com/static/8c6442c8d92624a830e6656baf633c3f/NHS-Staff-Survey-2022-National-briefing.pdf (accessed on 27 November 2023).
- Iliffe, S.; Manthorpe, J. Job Dissatisfaction, ‘Burnout’ and Alienation of Labour: Undercurrents in England’s NHS. J. R. Soc. Med. 2019, 112, 370–377. [Google Scholar] [CrossRef]
- Borritz, M.; Christensen, K.B.; Bültmann, U.; Rugulies, R.; Lund, T.; Andersen, I.; Villadsen, E.; Diderichsen, F.; Kristensen, T.S. Impact of Burnout and Psychosocial Work Characteristics on Future Long-Term Sickness Absence. Prospective Results of the Danish PUMA Study among Human Service Workers. J. Occup. Environ. Med. 2010, 52, 964–970. [Google Scholar] [CrossRef]
- Office for National Statistics (ONS). Cost of Living and Depression in Adults, Great Britain: 29 September to 23 October 2022; Office for National Statistics (ONS): Wales, UK, 2022.
| Group | Work Burnout (CBI) | Personal Burnout (CBI) | Client Burnout (CBI) | Wellbeing (SWEMWBS) | Job Satisfaction (SIJS) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | MIN–MAX | M | SD | MIN–MAX | M | SD | MIN–MAX | M | SD | MIN–MAX | M | SD | MIN–MAX | M | SD | |
| Full sample | 97 | 7.1–92.9 | 44.1 | 18.5 | 8.3–91.7 | 43.6 | 18.6 | 0.0–87.5 | 24.5 | 20.6 | 16.9–32.6 | 22.5 | 2.8 | 8.0–25.0 | 19.9 | 3.3 |
| Work pattern | ||||||||||||||||
| part-time | 29 | 14.3–89.3 | 43.6 | 19.3 | 16.7–70.8 | 40.8 | 15.7 | 0.0–62.5 | 28.9 | 20.3 | 19.3–27.0 | 22.9 | 2.4 | 13.0–25.0 | 19.5 | 2.9 |
| full-time | 59 | 17.9–92.9 | 46.4 | 18.2 | 12.5–92.3 | 46.1 | 19.7 | 0.0–87.5 | 23.9 | 20.4 | 16.9–32.6 | 22.0 | 3.0 | 8.0–25.0 | 19.9 | 3.6 |
| Professional group | ||||||||||||||||
| clinical staff | 85 | 14.3–89.3 | 45.0 | 17.9 | 12.5–83.3 | 43.7 | 18.2 | 0.0–87.5 | 24.3 | 19.6 | 16.9–32.6 | 22.4 | 2.9 | 8.0–25.0 | 19.8 | 3.2 |
| non-clinical staff | 12 | 7.1–92.9 | 37.8 | 21.6 | 8.33–91.7 | 42.4 | 22.25 | 0.0–75.0 | 25.7 | 23.3 | 16.9–25.0 | 22.7 | 2.3 | 11.0–25.0 | 20.5 | 4.1 |
| Age | ||||||||||||||||
| under 25 | 8 | 25.0–78.6 | 41.5 | 16.4 | 20.8–83.3 | 47.9 | 22.3 | 4.2–54.2 | 22.9 | 16.2 | 20.0–25.0 | 22.9 | 1.9 | 17.0–22.0 | 19.8 | 1.5 |
| between 25 and 34 | 27 | 17.9–89.3 | 47.6 | 18.9 | 12.5–79.2 | 42.1 | 116.0 | 0.0–87.5 | 28.2 | 19.6 | 16.9–27.0 | 22.0 | 2.7 | 10.0–25.0 | 20.2 | 3.6 |
| between 35 and 44 | 25 | 17.9–89.3 | 41.6 | 14.7 | 16.7–75.0 | 44.2 | 16.6 | 0.0–66.7 | 18.7 | 16.9 | 17.4–28.1 | 22.6 | 2.6 | 8.0–25.0 | 20.1 | 3.2 |
| between 45 and 54 | 28 | 7.1–92.9 | 44.9 | 21.7 | 8.3–91.7 | 43.3 | 21.0 | 0.0–75.0 | 26.2 | 22.8 | 16.9–32.6 | 22.9 | 3.3 | 10.0–25.0 | 19.5 | 4.0 |
| between 55 and 64 | 7 | 17.9–67.9 | 44.9 | 19.2 | 20.8–79.2 | 47.6 | 24.5 | 8.3–62.5 | 32.1 | 21.8 | 18.0–25.0 | 21.1 | 2.5 | 17.0–22.0 | 19.9 | 1.9 |
| 65 and over | 2 | 14.3–35.7 | 25.0 | 15.2 | 16.7–37.5 | 27.1 | 14.7 | 0.0–4.2 | 2.08 | 2.95 | 22.4–27.0 | 24.7 | 3.3 | 19.0–22.0 | 20.5 | 2.1 |
| Sex | ||||||||||||||||
| male | 13 | 17.9–89.3 | 47.3 | 21.5 | 16.7–75.0 | 37.5 | 16.8 | 4.17–58.3 | 25.0 | 15.8 | 17.4–27.0 | 22.4 | 2.9 | 8.0–24.0 | 19.5 | 3.9 |
| female | 83 | 7.1–92.9 | 43.6 | 18.2 | 8.3–91.7 | 44.8 | 18.8 | 0.0–87.5 | 24.7 | 20.6 | 16.9–32.6 | 22.4 | 2.9 | 10.0–25.0 | 20.0 | 3.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mareva, S.; Chapman, B.; Hardwick, R.; Hewlett, C.; Mitchell, S.; Sanders, A.; Hayes, R. The Mental Wellbeing of Child and Adolescent Mental Health Service (CAMHS) Workers in England: A Cross-Sectional Descriptive Study Reporting Levels of Burnout, Wellbeing and Job Satisfaction. Healthcare 2024, 12, 430. https://doi.org/10.3390/healthcare12040430
Mareva S, Chapman B, Hardwick R, Hewlett C, Mitchell S, Sanders A, Hayes R. The Mental Wellbeing of Child and Adolescent Mental Health Service (CAMHS) Workers in England: A Cross-Sectional Descriptive Study Reporting Levels of Burnout, Wellbeing and Job Satisfaction. Healthcare. 2024; 12(4):430. https://doi.org/10.3390/healthcare12040430
Chicago/Turabian StyleMareva, Silvana, Beth Chapman, Rebecca Hardwick, Charlotte Hewlett, Siobhan Mitchell, Amy Sanders, and Rachel Hayes. 2024. "The Mental Wellbeing of Child and Adolescent Mental Health Service (CAMHS) Workers in England: A Cross-Sectional Descriptive Study Reporting Levels of Burnout, Wellbeing and Job Satisfaction" Healthcare 12, no. 4: 430. https://doi.org/10.3390/healthcare12040430
APA StyleMareva, S., Chapman, B., Hardwick, R., Hewlett, C., Mitchell, S., Sanders, A., & Hayes, R. (2024). The Mental Wellbeing of Child and Adolescent Mental Health Service (CAMHS) Workers in England: A Cross-Sectional Descriptive Study Reporting Levels of Burnout, Wellbeing and Job Satisfaction. Healthcare, 12(4), 430. https://doi.org/10.3390/healthcare12040430






