Oral Health Status and Oral Health-Related Behaviours of Hong Kong Students with Vision Impairment
Abstract
1. Introduction
2. Materials and Methods
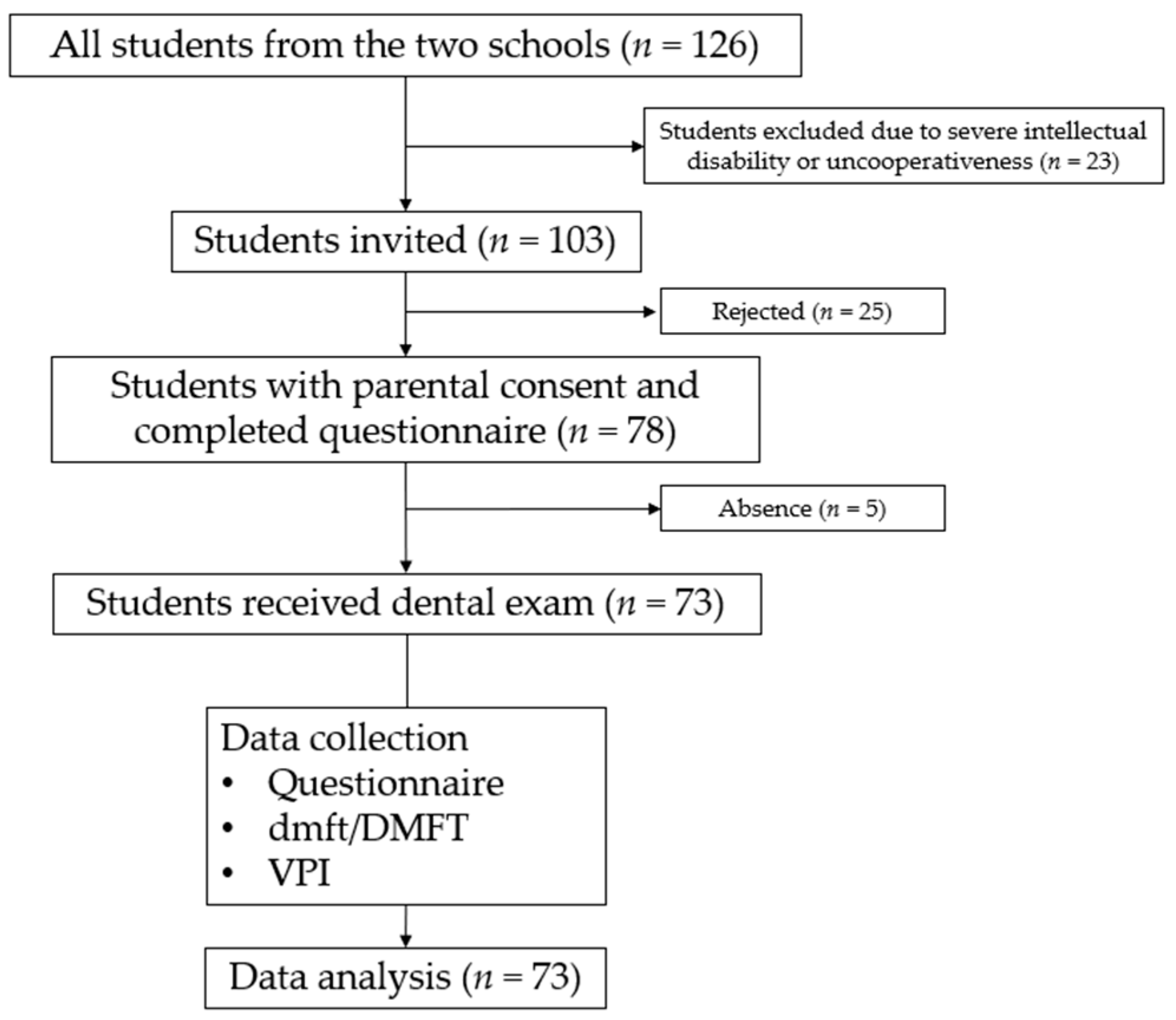
2.1. Sample Selection
2.2. Questionnaire
2.3. Clinical Examination
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Oral Health Status
3.2.1. Caries Status
- Overall, nearly half (43.8%, 32/73) of the participants had caries experiences (dmft or DMFT > 0). Their mean DMFT score (SD) was 1.0 (1.8) (Table 2).
- Caries experience in primary teeth: For children aged 6–11, their mean dmft score (SD) was 2.5 (4.2). The mean (SD) number of untreated decayed teeth (dt) was 2.4 (4.2), constituting more than 95% of the dmft score. The mean number of filled or missing teeth was small (ft = 0.1; mt = 0.04). A positively skewed distribution of the dmft score was found, with the skewness being 2.0.
- Caries experience in permanent teeth: The overall mean (SD) DMFT score was 1.0 (1.8). Altogether, DT (0.8) constituted 80% of the DMFT score. The mean number of FT and MT across all age groups was small (FT = 0.2; MT ≤ 0.1), except in the 15–21 age group, in which a larger proportion of FT was observed (0.5). A positively skewed distribution of the DMFT score was found, with the skewness being 2.3.
3.2.2. Oral Hygiene Status
3.3. Oral Health Behaviours
3.4. Univariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bourne, R.; Steinmetz, J.D.; Flaxman, S.; Briant, P.S.; Taylor, H.R.; Resnikoff, S.; Casson, R.J.; Abdoli, A.; Abu-Gharbieh, E.; Afshin, A.; et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e130–e143. [Google Scholar] [CrossRef]
- World Health Organisation. ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS) 9D90 Vision Impairment Including Blindness. Available online: https://icd.who.int/browse11/l-m/en#/http%253a%252f%252fid.who.int%252ficd%252fentity%252f1103667651 (accessed on 23 November 2023).
- Toledo, C.C.; Paiva, A.P.; Camilo, G.B.; Maior, M.R.; Leite, I.C.; Guerra, M.R. Early detection of visual impairment and its relation to academic performance. Rev. Assoc. Med. Bras. 2010, 56, 415–419. [Google Scholar] [CrossRef]
- Rainey, L.; Elsman, E.B.M.; Van Nispen, R.M.A.; Van Leeuwen, L.M.; Van Rens, G.H.M.B. Comprehending the impact of low vision on the lives of children and adolescents: A qualitative approach. Qual. Life Res. 2016, 25, 2633–2643. [Google Scholar] [CrossRef]
- Costa Silva-Freire, L.; Guimaraes, M.O.; Abreu, L.G.; Vargas-Ferreira, F.; Vieira-Andrade, R.G. Oral health issues in children and adolescents with vision impairment: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2022, 32, 877–893. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, Y.; Wu, W.; He, M.; Lu, Z.; Zhang, K.; Li, J.; Lei, S.; Guo, S.; Zhang, Y. Oral health status among visually impaired schoolchildren in Northeast China. BMC Oral Health 2019, 19, 63. [Google Scholar] [CrossRef]
- Alsadhan, S.A.; Al-Jobair, A.M.; Bafaqeeh, M.; Abusharifa, H.; Alagla, M. Dental and medical health status and oral health knowledge among visually impaired and sighted female schoolchildren in Riyadh: A comparative study. BMC Oral Health 2017, 17, 154. [Google Scholar] [CrossRef]
- Prashanth, S.T.; Bhatnagar, S.; Das, U.M.; Gopu, H. Oral health knowledge, practice, oral hygiene status, and dental caries prevalence among visually impaired children in Bangalore. J. Indian Soc. Pedod. Prev. Dent. 2011, 29, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Reddy, K. Prevalence of oral health status in visually impaired children. J. Indian Soc. Pedod. Prev. Dent. 2011, 29, 3. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, E.K.; Kumar, N.; Porter, S.R. Effect of visual impairment upon oral health care: A review. Br. Dent. J. 2008, 204, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Nowak, A.J. Dental care for the handicapped patient Past, present, future. In Dentistry for the Handicapped Patient; C.V. Mosby Company: St. Louis, MO, USA, 1976; p. 320. [Google Scholar]
- Hennequin, M.; Faulks, D.; Roux, D. Accuracy of estimation of dental treatment need in special care patients. J. Dent. 2000, 28, 131–136. [Google Scholar] [CrossRef]
- Nelson, L.P.; Getzin, A.; Graham, D.; Zhou, J.; Wagle, E.M.; McQuiston, J.; McLaughlin, S.; Govind, A.; Sadof, M.; Huntington, N.L. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr. Dent. 2011, 33, 29–36. [Google Scholar]
- Chan, H.T.; Chiu, H.C.; Kwok, Y.T.; Law, Y.T.; Loo, L.E.; Tang, H.Y.; Tsui, T.Y.; Wong, T.F. Outreach Dental Care Service to Hong Kong Adults with Visual Impairment. Bachelor’s Thesis, University of Hong Kong, Hong Kong, China, 2017. Available online: http://hdl.handle.net/10722/257599 (accessed on 23 November 2023).
- Blanco López, M.A.; Diniz Freitas, M.; Limeres Posse, J.; Hernández-Vallejo, G.; López-Pintor, R.M. Oral health status and dental care for individuals with visual impairment. A narrative review. Spec. Care Dent. 2023, 43, 221–231. [Google Scholar] [CrossRef]
- Community Special Dental Service in Hong Kong. Available online: https://www.dh.gov.hk/english/main/main_ds/main_ds_dcp.html (accessed on 23 November 2023).
- Gao, S.; Chen, K.; Duangthip, D.; Lo, E.; Chu, C. Oral Health Care in Hong Kong. Healthcare 2018, 6, 45. [Google Scholar] [CrossRef]
- So, A.; Cheung, E.; Tse, C.; Wong, M. Oral health education for visually impaired children in Hong Kong. In Proceedings of the 20th Annual Scientific Meeting of the International Association for Dental Research (Southeast Asia Division) & 16th Annual Scientific Meeting of the Southeast Asia Association for Dental Education, Malacca, Malaysia, 1–4 September 2005; Volume 84. [Google Scholar]
- Census and Statistics Department, The Government of the Hong Kong Special Administrative Region. Social Data Collected via the General Household Survey: Special Topics Report-Report No.63-Persons with Disabilities and Chronic Diseases; Census and Statistics Department, HKSAR: Hong Kong, China, 2021.
- World Health Organisation. Assessment of oral health status. In Oral Health Surveys: Basic Methods, 5th ed.; WHO: Geneva, Switzerland, 2013; pp. 35–57. [Google Scholar]
- Ainamo, J.; Bay, I. Problems and proposals for recording gingivitis and plaque. Int. Dent. J. 1975, 25, 229–235. [Google Scholar]
- Department of Health, The Government of the Hong Kong Special Administrative Region. Oral Health Survey 2011; Department of Health, HKSAR: Hong Kong, China, 2011.
- Duangthip, D.; Chen, K.J.; Gao, S.S.; Lo, E.C.M.; Chu, C.H. Early childhood caries among 3- to 5-year-old children in Hong Kong. Int. Dent. J. 2019, 69, 230–236. [Google Scholar] [CrossRef]
- Skafida, V.; Chambers, S. Positive association between sugar consumption and dental decay prevalence independent of oral hygiene in pre-school children: A longitudinal prospective study. J. Public Health 2018, 40, e275–e283. [Google Scholar] [CrossRef] [PubMed]
- Featherstone, J.D.B. The caries balance: The basis for caries management by risk assessment. Oral Health Prev. Dent. 2004, 2 (Suppl. S1), 259–264. [Google Scholar] [PubMed]
- Roberts, L.; Marx, J.M.; Musher-Eizenman, D.R. Using food as a reward: An examination of parental reward practices. Appetite 2018, 120, 318–326. [Google Scholar] [CrossRef]
- Bilyk, M.C.; Sontrop, J.M.; Chapman, G.E.; Barr, S.I.; Mamer, L. Food experiences and eating patterns of visually impaired and blind people. Can. J. Diet. Pract. Res. 2009, 70, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Karem Hassan, B.; Jabbar Ali, B.; Mahmood Alwan, A.; Badeia, R.A. Self-Reported Oral Health Attitudes and Behaviors, and Gingival Status of Dental Students. Clin. Cosmet. Investig. Dent. 2020, 12, 225–232. [Google Scholar] [CrossRef]
- Azodo, C.C.; Unamatokpa, B. Gender difference in oral health perception and practices among Medical House Officers. Russ. Open Med. J. 2012, 1, 0208. [Google Scholar] [CrossRef]
- Lipsky, M.S.; Su, S.; Crespo, C.J.; Hung, M. Men and Oral Health: A Review of Sex and Gender Differences. Am. J. Men’s Health 2021, 15, 15579883211016361. [Google Scholar] [CrossRef]
- Rajeh, M.T. Gender Differences in Oral Health Knowledge and Practices Among Adults in Jeddah, Saudi Arabia. Clin. Cosmet. Investig. Dent. 2022, 14, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Lipsky, M.S.; Licari, F.W.; Hung, M. Comparing oral health behaviours of men and women in the United States. J. Dent. 2022, 122, 104157. [Google Scholar] [CrossRef] [PubMed]
- Thomson, W.M.; Williams, S.M.; Broadbent, J.M.; Poulton, R.; Locker, D. Long-term dental visiting patterns and adult oral health. J. Dent. Res. 2010, 89, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Shivanna, V.; Jain, Y.; Valluri, R.; Birra, V.; Kumar, V.; Ealla, K.K.R. Estimation of Dental Anxiety Levels Before and After Dental Visit in Children with Visual Impairment Using Modified Dental Anxiety Scale in Braille Text. J. Int. Soc. Prev. Community Dent. 2020, 10, 76–84. [Google Scholar] [CrossRef]
- Chua, H.; Sardana, D.; Turner, R.; Ting, G.; Ekambaram, M. Effectiveness of oral health education methods on oral hygiene in children and adolescents with visual impairment: A systematic review. Int. J. Paediatr. Dent. 2021, 31, 724–741. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.A.; Bradley, N.; Fenesan, S. Dental management of patients with sensory impairments. Br. Dent. J. 2022, 233, 627–633. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | N | Frequency | |
|---|---|---|---|
| Age (years) | 6–11 | 32 | 43.8% |
| 12–14 | 14 | 19.2% | |
| 15–21 | 27 | 37.0% | |
| Sex | Female | 31 | 42.5% |
| Male | 42 | 57.5% | |
| Severity of vision impairment | Unable to see at all | 23 | 31.5% |
| Requires special visual aid | 25 | 34.2% | |
| Does not require special visual aid | 25 | 34.2% | |
| Family monthly income (HKD) | ≤HKD 16,000 | 15 | 20.5% |
| HKD 16,001–30,000 | 21 | 28.8% | |
| HKD 30,001–50,000 | 22 | 30.1% | |
| >HKD 50,000 | 15 | 20.5% | |
| Age (Years) | N | D Mean (SD) | M Mean (SD) | F Mean (SD) | DMFT Mean (SD) | Caries Prevalence (%) | VPI Mean (SD) |
|---|---|---|---|---|---|---|---|
| 6–11 | 32 | 0.7 (1.6) | 0.0 (0.0) | 0.07 (0.4) | 0.8 (1.6) | 31.1 | 0.69 (0.33) |
| 12–14 | 14 | 1.0 (1.8) | 0.0 (0.0) | 0.07 (0.3) | 1.1 (1.8) | 35.7 | 0.90 (0.16) |
| 15–21 | 27 | 0.7 (1.4) | 0.0 (0.0) | 0.5 (1.1) | 1.2 (1.9) | 40.7 | 0.78 (0.29) |
| Overall | 73 | 0.8 (1.6) | 0.0 (0.0) | 0.2 (0.8) | 1.0 (1.8) | 35.5 | 0.76 (0.30) |
| Independent Factors | N | Caries Prevalence | p-Value * | |
|---|---|---|---|---|
| Age (years) | 6–11 | 32 | 50.0% | 0.614 |
| 12–14 | 14 | 35.7% | ||
| 15–21 | 27 | 40.7% | ||
| Sex | Female | 31 | 51.6% | 0.250 |
| Male | 42 | 38.1% | ||
| Severity of vision impairment | Unable to see at all | 23 | 43.5% | 0.522 |
| Requires special visual aid | 25 | 36.0% | ||
| Does not require special visual aid | 25 | 52.0% | ||
| Father’s education level | Primary or below | 5 | 20.0% | 0.531 |
| Junior secondary | 16 | 56.3% | ||
| Senior secondary | 26 | 42.3% | ||
| Post-secondary | 26 | 42.3% | ||
| Mother’s education level | Primary or below | 7 | 28.6% | 0.590 |
| Junior secondary | 12 | 58.3% | ||
| Senior secondary | 31 | 45.2% | ||
| Post-secondary | 23 | 39.1% | ||
| Family monthly income (HKD) | ≤HKD 16,000 | 15 | 60.0% | 0.503 |
| HKD 16,001–30,000 | 21 | 42.9% | ||
| HKD 30,001–50,000 | 22 | 40.9% | ||
| >HKD 50,000 | 15 | 33.3% | ||
| Received oral hygiene instruction previously | Yes | 51 | 51.0% | 0.061 |
| No | 22 | 27.3% | ||
| Dental check-up experience | Yes | 64 | 46.9% | 0.163 |
| No | 9 | 22.2% | ||
| Frequency of daily snacking | 0–1 | 50 | 34.0% | 0.013 |
| ≥2 | 23 | 65.2% | ||
| Brushing habit | Independent brushing | 42 | 47.6% | 0.638 |
| Parent-supervised brushing | 7 | 42.9% | ||
| Parent-assisted brushing | 24 | 37.5% | ||
| Frequency of daily brushing | 0–1 | 7 | 14.3% | 0.097 |
| ≥2 | 66 | 47.0% | ||
| Frequency of daily interdental cleaning | 0 | 58 | 44.8% | 0.737 |
| ≥1 | 15 | 40.0% | ||
| Independent Factors | Median | p-Value | |
|---|---|---|---|
| Age (years) | 6–11 | 0.75 | 0.070 b |
| 12–14 | 1.00 | ||
| 15–21 | 0.92 | ||
| Sex | Female | 0.75 | 0.048 a |
| Male | 1.00 | ||
| Severity of vision impairment | Unable to see at all | 0.83 | 0.586 b |
| Requires special visual aid | 0.75 | ||
| Does not require special visual aid | 1.00 | ||
| Father’s education level | Primary or below | 1.00 | 0.287 b |
| Junior secondary | 0.67 | ||
| Senior secondary | 0.83 | ||
| Post-secondary | 0.10 | ||
| Mother’s education level | Primary or below | 0.75 | 0.593 b |
| Junior secondary | 0.92 | ||
| Senior secondary | 1.00 | ||
| Post-secondary | 0.75 | ||
| Family monthly income (HKD) | <HKD 16,000 | 1.00 | 0.560 b |
| HKD 16,001–30,000 | 0.75 | ||
| HKD 30,001–50,000 | 0.83 | ||
| >HKD 50,000 | 1.00 | ||
| Received oral hygiene instruction previously | Yes | 0.75 | 0.120 a |
| No | 1.00 | ||
| Dental check-up experience | Yes | 0.88 | 0.103 a |
| No | 0.58 | ||
| Frequency of daily snacking | 0–1 | 1.00 | 0.178 a |
| ≥2 | 0.83 | ||
| Brushing habit | Independent brushing | 0.79 | 0.216 b |
| Parent-supervised brushing | 0.75 | ||
| Parent-assisted brushing | 1.00 | ||
| Frequency of daily brushing | 0–1 | 1.00 | 0.628 a |
| ≥2 | 0.83 | ||
| Frequency of daily interdental cleaning | 0 | 1.00 | 0.103 a |
| ≥1 | 0.67 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.K.Y.; Yuen, A.W.T.; Leung, K.P.Y.; Li, J.T.W.; Bae, S.Y.; Chan, Y.Y.; Ip, C.K.; Lau, S.H.; Lau, Y.N.; Lo, H.Y.; et al. Oral Health Status and Oral Health-Related Behaviours of Hong Kong Students with Vision Impairment. Healthcare 2024, 12, 391. https://doi.org/10.3390/healthcare12030391
Lee JKY, Yuen AWT, Leung KPY, Li JTW, Bae SY, Chan YY, Ip CK, Lau SH, Lau YN, Lo HY, et al. Oral Health Status and Oral Health-Related Behaviours of Hong Kong Students with Vision Impairment. Healthcare. 2024; 12(3):391. https://doi.org/10.3390/healthcare12030391
Chicago/Turabian StyleLee, Jessica Ka Yi, Agatha Wing Tung Yuen, Karen Pui Yan Leung, Joyce Tin Wing Li, Seon Yeong Bae, Yi Yung Chan, Ching Kiu Ip, Sik Hong Lau, Yin Ngai Lau, Hei Yuet Lo, and et al. 2024. "Oral Health Status and Oral Health-Related Behaviours of Hong Kong Students with Vision Impairment" Healthcare 12, no. 3: 391. https://doi.org/10.3390/healthcare12030391
APA StyleLee, J. K. Y., Yuen, A. W. T., Leung, K. P. Y., Li, J. T. W., Bae, S. Y., Chan, Y. Y., Ip, C. K., Lau, S. H., Lau, Y. N., Lo, H. Y., Tang, S. K., & Duangthip, D. (2024). Oral Health Status and Oral Health-Related Behaviours of Hong Kong Students with Vision Impairment. Healthcare, 12(3), 391. https://doi.org/10.3390/healthcare12030391







