Effectiveness and Health Outcomes of Collaborative Nurse Prescribing for Patients Anticoagulated with Antivitamin K in Primary Care: A Study Protocol
Abstract
1. Introduction
- -
- Improve the assessment and monitoring of patients being treated with oral anticoagulation with VKAs.
- -
- Improve dosage adjustment with greater accuracy.
- -
- Encourage patient adherence to the prescribed treatment regimen.
- -
- Empower patients to take greater responsibility for self-care through comprehensive health education.
- -
- Reduce complications, hospitalizations and urgent care visits related to anticoagulation therapy.
- -
- Increase patient satisfaction and improve quality of life.
- -
- Decrease physicians’ workloads.
- -
- Establish a framework to assess the outcomes and quality of outpatient anticoagulation management services by nurses.
1.1. General Objective
Specifics Objectives
- -
- To evaluate the impact on the number of days of treatment that the patient is in therapeutic range.
- -
- To account for adverse events related to the procedure.
- -
- To describe adverse events related to the procedure.
- -
- To establish the economic impact on chapter I (personnel expenses).
- -
- To quantify the consumption of test strips for INR determination.
2. Materials and Methods
2.1. Research Hypothesis
2.2. Design
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Study Population and Sample
2.6. Variables and Data Collection
2.7. Procedure
2.7.1. Established Procedure of Follow-Up and Intervention
2.7.2. Experimental Procedure of Follow-Up and Intervention
2.8. Data Analysis
2.9. Validity and Reliability
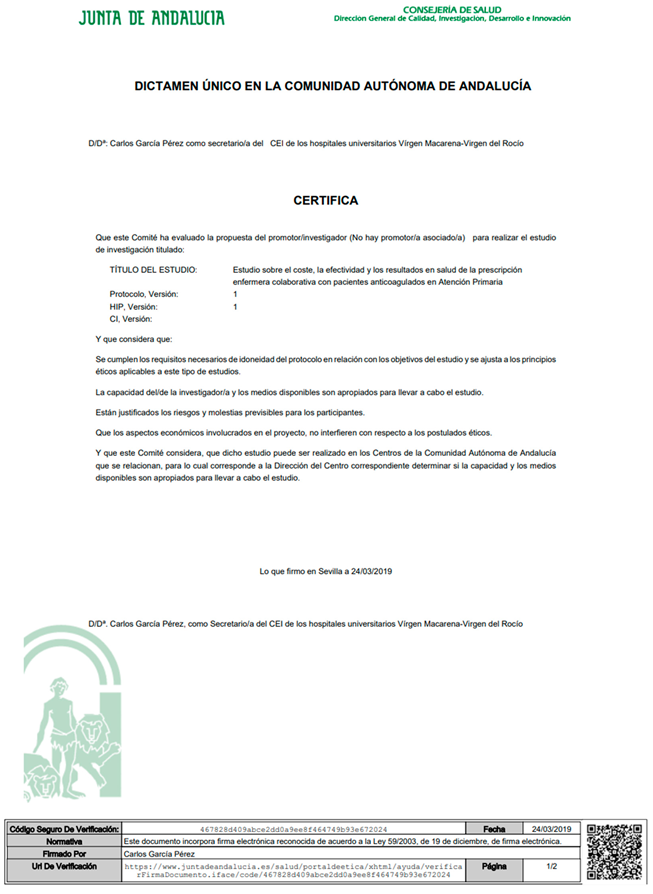
2.10. Ethical Considerations
2.11. Limitations
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
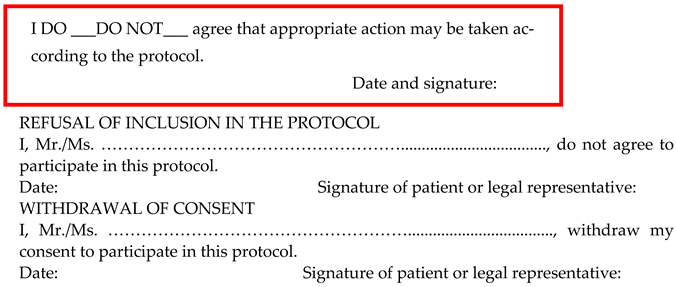
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- What are the date, month, and year?
- What is the day of the week?
- What is the name of this place?
- What is your phone number?
- How old are you?
- When were you born?
- Who is the current president?
- Who was the president before him?
- What was your mother’s maiden name?
- Can you count backward from 20 by 3’s?
Appendix B
- Your physician prescribes your anticoagulant therapy.
- After your anticoagulant therapy is stabilized, your physician authorizes a nurse to follow up on your treatment.
- By signing this document, you or your representative authorize the family nurse to follow up the treatment.
- The family nurse will follow up your treatment according to the protocol and will refer you back to the physician when appropriate, following the indications of the protocol.

- -
- I have read and understood the above information.
- -
- I was able to ask questions and clarify all my doubts.
- -
- I have consciously and freely made the decision to give my consent.
- -
- I know that I can withdraw my consent at any time.
Appendix C
References
- Sánchez-Martín, I. Chronic diseases and complexity: New roles in nursing. Advanced practice nurses and chronic patient. Enferm. Clin. 2014, 24, 79–89. [Google Scholar] [CrossRef]
- Padilla-Marín, C.; Terol-Fernández, E.; Camacho-Bejarano, R.; Padín-Lopez, S. Shared care-demand management in Primary Care: An opportunity for nursing staff? Enferm. Clin. 2012, 22, 237–238. [Google Scholar] [CrossRef]
- Casajuana-Brunet, J. In search of efficiency: Stop doing to be able to do. Form. Med. Contin. Aten. Prim. 2005, 12, 579–581. [Google Scholar]
- Gutiérrez-Sequera, J.L.; Serrano-Ortega, N. Healthcare and the sustainability of the public health system. Enferm. Clín. 2014, 24, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Romero, A.; Parrado, G.; Rodríguez, J.; Caparrós, I.; Vargas, M.; Ortiz, P. Anticoagulant therapy clinic: Moving towards Advanced Nursing Practice. Enferm. Clin. 2014, 24, 200–204. [Google Scholar]
- Horrocks, S.; Anderson, E.; Salisbury, C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002, 324, 819–823. [Google Scholar] [CrossRef]
- Laurant, M.; Van der Biezen, M.; Wijers, N.; Watananirun, K.; Kontopantelis, E.; Van Vught, A.J.A.H. Nurses as substitutes for doctors in primary care. Cochrane Database Syst. Rev. 2018, 7, CD001271. [Google Scholar] [CrossRef]
- Field, T.; Tjia, J.; Mazor, K.M.; Donovan, J.L.; Kanaan, A.O.; Harrold, L.R.; Reed, G.; Doherty, P.; Spenard, A.; Gurwitz, J.H. A Randomized Trial of a Warfarin Communication Protocol for Nursing Homes: An SBAR-based Approach. Am. J. Med. 2011, 124, 179. [Google Scholar] [CrossRef]
- Niiranen, S.; Wartiovaara-Kautto, U.; Syrjälä, M.; Puustinen, R.; Yli-Hietanen, J.; Mattila, H.; Kalli, S.; Lamminen, H. Reorganization of oral anticoagulant (warfarin) treatment follow-up. Scand. J. Prim. Health Care 2006, 24, 33–37. [Google Scholar]
- Ansell, J.; Hirsh, J.; Dalen, J.; Bussey, H.; Anderson, D.; Poller, L.; Jacobson, A.; Deykin, D.; Matchar, D. Managing oral anticoagulant therapy. Chest 2001, 119 (Suppl. 1), 22S–38S. [Google Scholar] [CrossRef]
- Francavilla, C. Registered Nurse-Managed Anticoagulation Clinic: Improving Patient Outcomes. Nurs. Econ. 2008, 26, 130–132. [Google Scholar]
- Protocolized Follow-Up of Individualized Pharmacological Treatment in People Undergoing Oral Anticoagulation Treatment, Review 3rd ed.; Ministry of Health and Family; Andalusian Health Service: Seville, Spain, 2019.
- García-Donas, G.; García, M.; Almendro, M.; Blasco, I.; Palomo-Lara, J.C.; Salamero, E. Manual of Oral Anticoagulation; Haematology Clinical Management Unit: Seville, Spain, 2018; ISBN 978-84-09-02390-5. [Google Scholar]
- Woyach, J.; Wurster, M. National experience with an electronic medical record for anticoagulation therapy. J. Thromb. Thrombolysis 2008, 25, 109–110. [Google Scholar] [CrossRef]
- Hefler, G.; Stach, J. Development of a dosing algorithm in a nurse-managed outpatient anticoagulation clinic. J. Am. Acad. Nurse Pract. 2011, 23, 546–551. [Google Scholar] [CrossRef]
- Rivera-Caravaca, J.M.; Gil-Perez, P.; Lopez-García, C.; Veliz-Martínez, A.; Quintana-Giner, M.; Romero-Aniorte, A.; Fernandez-Redondo, C.; Muñoz, L.; Quero, E.; Esteve-Pastor, M.A.; et al. A nurse-led atrial fibrillation clinic: Impact on anticoagulation therapy and clinical outcomes. Int. J. Clin. Pract. 2020, 74, e13634. [Google Scholar] [CrossRef] [PubMed]
- Weeks, G.; George, J.; Maclure, K.; Stewart, D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst. Rev. 2016, 11, CD011227. [Google Scholar] [CrossRef]
- Romero, A.; Parrado, G.; Caparrós, I.S.; Rodríguez, J.; Vargas, M.; Ortiz, P. An Advanced Nursing Practice experience in patients receiving oral anticoagulation therapy. Metas. Enferm. 2011, 14, 75–78. [Google Scholar]
- Rodríguez, S.; De la Fuente, N.; Casado, M.I.; Ayuso, M. Nurse prescribing within the Spanish national Health Service: Fact or fiction? Enferm. Clin. 2015, 25, 107–109. [Google Scholar]
- Roche Diagnostics. Spain. TAO Net Pro. Available online: https://diagnostics.roche.com/es/es/products/digital/taonet-pro-pid00000580.html#assay (accessed on 15 June 2019).
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Roche Diagnostics. Spain. CoaguChek® XS International System. Available online: https://diagnostics.roche.com/es/es/products/instruments/coaguchek-xs-ins-804.html#productSpecs (accessed on 14 June 2019).
- Kääriäinen, M.; Paukama, M.; Kyngäs, H. Adherence with health regimens of patients on warfarin therapy. J. Clin. Nurs. 2013, 22, 89–96. [Google Scholar] [CrossRef]
- Barón, G.; Escolar, G.; Zamorano, J.L.; Lourdes, N.; Canal, C.; De Salas-Cansado, M.; Rubio-Rodriguez, D.; Rubio-Terrés, C. Cost-effectiveness Analysis Comparing Apixaban and Acenocoumarol in the Prevention of Stroke in Patients with Non-valvular Atrial Fibrillation in Spain. Rev. Esp. Cardiol. 2015, 68, 680–690. [Google Scholar] [CrossRef]
- González-Juanatey, J.R.; Álvarez-Sabin, J.; Lobos, J.M.; Martínez-Rubio, A.; Reverter, J.C.; Oyagüez, I.; González-Rojas, N.; Becerra, V. Cost-effectiveness of Dabigatran for Stroke Prevention in Non-valvular Atrial Fibrillation in Spain. Rev. Esp. Cardiol. 2012, 65, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Restovic, G.; Carcedo, D.; McLeod, E.; Guillermin, A.L.; Evers, T. Cost-effectiveness of rivaroxaban versus acenocumarol in the stroke prevention in patients with non-valvular atrial fibrillation in the Spanish setting. Value Health 2012, 15, A375. [Google Scholar] [CrossRef]
- Connolly, S.J.; Ezekowitz, M.B.; Yusuf, S.; Elkeboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Mullin, R.; Blazawski, J.; Coleman, C.I. Cost-effectiveness of apixaban compared with warfarin for stroke prevention in atrial fibrillation. PLoS ONE 2012, 7, e47473. [Google Scholar] [CrossRef] [PubMed]
- Kamel, H.; Easton, J.D.; Johnston, S.C.; Kim, A.S. Cost-effectiveness of apixaban vs warfarin for secondary stroke prevention in atrial fibrillation. Neurology 2012, 79, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- Bonet, A.; Gosalbes, V.; Ridao-Lopez, M.; Navarro, J.; Navarro, B.; Peiro, S. Dabigatran versus Acenocumarol for the Prevention of Stroke in Atrial Fibrillation. Budget Impact Analysis in one Health Department in Spain. Rev. Esp. Salud Pública 2013, 87, 331–342. [Google Scholar]
- Romero, A.; Romero-Arana, A.; Gomez–Salgado, J. Direct anticoagulants and nursing: An approach from patient’s safety. Enferm. Clin. 2017, 27, 106–112. [Google Scholar] [CrossRef]
- Patel, M. Emergency Approach to Bleeding with NOAC: Do We Need an Antagonist? 2015. Available online: http://img.medscapestatic.com/images/851/796/851796_transcript_spa.pdf (accessed on 13 June 2018).
- Mak, K.H. Coronary and mortality risk of novel oral antithrombotic agents: A meta-analysis of large randomized trials. BMJ Open 2012, 2, e001592. [Google Scholar] [CrossRef]
- CADIME. Drug Evaluation Reports. Edoxaban. 2017. Available online: https://cadime.es/fichas-de-nuevos-medicamentos/437-edoxab%C3%A1n.html (accessed on 15 June 2019).
- Avorn, J. The relative cost-effectiveness of anticoagulants: Obvious, except for the cost and the effectiveness. Circulation 2011, 123, 2519–2521. [Google Scholar] [CrossRef]
- Palomo-Lara, J.C. Optimizing clinical management in a health care unit: An innovative experience. Rev. ROL Enferm. 2017, 40, 578–584. [Google Scholar]
- Polit, D.F.; Hungler, B.P. Ethical context of health sciences research. In Scientific Research in Health Sciences, 6th ed.; McGraw-Hill Interamericana: Ciudad de Mexico, Mexico, 2000; pp. 129–149. [Google Scholar]
- Organic Law for the Protection of Personal Data and Guarantee of Personal Rights. Organic Law 3/2018 of December 5; Official State Gazette No. 294 (12 June 2018); Government of Spain: Madrid, Spain, 2018. [Google Scholar]
- Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lara, J.C.P.; March-Cerdà, J.C.; Ponce-Blandón, J.A.; Pabón-Carrasco, M.; Jiménez-Picón, N. Effectiveness and Health Outcomes of Collaborative Nurse Prescribing for Patients Anticoagulated with Antivitamin K in Primary Care: A Study Protocol. Healthcare 2024, 12, 347. https://doi.org/10.3390/healthcare12030347
Lara JCP, March-Cerdà JC, Ponce-Blandón JA, Pabón-Carrasco M, Jiménez-Picón N. Effectiveness and Health Outcomes of Collaborative Nurse Prescribing for Patients Anticoagulated with Antivitamin K in Primary Care: A Study Protocol. Healthcare. 2024; 12(3):347. https://doi.org/10.3390/healthcare12030347
Chicago/Turabian StyleLara, Juan Carlos Palomo, Joan Carles March-Cerdà, José Antonio Ponce-Blandón, Manuel Pabón-Carrasco, and Nerea Jiménez-Picón. 2024. "Effectiveness and Health Outcomes of Collaborative Nurse Prescribing for Patients Anticoagulated with Antivitamin K in Primary Care: A Study Protocol" Healthcare 12, no. 3: 347. https://doi.org/10.3390/healthcare12030347
APA StyleLara, J. C. P., March-Cerdà, J. C., Ponce-Blandón, J. A., Pabón-Carrasco, M., & Jiménez-Picón, N. (2024). Effectiveness and Health Outcomes of Collaborative Nurse Prescribing for Patients Anticoagulated with Antivitamin K in Primary Care: A Study Protocol. Healthcare, 12(3), 347. https://doi.org/10.3390/healthcare12030347






