A Systematic Review of Virtual Reality’s Impact on Anxiety During Palliative Care
Abstract
1. Introduction
1.1. Positive Psychological Well-Being (PPWB) and Complementary Therapies in Palliative Care
1.2. Integrative Oncology: Yoga for Palliative Care Anxiety Management
1.3. The Potential of Harnessing VR in Palliative Care
1.4. Challenges of VR Adoption in Palliative Care
1.5. Objectives
- (A)
- Do VR treatments significantly impact anxiety in palliative care patients?
- (B)
- What are the types of VR interventions that have been used in palliative care, and have they been effective at reducing anxiety?
- (C)
- What specific design features of VR therapy (personalization, interactivity, session frequency) seem to sustain or enhance therapeutic performance in the palliative care environment?
2. Materials and Methods
2.1. Protocol Registration
2.2. Eligibility Criteria
2.3. Search Strategy
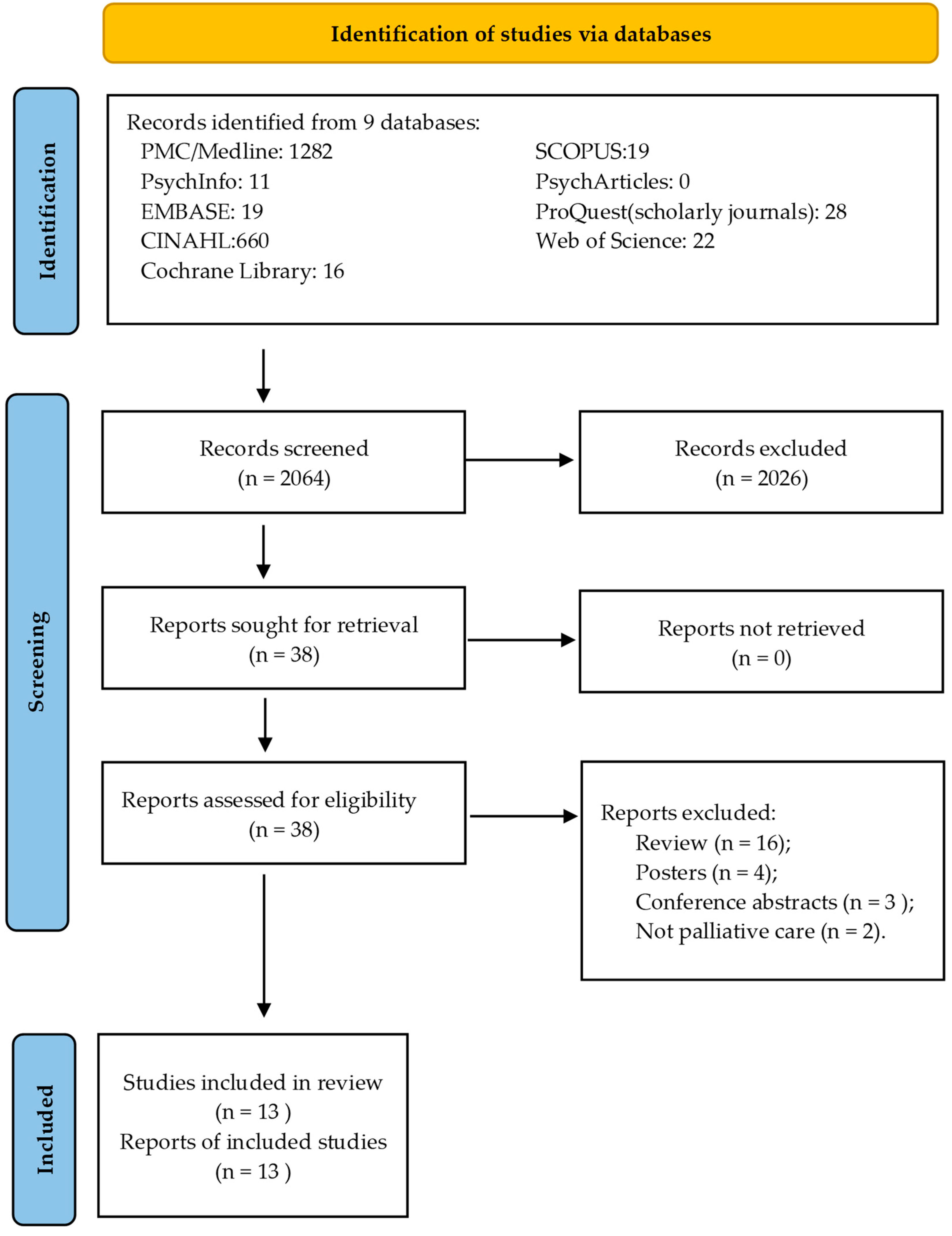
2.4. Study Selection Process
2.5. Data Extraction, Synthesis, Outcomes, and Statistical Analysis Feasibility
2.6. Risk of Bias Assessment
3. Results
3.1. Study Selection and Characteristics
3.2. Anxiety Reduction and Emotional Relief
3.3. Content and Personalization Impact on Results with VR
3.4. VR Perspectives in Palliative Care
3.5. The Physiological and Psychological Signatures of Relaxation
3.6. Limitations of VR Interventions
4. Discussion
4.1. VR Impact Beyond Anxiety
4.2. Feasibility and Acceptability of VR Interventions in Palliative Care
4.3. VR Interventions to Address “Total Pain”
4.4. Limitations
4.5. Future Directions and Implications for Practice
- Standardization of VR RCTs protocols design: Establishing evidence-based standardized parameters regarding session length, frequency, and content development could enhance the reproducibility and comparability of VR interventions across studies and clinical settings.
- Assessment of the long-term effects of VR exposure: Investigating the persistence of VR’s impact on anxiety, mood, and overall well-being will provide insights into its effectiveness as a long-term symptom management tool in palliative care.
- Multi-symptom applications: Beyond anxiety and physiological relaxation, VR’s potential to address pain, depression, and existential distress warrants exploration to expand its utility in palliative care.
- Improving accessibility and usability: Developing VR systems tailored to the needs of older adults and physically impaired patients will increase comfort and safety and broaden adoption in palliative care environments.
5. Conclusions
- Standardizing intervention protocols and developing uniform VR intervention guidelines to enhance comparability and reproducibility across studies;
- Long-term impact studies investigating the sustained effects of VR on anxiety and other related symptoms to understand its long-term benefits in palliative care;
- Enhancing device accessibility by focusing on the ergonomic design of VR devices to accommodate the unique needs of palliative care patients, ensuring that interventions are accessible and practical for all patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bandieri, E.; Borelli, E.; Bigi, S.; Mucciarini, C.; Gilioli, F.; Ferrari, U.; Eliardo, S.; Luppi, M.; Potenza, L. Positive Psychological Well-Being in Early Palliative Care: A Narrative Review of the Roles of Hope, Gratitude, and Death Acceptance. Curr. Oncol. 2024, 31, 672–684. [Google Scholar] [CrossRef] [PubMed]
- Truong, Q.X.N.; Than, T.N.H.; Le Dai, D.; Duong, K.D.D.; Herman, B.; Taneepanichskul, S. Anxiety and Depression in Palliative Care Cancer Patients in Vietnam: Baseline Data from a Randomized Controlled Trial of Multidisciplinary Palliative Care Versus Standard Care. J. Health Res. 2023, 38, 2–115. [Google Scholar] [CrossRef]
- Seven, A.; Sert, H. Anxiety, Dyspnea Management, and Quality of Life in Palliative Care Patients: A Randomized Controlled Trial. Florence Nightingale J. Nurs. 2023, 31 (Suppl. S1), S13–S21. [Google Scholar] [CrossRef] [PubMed]
- Garcia, G.S.G.; Meira, K.C.; de Souza, A.H.; Guimarães, N.S. Anxiety and Depression Disorders in Oncological Patients under Palliative Care at a Hospital Service: A Cross-Sectional Study. BMC Palliat. Care 2023, 22, 116. [Google Scholar] [CrossRef]
- Wulandari, F.; Nurachmah, E. Efektivitas Intervensi Relaksasi Imaginasi Terbimbing Terhadap Penurunan Kecemasan Dan Nyeri Pada Pasien Paliatif. J. Pharm. Health Res. 2022, 3, 106–111. [Google Scholar] [CrossRef]
- Gonzalez-Ling, A.; Vázquez, O.G.; Bello, M.E.; Robles, R.; Rascón-Gasca, M.L.; Lara-Mejía, L.; Heredia, D.; Arrieta, O. Quality of Life, Anxiety, Depression, and Distress in Patients with Advanced and Metastatic Lung Cancer. Palliat. Support. Care 2022, 21, 608–615. [Google Scholar] [CrossRef]
- Chiaramonte, D. All Palliative Care Should Be Integrative Palliative Care. J. Pain Palliat. Care Pharmacother. 2024, 38, 287–291. [Google Scholar] [CrossRef]
- Mattai, S.A.D.; Hui, K.-K.P. Reframing Palliative Care: An East-West Integrative Palliative Care Model. Chin. J. Integr. Med. 2021, 27, 723–728. [Google Scholar] [CrossRef]
- Kustiyati, S.; Fajri, I.K.; Masithoh, R.F.; Dewi, R.D.C.; Nurseha, N. Towards Holistic Healthcare: Integrating Traditional and Modern Medicine for Improved Patient Outcomes. Glob. Int. J. Innov. Res. 2024, 2, 942–951. [Google Scholar] [CrossRef]
- Wijnen, J.; Gordon, N.L.; Hullenaar, G.v.; Pont, M.L.; Geijselaers, M.W.H.; Van Oosterwijck, J.; de Jong, J. An Interdisciplinary Multimodal Integrative Healthcare Program for Depressive and Anxiety Disorders. Front. Psychiatry 2023, 14, 1113356. [Google Scholar] [CrossRef]
- Carlson, L.E.; Ismaila, N.; Addington, E.L.; Asher, G.N.; Atreya, C.; Balneaves, L.G.; Bradt, J.; Fuller-Shavel, N.; Goodman, J.; Hoffman, C.J.; et al. Integrative Oncology Care of Symptoms of Anxiety and Depression in Adults With Cancer: Society for Integrative Oncology–ASCO Guideline. J. Clin. Oncol. 2023, 41, 4562–4591. [Google Scholar] [CrossRef] [PubMed]
- Zoogman, S.; Goldberg, S.B.; Vousoura, E.; Diamond, M.C.; Miller, L. Effect of Yoga-Based Interventions for Anxiety Symptoms: A Meta-Analysis of Randomized Controlled Trials. Spiritual. Clin. Pract. 2019, 6, 256–278. [Google Scholar] [CrossRef]
- Bruce, A. Carnes How Long Must Humans Live. J. Gerontol. Geriatr. Res. 2015, 69, 965–970. [Google Scholar] [CrossRef]
- McDonald, A.; Burjan, E.; Martin, S. Yoga for Patients and Carers in a Palliative Day Care Setting. Int. J. Palliat. Nurs. 2006, 12, 519–523. [Google Scholar] [CrossRef]
- Thakar, N.; Jani, S.; Panchal, D. Harnessing the Power of Yoga: An Integrative Review on Anxiety Management. Int. Res. J. Ayurveda Yoga 2024, 7, 14–18. [Google Scholar] [CrossRef]
- Yadav, M.; Kumar, A.; Shandil, A. Therapeutic Mechanisms of Gut Microbiota and Probiotics in the Management of Mental Disorders; Springer Nature: Berlin/Heidelberg, Germany, 2022; Volume 4, ISBN 978-981166760-2. [Google Scholar]
- Pardini, S.; Gabrielli, S.; Olivetto, S.; Fusina, F.; Dianti, M.; Forti, S.; Lancini, C.; Novara, C. Personalized, Naturalistic Virtual Reality Scenarios Coupled with Web-Based Progressive Muscle Relaxation Training for the General Population: Protocol for a Proof-of-Principle Randomized Controlled Trial. JMIR Res. Protoc. 2023, 12, e44183. [Google Scholar] [CrossRef]
- Suseno, B.; Hastjarjo, T.D. The Effect of Simulated Natural Environments in Virtual Reality and 2D Video to Reduce Stress. Front. Psychol. 2023, 14, 1016652. [Google Scholar] [CrossRef]
- Mathias, E.G.; Pai, M.S.; Bramhagen, A.-C. Effect of Distraction Interventions on Anxiety in Children Undergoing Surgery: A Meta-Analysis. J. Health Allied Sci. NU 2022, 13, 323–331. [Google Scholar] [CrossRef]
- Cáceres-Matos, R.; Castillo-García, M.; Magni, E.; Pabón-Carrasco, M. Effectiveness of Virtual Reality for Managing Pain, Fear, and Anxiety in Children and Adolescents Undergoing Needle-Related Procedures: Systematic Review with Meta-Analysis. Nurs. Rep. 2024, 14, 2456–2484. [Google Scholar] [CrossRef]
- Priyadarshini, S.; Agarwala, S.; Priya, H.; Jain, V.; Goel, P.; Dhua, A.K.; Yadav, D.K.; Anand, S.; Patel, N. Is Virtual Reality Effective in Decreasing Pain during Clinical Procedures among Children: A Systematic Review and Meta-Analysis. J. Indian Assoc. Pediatr. Surg. 2024, 29, 465–478. [Google Scholar] [CrossRef]
- Hudson, S.; Rajagopal, M.; Gourlay, K.; Hartling, L.; Stinson, J.; Ma, K.; Vandermeer, B.; Schreiner, K.; Ali, S. 32 A Randomized Controlled Trial of Virtual Reality-Based Distraction for Intravenous Cannulation-Related Distress in Children. Paediatr. Child Health 2024, 29, e15. [Google Scholar] [CrossRef]
- Tippelt, L.; Sommer, F.; Schmid, S.; Theodoraki, M.N.; Laban, S.; Emmanuel, B.; Coburger, J.; Hoffmann, T.K.; Schuler, P.J. Intraoperative Use of Virtual Reality Decreases Anxiety during Surgery under Local Anaesthesia in the Head and Neck Region. Virtual Real. 2024, 28, 323–331. [Google Scholar] [CrossRef]
- Bashir, Z.S.; Misquith, C.; Has, P.; Bukhari, S.M. The Effectiveness of Virtual Reality on Anxiety and Pain Management in Patients Undergoing Cardiac Procedures: A Systematic Review and Meta-Analysis. Cureus 2024, 16, e57557. [Google Scholar] [CrossRef] [PubMed]
- el Mathari, S.; Hoekman, A.; Kharbanda, R.K.; Sadeghi, A.H.; Wijngaarden, R.d.L.v.; Götte, M.; Klautz, R.J.; Kluin, J. Virtual Reality for Pain and Anxiety Management in Cardiac Surgery and Interventional Cardiology. JACC Adv. 2024, 3, 100814. [Google Scholar] [CrossRef]
- Ghobadi, A.; Moradpoor, H.; Sharini, H.; Khazaie, H.; Moradpoor, P. The Effect of Virtual Reality on Reducing Patient’s Anxiety and Pain during Dental Implant Surgery. BMC Oral Health 2024, 24, 186. [Google Scholar] [CrossRef]
- Devan, A.; Hegde, S.; Bhat, S.S.; Ballal, R.; HT, A.R.; Harshitha, K. Effectiveness of Virtual Reality Eyeglasses as a Distraction Technique in Managing Anxious Paediatric Patients Undergoing Dental Treatment—A Cross-Sectional Study. Int. J. Oral Health Dent. 2021, 7, 131–137. [Google Scholar] [CrossRef]
- Lu, M.; Song, Y.; Niu, Y.; Liu, T.; Ge, S.; Sun, Y.; Wang, X.; Luo, Y.; Li, K.; Yang, X. Effectiveness of Virtual Reality in the Management of Anxiety and Pain Peri-Treatment for Breast Cancer: A Systematic Review and Meta-Analysis. J. Nurs. Res. 2024, 32, e343. [Google Scholar] [CrossRef]
- Nerini, C.; Burk, S.; Andretta, E.; Chirico, A.; Giordano, A. The Effects of Virtual Reality on Pain and Anxiety in Pediatric Oncology Patients. Ann. Res. Oncol. 2024, 4, 29. [Google Scholar] [CrossRef]
- Adeghe, E.P.; Okolo, C.A.; Ojeyinka, O.T. A Review of the Integration of Virtual Reality in Healthcare: Implications for Patient Education and Treatment Outcomes. Int. J. Sci. Technol. Res. Arch. 2024, 6, 79–88. [Google Scholar] [CrossRef]
- Gerlach, C.; Haas, L.; Greinacher, A.; Lantelme, J.; Guenther, M.; Thiesbonenkamp-Maag, J.; Alt-Epping, B.; Wrzus, C. My Virtual Escape from Patient Life: A Feasibility Study on the Experiences and Benefits of Individualized Virtual Reality for Inpatients in Palliative Cancer Care. BMC Palliat. Care 2024, 23, 247. [Google Scholar] [CrossRef]
- Huang, T.; Wang, W. Relationship between Fear of Evaluation, Ambivalence over Emotional Expression, and Self-Compassion among University Students. BMC Psychol. 2024, 12, 128. [Google Scholar] [CrossRef] [PubMed]
- Corvin, J.; Hoskinson, Z.; Mozolic-Staunton, B.; Hattingh, L.; Plumbridge-Jones, R. The Effects of Virtual Reality Interventions on Occupational Participation and Distress from Symptoms in Palliative Care Patients: A Pilot Study. Palliat. Support. Care 2024, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Brungardt, A.; Wibben, A.; Shanbhag, P.; Boeldt, D.; Youngwerth, J.; Tompkins, A.; Rolbiecki, A.J.; Coats, H.; LaGasse, A.B.; Kutner, J.S.; et al. Patient Outcomes of a Virtual Reality-Based Music Therapy Pilot in Palliative Care. Palliat. Med. Rep. 2024, 5, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Liszio, S.; Bäuerlein, F.; Hildebrand, J.; van Nahl, C.; Masuch, M.; Basu, O. Cooperative Virtual Reality Gaming for Anxiety and Pain Reduction in Pediatric Patients and Their Caregivers during Painful Medical Procedures: Research Protocol for a Randomized Control Trial. JMIR Prepr. 2024. [Google Scholar] [CrossRef]
- Mitello, L.; Marti, F.; Mauro, L.; Siano, L.; Pucci, A.; Tarantino, C.; Rocco, G.; Stievano, A.; Iacorossi, L.; Anastasi, G.; et al. The Usefulness of Virtual Reality in Symptom Management during Chemotherapy in Lung Cancer Patients: A Quasi-Experimental Study. J. Clin. Med. 2024, 13, 4374. [Google Scholar] [CrossRef]
- Li, M.; Yu, Z.; Li, H.; Cao, L.; Yu, H.; Deng, N.; Liu, Y. Effects of Virtual Reality Therapy for Patients with Breast Cancer During Chemotherapy: Randomized Controlled Trial. JMIR Serious Games 2024, 12, e53825. [Google Scholar] [CrossRef]
- Carneiro, L.; Araújo, F.; Oliveira, A.; Brito-Costa, S.; Amaral, A.P. Improving the Well-Being of Cancer Hospitalized Patients: SENTIR Meditation Program. Confin. Cephalalgica 2023, 33, e2023010. [Google Scholar]
- Herwest, S.; Bozem, A.; Iggena, D.; Kowski, A.; Willert, A.-C.; Ploner, C.; Finke, C. Virtual Reality Treatment in a Neuro-Palliative Care Unit (P5-6.002). Neurology 2024, 102, 5453. [Google Scholar] [CrossRef]
- Siriborvornratanakul, T. A Study of Virtual Reality Headsets and Physiological Extension Possibilities. In Computational Science and Its Applications–ICCSA 2016, Proceedings of the 16th International Conference, Beijing, China, 4–7 July 2016; Proceedings, Part II; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 497–508. ISBN 978-973-319-42107-0. [Google Scholar]
- Odell, D.; Dorbala, N. The Effects of Head Mounted Weight on Comfort for Helmets and Headsets, with a Definition of “Comfortable Wear Time”. Work 2023, 7, 651–658. [Google Scholar] [CrossRef]
- Ito, K.; Tada, M.; Ujike, H.; Hyodo, K. Effects of the Weight and Balance of Head-Mounted Displays on Physical Load. Appl. Sci. 2021, 11, 6802. [Google Scholar] [CrossRef]
- Zhuang, J.; Liu, Y.; Jia, Y.; Huang, Y. User Discomfort Evaluation Research on the Weight and Wearing Mode of Head-Wearable Device. In Advances in Human Factors in Wearable Technologies and Game Design, Proceedings of the AHFE 2018 International Conferences on Human Factors and Wearable Technologies, and Human Factors in Game Design and Virtual Environments, 21–25 July 2018, in Loews Sapphire Falls Resort at Universal Studios, Orlando, Florida, USA; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 98–110. [Google Scholar]
- Yan, Y.; Chen, K.; Xie, Y.; Song, Y.; Liu, Y. The Effects of Weight on Comfort of Virtual Reality Devices. In Advances in Ergonomics in Design, Proceedings of the AHFE 2018 International Conference on Ergonomics in Design, 21–25 July 2018, Loews Sapphire Falls Resort at Universal Studios, Orlando, Florida, USA; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 239–248. [Google Scholar]
- Woo, O.K.L.; Lee, A.M. Case Report: Therapeutic Potential of Flourishing-Life-Of-Wish Virtual Reality Therapy on Relaxation (FLOW-VRT-Relaxation)—A Novel Personalized Relaxation in Palliative Care. Front. Digit. Health 2023, 5, 1228781. [Google Scholar] [CrossRef] [PubMed]
- Koulieris, G.-A.; Bui, B.; Banks, M.S.; Drettakis, G. Accommodation and Comfort in Head-Mounted Displays. ACM Trans. Graph. 2017, 36, 87. [Google Scholar] [CrossRef]
- Rachmawati, A.K.; Tornando, H. Challenges in Consumer Adaptation to Immersive Technologies: A Comprehensive Literature Review. eCo-Buss 2024, 7, 317–328. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024); Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., Welch, V., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Lloyd, A.; Haraldsdottir, E. Virtual Reality in Hospice: Improved Patient Well-Being. BMJ Support. Palliat. Care 2021, 11, 344–350. [Google Scholar] [CrossRef]
- Nwosu, A.C.; Mills, M.; Roughneen, S.; Stanley, S.; Chapman, L.; Mason, S.R. Virtual Reality in Specialist Palliative Care: A Feasibility Study to Enable Clinical Practice Adoption. BMJ Support. Palliat. Care 2024, 14, 47–51. [Google Scholar] [CrossRef]
- Schrempf, M.C.; Petzold, J.; Petersen, M.A.; Arndt, T.T.; Schiele, S.; Vachon, H.; Vlasenko, D.; Wolf, S.; Anthuber, M.; Müller, G.; et al. A Randomised Pilot Trial of Virtual Reality-Based Relaxation for Enhancement of Perioperative Well-Being, Mood and Quality of Life. Sci. Rep. 2022, 12, 12067. [Google Scholar] [CrossRef]
- O’Gara, G.; Murray, L.; Georgopoulou, S.; Anstiss, T.; Macquarrie, A.; Wheatstone, P.; Bellman, B.; Gilbert, P.; Steed, A.; Wiseman, T. SafeSpace: What Is the Feasibility and Acceptability of a Codesigned Virtual Reality Intervention, Incorporating Compassionate Mind Training, to Support People Undergoing Cancer Treatment in a Clinical Setting? BMJ Open 2022, 12, e047626. [Google Scholar] [CrossRef]
- Burridge, N.; Sillence, A.; Teape, L.; Clark, B.; Bruce, E.; Armoogum, J.; Leloch, D.; Spathis, A.; Etkind, S. Virtual Reality Reduces Anxiety and Pain in Acute Hospital Palliative Care: Service Evaluation. BMJ Support. Palliat. Care 2023. [Google Scholar] [CrossRef]
- Kupczik, L.; Farrelly, W.; Wilson, S. Appraising Virtual Technologies’ Impact on Older Citizens’ Mental Health-A Comparative between 360° Video and Virtual Reality. Int. J. Environ. Res. Public Health 2022, 19, 11250. [Google Scholar] [CrossRef] [PubMed]
- Moscato, S.; Sichi, V.; Giannelli, A.; Palumbo, P.; Ostan, R.; Varani, S.; Pannuti, R.; Chiari, L. Virtual Reality in Home Palliative Care: Brief Report on the Effect on Cancer-Related Symptomatology. Front. Psychol. 2021, 12, 709154. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, S.A.; Fisher, H.M.; Winger, J.G.; Miller, S.N.; Amaden, G.H.; Somers, T.J.; Colloca, L.; Uronis, H.E.; Keefe, F.J. Virtual Reality for Improving Pain and Pain-Related Symptoms in Patients with Advanced Stage Colorectal Cancer: A Pilot Trial to Test Feasibility and Acceptability. Palliat. Support. Care 2022, 20, 471–481. [Google Scholar] [CrossRef]
- Greinacher, A.; Alt-Epping, B.; Gerlach, C.; Wrzus, C. Expected Benefits and Concerns Regarding Virtual Reality in Caring for Terminally Ill Cancer Patients—A Qualitative Interview Study. BMC Palliat. Care 2024, 23, 254. [Google Scholar] [CrossRef]
- McAnirlin, O.; Thrift, J.; Li, F.; Pope, J.K.; Browning, M.H.E.M.; Moutogiannis, P.P.; Thomas, G.; Farrell, E.; Evatt, M.M.; Fasolino, T. The Tandem VRTM Protocol: Synchronized Nature-Based and Other Outdoor Experiences in Virtual Reality for Hospice Patients and Their Caregivers. Contemp. Clin. Trials Commun. 2024, 40, 101318. [Google Scholar] [CrossRef]
- Deming, J.R.; Dunbar, K.J.; Lueck, J.F.; Oh, Y. Virtual Reality Videos for Symptom Management in Hospice and Palliative Care. Mayo Clin. Proc. Digit. Health 2024, 2, 477–485. [Google Scholar] [CrossRef]
- Guenther, M.; Görlich, D.; Bernhardt, F.; Pogatzki-Zahn, E.; Dasch, B.; Krueger, J.; Lenz, P. Virtual Reality Reduces Pain in Palliative Care–A Feasibility Trial. BMC Palliat. Care 2022, 21, 169. [Google Scholar] [CrossRef]
- Ahmadpour, N.; Keep, M.; Janssen, A.; Rouf, A.; Marthick, M. Design Strategies for Virtual Reality Interventions for Managing Pain and Anxiety in Children and Adolescents: Scoping Review. JMIR Serious Games 2020, 8, e14565. [Google Scholar] [CrossRef]
- Ioannou, A.; Papastavrou, E.; Avraamides, M.N.; Charalambous, A. Virtual Reality and Symptoms Management of Anxiety, Depression, Fatigue, and Pain: A Systematic Review. Sage Open Nurs. 2020, 6, 2377960820936163. [Google Scholar] [CrossRef]
- Kremeike, K.; Frerich, G.; Romotzky, V.; Boström, K.; Dojan, T.; Galushko, M.; Shah-Hosseini, K.; Jünger, S.; Rodin, G.; Pfaff, H.; et al. The Desire to Die in Palliative Care: A Sequential Mixed Methods Study to Develop a Semi-Structured Clinical Approach. BMC Palliat. Care 2020, 19, 49. [Google Scholar] [CrossRef]
- Seuling, P.D.; Czernin, N.S.; Schiele, M.A. Virtual Reality Exposure Therapy in the Treatment of Public Speaking Anxiety and Social Anxiety Disorder. Neurosci. Appl. 2024, 2024, 104074. [Google Scholar] [CrossRef]
- Goetter, E.M.; Yuen, E.K. Technological Advances in Treating Anxiety Disorders. Psychiatr. Clin. N. Am. 2024, 47, 813–827. [Google Scholar] [CrossRef] [PubMed]
- Moloney, M.; Doody, O.; O’reilly, M.; Lucey, M.; Callinan, J.; Exton, C.; Colreavy, S.; O’mahony, F.; Meskell, P.; Coffey, A. Virtual Reality Use and Patient Outcomes in Palliative Care: A Scoping Review. Digit. Health 2023, 9, 7574. [Google Scholar] [CrossRef] [PubMed]
- Carmont, H.; McIlfatrick, S. Using Virtual Reality in Palliative Care: A Systematic Integrative Review. Int. J. Palliat. Nurs. 2022, 28 3, 132–144. [Google Scholar] [CrossRef]
- Ong, C.-K.; Forbes, D. Embracing Cicely Saunders’s Concept of Total Pain. BMJ 2005, 331, 576. [Google Scholar] [CrossRef]
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | Patients receiving palliative/hospice care. | Studies not focused on palliative care settings. |
| Intervention | Receiving immersive VR HMD interventions. | Non-immersive VR interventions. |
| Comparator | Standard care, waitlist, placebo, or other non-VR interventions; single-arm pilot trials. | Studies without a comparator group or with insufficient control conditions (e.g., case reports). |
| Outcome | Anxiety, stress, or psychological distress assessed via validated psychometric tools. | Studies without outcomes related to anxiety, stress, or psychological distress. |
| Study design | Randomized controlled trials (RCTs), pilot studies, or feasibility trials published in peer-reviewed journals. | Observational studies, conference abstracts, posters, reviews, commentaries, editorials, or letters. |
| Language | Studies published in English due to resource constraints for accurate translation. | Non-English publications. |
| Database | Search Phrase Terms |
|---|---|
| PubMed/ MEDLINE | (“virtual reality”[MeSH] OR “virtual reality” OR “VR” OR “immersive experience” OR “computer-generated environment” OR “simulated environment”) AND (“anxiety”[MeSH] OR “anxiety” OR “psychological distress” OR “stress” OR “fear”) AND (“palliative care”[MeSH] OR “palliative care” OR “hospice care”[MeSH] OR “hospice” OR “end-of-life care”) |
| PsycINFO | (“virtual reality” OR “VR” OR “immersive technology” OR “simulated environment” OR “virtual therapy”) AND (“anxiety” OR “fear” OR “psychological distress” OR “mental stress”) AND (“palliative care” OR “hospice” OR “end-of-life care” OR “terminal care”) AND (“outcome” OR “impact” OR “effect” OR “efficacy” OR “effectiveness”) |
| EMBASE | (‘virtual reality’/exp OR ‘VR’ OR ‘immersive technology’ OR ‘simulated environment’ OR ‘computer simulation’) AND (‘anxiety’/exp OR ‘psychological distress’ OR ‘fear’ OR ‘stress’) AND (‘palliative care’/exp OR ‘hospice care’ OR ‘end-of-life care’ OR ‘terminal care’) AND (‘treatment outcome’/exp OR ‘efficacy’ OR ‘effectiveness’ OR ‘impact’) |
| CINAHL | (MH “Virtual Reality” OR “VR” OR “immersive technology” OR “virtual environment”) AND (MH “Anxiety” OR “psychological distress” OR “fear” OR “stress”) AND (MH “Palliative Care” OR “hospice” OR “end-of-life care”) AND (MH “Treatment Outcomes” OR “effect” OR “efficacy” OR “impact”) |
| Cochrane Library | (virtual reality OR immersive technology OR virtual environment) AND (anxiety OR psychological stress OR fear) AND (palliative care OR hospice OR end-of-life) AND (outcome OR impact OR effect OR efficacy) |
| PsycARTICLES | (“virtual reality” OR “VR” OR “immersive technology”) AND (“anxiety” OR “psychological distress” OR “fear” OR “stress”) AND (“palliative care” OR “hospice” OR “terminal care” OR “end-of-life care”) AND (“effectiveness” OR “efficacy” OR “outcome” OR “impact”) |
| ProQuest Psychology Database | (“virtual reality” OR “VR” OR “immersive technology”) AND (“anxiety” OR “stress” OR “fear” OR “psychological distress”) AND (“palliative care” OR “hospice” OR “end-of-life care”) AND (“outcome” OR “impact” OR “efficacy” OR “effectiveness”) AND (“clinical trial” OR “randomized controlled trial” OR “case report”) NOT (“literature review” OR “systematic review” OR “meta-analysis”) |
| Web of Science | (TS = (“virtual reality” OR “VR” OR “immersive technology”)) AND (TS = (“anxiety” OR “psychological distress” OR “fear” OR “stress”)) AND (TS = (“palliative care” OR “hospice” OR “end-of-life care”)) AND (TS = (“outcome” OR “impact” OR “efficacy”)) |
| Scopus | (TITLE-ABS-KEY(“virtual reality” OR “VR” OR “immersive technology”)) AND (TITLE-ABS-KEY(“anxiety” OR “stress” OR “fear” OR “psychological distress”)) AND (TITLE-ABS-KEY(“palliative care” OR “hospice” OR “end-of-life care”)) AND (TITLE-ABS-KEY(“outcome” OR “impact” OR “efficacy” OR “effectiveness”)) |
| Category | Detail Sheet |
|---|---|
| Study description: | Author, publication year, study design (e.g., RCT, pilot study, feasibility trial) |
| Participant demographics: | Number of participants, age group, population (i.e., advanced cancer, hospice care) |
| VR intervention: | VR hardware, software, type of VR, number of sessions, duration of interventions, customization |
| Anxiety-linked outcomes: | Psychometric outcome measures (e.g., Hospital Anxiety and Depression Scale [HADS], Generalized Anxiety Disorder-7 [GAD-7]) and other anxiety-specific outcome measures |
| Secondary outcomes: | Other secondary outcomes, like pain relief, improved quality of life, and physiological parameters (e.g., heart and/or respiratory rate) |
| Authors | Study Design; Participants (n *) | VR Intervention: Hardware, Software, Duration | Psychometric and Physical Evaluation of Anxiety |
|---|---|---|---|
| Gerlach et al. (2024) [31] | Feasibility study; inpatients in palliative cancer care (n = 12) | VR with personalized settings such as patient-selected home environments; 15–20 min per session. | Anxiety and well-being assessed pre- and post-intervention; reported significant increase in comfort with reduction in emotional burden and anxiety levels. |
| Brungardt et al. (2024) [34] | Pilot study; hospitalized palliative care patients (n = 20) | VR HMD combined with music therapy; 25 min sessions using serene auditory–visual experiences. | Symptom distress measured with quality-of-life scores improved moderately; psychological stress and anxiety reduced based on self-report scales. |
| Lloyd and Haraldsdottir (2021) [51] | Qualitative study; VRG (n = 19) | 30 min VR session using “room-scale” VR with participant-chosen locations (e.g., childhood home, holiday spots). Guided by an experienced facilitator to create personalized experiences. | Positive impact observed: Participants reported fulfilling experiences and meaningful memories. Mild negative responses were rare. |
| Nwosu et al. (2021) [52] | Qualitative study; VRG (n = 15) | Samsung Gear VR system with options for (1) a 5 min beach relaxation video, (2) a 10 min forest meditation, or (3) a 5 min rollercoaster ride. | High acceptance rate: 93.3% of participants had positive experiences, preferring the forest and beach scenes. Minor issues included headset weight and focus adjustments. |
| Schrempf et al. (2022) [53] | Pilot study; VRG (n = 54) | Oculus Go with TRIPP (TRIPP Inc., Los Angeles, USA, www.tripp.com; accessed on 10 December 2024) software. Two daily sessions: morning (7–8 min) with breathing exercises and evening (10 min) calming sessions with interactive breath visualization. | Statistically significant reductions in anxiety and physical markers: higher contentment (+19.3%), calmness (+16.3%), relaxation (+28.2%); lower heart rate (−1.3 bpm) and respiratory rate (−0.6 bpm; 26.4% reduction in anxiety post-intervention. |
| O’Gara et al. (2022) [54] | Two-phase study; VRG1 (n = 20), VRG2 (n = 16), VRG3 (n = 13) | Three progressive VR sessions using compassionate mind training (CMT). VR1 familiarized participants with VR; VR2 included breathing exercises; VR3 introduced CMT with a choice of beach, mountain, or forest environments. | Significant mood (POMS) and mental well-being (WEMWBS) improvements across sessions. VR3 showed a consistent beneficial effect and a statistically significant increase in WEMWBS scores from baseline to VR3. The final session significantly reduced stress levels (DASS21, p = 0.03). |
| Burridge et al. (2022) [55] | Qualitative study; VR Group (n = 28) | DR.VR Immersive Therapeutic System (DR VR., Rescape Health, https://www.rescape.health/news/drvrfrontline-0; accessed on 10 December 2024) has options for short 7.5 min experiences (e.g., walk on the beach, swim underwater, meditation). | Mean anxiety scores decreased by 40% (p < 0.001; mean anxiety score decreased from 4.43 to 2.65), and mean pain scores by 29% immediately post-intervention. All participants rated the experience positively and would recommend it to others. |
| Kupczik et al. (2022) [56] | Qualitative study; VRG (n = 20) | HTC Vive HMD with two immersive experiences: (A) a 360° video of a walk through a sanctuary or (B) interactive woodland and beach scenes with object interaction (e.g., rocks, shells). | A total of 85% preferred the VR experience due to its interactivity and greater realism than the 360° video. Higher immersion scores were linked to the freedom to interact with the environment in VR, which significantly increased participant immersion and engagement. |
| Moscato et al. (2021) [57] | Feasibility study; home-based palliative care cancer patients (n = 25) | VR HMD with individualized content; 30 min sessions tailored to personal interests and comforting environments. | Anxiety and pain levels were measured pre- and post-session, showing a statistically significant reduction in anxiety and improvement in overall well-being. |
| Kelleher et al. (2022) [58] | Pilot trial; advanced colorectal cancer patients in palliative care (n = 15) | VR HMD focused on guided meditative environments for pain and anxiety reduction; 20 min sessions daily. | Pain and anxiety measured pre- and post-session indicating substantial reduction; results support VR as a complementary therapy for pain management. |
| Greinacher et al. (2024) [59] | Qualitative study; terminally ill cancer patients (n = 18) | Interviews exploring patient perspectives on VR; sessions used calming, customized VR content in 30 min blocks. | Interviews revealed positive patient feedback, with VR seen as effective for distraction, emotional relief, and reducing anxiety. |
| McAnirlin et al. (2024) [60] | Protocol study; hospice patient–caregiver dyads (n = 30) | Tandem VR™ (Virtual Nature Lab, https://www.virtualnaturelab.org/tandemvr; accessed on 10 December 2024) using synchronized nature-based content for both patients and caregivers; 30 min sessions. | Psychological measures showed improvements in anxiety and quality of life; also noted reduction in fear of death and enhanced emotional support for caregivers. |
| Deming et al. (2024) [61] | Prospective study; hospice patients (n = 28) | VR with serene nature video content for calming effects; 15 min sessions twice daily. | Anxiety and depression measured with psychometric tools showed a 30% reduction in anxiety scores and improved well-being after consistent VR exposure. |
| Study | Randomization Process | Deviations from Interventions | Missing Data | Outcome Measurement | Selective Reporting | Overall Bias | Summary of Justifications |
|---|---|---|---|---|---|---|---|
| Gerlach et al. (2024) [31] | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Clear randomization and adherence protocol. Outcome measures are complete and consistently applied, with no selective reporting identified. |
| Corvin et al. (2024) [33] | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Some Concerns | Randomization lacks full transparency. Adherence checks are robust, but selective reporting concerns exist for some secondary measures, potentially impacting outcome interpretation. |
| Brungardt et al. (2024) [34] | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Randomization process clearly documented with strong adherence monitoring. Anxiety and quality of life outcomes fully reported without bias. |
| Nwosu et al. (2021) [52] | Some Concerns | Some Concerns | Low Risk | Some Concerns | Some Concerns | Some Concerns | The randomization process is not fully detailed, with minor deviations noted. All outcomes are generally reported, though reporting completeness is unclear for some qualitative feedback. |
| Schrempf et al. (2022) [53] | Low risk | Low risk | Low risk | Low Risk | Some Concerns | Low risk | The study is well designed with robust randomization, high adherence, and consistent outcome measures. Minor concerns about selective reporting were noted, but they do not detract from the study’s overall validity. |
| O’Gara et al. (2022) [54] | Some Concerns | Low Risk | Low Risk | Low Risk | Low Risk | Some Concerns | Randomization is limitedly transparent. The intervention is consistent across participants, with minimal missing data. However, there are some concerns over selective reporting clarity. |
| Burridge et al. (2023) [55] | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Well-implemented randomization, with robust checks on adherence and precise outcomes. They report full anxiety and pain results pre- and post-intervention without selective reporting. |
| Kupczik et al. (2022) [56] | Some Concerns | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Randomization lacks detail, and minor adherence issues were noted. Outcomes are measured thoroughly, though minor selective reporting concerns remain in the feedback results. |
| Moscato et al. (2021) [57] | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Some Concerns | Limited transparency in randomization process, but adherence is well managed. Outcome measures are consistent; some concerns over selective reporting due to limited secondary outcome detail. |
| Kelleher et al. (2022) [58] | Low Risk | Low Risk | Low Risk | Low Risk | Some Concerns | Low Risk | Strong randomization and outcome reporting. Minor concerns regarding selective reporting of secondary outcomes, but primary results are clear and well-supported. |
| McAnirlin et al. (2024) [60] | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Some Concerns | Limited details on randomization; consistent adherence and outcome measurement, though selective reporting on some secondary outcomes. Results are reliable for primary measures. |
| Deming et al. (2024) [61] | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Thorough randomization and adherence tracking. Full reporting on anxiety and depression measures with no bias or selective reporting noted. |
| Guenther et al. (2022) [62] | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Some Concerns | Some concerns in randomization detail and selective reporting were noted. Adherence is high, and outcome measures are reliably assessed with consistent reporting of results. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaina, A.-M.; Stefanescu, C.; Szalontay, A.-S.; Gaina, M.-A.; Poroch, V.; Mosoiu, D.V.; Stefanescu, B.-V.; Axinte, M.; Tofan, C.-M.; Magurianu, L.A. A Systematic Review of Virtual Reality’s Impact on Anxiety During Palliative Care. Healthcare 2024, 12, 2517. https://doi.org/10.3390/healthcare12242517
Gaina A-M, Stefanescu C, Szalontay A-S, Gaina M-A, Poroch V, Mosoiu DV, Stefanescu B-V, Axinte M, Tofan C-M, Magurianu LA. A Systematic Review of Virtual Reality’s Impact on Anxiety During Palliative Care. Healthcare. 2024; 12(24):2517. https://doi.org/10.3390/healthcare12242517
Chicago/Turabian StyleGaina, Alexandra-Maria, Cristinel Stefanescu, Andreea-Silvana Szalontay, Marcel-Alexandru Gaina, Vladimir Poroch, Daniela Viorica Mosoiu, Bogdan-Victor Stefanescu, Magdalena Axinte, Cristina-Maria Tofan, and Liviu Adrian Magurianu. 2024. "A Systematic Review of Virtual Reality’s Impact on Anxiety During Palliative Care" Healthcare 12, no. 24: 2517. https://doi.org/10.3390/healthcare12242517
APA StyleGaina, A.-M., Stefanescu, C., Szalontay, A.-S., Gaina, M.-A., Poroch, V., Mosoiu, D. V., Stefanescu, B.-V., Axinte, M., Tofan, C.-M., & Magurianu, L. A. (2024). A Systematic Review of Virtual Reality’s Impact on Anxiety During Palliative Care. Healthcare, 12(24), 2517. https://doi.org/10.3390/healthcare12242517







