The Bleeding Must Be Stopped! Management in the Situation of Hemorrhages—A Prospective Randomized Controlled Prospective Simulation Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacobs, L.M.; Burns, K.J. Tourniquet application training for individuals with and without a medical background in a hospital setting. J. Trauma Acute Care Surg. 2015, 78, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mitra, B.; Tullio, F.; Cameron, P.A.; Fitzgerald, M. Trauma patients with the ‘triad of death’. Emerg. Med. J. 2012, 29, 622–625. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Hendrix, V.; Shapiro, M.; Duchesne, J.; Taghavi, S.; Schroll, R.; Tatum, D.; Guidry, C. Is the “Death Triad” a Casualty of Modern Damage Control Resuscitation. J. Surg. Res. 2021, 259, 393–398. [Google Scholar] [CrossRef] [PubMed]
- The Committee on Trauma. Atls Advanced Trauma Life Support: Student Course Manual; American College of Surgeons: Chicago, IL, USA, 2018; ISBN -13:9780996826235. [Google Scholar]
- National Association of Emergency Medical Technicians (NAEMT). Phtls: Prehospital Trauma Life Support; Jones & Bartlett Learning: Burlington, MA, USA, 2022; ISBN -13: 9781284272277. [Google Scholar]
- Alson, R.L.; Han, K.H.; Campbell, J.E. International Trauma Life Support for Emergency Care Providers; Pearson: London, UK, 2020. [Google Scholar]
- Smith, A.A.; Ochoa, J.E.; Wong, S.; Beatty, S.; Elder, J.; Guidry, C.; McGrew, P.; McGinness, C.; Duchesne, J.; Schroll, R. Prehospital tourniquet use in penetrating extremity trauma: Decreased blood transfusions and limb complications. J. Trauma Acute Care Surg. 2019, 86, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.M.; Coleman, M.; Parker, P.J. The evaluation of an abdominal aortic tourniquet for the control of pelvic and lower limb hemorrhage. Mil. Med. 2013, 178, 1196–1201. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, B.M.; Berben, S.A.; van Dongen, R.T.; Schoonhoven, L. Review on pharmacological pain management in trauma patients in (pre-hospital) emergency medicine in the Netherlands. Eur. J. Pain. 2014, 18, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Wiles, M.D. Blood pressure in trauma resuscitation: ‘Pop the clot’ vs. ‘drain the brain’? Anaesthesia 2017, 72, 1448–1455. [Google Scholar] [CrossRef] [PubMed]
- Sawhney, C.; Subramanian, A.; Kaur, M.; Anjum, A.; Albert, V.; Soni, K.D.; Kumar, A. Assessment of hemostatic changes after crystalloid and colloid fluid preloading in trauma patients using standard coagulation parameters and thromboelastography. Saudi. J. Anaesth. 2013, 7, 48–56. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lewis, S.R.; Pritchard, M.W.; Evans, D.J.; Butler, A.R.; Alderson, P.; Smith, A.F.; Roberts, I. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst. Rev. 2018, 8, CD000567. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kragh, J.F., Jr.; Walters, T.J.; Baer, D.G.; Fox, C.J.; Wade, C.E.; Salinas, J.; Holcomb, J.B. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann. Surg. 2009, 249, 1–7. [Google Scholar] [CrossRef] [PubMed]
- STB Home Page. Stop The Bleed. (n.d.). Retrieved 29 March 2023. Available online: https://www.stopthebleed.org/ (accessed on 31 May 2022).
- Baruch, E.N.; Benov, A.; Shina, A.; Berg, A.L.; Shlaifer, A.; Glassberg, E.; Aden, J.K., 3rd; Bader, T.; Kragh, J.F., Jr.; Yitzhak, A. Does practice make perfect? Prospectively comparing effects of 2 amounts of practice on tourniquet use performance. Am. J. Emerg. Med. 2016, 34, 2356–2361. [Google Scholar] [CrossRef] [PubMed]
- McCarty, J.C.; Hashmi, Z.G.; Herrera-Escobar, J.P.; De Jager, E.; Chaudhary, M.A.; Lipsitz, S.R.; Jarman, M.; Caterson, E.J.; Goralnick, E. Effectiveness of the American College of Surgeons Bleeding Control Basic Training Among Laypeople Applying Different Tourniquet Types: A Randomized Clinical Trial. JAMA Surg. 2019, 154, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Hart, S.G. Nasa-Task Load Index (NASA-TLX); 20 Years Later. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2006, 50, 904–908. [Google Scholar] [CrossRef]
- Hart, S.; Staveland, L. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Human Mental Workload; Hancock, P., Meshkati, N., Eds.; North Holland Press: Amsterdam, The Netherlands, 1988; pp. 139–183. [Google Scholar]
- Tsur, A.M.; Binyamin, Y.; Koren, L.; Ohayon, S.; Thompson, P.; Glassberg, E. High Tourniquet Failure Rates Among Non-Medical Personnel Do Not Improve with Tourniquet Training, Including Combat Stress Inoculation: A Randomized Controlled Trial. Prehospital Disaster Med. 2019, 34, 282–287. [Google Scholar] [CrossRef]
- Clumpner, B.R.; Polston, R.W.; Kragh, J.F., Jr.; Westmoreland, T.; Harcke, H.T.; Jones, J.A.; Dubick, M.A.; Baer, D.G.; Blackbourne, L.H. Single versus Double Routing of the Band in the Combat Application Tourniquet. J. Spec. Oper. Med. A Peer Rev. J. SOF Med. Prof. 2013, 13, 34–41. [Google Scholar] [CrossRef]
- Weppner, J.; Lang, M.; Sunday, R.; Debiasse, N. Efficacy of Tourniquets Exposed to the Afghanistan Combat Environment Stored in Individual First Aid Kits Versus on the Exterior of Plate Carriers. Mil. Med. 2013, 178, 334–337. [Google Scholar] [CrossRef]
- Brosnan, M.; Evans, W.; Brosnan, E.; Brown, G. Implementing objective structured clinical skills evaluation (OSCE) in nurse registration programmes in a centre in Ireland: A utilisation focused evaluation. Nurse Educ. Today 2006, 26, 115–122. [Google Scholar] [CrossRef]
- Taylor, D.; Quick, S. Students’ perceptions of a near-peer Objective Structured Clinical Examination (OSCE) in medical imaging. Radiography 2020, 26, 42–48. [Google Scholar] [CrossRef]
- Pasley, A.M.; Parker, B.M.; Levy, M.J.; Christiani, A.; Dubose, J.; Brenner, M.L.; Scalea, T.; Pasley, J.D. Stop the Bleed: Does the Training Work One Month Out? Am. Surg. 2018, 84, 1635–1638. [Google Scholar] [CrossRef]
- Dadario, N.B.; Felipes RC, S.; Cooney, J.V.; Stephenson, K.M.; Shleiwet, N.H.; Liang, T.; Jafri, F.N. The Impact of a Mobile Phone Application for Retention of Bleeding Control Skills. J. Surg. Res. 2021, 267, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Dunning, D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Personal. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Deb, N.; Roy, P. Prevalence of Dunning Kruger effect in first year medical students in a tertiary care hospital. Int. J. Community Med. Public Health 2021, 8, 5283–5287. [Google Scholar] [CrossRef]
- Dennis, A.; Bajani, F.; Schlanser, V.; Tatebe, L.C.; Impens, A.; Ivkovic, K.; Li, A.; Pickett, T.; Butler, C.; Kaminsky, M.; et al. Missing expectations: Windlass tourniquet use without formal training yields poor results. J. Trauma Acute Care Surg. 2019, 87, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
- Garner, S.-L.; Killingsworth, E.; Raj, L. Partnering to establish and study simulation in international nursing education. Nurse Educator. 2017, 42, 145–151. [Google Scholar] [CrossRef]
- Dieckmann, P.P.M. Variation and adaptation: Learning from success in patient safety-oriented simulation training. Adv. Simul. 2017, 31, 21. [Google Scholar] [CrossRef]
| Study Group (n = 49) | Control Group (n = 52) | p Value | |
|---|---|---|---|
| Year of study | 0.233 | ||
| 24 (49%) | 32 (61.5%) | |
| 25 (51%) | 20 (38.5%) | |
| Female sex | 36 (73.5%) | 37 (71.2%) | 0.827 |
| Effective bleeding control = proper use of tourniquet | 36 (73.5%) | 22 (42.3%) | 0.002 |
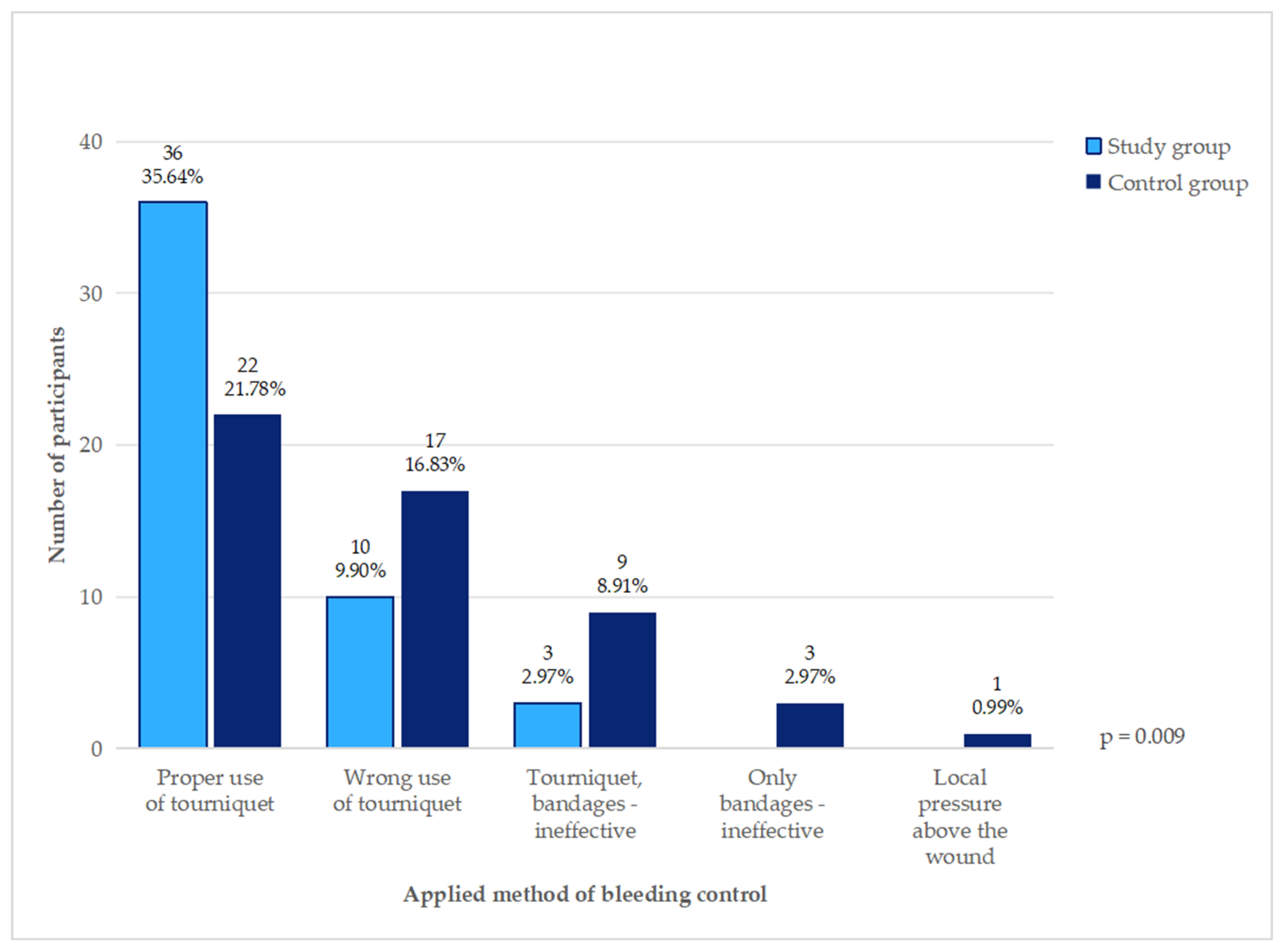
| Methods of bleeding control | 0.009 | ||
| 36 (73.5%) | 22 (42.3%) | |
| 10 (20.4%) | 17 (32.7%) | |
| 3 (6.1%) | 9 (17.3%) | |
| 0 | 3 (5.8%) | |
| 0 | 1 (1.9%) | |
| Use of tourniquet | 49 (100%) | 48 (92.3%) | 0.118 |
| 36/49 (73.5%) | 23/48 (47.9%) | 0.013 |
| 5/49 (10.2%) | 12/48 (25%) | |
| 1/49 (2%) | 2/48 (4.2%) | |
| 0 | 1/48 (2.1%) | |
| Blood loss (mL) | 32 (24) | 53 (26) | 0.013 |
| Time to effective bleeding control (minutes) | 1.07 (2.17) | 3.00 (2.15) | 0.034 |
| NASA scale | |||
| 55 (43) | 53 (40) | 0.827 |
| 55 (40) | 53 (35) | 0.705 |
| 65 (45) | 70 (25) | 0.283 |
| 20 (45) | 40 (34) | 0.036 |
| 50 (48) | 48 (55) | 0.731 |
| 55.1 (18.81) | 52.3 (17.39) | 0.44 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starosolski, M.; Kalemba, A.; Kaplan, C.; Majewska, K.; Ulbrich, K. The Bleeding Must Be Stopped! Management in the Situation of Hemorrhages—A Prospective Randomized Controlled Prospective Simulation Study. Healthcare 2024, 12, 2370. https://doi.org/10.3390/healthcare12232370
Starosolski M, Kalemba A, Kaplan C, Majewska K, Ulbrich K. The Bleeding Must Be Stopped! Management in the Situation of Hemorrhages—A Prospective Randomized Controlled Prospective Simulation Study. Healthcare. 2024; 12(23):2370. https://doi.org/10.3390/healthcare12232370
Chicago/Turabian StyleStarosolski, Michal, Alicja Kalemba, Cezary Kaplan, Karolina Majewska, and Krzysztof Ulbrich. 2024. "The Bleeding Must Be Stopped! Management in the Situation of Hemorrhages—A Prospective Randomized Controlled Prospective Simulation Study" Healthcare 12, no. 23: 2370. https://doi.org/10.3390/healthcare12232370
APA StyleStarosolski, M., Kalemba, A., Kaplan, C., Majewska, K., & Ulbrich, K. (2024). The Bleeding Must Be Stopped! Management in the Situation of Hemorrhages—A Prospective Randomized Controlled Prospective Simulation Study. Healthcare, 12(23), 2370. https://doi.org/10.3390/healthcare12232370







