Perceptions of Patient Safety Culture among Triage Nurses in the Emergency Department: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting and Sample
2.3. Study Tools/Instruments
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
4. Discussion
4.1. Implications for Nursing Practice
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wireklint, S.C.; Elmqvist, C.; Parenti, N.; Göransson, K.E. A descriptive study of registered nurses’ application of the triage scale RETTS©; a Swedish reliability study. Int. Emerg. Nurs. 2018, 38, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Alumran, A.; Alkhaldi, O.; Aldroorah, Z.; Alsayegh, Z.; Alsafwani, F.; Almaghraby, N. Utilization of an Electronic Triage System by Emergency Department Nurses. J. Multidiscip. Healthc. 2020, 13, 339–344. [Google Scholar] [CrossRef]
- Bijani, M.; Khaleghi, A.A. Challenges and Barriers Affecting the Quality of Triage in Emergency Departments: A Qualitative Study. Galen Med. J. 2019, 8, e1619. [Google Scholar] [CrossRef]
- Mélot, C. To score or not to score during triage in the emergency department? Intensive Care Med. 2015, 41, 1135–1137. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johnson, K.D.; Schumacher, D.; Lee, R.C. Identifying Strategies for the Management of Interruptions for Novice Triage Nurses Using an Online Modified Delphi Method. J. Nurs. Scholarsh. 2021, 53, 718–726. [Google Scholar] [CrossRef] [PubMed]
- Malmström, T.; Harjola, V.P.; Torkki, P.; Kumpulainen, S.; Malmström, R. Triage quality control is missing tools-a new observation technique for ED quality improvement. Int. J. Qual. Health Care 2017, 29, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Bijani, M.; Torabizadeh, C.; Rakhshan, M.; Fararouei, M. Professional capability in triage nurses in emergency department: A qualitative study. Rev. Latinoam. Hipertens. 2018, 13, 554–560. [Google Scholar]
- Farrohknia, N.; Castrén, M.; Ehrenberg, A.; Lind, L.; Oredsson, S.; Jonsson, H.; Asplund, K.; Göransson, K.E. Emergency department triage scales and their components: A systematic review of the scientific evidence. Scand. J. Trauma Resusc. Emerg. 2011, 19, 42. [Google Scholar] [CrossRef]
- Fekonja, Z.; Kmetec, S.; Fekonja, U.; Mlinar Reljić, N.; Pajnkihar, M.; Strnad, M. Factors contributing to patient safety during triage process in the emergency department: A systematic review. J. Clin. Nurs. 2023, 32, 5461–5477. [Google Scholar] [CrossRef] [PubMed]
- Alshyyab, M.A.; FitzGerald, G.; Dingle, K.; Ting, J.; Bowman, P.; Kinnear, F.B.; Borkoles, E. Developing a conceptual framework for patient safety culture in emergency department: A review of the literature. Int. J. Health Plan. Manag. 2019, 34, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.A.; Chalak, M.; Montazeralfaraj, R.; Dehghani Tafti, A. Iranian nurses’ perception of patient safety culture. Iran. Red. Crescent Med. J. 2014, 16, e11894. [Google Scholar] [CrossRef] [PubMed]
- Khamaiseh, A.; Al-Twalbeh, D.; Al-Ajlouni, K. Patient safety culture in Jordanian primary health-care centres as perceived by nurses: A cross-sectional study. EMJH 2020, 26, 1242–1250. [Google Scholar] [CrossRef] [PubMed]
- Im, D.; Aaronson, E. Best practices in patient safety and communication. Emerg. Med. Clin. N. Am. 2020, 38, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Kaczorowski, K.M.; Drayton, N.A.; Grimston, M.R. Gaining perspective into the term ‘safety culture’; how emergency nurses view its meaning in their everyday practice: A focus group study in an Australian setting. Australas. Emerg. Care 2020, 23, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Alshyyab, M.A.; Albsoul, R.; Fitzgerald, G. Factors influencing patient safety culture in operating room in a teaching hospital in Jordan: A qualitative descriptive study. TQM J. 2023, 35, 1722–1742. [Google Scholar] [CrossRef]
- Lee, Y.m.; Oh, H. The Influence of Patient Safety Culture and Patient Safety Error Experience on Safety Nursing Activities of Emergency Nurses in South Korea. J. Emerg. Nurs. 2020, 46, 838–847.e832. [Google Scholar] [CrossRef]
- Karaca, A.; Akin, S.; Harmanci Seren, A.K. The Relationship Between Perceived Quality of Care and the Patient Safety Culture of Turkish Nurses. J. Nurs. Res. 2022, 30, e223. [Google Scholar] [CrossRef]
- Khater, W.A.; Akhu-Zaheya, L.M.; AL-Mahasneh, S.I.; Khater, R. Nurses’ perceptions of patient safety culture in Jordanian hospitals. Int. Nurs. Rev. 2015, 62, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Alshyyab, M.A.; Albsoul, R.A.; Kinnear, F.B.; Saadeh, R.A.; Alkhaldi, S.M.; Borkoles, E.; Fitzgerald, G. Assessment of patient safety culture in two emergency departments in Australia: A cross sectional study. TQM J. 2022, 35, 540–553. [Google Scholar] [CrossRef]
- Kosydar-Bochenek, J.; Religa, D.; Knap, M.; Czop, M.; Knap, B.; Mędrzycka-Dąbrowska, W.; Krupa, S. Safety climate perceived by pre-hospital emergency care personnel—An international cross-sectional study. Front. Public. Health 2023, 11, 1192315. [Google Scholar] [CrossRef] [PubMed]
- Ministrstvo za zdravje. Pregled Stanja na Področju Zdravstva v Sloveniji—Januar 2023; Ministrstvo za Zdravje: Ljubljana, Slovenia, 2023.
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th, International ed.; Wolters Kluwer: Philadelphia, PA, USA, 2021; Volume 839, p. XVIII. [Google Scholar]
- Rajapakse, R. Triaža v urgentnih ambulantah. Zdrav. Vest. 2015, 84, 259–267. [Google Scholar] [CrossRef][Green Version]
- Cochran, W.G. Sampling Techniques, 3rd ed.; John Wiley & Sons: New York, NY, USA, 1977. [Google Scholar]
- Patterson, P.D.; Huang, D.T.; Fairbanks, R.J.; Wang, H.E. The emergency medical services safety attitudes questionnaire. Am. J. Med. Qual. 2010, 25, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef] [PubMed]
- Lambrou, P.; Papastavrou, E.; Merkouris, A.; Middleton, N. Professional environment and patient safety in emergency departments. Int. Emerg. Nurs. 2015, 23, 150–155. [Google Scholar] [CrossRef] [PubMed]
- AL-Mugheed, K.; Bayraktar, N.; Al-Bsheish, M.; AlSyouf, A.; Jarrar, M.T.; AlBaker, W.; Aldhmadi, B.K. Patient Safety Attitudes among Doctors and Nurses: Associations with Workload, Adverse Events, Experience. Healthcare 2022, 10, 631. [Google Scholar] [CrossRef]
- Nekoei-Moghadam, M.; Raadabadi, M.; Heidarijamebozorgi, M. Patient safety culture in university hospital’s emergency departments: A case study. Int. J. Health Plan. Manag. 2020, 35, 852–858. [Google Scholar] [CrossRef]
- Al-Nawafleh, A.H.; Abu-Helalah, M.A.; Hill, V.; Masoud, M.I.; Al-Mahasneh, H.A.; Salti, E.T.A. Patient Safety Culture in Jordanian Hospitals. Health Sci. J. 2016, 10, 5. [Google Scholar]
- El-Shabrawy, E.M.A.; Anwar, M.; Mostafa, Z.M. Assessment of Patient Safety Culture among Health Care Workers in Beni-Suef University Hospital, Egypt. Egypt. J. Community Med. 2017, 35, 11–19. [Google Scholar] [CrossRef]
- El-Sherbiny, N.A.; Ibrahim, E.H.; Abdel-Wahed, W.Y. Assessment of patient safety culture among paramedical personnel at general and district hospitals, Fayoum Governorate, Egypt. J. Egypt. Public Health Assoc. 2020, 95, 4. [Google Scholar] [CrossRef] [PubMed]
- Alsabri, M.; Mervat, A.; Farouk, A.-Q.; Asma, Z.; Adekemi, E.; Sayed, G.; Adel, H.; Mohammed, H.; Shahenaz, N.; Abdelouahab, B. Patient Safety Culture in Emergency Departments of Yemeni Public Hospitals: A Survey Study. Front. Emerg. Med. 2021, 5, e21. [Google Scholar] [CrossRef]
- Alquwez, N.; Cruz, J.P.; Almoghairi, A.M.; Al-Otaibi, R.S.; Almutairi, K.O.; Alicante, J.G.; Colet, P.C. Nurses’ Perceptions of Patient Safety Culture in Three Hospitals in Saudi Arabia. J. Nurs. Sch. 2018, 50, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Najafi Ghezeljeh, T.; Balouchi, M.; Haghani, S. Attitudes Towards Patient Safety in Pre-Hospital Emergency Medical Staff in Mashhad, Iran. Iran J. Nurs. Res. 2022, 35, 260–275. [Google Scholar] [CrossRef]
- Gozlu, K.; Kaya, S. Patient Safety Culture as Perceived by Nurses in a Joint Commission International Accredited Hospital in Turkey and its Comparison with Agency for Healthcare Research and Quality Data. J. Patient Saf. 2016, 4, 441–449. [Google Scholar] [CrossRef]
- Rigobello, M.C.G.; Carvalho, R.; Guerreiro, J.M.; Motta, A.P.G.; Atila, E.; Gimenes, F.R.E. The perception of the patient safety climate by professionals of the emergency department. Int. Emerg. Nurs. 2017, 33, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Weaver, M.D.; Wang, H.E.; Fairbanks, R.J.; Patterson, D. The association between EMS workplace safety culture and safety outcomes. Prehospital Emerg. Care 2012, 16, 43–52. [Google Scholar] [CrossRef]
- Venesoja, A.; Lindström, V.; Aronen, P.; Castrén, M.; Tella, S. Exploring safety culture in the Finnish ambulance service with Emergency Medical Services Safety Attitudes Questionnaire. Scand. J. Trauma Resusc. Emerg. 2021, 29, 148. [Google Scholar] [CrossRef] [PubMed]
- Chaulagain, N.; Khadka, D.K. Factors Influencing Job Satisfaction Among Healthcare Professionals At Tilganga Eye Centre, Kathmandu, Nepal. Int. J. Sci. Technol. Res. 2012, 1, 32–36. [Google Scholar]
- Sasso, L.; Bagnasco, A.; Catania, G.; Zanini, M.; Aleo, G.; Watson, R.; RN4CAST@ IT Working Group. Push and pull factors of nurses’ intention to leave. J. Nurs. Manag. 2019, 27, 946–954. [Google Scholar] [CrossRef]
- Penconek, T.; Tate, K.; Bernardes, A.; Lee, S.; Micaroni, S.P.M.; Balsanelli, A.P.; de Moura, A.A.; Cummings, G.G. Determinants of nurse manager job satisfaction: A systematic review. Int. J. Nurs. Stud. 2021, 118, 103906. [Google Scholar] [CrossRef]
- Boamah, S.A.; Spence Laschinger, H.K.; Wong, C.; Clarke, S. Effect of transformational leadership on job satisfaction and patient safety outcomes. Nurs. Outlook 2018, 66, 180–189. [Google Scholar] [CrossRef]
- Güneş, Ü.Y.; Gürlek, Ö.; Sönmez, M. A survey of the patient safety culture of hospital nurses in Turkey. Collegian 2016, 23, 225–232. [Google Scholar] [CrossRef]
- Wang, X.; Liu, K.; You, L.M.; Xiang, J.G.; Hu, H.G.; Zhang, L.F.; Zheng, J.; Zhu, X.W. The relationship between patient safety culture and adverse events: A questionnaire survey. Int. J. Nurs. Stud. 2014, 51, 1114–1122. [Google Scholar] [CrossRef]
- Wang, Y.; Wan, Q.; Guo, J.; Jin, X.; Zhou, W.; Feng, X.; Shang, S. The influence of effective communication, perceived respect and willingness to collaborate on nurses’ perceptions of nurse-physician collaboration in China. Appl. Nurs. Res. 2018, 41, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Yurdanur Ege, R. Patient safety culture: Evaluating Turkish nurses’ attitudes and knowledge. Int. J. Caring Sci. 2019, 12, 430–441. [Google Scholar]
- Farokhzadian, J.; Dehghan Nayeri, N.; Borhani, F. The long way ahead to achieve an effective patient safety culture: Challenges perceived by nurses. BMC Health Serv. Res. 2018, 18, 654. [Google Scholar] [CrossRef]
- Samsuri, S.E.; Lin, L.P.; Fahrni, M.L. Safety culture perceptions of pharmacists in Malaysian hospitals and health clinics: A multicentre assessment using the Safety Attitudes Questionnaire. BMJ Open 2015, 5, e008889. [Google Scholar] [CrossRef] [PubMed]
- Bottcher, B.; Abu-El-Noor, N.; Abuowda, Y.; Alfaqawi, M.; Alaloul, E.; El-Hout, S.; Al-Najjar, I.; Abu-El-Noor, M. Attitudes of doctors and nurses to patient safety and errors in medical practice in the Gaza-Strip: A cross-sectional study. BMJ Open 2019, 9, e026788. [Google Scholar] [CrossRef]
- Magalhães, A.M.M.; Costa, D.G.D.; Riboldi, C.O.; Mergen, T.; Barbosa, A.D.S.; Moura, G. Association between workload of the nursing staff and patient safety outcomes. Rev. Esc. Enferm. USP 2017, 51, e03255. [Google Scholar] [CrossRef]
- Huang, D.T.; Clermont, G.; Sexton, J.B.; Karlo, C.A.; Miller, R.G.; Weissfeld, L.A.; Rowan, K.M.; Angus, D.C. Perceptions of safety culture vary across the intensive care units of a single institution. Crit. Care Med. 2007, 35, 165–176. [Google Scholar] [CrossRef]
- Lee, W.C.; Wung, H.Y.; Liao, H.H.; Lo, C.M.; Chang, F.L.; Wang, P.C.; Fan, A.; Chen, H.H.; Yang, H.C.; Hou, S.M. Hospital safety culture in Taiwan: A nationwide survey using Chinese version Safety Attitude Questionnaire. BMC Health Serv. Res. 2010, 10, 234. [Google Scholar] [CrossRef]
- Burström, L.; Letterstål, A.; Engström, M.-L.; Berglund, A.; Enlund, M. The patient safety culture as perceived by staff at two different emergency departments before and after introducing a flow-oriented working model with team triage and lean principles: A repeated cross-sectional study. BMC Health Serv. Res. 2014, 14, 296. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Egea, F.; Tomas, S.; Chanovas-Borràs, M. Patient safety culture in 30 Spanish hospital emergency departments: Results of the Agency for Healthcare Research and Quality’s Hospital Survey on Patient Safety Culture. Emergencias 2011, 23, 356–364. [Google Scholar]
- Tourani, S.; Hassani, M.; Ayoubian, A.; Habibi, M.; Zaboli, R. Analyzing and Prioritizing the Dimensions of Patient Safety Culture in Emergency Wards Using the TOPSIS Technique. Glob. J. Health Sci. 2015, 7, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Verbeek-Van Noord, I.; Wagner, C.; Van Dyck, C.; Twisk, J.W.; De Bruijne, M.C. Is culture associated with patient safety in the emergency department? A study of staff perspectives. Int. J. Qual. Health Care 2014, 26, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Tear, M.; Reader, T.; Shorrock, S.; Kirwan, B. Safety culture and power: Interactions between perceptions of safety culture, organisational hierarchy, and national culture. Saf. Sci. 2018, 121, 550–561. [Google Scholar] [CrossRef]
- Azyabi, A.; Karwowski, W.; Davahli, M.R. Assessing Patient Safety Culture in Hospital Settings. Int. J. Environ. Res. Public Health 2021, 18, 2466. [Google Scholar] [CrossRef]
- Hu, S.H.; Wang, T.; Ramalho, N.C.; Zhou, D.; Hu, X.; Zhao, H. Relationship between patient safety culture and safety performance in nursing: The role of safety behaviour. Int. J. Nurs. Pract. 2021, 27, e12937. [Google Scholar] [CrossRef] [PubMed]
- Isa, A.A.M.; Wahab, W.A.; Omar, R.C.; Nordin, M.Z.M.; Taha, H.; Roslan, R. Impact of employee age and work experience on safety culture at workplace. In Proceedings of the E3S Web of Conferences, St. Petersburg, Russia, 24–26 September 2021; p. 06007. [Google Scholar]
- Bondevik, G.T.; Hofoss, D.; Husebø, B.S.; Deilkås, E.C.T. Patient safety culture in Norwegian nursing homes. BMC Health Serv. Res. 2017, 17, 424. [Google Scholar] [CrossRef]
- Patterson, P.D.; Huang, D.T.; Fairbanks, R.J.; Simeone, S.; Weaver, M.; Wang, H.E. Variation in emergency medical services workplace safety culture. Prehospital Emerg. Care 2010, 14, 448–460. [Google Scholar] [CrossRef]
- Malak, M.Z.; Salouk, J.; Al-Shawawreh, R.; Al-Kamiseh, H.; Ayed, A. Perceptions of patient safety culture among emergency room nurses in Jordanian accredited hospitals. J. Nurs. Manag. 2022, 30, 3131–3138. [Google Scholar] [CrossRef]
- Wu, A.W.; Busch, I.M. Patient safety: A new basic science for professional education. GMS J. Med. Educ. 2019, 36, Doc21. [Google Scholar] [CrossRef]
- Elsous, A.; Akbari Sari, A.; AlJeesh, Y.; Radwan, M. Nursing perceptions of patient safety climate in the Gaza Strip, Palestine. Int. Nurs. Rev. 2017, 64, 446–454. [Google Scholar] [CrossRef]
- Tunçer Ünver, G.; Harmanci Seren, A.K. Defining the patient safety attitudes and influencing factors of health professionals working at maternity hospitals. J. Nurs. Manag. 2018, 26, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Abdul Rahman, H.; Jarrar, M.t.; Omira, O.D. Leadership Styles and Performance of Public Sector Organizations: The Case of Saudi Arabia. J. Bus. Financ. Account. 2020, 4, 55–62. [Google Scholar] [CrossRef]
- Rahman, H.A.; Jarrar, M.; Don, M.S. Nurse Level of Education, Quality of Care and Patient Safety in the Medical and Surgical Wards in Malaysian Private Hospitals: A Cross-sectional Study. Glob. J. Health Sci. 2015, 7, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Li, Y.; Ning, J.; Hou, Y.; Huang, Y.; Zhang, M. Patient safety research in China: A literature review. J. Evid. Based Med. 2011, 4, 66–72. [Google Scholar] [CrossRef]
- Wagner, C.; Kristensen, S.; Sousa, P.; Panteli, D. Patient safety culture as a quality strategy. In Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies; Busse, R., Klazinga, N., Panteli, D., Quentin, W., Eds.; WHO: Copenhagen, Denmark, 2019; pp. 287–306. [Google Scholar]
| Variables | n | % | M (SD) |
|---|---|---|---|
| Gender (n = 201) | - | ||
| Male | 42 | 21 | - |
| Female | 159 | 79 | - |
| Education (n = 201) | |||
| Vocational nursing education | 42 | 21 | - |
| Bachelor’s degree in nursing | 139 | 69 | - |
| Master’s degree in nursing | 20 | 10 | - |
| Age (n = 201) | 37 (9.89) | ||
| ≤30 | 57 | 28 | - |
| 31–40 | 87 | 43 | - |
| 41–50 | 37 | 18 | - |
| ≥51 | 20 | 10 | - |
| Working experience (n = 201) | 14 (10.34) | ||
| ≤5 years | 53 | 26 | - |
| 6–10 years | 38 | 19 | - |
| 11–15 years | 45 | 22 | - |
| ≥16 years | 65 | 32 | - |
| Working experience in ED (n = 201) | 9 (8.40) | ||
| ≤5 years | 99 | 49 | - |
| 6–10 years | 46 | 23 | - |
| 11–15 years | 24 | 12 | - |
| ≥16 years | 32 | 16 | - |
| MTS triage performance in years | 201 | 100 | 5 (3.45) |
| Daily contact with patients | 201 | 100 | 63 (40.81) |
| Duration of triage working day (n = 201) | - | ||
| 4 h | 2 | 1 | - |
| 8 h | 104 | 52 | - |
| 12 h | 95 | 47 | - |
| No. of consecutive days in triage (n = 201) | - | ||
| One day | 18 | 9 | - |
| Two days | 25 | 12 | - |
| Three days | 29 | 14 | - |
| Four days | 29 | 14 | - |
| More than four days | 100 | 50 | - |
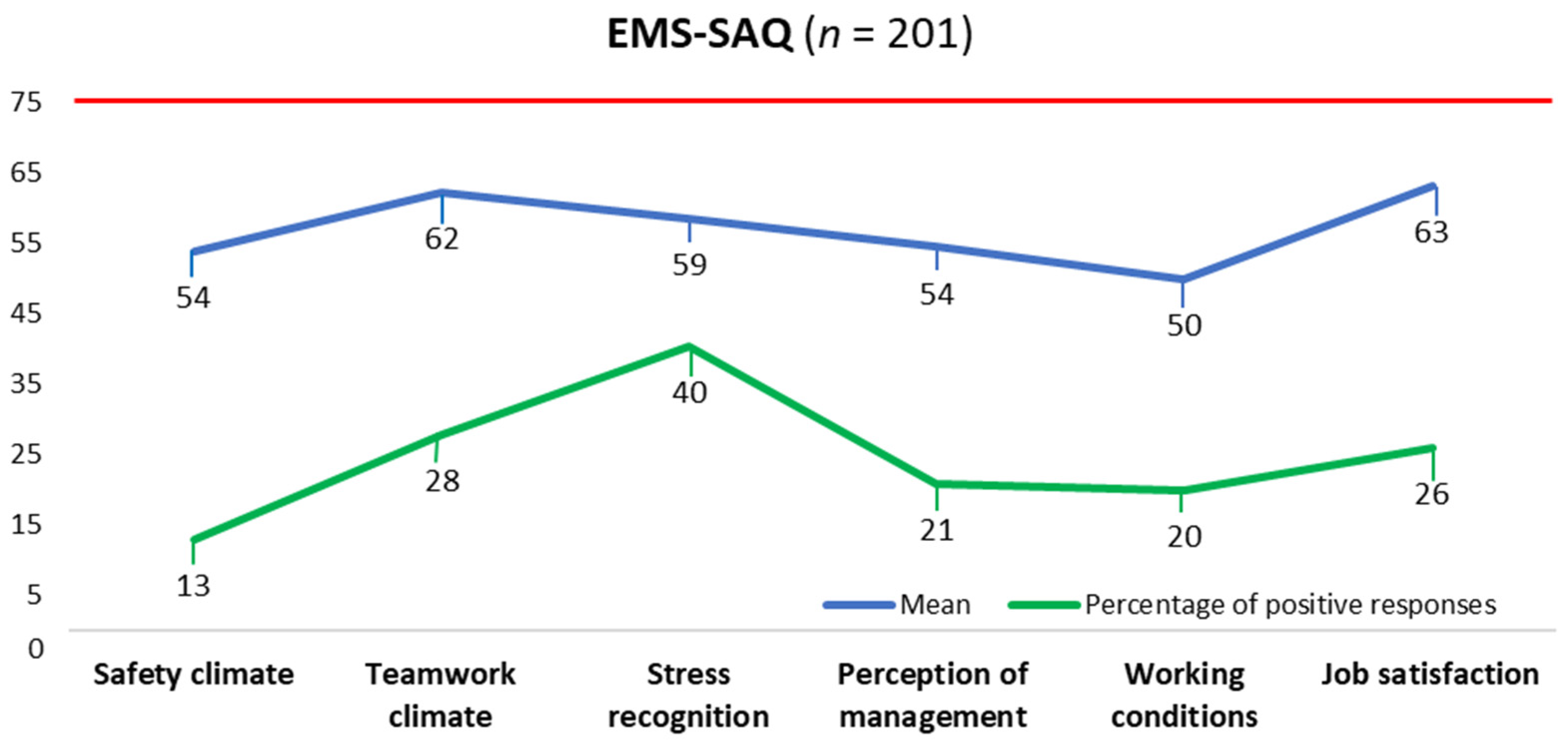
| Domain | No. of Items | Min–Max | M (SD) | Mdn (IQR) |
|---|---|---|---|---|
| Total EMS-SAQ | 30 | 14–85 | 57.27 (13.81) | 56.67 (47.50–67.92) |
| Safety climate | 7 | 11–96 | 53.82 (18.50) | 53.57 (42.86–64.29) |
| Teamwork climate | 6 | 13–100 | 62.31 (16.32) | 62.50 (50–75) |
| Stress recognition | 4 | 0–100 | 58.55 (24.20) | 62.50 (37.50–75) |
| Perception of management | 4 | 6–94 | 54.45 (21.02) | 56.25 (37.50–68.75) |
| Working conditions | 4 | 13–94 | 49.91 (17.37) | 43.75 (37.50–62.50) |
| Job satisfaction | 5 | 10–100 | 63.18 (17.19) | 60 (50–75) |
| Variables | <75 n (%) | >75 n (%) | U or χ2 | df | p * |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 136 (86) | 20 (17) | 3316.50 | 1 | 0.907 |
| Male | 37 (88) | 5 (12) | |||
| Age | |||||
| ≤30 | 49 (28) | 8 (32) | 17.750 | 3 | <0.001 * |
| 31–40 | 82 (47) | 5 (20) | |||
| 41–50 | 33 (19) | 4 (16) | |||
| ≥51 | 12 (7) | 8 (32) | |||
| Education | |||||
| Vocational NE | 41 (98) | 1 (2) | 6.957 | 2 | 0.031 * |
| BSN | 120 (86) | 19 (14) | |||
| MSN/MN | 15 (75) | 5 (25) | |||
| Working experience | |||||
| ≤5 years | 45 (85) | 8 (15) | 8.875 | 3 | 0.031 * |
| 6–10 years | 33 (87) | 5 (13) | |||
| 11–15 years | 45 (100) | 0 (0) | |||
| ≥16 years | 53 (82) | 12 (19) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fekonja, Z.; Kmetec, S.; Mlinar Reljić, N.; Černe Kolarič, J.; Pajnkihar, M.; Strnad, M. Perceptions of Patient Safety Culture among Triage Nurses in the Emergency Department: A Cross-Sectional Study. Healthcare 2023, 11, 3155. https://doi.org/10.3390/healthcare11243155
Fekonja Z, Kmetec S, Mlinar Reljić N, Černe Kolarič J, Pajnkihar M, Strnad M. Perceptions of Patient Safety Culture among Triage Nurses in the Emergency Department: A Cross-Sectional Study. Healthcare. 2023; 11(24):3155. https://doi.org/10.3390/healthcare11243155
Chicago/Turabian StyleFekonja, Zvonka, Sergej Kmetec, Nataša Mlinar Reljić, Jožica Černe Kolarič, Majda Pajnkihar, and Matej Strnad. 2023. "Perceptions of Patient Safety Culture among Triage Nurses in the Emergency Department: A Cross-Sectional Study" Healthcare 11, no. 24: 3155. https://doi.org/10.3390/healthcare11243155
APA StyleFekonja, Z., Kmetec, S., Mlinar Reljić, N., Černe Kolarič, J., Pajnkihar, M., & Strnad, M. (2023). Perceptions of Patient Safety Culture among Triage Nurses in the Emergency Department: A Cross-Sectional Study. Healthcare, 11(24), 3155. https://doi.org/10.3390/healthcare11243155





