Dermatology-Related Emergency Department Visits in Tertiary Care Center in Riyadh, Saudi Arabia: A Descriptive Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Study Population
2.4. Data Collection and Management
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kilic, D.; Yigit, O.; Kilic, T.; Buyurgan, C.S.; Dicle, O. Epidemiologic Characteristics of Patients Admitted to Emergency Department with Dermatological Complaints; a Retrospective Cross sectional Study. Arch. Acad. Emerg. Med. 2019, 7, e47. [Google Scholar] [PubMed]
- Arabi, Y.E.; Hali, F.; Skali, H.D.; Chiheb, S. Dermatological emergencies: A Moroccan retrospective case series over a period of two years. Pan Afr. Med. J. 2022, 41, 348. [Google Scholar] [CrossRef] [PubMed]
- Ozkur, E.; Altunay, I.; Sekerlisoy, G.; Erdem, Y. Evaluation of Dermatology Consultations in a Tertiary Care Centre Emergency Service. Sisli Etfal Hastan. Tip Bul. 2020, 54, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Abedini, R.; Matinfar, A.; Sasani, P.; Salehi, A.; Daneshpazhooh, M. Evaluation of Patients Visiting the Dermatology Emergency Unit of a University Dermatology Hospital in Tehran, Iran. Acta Med. Iran. 2017, 55, 705–711. [Google Scholar] [PubMed]
- Francés Rodríguez, L.; Leiva-Salinas, M. FR-Las urgencias en dermatología [Dermatologic emergencies]. Actas Dermo-Sifiliogr. 2015, 106, 322–323. [Google Scholar] [CrossRef] [PubMed]
- Kody, S.; Cline, A.; Pereira, F.A. Dermatological trends in emergency medicine. J. Dermatol. Treat. 2022, 33, 1746–1748. [Google Scholar] [CrossRef] [PubMed]
- Jack, A.R.; Spence, A.A.; Nichols, B.J.; Chong, S.; Williams, D.T.; Swadron, S.P.; Peng, D.H. Cutaneous conditions leading to dermatology consultations in the emergency department. West. J. Emerg. Med. 2011, 12, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Bancalari-Díaz, D.; Gimeno-Mateos, L.I.; Cañueto, J.; Andrés-Ramos, I.; Fernández-López, E.; Román-Curto, C. Dermatologic emergencies in a tertiary hospital: A descriptive study. Estudio descriptivo de urgencias dermatológicas en un hospital terciario. Actas Dermo-Sifiliogr. 2016, 107, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Mitra, D.; Chopra, A.; Saraswat, N.; Agarwal, R.; Kumar, S. An Observational Study to Describe the Clinical Pattern of Dermatological Emergencies from Emergency Department and Intensive Care Unit: Our Experience from a Tertiary Care Hospital in Northern India. Indian Dermatol. Online J. 2019, 10, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Shahzad, M.; Alzolibani, A.A.; Al Robaee, A.A.; Al Shobaili, H.A.; Alsharkasy, M.H.; Al Marshood, A.A.; Al Mutiari, A.; Aldukhayel, A. Patients seen at the Dermatology ambulatory office in a tertiary care center in Qassim region, Saudi Arabia. Int. J. Health Sci. 2013, 7, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martínez, M.L.; Escario-Travesedo, E.; Rodríguez-Vázquez, M.; Azaña-Defez, J.M.; de Hijas-Santos, M.M.; Juan-Pérez-García, L. Dermatology consultations in an emergency department prior to establishment of emergency dermatology cover. Actas Dermo-Sifiliogr. Engl. Ed. 2011, 102, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Nadkarni, A.; Domeisen, N.; Hill, D.; Feldman, S.R. The most common dermatology diagnoses in the emergency department. J. Am. Acad. Dermatol. 2016, 75, 1261–1262. [Google Scholar] [CrossRef] [PubMed]
- Usatine, R.P.; Sandy, N. Dermatologic emergencies. Am. Fam. Physician 2010, 82, 773–780. [Google Scholar] [PubMed]
- Bahamdan, K.A.; Egere, J.U.; Khare, A.K.; Tallab, T.; Ibrahim, K.; Mourad, M. The pattern of skin diseases in Asir region, Saudi Arabia: A 12-month prospective study in a referral hospital. Ann. Saudi Med. 1995, 15, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Mempel, M.; Traidl-Hofmann, C.; Al Khusaei, S.; Ring, J. Gender aspects in skin diseases. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Sandhu, K.; Kumar, B. Evaluation of emergency dermatological consultations in a tertiary care centre in North India. J. Eur. Acad. Dermatol. Venereol. 2003, 17, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Moon, A.T.; Castelo-Soccio, L.; Yan, A.C. Emergency department utilization of pediatric dermatology (PD) consultations. J. Am. Acad. Dermatol. 2016, 74, 1173–1177. [Google Scholar] [CrossRef] [PubMed]
- Aljohani, A.G.; Abduljabbar, M.H.; Hariri, J.; Zimmo, B.S.; Magboul, M.A.; Aleissa, S.M.; Baabdullah, A.; Alqutub, A.; Alafif, K.; Faidah, H. Assessing the Ability of Non-dermatology Physicians to Recognize Urgent Skin Diseases. Cureus 2023, 15, e37823. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- AlJasser, M.I. Severe Cutaneous Adverse Drug Reactions at a Tertiary Care Center in Saudi Arabia. Dermatol. Res. Pract. 2023, 2023, 8928198. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Characteristic | Description |
|---|---|
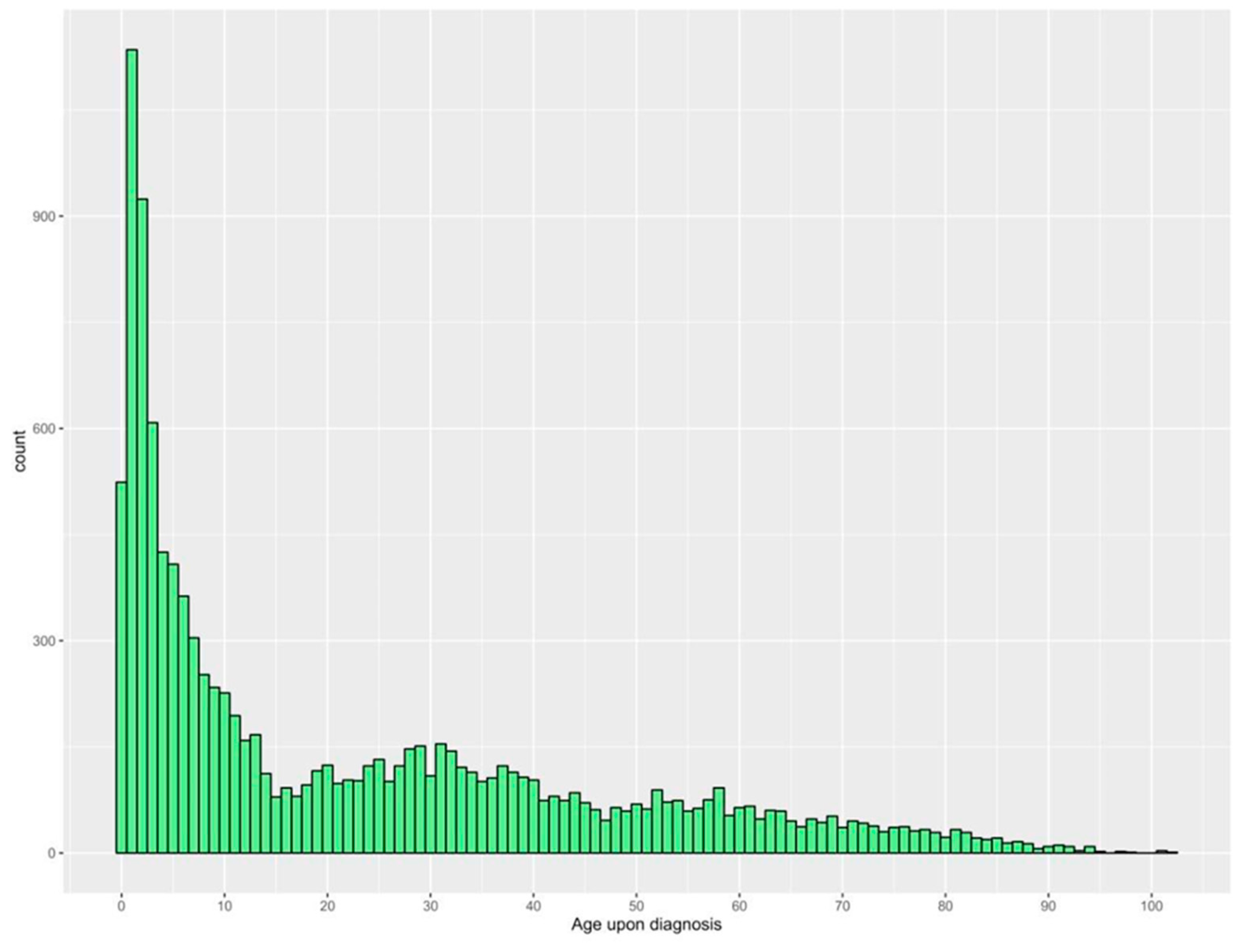
| Age at diagnosis (years) | 22.4 ± 23.2 |
| Gender | |
| Male | 6285 (54.9%) |
| Female | 5158 (45.1%) |
| Comorbidities | |
| Diabetes | 1077 (9.4%) |
| Dyslipidemia | 736 (6.4%) |
| Hypertension | 576 (5.0%) |
| Stroke | 122 (1.1%) |
| Heart failure | 48 (0.4%) |
| Nationality | |
| Saudi | 11,031 (96.4%) |
| Non-Saudi | 412 (3.6%) |
| Non-Saudi nationalities | |
| Filipino | 124 (30.1%) |
| Syrian | 106 (25.7%) |
| Malaysian | 36 (8.7%) |
| Other Asian nationalities countries | 74 (18.0%) |
| Other African nationalities | 48 (11.7%) |
| Other European nationalities | 11 (2.7%) |
| USA | 10 (2.4%) |
| Canada | 2 (0.5%) |
| Australia | 1 (0.2%) |
| Characteristic | Description n (%) |
|---|---|
| Infections of the skin and subcutaneous tissue | 3529 (30.8%) |
| Cellulitis | 1558 (13.6%) |
| Cutaneous abscess, furuncle, and carbuncle | 1001 (8.7%) |
| Acute lymphadenitis | 294 (2.6%) |
| Pilonidal cyst | 258 (2.3%) |
| Other local infections of skin and subcutaneous tissue | 241 (2.1%) |
| Impetigo | 176 (1.5%) |
| Staphylococcal scalded skin syndrome | 1 (0.0%) |
| Symptoms and signs involving the skin and subcutaneous tissue | 1850 (16.2%) |
| Rash and other non-specific skin eruption | 1828 (16.0%) |
| Other skin changes | 22 (0.2%) |
| Urticaria and erythema | 1430 (12.5%) |
| Urticaria | 1400 (12.2%) |
| Other erythematous conditions | 16 (0.1%) |
| Erythema multiforme | 12 (0.1%) |
| Erythema nodosum | 1 (0.0%) |
| Erythema in diseases classified elsewhere | 1 (0.0%) |
| Burns and corrosions | 1353 (11.8%) |
| Burn and corrosion, body region unspecified | 735 (6.4%) |
| Burn and corrosion of ankle and foot | 137 (1.2%) |
| Burn and corrosion of wrist and hand | 132 (1.2%) |
| Burn and corrosion of trunk | 122 (1.1%) |
| Burns and corrosions of multiple body regions | 69 (0.6%) |
| Burn and corrosion of hip and lower limb, except ankle and foot | 52 (0.5%) |
| Burn and corrosion of head and neck | 47 (0.4%) |
| Burn and corrosion of shoulder and upper limb, except wrist and hand | 45 (0.4%) |
| Burns classified according to extent of body surface involved | 14 (0.1%) |
| Viral infections characterized by skin and mucous membrane lesions | 1322 (11.6%) |
| Other viral infections characterized by skin and mucous membrane lesions, not classified elsewhere | 459 (4.0%) |
| Herpesviral [herpes simplex] infections | 397 (3.5%) |
| Unspecified viral infection characterized by skin and mucous membrane lesions | 140 (1.2%) |
| Zoster [herpes zoster] | 112 (1.0%) |
| Varicella [chickenpox] | 84 (0.7%) |
| Measles | 74 (0.6%) |
| Viral warts | 48 (0.4%) |
| Monkeypox | 8 (0.1%) |
| Other disorders of the skin and subcutaneous tissue | 780 (6.8%) |
| Ulcer of lower limb, not classified elsewhere | 179 (1.6%) |
| Granulomatous disorders of skin and subcutaneous tissue | 156 (1.4%) |
| Decubitus ulcer and pressure area | 148 (1.3%) |
| Other disorders of skin and subcutaneous tissue, not classified elsewhere | 137 (1.2%) |
| Atrophic disorders of skin | 81 (0.7%) |
| Vasculitis limited to skin, not classified elsewhere | 25 (0.2%) |
| Other disorders of pigmentation | 10 (0.1%) |
| Hypertrophic disorders of skin | 10 (0.1%) |
| Corns and callosities | 9 (0.1%) |
| Lupus erythematosus | 6 (0.1%) |
| Pyoderma gangrenosum | 4 (0.0%) |
| Other epidermal thickening | 3 (0.0%) |
| Other localized connective tissue disorders | 3 (0.0%) |
| Seborrhoeic keratosis | 3 (0.0%) |
| Other disorders of skin and subcutaneous tissue in diseases classified elsewhere | 3 (0.0%) |
| Vitiligo | 2 (0.0%) |
| Acanthosis nigricans | 1 (0.0%) |
| Dermatitis and eczema | 680 (5.9%) |
| Atopic dermatitis | 504 (4.4%) |
| Other dermatitis | 176 (1.5%) |
| Disorders of skin appendages | 318 (2.8%) |
| Nail disorders | 140 (1.2%) |
| Follicular cysts of skin and subcutaneous tissue | 82 (0.7%) |
| Other follicular disorders | 50 (0.4%) |
| Acne | 22 (0.2%) |
| Nail disorders in diseases classified elsewhere | 10 (0.1%) |
| Alopecia areata | 4 (0.0%) |
| Other non-scarring hair loss | 4 (0.0%) |
| Eccrine sweat disorders | 3 (0.0%) |
| Hair colour and hair shaft abnormalities | 1 (0.0%) |
| Cicatricial alopecia [scarring hair loss] | 1 (0.0%) |
| Rosacea | 1 (0.0%) |
| Neoplasms | 94 (0.8%) |
| Benign lipomatous neoplasm | 65 (0.6%) |
| Other malignant neoplasms of skin | 14 (0.1%) |
| Malignant melanoma of skin | 8 (0.1%) |
| Melanoma in situ | 4 (0.0%) |
| Melanocytic naevi | 2 (0.0%) |
| Other benign neoplasms of skin | 1 (0.0%) |
| Papulosquamous disorders | 53 (0.5%) |
| Psoriasis | 24 (0.2%) |
| Pityriasis rosea | 19 (0.2%) |
| Other papulosquamous disorders | 7 (0.1%) |
| Lichen planus | 2 (0.0%) |
| Parapsoriasis | 1 (0.0%) |
| Other congenital malformations | 19 (0.2%) |
| Epidermolysis bullosa | 9 (0.1%) |
| Other congenital malformations of skin | 7 (0.1%) |
| Congenital ichthyosis | 3 (0.0%) |
| Frostbite | 8 (0.1%) |
| Superficial frostbite | 6 (0.1%) |
| Frostbite involving multiple body regions and unspecified frostbite | 2 (0.0%) |
| Radiation-related disorders of the skin and subcutaneous tissue | 3 (0.0%) |
| Sunburn | 3 (0.0%) |
| Bullous disorders | 2 (0.0%) |
| Other bullous disorders | 1 (0.0%) |
| Bullous disorders in diseases classified elsewhere | 1 (0.0%) |
| Mycoses | 2 (0.0%) |
| Chromomycosis and phaeomycotic abscess | 2 (0.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshibani, A.; Alagha, S.O.; Alshammari, A.J.; Alshammari, K.J.; Alghamdi, A.S.; Nagshabandi, K.N. Dermatology-Related Emergency Department Visits in Tertiary Care Center in Riyadh, Saudi Arabia: A Descriptive Study. Healthcare 2024, 12, 2332. https://doi.org/10.3390/healthcare12232332
Alshibani A, Alagha SO, Alshammari AJ, Alshammari KJ, Alghamdi AS, Nagshabandi KN. Dermatology-Related Emergency Department Visits in Tertiary Care Center in Riyadh, Saudi Arabia: A Descriptive Study. Healthcare. 2024; 12(23):2332. https://doi.org/10.3390/healthcare12232332
Chicago/Turabian StyleAlshibani, Abdullah, Saif Osama Alagha, Abdulmohsen Jameel Alshammari, Khaled Jameel Alshammari, Abdulelah Saeed Alghamdi, and Khalid Nabil Nagshabandi. 2024. "Dermatology-Related Emergency Department Visits in Tertiary Care Center in Riyadh, Saudi Arabia: A Descriptive Study" Healthcare 12, no. 23: 2332. https://doi.org/10.3390/healthcare12232332
APA StyleAlshibani, A., Alagha, S. O., Alshammari, A. J., Alshammari, K. J., Alghamdi, A. S., & Nagshabandi, K. N. (2024). Dermatology-Related Emergency Department Visits in Tertiary Care Center in Riyadh, Saudi Arabia: A Descriptive Study. Healthcare, 12(23), 2332. https://doi.org/10.3390/healthcare12232332






