How Does Trauma Make You Sick? The Role of Attachment in Explaining Somatic Symptoms of Survivors of Childhood Trauma
Abstract
1. Introduction
2. Methods
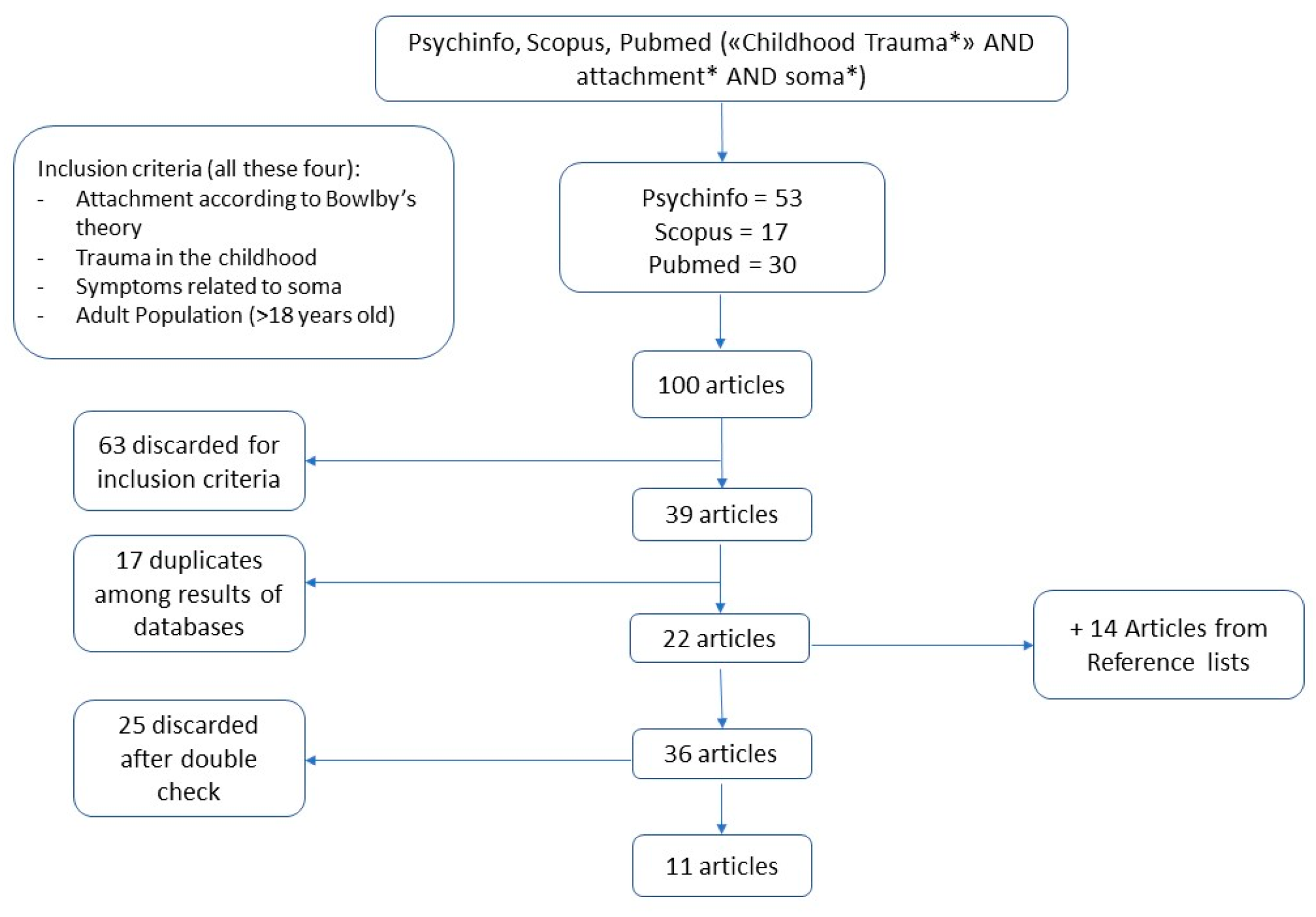
2.1. Search Strategy and Selection Criteria
2.2. The Search
3. Results
3.1. DNA Damage
3.2. Metabolic Syndrome and Obesity
3.3. Physical Pain
3.4. Functional Neurological Disorder
3.5. Motor FND
3.6. PNES (NEAD)
3.7. Somatization
| Author and Year | Title | Scale * | Participants’ Information | Results |
|---|---|---|---|---|
| DNA Damage | ||||
| Bergholz et al., 2017 [26] | DNA damage in lymphocytes of patients suffering from complex traumatization | CTQ, AAP, LEAS | Clinical group n = 40 (25 F; 15 M; mean age = 41.8; sd = 12.5) Control group n = 20 (14 F; 6 M; mean age = 44; sd = 13.1) | Patients with severe early trauma showed greater damage to DNA than did patients with mild early trauma and healthy controls. Patients with avoidant attachment showed greater DNA damage than did patients with secure or anxious attachment. |
| Metabolic Syndrome and Obesity | ||||
| Davis et al., 2014 [29] | Adult attachment interview discourse patterns predict metabolic syndrome in midlife | ELS, AAI, SCID-I, SAS, BDI, FFQ | n = 215 (112 F; 103 M; mean age = 45.9; sd = 3.3) | Less consistency, unresolved attachment, and idealization correlated with more MetS components; indirect paths led from childhood adversity to MetS. |
| D’Argenio et al., 2009 [28] | Early trauma and adult obesity: Is psychological dysfunction the mediating mechanism? | ETLE, RQ, SCID | Obese group n = 65 (23 F; 42 M; mean age = 40.4; sd = 12) Obese + Psychiatric group n = 85 (22 F; 64 M; mean age = 39.1; sd = 11.5) Control group n = 50 (426 F; 124 M; mean age = 32.6; sd = 11.2) | Not only sexual and physical abuse, but also minor traumas in childhood were associated with obesity in adulthood; strong association between anxious attachment and obesity, but childhood trauma predicted obesity independently from attachment. |
| Physical Pain | ||||
| Nacak et al., 2017 [31] | Insecure attachment style and cumulative traumatic life events in patients with somatoform pain disorder: A cross-sectional study | CTQ, ETI, RSQ, PHQ-9, PHQ-15, SCID-I | Clinical group n = 65 (45 F; 20 M; mean age 47.5; sd = 10.6) Control group n = 65 (49 F; 16 M; mean age = 43.9, sd = 11.8) | Patients with SPD report greater insecure attachment than healthy controls; patients with SPD report increased frequency of traumatic events compared to healthy controls. |
| Nacak et al., 2021 [30] | High rejection sensitivity in patients wit hsomatoform pain disorder | CTQ, ETI, RS, PHQ-9, PHQ-15, SCID, Rejection Sensitivity Questionnaire | Clinical group n = 65 (45 F; 20 M; mean age = 47.5 sd = 10.6) Control group n = 65 (49 F; 16 M; mean age = 43.9 sd = 11.8) | Insecure attachment and related childhood adversities predicted higher levels of RS, regardless of the presence of SPD. |
| Functional Neurological Disorder | ||||
| Williams et al., 2019 [35] | Fearful attachment linked to childhood abuse, alexithymia, and depression in motor functional neurological disorders | CTQ, LEC-5, RSQ, SF-36, PHQ-15, PTSD-CL5, SOMS:CD, DES, TAS, BIS, SDQ, CD-RISC, STAI-T, NEO, BDI | n = 56 (41 F; 15 M; mean age = 40.2; sd = 13) | In patients with motor FND, fearful attachment correlated with adverse events and greater severity of symptoms. |
| Gerhardt et al., 2021 [40] | Insecure and unresolved/disorganized attachment in patients with psychogenic nonepileptic seizures | CTQ, AAP, PHQ-9, SDQ, SCID-II-WHY | Clinical group n = 44 (34 F; 10 M; mean age = 37.3; sd = 12) Control group n = 44 (34 F; 10 M; mean age = 37.3; sd = 12.3) | Patients with PNES reported more insecure attachment and unresolved resolved attachment than did healthy controls; in the patients with PNES, unresolved attachment was associated with childhood emotional abuse. |
| Holman et al., 2008 [36] | Adult attachment style and childhood interpersonal trauma in non-epileptic attack disorder | FBQ, RSQ, BDI, BAI, MCMI-III | NEAD group n = 17 (14 F; 3 M; mean age = 36.2; sd not available) Epilepsy group n = 26 (20 F; 6 M; mean age = 38.4; sd not available) | Patients with NEAD reported more insecure attachment and fearful attachment than did patients with epilepsy; patients with NEAD reported more traumatic experiences than did patients with epilepsy. |
| Somatization | ||||
| Waldinger et al., 2006 [50] | Mapping the road from childhood trauma to adult somatization: the role of attachment | CTQ, RSQ, SSI, BDI, CTS | n = 101 couples (101 F; 101 M; women mean age = 31.6; sd = 8.6; men mean age = 33.2; sd = 8.8) | In women, insecure attachment mediated the relationship between childhood trauma and somatization. In men, insecure attachment and childhood trauma predicted somatization independently. |
| Brianda et al., 2017 [48] | Emotional abuse and somatic symptoms in young adulthood. The mediating role of the romantic attachment style in a population female | CTQ-SF, ECR-R, SCL-90-R | n = 346 F (mean age = 23.2; sd not available) | Childhood emotional abuse correlated with somatic symptoms. Childhood emotional maltreatment correlated with avoidant attachment. Dysfunctional attachment strengthened the relationship between childhood maltreatment and somatic symptoms. |
| Caplan et al., 2014 [49] | Attachment, childhood abuse, and IBD-related quality of life and disease activity outcomes | CMH, ECR-R, HBI, IBDQ, MSS, UCLA | n = 193 (88 F; 105 M; mean age = 46.3; sd = 14.2) | Avoidant attachment moderated the relationship between childhood abuse and QOL in IBD patients, and between childhood abuse and disease activity in UC patients. |
4. Discussion
5. Clinical Implications and Conclusions
6. Limitations and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The Effect of Multiple Adverse Childhood Experiences on Health: A Systematic Review and Meta-Analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef] [PubMed]
- Giano, Z.; Wheeler, D.L.; Hubach, R.D. The Frequencies and Disparities of Adverse Childhood Experiences in the U.S. BMC Public Health 2020, 20, 1327. [Google Scholar] [CrossRef] [PubMed]
- Bellis, M.A.; Hughes, K.; Ford, K.; Ramos Rodriguez, G.; Sethi, D.; Passmore, J. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019, 4, e517–e528. [Google Scholar] [CrossRef] [PubMed]
- Courtois, C.A. Complex Trauma, Complex Reactions: Assessment and Treatment. Psychother. Theory Res. Pract. Train. 2004, 41, 412–425. [Google Scholar] [CrossRef]
- Herman, J.L.; Harvey, M.R. Adult Memories of Childhood Trauma: A Naturalistic Clinical Study. J. Trauma Stress 1997, 10, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Milot, T.; Éthier, L.S.; St-Laurent, D.; Provost, M.A. The Role of Trauma Symptoms in the Development of Behavioral Problems in Maltreated Preschoolers. Child Abus. Negl. 2010, 34, 225–234. [Google Scholar] [CrossRef]
- Van Der Kolk, B.A. Developmental Trauma Disorder: Toward a Rational Diagnosis for Children with Complex Trauma Histories. Psychiatr. Ann. 2005, 35, 401–408. [Google Scholar] [CrossRef]
- Department of Health and Human Services. Child Maltreatment Report, 2019; The Administration for Children and Families: Washington, DC, USA, 2019. [Google Scholar]
- Dye, H. The Impact and Long-Term Effects of Childhood Trauma. J. Hum. Behav. Soc. Environ. 2018, 28, 381–392. [Google Scholar] [CrossRef]
- Herzog, J.I.; Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front. Psychiatry 2018, 9, 420. [Google Scholar] [CrossRef]
- Godbout, N.; Daspe, M.-È.; Runtz, M.; Cyr, G.; Briere, J. Childhood Maltreatment, Attachment, and Borderline Personality–Related Symptoms: Gender-Specific Structural Equation Models. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 90–98. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R. Attachment in Adulthood: Structure, Dynamics, and Change, 2nd ed.; Guilford Press: New York, NY, USA, 2016; ISBN 978-1-4625-2554-6. [Google Scholar]
- Bartholomew, K.; Horowitz, L.M. Attachment Styles among Young Adults: A Test of a Four-Category Model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, K. Assessment of Individual Differences in Adult Attachment. Psychol. Inq. 1994, 5, 23–67. [Google Scholar] [CrossRef]
- Greenberg, M.T.; Cicchetti, D.; Cummings, E.M. Attachment in the Preschool Years: Theory, Research and Intervention; The John D. and Catherine T. MacArthur Foundation Series on Mental Health and Development; University of Chicago Press: Chicago, IL, USA; London, UK, 1993; ISBN 978-0-226-30630-8. [Google Scholar]
- Pietromonaco, P.R.; Beck, L.A. Adult Attachment and Physical Health. Curr. Opin. Psychol. 2019, 25, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Greenman, P.S.; Johnson, S.M. Emotionally Focused Therapy: Attachment, Connection, and Health. Curr. Opin. Psychol. 2022, 43, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Pietromonaco, P.R.; Collins, N.L. Interpersonal Mechanisms Linking Close Relationships to Health. Am. Psychol. 2017, 72, 531–542. [Google Scholar] [CrossRef]
- Stuart, S.; Noyes, R. Attachment and Interpersonal Communication in Somatization. Psychosomatics 1999, 40, 34–43. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping Studies: Advancing the Methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An Evidence-Based Approach to Scoping Reviews: EBP Approach to Scoping Reviews. Worldviews Evid. Based Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and Loss: Retrospect and Prospect. Am. J. Orthopsychiatry 1982, 52, 664–678. [Google Scholar] [CrossRef] [PubMed]
- Hepplestone, S.; Holden, G.; Irwin, B.; Parkin, H.J.; Thorpe, L. Using Technology to Encourage Student Engagement with Feedback: A Literature Review. Res. Learn. Technol. 2011, 19, 117–127. [Google Scholar] [CrossRef]
- Bergholz, L.M.; Subic-Wrana, C.; Heylmann, D.; Beutel, M.E.; Wiltink, J.; Kaina, B. DNA Damage in Lymphocytes of Patients Suffering from Complex Traumatization. DNA Repair 2017, 52, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Fagundes, C.P.; Glaser, R.; Kiecolt-Glaser, J.K. Stressful Early Life Experiences and Immune Dysregulation across the Lifespan. Brain. Behav. Immun. 2013, 27, 8–12. [Google Scholar] [CrossRef] [PubMed]
- D’Argenio, A.; Mazzi, C.; Pecchioli, L.; Di Lorenzo, G.; Siracusano, A.; Troisi, A. Early Trauma and Adult Obesity: Is Psychological Dysfunction the Mediating Mechanism? Physiol. Behav. 2009, 98, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.R.; Usher, N.; Dearing, E.; Barkai, A.R.; Crowell-Doom, C.; Neupert, S.D.; Mantzoros, C.S.; Crowell, J.A. Attachment and the Metabolic Syndrome in Midlife: The Role of Interview-Based Discourse Patterns. Psychosom. Med. 2014, 76, 611–621. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nacak, Y.; Morawa, E.; Erim, Y. High Rejection Sensitivity in Patients with Somatoform Pain Disorder. Front. Psychiatry 2021, 12, 602981. [Google Scholar] [CrossRef]
- Nacak, Y.; Morawa, E.; Tuffner, D.; Erim, Y. Insecure Attachment Style and Cumulative Traumatic Life Events in Patients with Somatoform Pain Disorder: A Cross-Sectional Study. J. Psychosom. Res. 2017, 103, 77–82. [Google Scholar] [CrossRef]
- DiTommaso, E.; Brannen-McNulty, C.; Ross, L.; Burgess, M. Attachment Styles, Social Skills and Loneliness in Young Adults. Personal. Individ. Differ. 2003, 35, 303–312. [Google Scholar] [CrossRef]
- Downey, G.; Feldman, S.I. Implications of Rejection Sensitivity for Intimate Relationships. J. Pers. Soc. Psychol. 1996, 70, 1327–1343. [Google Scholar] [CrossRef]
- Reuber, M.; Howlett, S.; Khan, A.; Grünewald, R.A. Non-Epileptic Seizures and Other Functional Neurological Symptoms: Predisposing, Precipitating, and Perpetuating Factors. Psychosomatics 2007, 48, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Ospina, J.P.; Jalilianhasanpour, R.; Fricchione, G.L.; Perez, D.L. Fearful Attachment Linked to Childhood Abuse, Alexithymia, and Depression in Motor Functional Neurological Disorders. J. Neuropsychiatry Clin. Neurosci. 2019, 31, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R.; Paul, S.K.; Bethel, M.A.; Matthews, D.R.; Neil, H.A.W. 10-Year Follow-up of Intensive Glucose Control in Type 2 Diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, L.; Pasman, J.A.; Nicholson, T.; Aybek, S.; David, A.S.; Tuck, S.; Kanaan, R.A.; Roelofs, K.; Carson, A.; Stone, J. Stressful Life Events and Maltreatment in Conversion (Functional Neurological) Disorder: Systematic Review and Meta-Analysis of Case-Control Studies. Lancet Psychiatry 2018, 5, 307–320. [Google Scholar] [CrossRef]
- Perez, D.L.; Matin, N.; Barsky, A.; Costumero-Ramos, V.; Makaretz, S.J.; Young, S.S.; Sepulcre, J.; LaFranceJr, W.C.; Keshavan, M.S.; Dickerson, B.C. Cingulo-Insular Structural Alterations Associated with Psychogenic Symptoms, Childhood Abuse and PTSD in Functional Neurological Disorders. J. Neurol. Neurosurg. Psychiatry 2017, 88, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Selkirk, M.; Duncan, R.; Oto, M.; Pelosi, A. Clinical Differences between Patients with Nonepileptic Seizures Who Report Antecedent Sexual Abuse and Those Who Do Not. Epilepsia 2008, 49, 1446–1450. [Google Scholar] [CrossRef]
- Gerhardt, C.; Hamouda, K.; Irorutola, F.; Rose, M.; Hinkelmann, K.; Buchheim, A.; Senf-Beckenbach, P. Insecure and Unresolved/Disorganized Attachment in Patients with Psychogenic Nonepileptic Seizures. J. Acad. Consult. Liaison Psychiatry 2021, 62, 337–344. [Google Scholar] [CrossRef]
- Bodde, N.M.G.; Brooks, J.L.; Baker, G.A.; Boon, P.A.J.M.; Hendriksen, J.G.M.; Mulder, O.G.; Aldenkamp, A.P. Psychogenic Non-Epileptic Seizures—Definition, Etiology, Treatment and Prognostic Issues: A Critical Review. Seizure 2009, 18, 543–553. [Google Scholar] [CrossRef]
- Brown, R.J.; Reuber, M. Psychological and Psychiatric Aspects of Psychogenic Non-Epileptic Seizures (PNES): A Systematic Review. Clin. Psychol. Rev. 2016, 45, 157–182. [Google Scholar] [CrossRef]
- LaFrance, W.C.; Reuber, M.; Goldstein, L.H. Management of Psychogenic Nonepileptic Seizures. Epilepsia 2013, 54, 53–67. [Google Scholar] [CrossRef]
- Muller, R.T.; Lemieux, K.E.; Sicoli, L.A. Attachment and Psychopathology Among Formerly Maltreated Adults. J. Fam. Violence 2001, 16, 151–169. [Google Scholar] [CrossRef]
- Murphy, B.; Bates, G.W. Adult Attachment Style and Vulnerability to Depression. Personal. Individ. Differ. 1997, 22, 835–844. [Google Scholar] [CrossRef]
- Crittenden, P.M. Maltreated Infants: Vulnerability and Resilience. J. Child Psychol. Psychiatry 1985, 26, 85–96. [Google Scholar] [CrossRef]
- Steele, M.; Baradon, T. Clinical Use of the Adult Attachment Interview in Parent-Infant Psychotherapy. Infant Ment. Health J. 2004, 25, 284–299. [Google Scholar] [CrossRef]
- Brianda, M.E.; Sacchi, C.; De Carli, P.; Simonelli, A. Maltrattamento Emotivo e Sintomi Somatici in Età Giovanile Adulta. Il Ruolo Di Mediazione Dello Stile Di Attaccamento Romantico in Una Popolazione Femminile. Psicol. Della Salut. 2018, 2018/1, 81–101. [Google Scholar] [CrossRef]
- Caplan, R.A.; Maunder, R.G.; Stempak, J.M.; Silverberg, M.S.; Hart, T.L. Attachment, Childhood Abuse, and IBD-Related Quality of Life and Disease Activity Outcomes. Inflamm. Bowel Dis. 2014, 20, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Waldinger, R.J.; Schulz, M.S.; Barsky, A.J.; Ahern, D.K. Mapping the Road from Childhood Trauma to Adult Somatization: The Role of Attachment. Psychosom. Med. 2006, 68, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Ensink, K.; Borelli, J.L.; Normandin, L.; Target, M.; Fonagy, P. Childhood Sexual Abuse and Attachment Insecurity: Associations with Child Psychological Difficulties. Am. J. Orthopsychiatry 2020, 90, 115–124. [Google Scholar] [CrossRef]
- Drossman, D.A.; Patrick, D.L.; Mitchell, C.M.; Zagami, E.A.; Appelbaum, M.I. Health-Related Quality of Life in Inflammatory Bowel Disease: Functional Status and Patient Worries and Concerns. Dig. Dis. Sci. 1989, 34, 1379–1386. [Google Scholar] [CrossRef]
- Dagan, O.; Facompré, C.R.; Bernard, K. Adult Attachment Representations and Depressive Symptoms: A Meta-Analysis. J. Affect. Disord. 2018, 236, 274–290. [Google Scholar] [CrossRef]
- Farrell, A.K.; Waters, T.E.A.; Young, E.S.; Englund, M.M.; Carlson, E.E.; Roisman, G.I.; Simpson, J.A. Early Maternal Sensitivity, Attachment Security in Young Adulthood, and Cardiometabolic Risk at Midlife. Attach. Hum. Dev. 2019, 21, 70–86. [Google Scholar] [CrossRef] [PubMed]
- Bernard, K.; Hostinar, C.E.; Dozier, M. Longitudinal Associations between Attachment Quality in Infancy, C-Reactive Protein in Early Childhood, and BMI in Middle Childhood: Preliminary Evidence from a CPS-Referred Sample. Attach. Hum. Dev. 2019, 21, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Goulter, N.; McMahon, R.J.; Pasalich, D.S.; Dodge, K.A. Indirect Effects of Early Parenting on Adult Antisocial Outcomes via Adolescent Conduct Disorder Symptoms and Callous-Unemotional Traits. J. Clin. Child Adolesc. Psychol. 2020, 49, 930–942. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, S.; Mark, A.G.; Rinawi, F.; Shamir, R.; Assa, A. Micronutrient Deficiencies in Children with Inflammatory Bowel Diseases. Nutr. Clin. Pract. 2020, 35, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Heenan, A.; Greenman, P.S.; Tassé, V.; Zachariades, F.; Tulloch, H. Traumatic Stress, Attachment Style, and Health Outcomes in Cardiac Rehabilitation Patients. Front. Psychol. 2020, 11, 75. [Google Scholar] [CrossRef] [PubMed]
- Akdoğan, R. A Model Proposal on the Relationships between Loneliness, Insecure Attachment, and Inferiority Feelings. Personal. Individ. Differ. 2017, 111, 19–24. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef]
- Kiecolt-Glaser, J.K.; Gouin, J.-P.; Hantsoo, L. Close Relationships, Inflammation, and Health. Neurosci. Biobehav. Rev. 2010, 35, 33–38. [Google Scholar] [CrossRef]
- Bucci, W. Psychoanalysis and Cognitive Science: A Multiple Code Theory; Guilford Press: New York, NY, USA, 1997; ISBN 978-1-57230-213-6. [Google Scholar]
- Bucci, W. Symptoms and Symbols: A Multiple Code Theory of Somatization. Psychoanal. Inq. 1997, 17, 151–172. [Google Scholar] [CrossRef]
- Coan, J.A.; Sbarra, D.A. Social Baseline Theory: The Social Regulation of Risk and Effort. Curr. Opin. Psychol. 2015, 1, 87–91. [Google Scholar] [CrossRef]
- Bucci, W. Emotional Communication and Therapeutic Change: Understanding Psychotherapy through Multiple Code Theory, 1st ed.; Cornell, W.F., Ed.; Series: Relational Perspectives 2020; Routledge: Oxford, UK; New York, NY, USA, 2021; ISBN 978-1-00-312514-3. [Google Scholar]
- Midolo, L.R.; Santoro, G.; Ferrante, E.; Pellegriti, P.; Russo, S.; Costanzo, A.; Schimmenti, A. Childhood Trauma, Attachment and Psychopathology: A Correlation Network Approach. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Granqvist, P.; Sroufe, L.A.; Dozier, M.; Hesse, E.; Steele, M.; Van Ijzendoorn, M.; Solomon, J.; Schuengel, C.; Fearon, P.; Bakermans-Kranenburg, M.; et al. Disorganized Attachment in Infancy: A Review of the Phenomenon and Its Implications for Clinicians and Policy-Makers. Attach. Hum. Dev. 2017, 19, 534–558. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.M. The Practice of Emotionally Focused Couple Therapy: Creating Connection, 3rd ed.; Routledge: Abingdon, UK, 2019; ISBN 978-1-351-16836-6. [Google Scholar]
- McLean, H.Q.; Fiebelkorn, A.P.; Temte, J.L.; Wallace, G.S.; Centers for Disease Control and Prevention. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2013, 62, 1–34. [Google Scholar]
- Tulloch, H.; Johnson, S.; Demidenko, N.; Clyde, M.; Bouchard, K.; Greenman, P.S. An Attachment-Based Intervention for Patients with Cardiovascular Disease and Their Partners: A Proof-of-Concept Study. Health Psychol. 2021, 40, 909–919. [Google Scholar] [CrossRef]
- Main, M.; Goldwyn, R.; Hesse, E. Adult Attachment Scoring and Classification Systems; [Unpublished manuscript]; University of California at Berkeley: Berkeley, CA, USA, 2003. [Google Scholar]
- King, J.A.; Solomon, P.; Ford, J.D. The Cameron Complex Trauma Interview (CCTI): Development, Psychometric Properties, and Clinical Utility. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 18–22. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Greenman, P.S.; Renzi, A.; Monaco, S.; Luciani, F.; Di Trani, M. How Does Trauma Make You Sick? The Role of Attachment in Explaining Somatic Symptoms of Survivors of Childhood Trauma. Healthcare 2024, 12, 203. https://doi.org/10.3390/healthcare12020203
Greenman PS, Renzi A, Monaco S, Luciani F, Di Trani M. How Does Trauma Make You Sick? The Role of Attachment in Explaining Somatic Symptoms of Survivors of Childhood Trauma. Healthcare. 2024; 12(2):203. https://doi.org/10.3390/healthcare12020203
Chicago/Turabian StyleGreenman, Paul Samuel, Alessia Renzi, Silvia Monaco, Francesca Luciani, and Michela Di Trani. 2024. "How Does Trauma Make You Sick? The Role of Attachment in Explaining Somatic Symptoms of Survivors of Childhood Trauma" Healthcare 12, no. 2: 203. https://doi.org/10.3390/healthcare12020203
APA StyleGreenman, P. S., Renzi, A., Monaco, S., Luciani, F., & Di Trani, M. (2024). How Does Trauma Make You Sick? The Role of Attachment in Explaining Somatic Symptoms of Survivors of Childhood Trauma. Healthcare, 12(2), 203. https://doi.org/10.3390/healthcare12020203






