The Role of Emotion Dysregulation in Understanding Suicide Risk: A Systematic Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
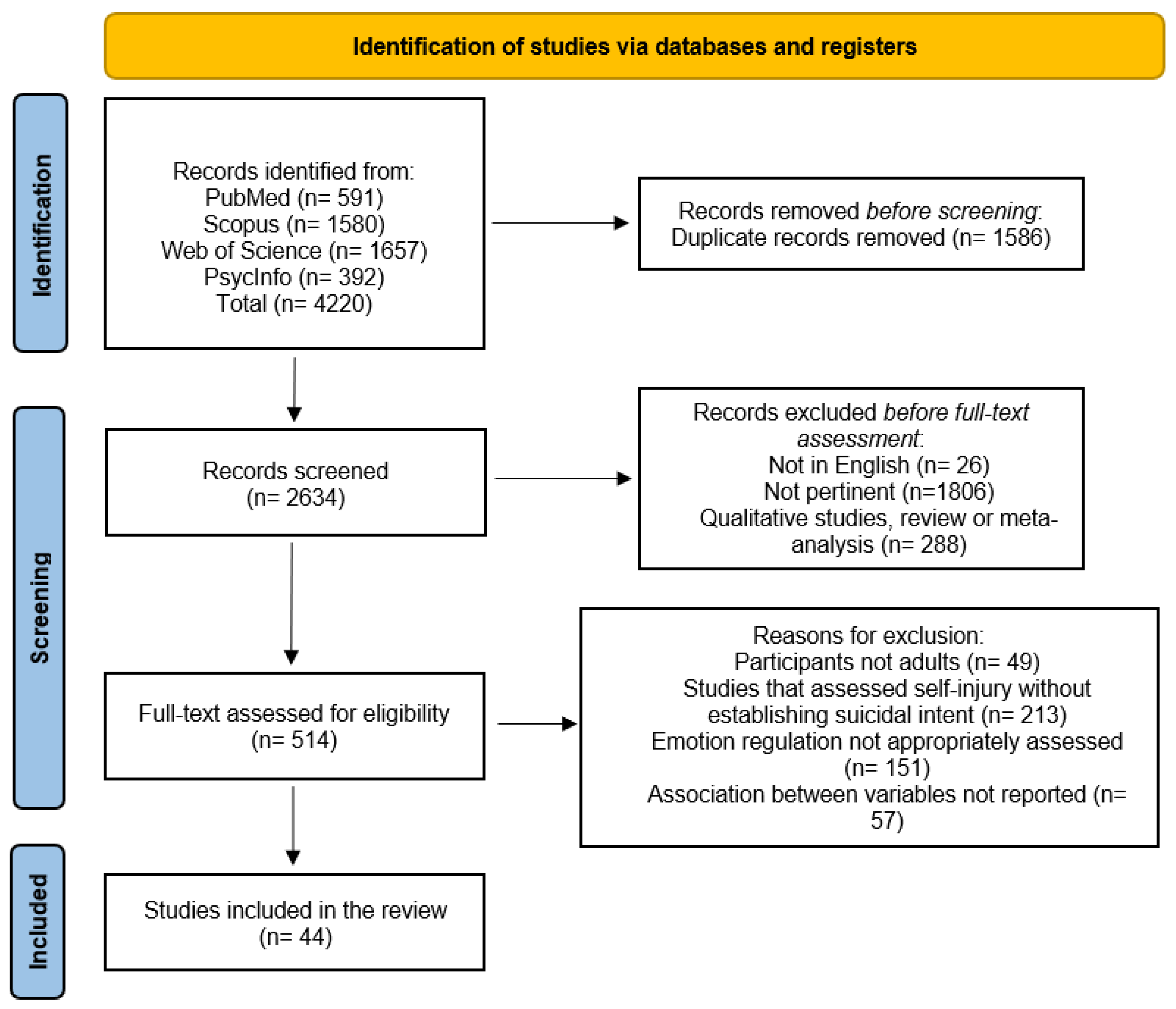
2.3. Study Selection and Data Collection
2.4. Study Inclusion
2.5. Study Quality Assessment
3. Results
3.1. Study Characteristics
3.2. Suicidal Ideation and Suicidal Behavior Measures
3.3. Emotional Regulation and Suicidal Ideation
3.3.1. Emotional Regulation and Suicidal Ideation in Clinical Samples
3.3.2. Specific Dimensions of Emotional Regulation
3.3.3. Emotional Regulation and Suicidal Ideation in Nonclinical Samples
3.4. Emotional Regulation and Suicide Attempts
3.4.1. Emotional Regulation and Suicide Attempts in Clinical Samples
3.4.2. Emotional Regulation and Suicide Attempts in Nonclinical Samples
3.5. Emotional Regulation as a Mediator
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Live Life: An Implementation Guide for Suicide Prevention in Countries; World Health Organization: Geneva, Switzerland, 2021; p. 12. [Google Scholar]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, K.C.; Jazaieri, H.; Gross, J.J. Emotion Regulation: A Transdiagnostic Perspective on a New RDoC Domain. Cognit. Ther. Res. 2016, 40, 426–440. [Google Scholar] [CrossRef]
- Shneidman, E.S. Suicide as psychache. J. Nerv. Ment. Dis. 1993, 181, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Joiner, T.E. Why People Die by Suicide; Harvard University Press: Cambridge, MA, USA, 2005. [Google Scholar]
- Gross, J.J.; Muñoz, R.F. Emotion regulation and mental health. Clin. Psychol. Sci. Pract. 1995, 2, 151. [Google Scholar] [CrossRef]
- Adrian, M.; Zeman, J.; Erdley, C.; Lisa, L.; Sim, L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. J. Abnorm. Child. Psychol. 2011, 39, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Pope, A.W.; Bierman, K.L. Predicting adolescent peer problems and antisocial activities: The relative roles of aggression and dysregulation. Dev. Psychol. 1999, 35, 335–346. [Google Scholar] [CrossRef]
- Anestis, M.D.; Pennings, S.M.; Lavender, J.M.; Tull, M.T.; Gratz, K.L. Low distress tolerance as an indirect risk factor for suicidal behavior: Considering the explanatory role of nonsuicidal self-injury. Compr. Psychiatry 2013, 54, 996–1002. [Google Scholar] [CrossRef]
- Anestis, M.D.; Kleiman, E.M.; Lavender, J.M.; Tull, M.T.; Gratz, K.L. The pursuit of death versus escape from negative affect: An examination of the nature of the relationship between emotion dysregulation and both suicidal behavior and nonsuicidal self-injury. Compr. Psychiatry 2014, 55, 1820–1830. [Google Scholar] [CrossRef]
- O’Connor, R.C. Toward an integrated motivational–volitional model of suicidal behavior. In International Handbook of Suicide Prevention: Research, Policy and Practice; O’Connor, R.C., Platt, S., Gordon, J., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2011; pp. 181–198. [Google Scholar]
- Klonsky, E.D.; May, A.M. The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” framework. Int. J. Cogn. Ther. 2015, 8, 114–129. [Google Scholar] [CrossRef]
- Pompili, M.; Innamorati, M.; Venturini, P.; Serafini, G.; Lester, D.; Girardi, P. Child abuse as a risk factor for suicide in life: A selective overview. Minerva Psichiatr. 2011, 52, 61–69. [Google Scholar]
- Mayorga, N.A.; Jardin, C.; Bakhshaie, J.; Garey, L.; Viana, A.G.; Cardoso, J.B.; Zvolensky, M. Acculturative stress, emotion regulation, and affective symptomology among Latino/a college students. J. Couns. Psychol. 2018, 65, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.B.; McLaughlin, K.A.; Busso, D.S.; Brueck, S.; Peverill, M.; Sheridan, M.A. Neural Correlates of Emotion Regulation and Adolescent Suicidal Ideation. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2018, 3, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Eaddy, M.; Zullo, L.; Horton, S.E.; Hughes, J.L.; Kennard, B.; Diederich, A.; Emslie, G.J.; Schuster, L.; Stewart, S.M. A Theory-Driven Investigation of the Association Between Emotion Dysregulation and Suicide Risk in a Clinical Adolescent Sample. Suicide Life Threat. Behav. 2019, 49, 928–940. [Google Scholar] [CrossRef]
- Gratz, K.L.; Spitzen, T.L.; Tull, M.T. Expanding our understanding of the relationship between nonsuicidal self-injury and suicide attempts: The roles of emotion regulation self-efficacy and the acquired capability for suicide. J. Clin. Psychol. 2020, 76, 1653–1667. [Google Scholar] [CrossRef] [PubMed]
- De la Torre-Luque, A.; Essau, C.A.; Lara, E.; Leal-Leturia, I.; Borges, G. Childhood emotional dysregulation paths for suicide-related behavior engagement in adolescence. Eur. Child Adolesc. Psychiatry 2023, 32, 2581–2592. [Google Scholar] [CrossRef] [PubMed]
- Colmenero-Navarrete, L.; García-Sancho, E.; Salguero, J.M. Relationship Between Emotion Regulation and Suicide Ideation and Attempt in Adults and Adolescents: A Systematic Review. Arch. Suicide Res. 2022, 26, 1702–1735. [Google Scholar] [CrossRef]
- Anestis, M.D.; Bagge, C.L.; Tull, M.T.; Joiner, T.E. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. J. Psychiatr. Res. 2011, 45, 603–611. [Google Scholar] [CrossRef]
- Pisani, A.R.; Wyman, P.A.; Petrova, M.; Schmeelk-Cone, K.; Goldston, D.B.; Xia, Y.; Gould, M.S. Emotion regulation difficulties, youth-adult relationships, and suicide attempts among high school students in underserved communities. J. Youth Adolesc. 2013, 42, 807–820. [Google Scholar] [CrossRef]
- Domínguez-García, E.; Fernández-Berrocal, P. The Association Between Emotional Intelligence and Suicidal Behavior: A Systematic Review. Front. Psychol. 2018, 30, 2380. [Google Scholar] [CrossRef]
- Turton, H.; Berry, K.; Danquah, A.; Pratt, D. The relationship between emotion dysregulation and suicide ideation and behavior: A systematic review. J. Affect. Disord. Rep. 2021, 5, 100136. [Google Scholar] [CrossRef]
- Rigucci, S.; Sarubbi, S.; Erbuto, D.; Rogante, E.; Hantouche, E.G.; Innamorati, M.; Lester, D.; Pompili, M. Negative emotion dysregulation is linked to the intensity of suicidal ideation in a mixed inpatient sample. J. Affect. Disord. 2021, 15, 605–608. [Google Scholar] [CrossRef]
- Laghaei, M.; Mehrabizadeh Honarmand, M.; Jobson, L.; Abdollahpour Ranjbar, H.; Habibi Asgarabad, M. Pathways from childhood trauma to suicidal ideation: Mediating through difficulties in emotion regulation and depressive symptoms. BMC Psychiatry 2023, 23, 295. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Al-Dajani, N.; Uliaszek, A.A.; Hamdullahpur, K. It is the thought that counts: Belief in suicide as an escape moderates the relationship between emotion dysregulation and suicidal ideation cross-sectionally and longitudinally. Borderline Personal. Disord. Emot. Dysregul. 2019, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Ammerman, B.A.; Kleiman, E.M.; Uyeji, L.L.; Knorr, A.C.; McCloskey, M.S. Suicidal and violent behavior: The role of anger, emotion dysregulation, and impulsivity. Pers. Individ. Dif. 2015, 79, 57–62. [Google Scholar] [CrossRef]
- Baer, M.M.; LaCroix, J.M.; Browne, J.C.; Hassen, H.O.; Perera, K.U.; Soumoff, A.; Weaver, J.; Ghahramanlou-Holloway, M. Impulse control difficulties while distressed: A facet of emotion dysregulation links to Non-Suicidal Self-Injury among psychiatric inpatients at military treatment facilities. Psychiatry Res. 2018, 269, 419–424. [Google Scholar] [CrossRef]
- Bentley, K.H.; Sauer-Zavala, S.; Stevens, K.T.; Washburn, J.J. Implementing an evidence-based psychological intervention for suicidal thoughts and behaviors on an inpatient unit: Process, challenges, and initial findings. Gen. Hosp. Psychiatry 2020, 63, 76–82. [Google Scholar] [CrossRef]
- Clapham, R.; Brausch, A. Emotion regulation deficits across the spectrum of self-harm. Death Stud. 2022, 46, 2477–2484. [Google Scholar] [CrossRef]
- Decker, S.E.; Hoff, R.; Martino, S.; Mazure, C.M.; Park, C.L.; Porter, E.; Kraus, S.W. Is Emotion Dysregulation Associated with Suicidal Ideation in Post 9/11 Veterans? Arch. Suicide Res. 2021, 25, 126–140. [Google Scholar] [CrossRef]
- Denning, D.M.; Perry, T.R.; Reilly, E.E.; Berner, L.A.; Velkoff, E.A.; Kaye, W.H.; Wierenga, C.E.; Brown, T.A. Associations of suicide risk with emotional reactivity, dysregulation, and eating disorder treatment outcomes. Suicide Life Threat. Behav. 2022, 52, 1126–1139. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Gordon, K.L.; Tull, M.T.; Gratz, K.L. Self-injurious behaviors in posttraumatic stress disorder: An examination of potential moderators. J. Affect. Disord. 2014, 166, 359–367. [Google Scholar] [CrossRef]
- Duggan, J.M.; Toste, J.R.; Heath, N.L. An examination of the relationship between body image factors and nonsuicidal self-injury in young adults: The mediating influence of emotion dysregulation. Psychiatry Res. 2013, 206, 256–264. [Google Scholar] [CrossRef]
- Fadoir, N.A.; Lutz-Zois, C.J.; Goodnight, J.A. Psychopathy and suicide: The mediating effects of emotional and behavioral dysregulation. Pers. Individ. Dif. 2019, 142, 1–6. [Google Scholar] [CrossRef]
- Ghorbani, F.; Khosravani, V.; Sharifi Bastan, F.; Jamaati Ardakani, R. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol-dependent outpatients. Psychiatry Res. 2017, 252, 223–230. [Google Scholar] [CrossRef]
- Gómez-Expósito, A.; Wolz, I.; Fagundo, A.B.; Granero, R.; Steward, T.; Jiménez-Murcia, S.; Agüera, Z.; Fernández-Aranda, F. Correlates of Nonsuicidal Self-Injury and Suicide Attempts in Bulimic Spectrum Disorders. Front. Psychol. 2016, 7, 1244. [Google Scholar] [CrossRef] [PubMed]
- Haliczer, L.A.; Harnedy, L.E.; Oakley, M.; Dixon-Gordon, K.L. Clarifying the Role of Multiple Self-Damaging Behaviors in the Association Between Emotion Dysregulation and Suicide Risk Among College Students. J. Prim. Prev. 2021, 42, 473–492. [Google Scholar] [CrossRef] [PubMed]
- Harris, L.; Chelminski, I.; Dalrymple, K.; Morgan, T.; Zimmerman, M. Suicide attempts and emotion regulation in psychiatric outpatients. J. Affect. Disord. 2018, 232, 300–304. [Google Scholar] [CrossRef]
- Khazem, L.R.; Anestis, M.D. Thinking or doing? An examination of well-established suicide correlates within the ideation-to-action framework. Psychiatry Res. 2016, 245, 321–326. [Google Scholar] [CrossRef]
- Lemaigre, C.; Taylor, E.P. Mediators of childhood trauma and suicidality in a cohort of socioeconomically deprived Scottish men. Child Abuse Negl. 2019, 88, 159–170. [Google Scholar] [CrossRef]
- Mallorquí-Bagué, N.; Mena-Moreno, T.; Granero, R.; Vintró-Alcaraz, C.; Sánchez-González, J.; Fernández-Aranda, F.; Pino-Gutiérrez, A.D.; Mestre-Bach, G.; Aymamí, N.; Gómez-Peña, M.; et al. Suicidal ideation and history of suicide attempts in treatment-seeking patients with gambling disorder: The role of emotion dysregulation and high trait impulsivity. J. Behav. Addict. 2018, 7, 1112–1121. [Google Scholar] [CrossRef]
- Martin, C.; Vujanovic, A.; Day, S.X. Posttraumatic stress disorder symptom severity and emotion regulation in acute-care psychiatric inpatients: Associations with suici- dality. J. Aggress. Maltreat. Trauma 2017, 26, 1024–1041. [Google Scholar] [CrossRef]
- Mata-Greve, F.; Johnson, M.; Blanchard, B.E. A longitudinal examination of cultural risk factors for suicide and emotion regulation. Am. J. Orthopsychiatry 2022, 92, 635–645. [Google Scholar] [CrossRef]
- Miranda, R.; Tsypes, A.; Gallagher, M.; Rajappa, K. Rumination and hopelessness as mediators of the relation between perceived emotion dysregulation and suicidal ideation. Cognit Ther. Res. 2013, 37, 786–795. [Google Scholar] [CrossRef]
- Mohammadzadeh, A.; Ganji, Z.; Khosravani, V.; Mohammadpanah Ardakan, A.; Amirinezhad, A. Direct and indirect associations between perception of childhood trauma and suicidal ideation through emotion dysregulation in males who use heroin. Addict. Behav. 2019, 98, 106011. [Google Scholar] [CrossRef]
- Neacsiu, A.D.; Fang, C.M.; Rodriguez, M.; Rosenthal, M.Z. Suicidal Behavior and Problems with Emotion Regulation. Suicide Life Threat. Behav. 2018, 48, 52–74. [Google Scholar] [CrossRef]
- Orr, M.F.; Rogers, A.H.; Shepherd, J.M.; Buckner, J.D.; Ditre, J.W.; Bakhshaie, J.; Zvolensky, M.J. Is there a relationship between cannabis use problems, emotion dysregulation, and mental health problems among adults with chronic pain? Psychol. Health Med. 2020, 25, 742–755. [Google Scholar] [CrossRef]
- Palagini, L.; Cipollone, G.; Masci, I.; Caruso, D.; Paolilli, F.; Perugi, G.; Riemann, D. Insomnia symptoms predict emotional dysregulation, impulsivity and suicidality in depressive bipolar II patients with mixed features. Compr. Psychiatry 2019, 89, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Palagini, L.; Cipollone, G.; Moretto, U.; Masci, I.; Tripodi, B.; Caruso, D.; Perugi, G. Chronobiological dis-rhythmicity is related to emotion dysregulation and suicidality in depressive bipolar II disorder with mixed features. Psychiatry Res. 2019, 271, 272–278. [Google Scholar] [CrossRef]
- Palagini, L.; Miniati, M.; Marazziti, D.; Massa, L.; Grassi, L.; Geoffroy, P.A. Circadian Rhythm Alterations May be Related to Impaired Resilience, Emotional Dysregulation and to the Severity of Mood Features in Bipolar I and II Disorders. Clin. Neuropsychiatry 2022, 19, 174–186. [Google Scholar] [PubMed]
- Pisetsky, E.M.; Haynos, A.F.; Lavender, J.M.; Crow, S.J.; Peterson, C.B. Associations between emotion regulation difficulties, eating disorder symptoms, nonsuicidal self-injury, and suicide attempts in a heterogeneous eating disorder sample. Compr. Psychiatry 2017, 73, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Ponzoni, S.; Beomonte Zobel, S.; Rogier, G.; Velotti, P. Emotion dysregulation acts in the relationship between vulnerable narcissism and suicidal ideation. Scand. J. Psychol. 2021, 62, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Raudales, A.M.; Carosa, C.L.; Weiss, N.H.; Schatten, H.T.; Armey, M.F. Emotion dysregulation as a mechanism linking posttraumatic stress disorder to subsequent suicidal thoughts and behaviors following inpatient psychiatric discharge. J. Psychiatr. Res. 2023, 161, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Cano, R.; Paulus, D.J.; Derrick, J.L.; Blalock, J.A.; Zvolensky, M.J. Emotion dysregulation and hazardous drinking in relation to suicidal ideation among Spanish-speaking Latinx daily smokers. J. Subst. Abuse Treat. 2022, 132, 108508. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.L.; Joiner, T.E. Suicide-Specific Rumination Relates to lifetime suicide attempts above and beyond a variety of other suicide risk factors. J. Psychiatr. Res. 2018, 98, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.L.; Hom, M.A.; Dougherty, S.P.; Gallyer, A.J.; Joiner, T.E. Comparing Suicide Risk Factors Among Individuals with a History of Aborted, Interrupted, and Actual Suicide Attempts. Arch. Suicide Res. 2020, 24 (Suppl. S1), 57–74. [Google Scholar] [CrossRef]
- Rufino, K.A.; Viswanath, H.; Wagner, R.; Patriquin, M.A. Body dissatisfaction and suicidal ideation among psychiatric inpatients with eating disorders. Compr. Psychiatry 2018, 84, 22–25. [Google Scholar] [CrossRef]
- Rufino, K.A.; Ward-Ciesielski, E.F.; Webb, C.A.; Nadorff, M.R. Emotion regulation difficulties are associated with nightmares and suicide attempts in an adult psychiatric inpatient sample. Psychiatry Res. 2020, 293, 113437. [Google Scholar] [CrossRef]
- Silvers, J.A.; Hubbard, A.D.; Chaudhury, S.; Biggs, E.; Shu, J.; Grunebaum, M.F.; Fertuck, E.; Weber, J.; Kober, H.; Carson-Wong, A.; et al. Suicide attempters with borderline personality disor- der show differential orbitofrontal and parietal recruitment when reflecting on aver- sive memories. J. Psychiatr. Res. 2016, 81, 71–78. [Google Scholar] [CrossRef]
- Turton, H.; Berry, K.; Danquah, A.; Green, J.; Pratt, D. An investigation of whether emotion regulation mediates the relationship between attachment insecurity and suicidal ideation and behavior. Clin. Psychol. Psychother. 2022, 29, 1587–1598. [Google Scholar] [CrossRef]
- Van Eck, K.; Ballard, E.; Hart, S.; Newcomer, A.; Musci, R.; Flory, K. ADHD and Suicidal Ideation: The Roles of Emotion Regulation and Depressive Symptoms Among College Students. J. Atten. Disord. 2015, 19, 703–714. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zhang, S.; Liu, X.; Hou, J.; Hou, X. Emotion reactivity, emotion dysregulation, and suicidality among Chinese undergraduates: A study based on the “ideation-to-action” framework. Curr. Psychol. 2021, 42, 3204–3212. [Google Scholar] [CrossRef]
- Yang, C.; Wang, J.; Shao, Y.; Liu, M.; Geng, F. Antisocial and borderline personality traits and childhood trauma in male prisoners: Mediating effects of difficulties in emotional regulation. Child Abuse Negl. 2022, 132, 105822. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Shim, S.H.; Kim, J.S. Electrophysiological Changes Between Patients with Suicidal Ideation and Suicide Attempts: An Event-Related Potential Study. Front. Psychiatry 2022, 13, 900724, Erratum in Front. Psychiatry 2022, 13, 969450. [Google Scholar] [CrossRef] [PubMed]
- Zeifman, R.J.; Antony, M.M.; Kuo, J.R. When being imperfect just will not do: Exploring the relationship between perfectionism, emotion dysregulation, and suicidal ideation. Pers. Individ Differ. 2020, 152, 109612. [Google Scholar] [CrossRef]
- Zemestani, M.; Abdolmaleki, S.; McGrew, S.J.; Vujanovic, A. Associations between Sleep Disturbance and Suicidal Ideation Severity in Iranian University Students: Evaluating Emotion Regulation Difficulties and Distress Tolerance. Arch. Suicide Res. 2023, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Zobel, S.B.; Bruno, S.; Torru, P.; Rogier, G.; Velotti, P. Investigating the Path from Non-Suicidal Self-Injury to Suicidal Ideation: The Moderating Role of Emotion Dysregulation. Psychiatry Investig. 2023, 20, 616–624. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Ranieri, W.F. Scale for Suicide Ideation: Psychometric properties of a self-report version. J. Clin. Psychol. 1988, 44, 499–505. [Google Scholar] [CrossRef]
- Osman, A.; Bagge, C.L.; Gutierrez, P.M.; Konick, L.C.; Kopper, B.A.; Barrios, F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment 2001, 8, 443–454. [Google Scholar] [CrossRef]
- Beck, A.T.; Kovacs, M.; Weissman, A. Assessment of suicidal intention: The Scale for Suicide Ideation. J. Consult. Clin. Psychol. 1979, 47, 343–352. [Google Scholar] [CrossRef]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S.; et al. The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef]
- Nock, M.K.; Holmberg, E.B.; Photos, V.I.; Michel, B.D. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychol. Assess. 2007, 19, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Rajappa, K.; Gallagher, M.; Miranda, R. Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cognit Ther. Res. 2012, 36, 833–839. [Google Scholar] [CrossRef]
- Hatkevich, C.; Penner, F.; Sharp, C. Difficulties in emotion regulation and suicide ideation and attempt in adolescent inpatients. Psychiatry Res. 2019, 271, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Turecki, G.; Ernst, C.; Jollant, F.; Labonté, B.; Mechawar, N. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012, 35, 14–23. [Google Scholar] [CrossRef]
- Turecki, G. The molecular bases of the suicidal brain. Nat. Rev. Neurosci. 2014, 15, 802–816. [Google Scholar] [CrossRef]
- Turecki, G.; Brent, D.A.; Gunnell, D.; O’Connor, R.C.; Oquendo, M.A.; Pirkis, J.; Stanley, B.H. Suicide and suicide risk. Nat. Rev. Dis. Primers 2019, 5, 74. [Google Scholar] [CrossRef]
- Porges, S.W. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology 1995, 32, 301–318. [Google Scholar] [CrossRef]
- Porges, S.W. Polyvagal Theory: A Science of Safety. Front. Integr. Neurosci. 2022, 16, 871227. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.P.; Bittencourt-Hewitt, A.; Sebastian, C.L. Neurocognitive bases of emotion regulation development in adolescence. Dev. Cogn. Neurosci. 2015, 15, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Linehan, M.M. DBT Skills Training Manual, 2nd ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- O’Connor, R.C.; Nock, M.K. The psychology of suicidal behavior. Lancet Psychiatry 2014, 1, 73–85. [Google Scholar] [CrossRef] [PubMed]
| Authors and Year | Country | Sample Characteristics | Design | Main Suicidal Outcomes and Measures Used | Main Findings | Quality Score |
|---|---|---|---|---|---|---|
| Al-Dajani et al., 2019 [28] | Canada | 101 community participants recruited through advertisement | Longitudinal | SI through18 items of the BSS and 2 items of the SBQ-14 | ED is significantly and positively correlated with SI at baseline and at follow-up. Baseline ED predicted SI at follow-up. Finally, the belief that suicide is a solution to a problem did not moderate the ED-SI longitudinal relationship. | 4 |
| Ammerman et al., 2014 [29] | USA | 2295 undergraduate students | Cross-sectional | SA through 1 item of the SBQ-R | Those with previous SAs had significantly higher DERS scores. DERS was a mediator in the relationship between anger and SA. | 3 |
| Anestis et al., 2014 [11] | USA | Study 1: 1317 undergraduate students; Study 2: 93 adult inpatients in treatment for SUD | Cross-sectional | Study 1: SA through MEPOS Study 2: SA through L-SASI | The results showed significant and positive correlations between SAs and DERS scores. DERS directly affected SA, which remained significant when NSSI was entered into the model. | 3 |
| Baer et al., 2018 [30] | USA | 186 psychiatric inpatients hospitalized for SI or SA and with at least one SA | Cross-sectional | SI through SSI and C-SSRS SA through C-SSRS | Worst lifetime SI was significantly and positively correlated with the “Strategies” dimension of DERS. The results of multiple linear regression with SI as a dependent variable were not significant. Individuals with multiple SAs scored higher on the Strategies subscale than individuals with a single attempt. In multiple logistic regression, no DERS subscale significantly differentiated between individuals with single vs. multiple SA. | 4 |
| Bentley et al., 2018 [31] | USA | 150 inpatients with SI and SA | Cross-sectional | SI through item 9 of PHQ-9 | There was a positive and significant correlation between SI and DERS scores. | 3 |
| Clapham et al., 2022 [32] | USA | 708 undergraduate students | Cross-sectional | SI through item 9 of BDI SA through 1 dichotomic question | The linear regression with ED as an independent variable and SI as a dependent variable was significant, accounting for 36.7% of the variance. After controlling for depression and gender, the “Strategies” dimension of DERS was the only subscale significantly associated with SI. The linear regression with ED as an independent variable and SA as a dependent variable was not significant. | 3 |
| Decker et al., 2019 [33] | USA | 278 U.S. veterans | Cross-sectional | SI and SA through C-SSRS | There were weak significant positive correlations between DERS and passive SI, active SI, and lifetime SAs. DERS remained a significant predictor when controlling for homelessness, deployment, sexual harassment, and postdeployment social support, but not when controlling for depression and PTSD symptoms. | 5.5 |
| Denning et al., 2022 [34] | USA | 201 patients with eating disorders in a partial hospitalization program | Cross-sectional | Suicide risk and lifetime SA through MINI-suicidality module. The total score was used to classify participants into three clinical risk categories: low, moderate, and high risk. | At a bivariate level, all DERS subscales, except for “Awareness”, were significantly associated with suicide risk severity and frequency of lifetime SAs. Limited access to adaptive ER strategies, difficulties engaging in goal-oriented behaviors, and engaging in impulsive behavior when experiencing negative emotions were associated with SA frequency. ED was not associated with suicide risk severity, even when controlling for depressive symptoms. | 4 |
| Dixon-Gordon et al., 2014 [35] | USA | 246 patients admitted to a SUD residential treatment facility | Cross-sectional | SA through LPC | There was no significant relationship between DERS and SA history. | 4 |
| Duggan et al., 2013 [36] | Canada | 202 university students (101 reporting lifetime NSSI + 101 matched controls) | Cross-sectional | SI related to bodily experiences through BIAI | BIAI suicide-related rumination was significantly associated with DERS scores. DERS scores significantly mediated the relationship between suicide-related rumination and NSSI. | 4 |
| Fadoir et al., 2019 [37] | USA | 228 offenders | Cross-sectional | SI and SA through items 2 and 4 of SBQ-R | There were weak but significant positive correlations between DERS and SI. DERS, rumination, recent ideation, and NSSI mediated the relationship between psychopathy and SI. | 3 |
| Ghorbani et al., 2017 [38] | Iran | 205 treatment-seeking alcohol dependent outpatients + 100 healthy controls | Cross-sectional | Suicide risk through the SSI. SA through anamnestic questions | Patients with lifetime SA showed higher scores on DERS. Suicide risk showed significant and positive correlations with all of the subscales of DERS. The results of the binary logistic regression showed that two dimensions of DERS (impulsivity and difficulties in goal-directed behaviors) were significant predictors of suicide risk. | 4.5 |
| Gomez-Exposito et al., 2016 [39] | Spain | 122 female patients from an eating disorder unit | Cross-sectional | SA through a dichotomic question | DERS scores were significantly higher in those with a history of SA. | 2 |
| Haliczer et al., 2021 [40] | USA | 181 undergraduate students | Cross-sectional | Suicide risk (including lifetime SI and SA) through SBQ-R | The total score of DERS was significantly and positively associated with suicide risk. The findings revealed an interaction between emotion dysregulation and self-damaging behaviors for suicide risk, with engagement in more forms of self-damaging behaviors (NSSI, eating disorders, alcohol, and drug use) conferring a higher risk for suicide, particularly in the context of greater emotion dysregulation. Moreover, greater emotion dysregulation had an indirect effect on elevated suicide risk via the number of self-damaging behaviors. | 2.5 |
| Harris et al., 2018 [41] | USA | 1046 psychiatric outpatients (160 with previous SA) | Cross-sectional | SA through a dichotomic question | Significantly higher total DERS scores were found in patients with previous SAs. DERS was not independently associated with SA history. | 3 |
| Khazem and Anestis, 2016 [42] | USA | 378 adults recruited online | Cross-sectional | SI and SA through 2 items of SITBI | Those with SI or SA had significantly higher mean DERS scores than participants without SI or SA. | 4 |
| Lemaigre and Taylor, 2019 [43] | Scotland | 86 males from a community group for past or current suicidality | Cross-sectional | SI and SA through SBQ-R | There was a significant positive correlation between DERS and both SI and SA. DERS total score and social inhibition mediated the relationship between CT and SA. | 4.5 |
| Mallorquì-Bagué et al., 2018 [44] | Spain | 249 inpatients with GD | Cross-sectional | SI and SA through clinical interview | DERS scores were significantly higher in the SI group. There was no significant difference in DERS scores in this group between those with SA and those without SA. DERS and GD severity indirectly increased the risk of SI through psychopathological symptoms. | 4 |
| Martin et al., 2017 [45] | USA | 128 psychiatric inpatients | Cross-sectional | SA, suicidality at admission and suicidality during hospitalization through BSS | There were significant positive correlations between DERS, suicidality upon admission, and SI severity (not significant when controlling for other variables). No significant correlation between DERS and SA, or suicidality during hospitalization. | 3 |
| Mata-Greve et al., 2022 [46] | USA | 387 LGBTQ (203) and/or BIPOC (246) individuals | Longitudinal | SB through SBQ-R | ED measured at T2 was positively related to SB at T3 in both populations. In both samples, the total indirect effect of cultural stressors of suicide at T1 on SB at T3 via DERS at T2 was not significant. | 4.5 |
| Miranda et al., 2013 [47] | USA | 143 university students | Longitudinal | SI through BSS SA through a dichotomic question | There was a significant difference in DERS scores between those with multiple SAs, one SA, and no SA. There was a weak but significant positive correlation between baseline DERS and BSS at follow-up and a moderate positive correlation between baseline DERS and baseline SA history. | 4 |
| Mohammadzadeh et al., 2019 [48] | Iran | 310 males with SUD | Cross-sectional | SI through SSI Lifetime SA through anamnestic questions | All DERS dimensions were significantly associated with SI. CT was indirectly associated with suicidal ideation through some DERS dimensions (Nonacceptance, Strategies, and Awareness). | 3.5 |
| Neacsiu et al., 2018 [49] | USA | Study 1: 120 adults Study 2: 95 adults (51 with MDD + 44 healthy controls) | Cross-sectional | Study 1: SI through ASIQ Study 2: SA through SASII | In study 1, DERS was a significant predictor of SI and accounted for 11% of the variance. In study 2, those with a SA history had significantly higher DERS scores. | 4.5 |
| Orr et al., 2020 [50] | USA | 431 opioid-using adults with chronic pain | Cross-sectional | SI through item 9 of BDI | ED was significantly and positively correlated with SI. The results indicated a significant indirect relationship between cannabis-use problems and SI through ED. | 3.5 |
| Palagini et al., 2019 [51] | Italy | 77 patients with BD-II | Cross-sectional | SI through SSI | There was a significant positive correlation between DERS and SI. | 3.5 |
| Palagini et al., 2019 [52] | Italy | 85 patients with BD-II + 35 healthy controls | Cross-sectional | SI through SSI | There was no correlation between suicidality and DERS in the group of healthy controls. In those with BD, there was a significant positive correlation between suicidality and DERS. DERS mediated the association between disrhythmicity of social aspects and suicidality. | 4.5 |
| Palagini et al., 2022 [53] | Italy | 197 psychiatric inpatients with BD | Cross-sectional | SI through SSI | SI showed significant correlations with DERS total score and Impulsivity, Awareness, and Strategies dimensions. According to linear regression analyses, passive SI was related to several DERS dimensions (Strategies and Impulsivity). The dimension of Strategies was a significant predictor of active SI and suicide plans. The results of the mediation analyses showed that the DERS total score acted as a mediator between chronobiological disrythmicity and suicidal risk. Finally, the DERS total score and the dimension of Impulsivity acted as mediators between depressive symptoms and suicidal risk. | 2.5 |
| Pisetsky et al., 2017 [54] | USA | 110 patients in treatment for eating disorders | Cross-sectional | SA through 1 dichotomic question adapted from the SITBI | None of the DERS scores significantly differed between those with and without a lifetime history of SA. | 2.5 |
| Ponzoni et al., 2021 [55] | Italy | 70 individuals with SI + 154 community participants | Cross-sectional | SI through BSS | Significant positive correlation between SI, DERS total score, and all DERS dimensions, except for Awareness. Moreover, DERS total score fully mediated the relationship between vulnerable narcissism and SI. | 4 |
| Raudales et al., 2023 [56] | USA | 362 psychiatric inpatients with PTSD | Longitudinal | SI and SA through C-SSRS assessed at 6-week postdischarge | ED at the 3-week follow-up was significantly and positively associated with SI, but not SAs at the 6-week follow-up. The association between PTSD and ED was significant, as was the association between ED and SI. Furthermore, the indirect effect of PTSD on SI through ED was also significant, while the direct effect linking PTSD and SI was not significant when accounting for ED. The association between PTSD and ED was significant while the association between ED and SA was not significant. The indirect effect of PTSD on SA through ED was also not significant, nor was the direct effect linking PTSD and SA when accounting for ED. Significant indirect effects of PTSD on SI through ED were found for the dimensions “Goal”, “Impulse”, “Strategies”, and ”Clarity”, while the subscales “Accept” and ”Awareness” were not significant. | 5 |
| Rodriguez-Cano et al., 2022 [57] | USA | 371 Spanish-speaking daily smokers | Cross-sectional | SI through item 9 of BDI | SI was significantly and positively correlated with the DERS total score. There was a positive and statistically significant main effect of ED on SI. Moreover, there was a statistically significant interaction of ED and hazardous drinking status; ED was significantly related to SI among hazardous drinkers. | 3.5 |
| Rogers and Joiner, 2018 [58] | USA | 300 undergraduate students | Cross-sectional | SI and SA through SRS and BSS | There was a significant but weak positive correlation between DERS and previous SAs. There was a significant moderate correlation between DERS and SI. Logistic regression suggested that DERS was unrelated to lifetime SA. | 3 |
| Rogers et al., 2020 [59] | USA | 167 undergraduate students who reported SI and/or SA | Cross-sectional | SI through BSS and DSI-SS SAs, method and lethality through a semistructured interview adapted from SITBI and BLS | ED total score differed between aborted, interrupted, and actual attempters, specifically those with higher mean scores. | 2.5 |
| Rufino et al., 2018 [60] | USA | 432 psychiatric inpatients | Cross-sectional | SI and SA through C-SSRS | Significant positive correlations existed between DERS and passive SI, active SI, and SI intensity. In ANCOVA, the covariate DERS was significantly related to SI. | 3.5 |
| Rufino et al., 2020 [61] | USA | 2683 psychiatric inpatients | Cross-sectional | Number of SA through 1 dichotomic question | ED, nightmare frequency, and their interaction were significantly related to previous SAs. This interaction was significant at moderate and high levels of ED, but not at low levels. Furthermore, the interaction of nightmare frequency and DERS subscales was significant for each dimension, except for difficulties engaging in goal-directed behavior at moderate and high levels. | 2 |
| Silvers et al., 2016 [62] | USA | 60 females with BPD | Cross-sectional | SI and SA through CSHF | No significant difference between DERS scores in those with and without SA. | 4 |
| Turton et al., 2022 [63] | UK | 65 adults with SI in the past year | Cross-sectional | SI and number of previous SA through BSS | There was a significant positive correlation between DERS total score and SI, while only 3 subscales of DERS (“Goal”, “Impulse”, and “Strategies”) were positively related to SI. The 2 models where ED was tested as a mediator between avoidant or anxious attachment and SI were insignificant. Finally, individuals with multiple SAs reported higher ED than those without a history of SA but there was no significant difference in ED between single and multiple attempters or between single and nonattempters. | 4.5 |
| Van Eck et al., 2015 [64] | USA | 627 undergraduate students | Cross-sectional | SI through 1 item of the BSI | Students who reported SI had significantly higher scores on ED constructs. Moreover, results of moderated mediation models with the single dimensions of DERS have shown that ED moderated the indirect effect of ADHD on SI. | 3 |
| Yang et al., 2021 [65] | China | 1596 undergraduate students | Cross-sectional | Passive and active SI through 2 items of BSS SA through 1 item of SITBI | Both suicide ideators and suicide attempters scored significantly higher on DERS than nonideators and suicide attempters scored significantly higher on ED than suicide ideators. Both suicide ideators and suicide attempters scored significantly higher on “Goal”, “Impulse”, and “Strategies”, suicide ideators scored significantly higher on “Clarity” than nonideators, while suicide attempters scored significantly higher on “Acceptance” and “Impulse” than suicide ideators. According to the results of the multinomial regression model, the dimensions of “Goal”, “Clarity”, and “Strategies” significantly discriminated suicide ideators from nonideators, “Impulse” significantly discriminated suicide attempters from nonideators, and “Awareness”, and “Clarity”, and “Impulse” significantly discriminated suicide attempters from suicide ideators. | 3 |
| Yang et al., 2022 [66] | China | 1491 male prisoners (316 with probable ASPD and 169 with probable BPD) | Cross-sectional | SI and SA through SITBI | For the sample with ASPD, all DERS dimensions showed positive and significant correlations with lifetime and last year SI and with the previous year’s suicide plans, while only “Impulse” and ”Strategies” showed a correlation with the previous year’s SAs. For the sample with BPD, all DERS dimensions showed positive and significant correlations with the previous year SI; “Goals”, ”Impulse”, and ”Strategies” were related to lifetime SI; “Nonacceptance”, “Strategies”, and “Impulse” were related to last year suicide plans; and none of the subscales of DERS showed a significant correlation with the previous year’s SAs. | 3.5 |
| Yoon et al., 2022 [67] | Korea | 150 Emergency room patients with SI (76) or SA (74) | Cross-sectional | SI and SA through anamnestic questions | There were no differences in ED between suicide ideators and suicide attempters. | 3 |
| Zeifman et al., 2020 [68] | Canada | 130 university students | Cross-sectional | SI through BSS | Both DERS total score and all the subscales were significantly and positively associated with SI. Furthermore, the DERS total score indirectly affected the positive relationship between perfectionistic concerns, strivings, and SI. Two dimensions of ED (“Strategies” and “Clarity”) were the only significant indirect effects of the relationship between perfectionistic concerns and SI, while “Strategies” was the only significant indirect effect of the relationship between perfectionistic strivings and SI. | 2 |
| Zemestani et al., 2023 [69] | Iran | 679 university students | Cross-sectional | SI through the first 5 items of BSS | DERS total score and all its dimension were positively and significantly associated with SI. The results of the mediation model revealed a significant direct effect of sleep disturbance on SI severity. Additionally, they supported the indirect relationship between sleep disturbance and SI severity mediated by ED. | 2 |
| Zobel et al., 2023 [70] | Italy | 1202 community participants | Cross-sectional | SI and SA through BSS | DERS total score and all its dimensions were positively and significantly associated with SI. The results indicated that levels of ED partially mediated the pathways by which SI leads to NSSI. | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogante, E.; Cifrodelli, M.; Sarubbi, S.; Costanza, A.; Erbuto, D.; Berardelli, I.; Pompili, M. The Role of Emotion Dysregulation in Understanding Suicide Risk: A Systematic Review of the Literature. Healthcare 2024, 12, 169. https://doi.org/10.3390/healthcare12020169
Rogante E, Cifrodelli M, Sarubbi S, Costanza A, Erbuto D, Berardelli I, Pompili M. The Role of Emotion Dysregulation in Understanding Suicide Risk: A Systematic Review of the Literature. Healthcare. 2024; 12(2):169. https://doi.org/10.3390/healthcare12020169
Chicago/Turabian StyleRogante, Elena, Mariarosaria Cifrodelli, Salvatore Sarubbi, Alessandra Costanza, Denise Erbuto, Isabella Berardelli, and Maurizio Pompili. 2024. "The Role of Emotion Dysregulation in Understanding Suicide Risk: A Systematic Review of the Literature" Healthcare 12, no. 2: 169. https://doi.org/10.3390/healthcare12020169
APA StyleRogante, E., Cifrodelli, M., Sarubbi, S., Costanza, A., Erbuto, D., Berardelli, I., & Pompili, M. (2024). The Role of Emotion Dysregulation in Understanding Suicide Risk: A Systematic Review of the Literature. Healthcare, 12(2), 169. https://doi.org/10.3390/healthcare12020169








