Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Data Sources
2.2. Selection of Studies and Eligibility Criteria
2.3. Data Extraction
2.4. Variables
2.5. Quality Assessment
3. Results
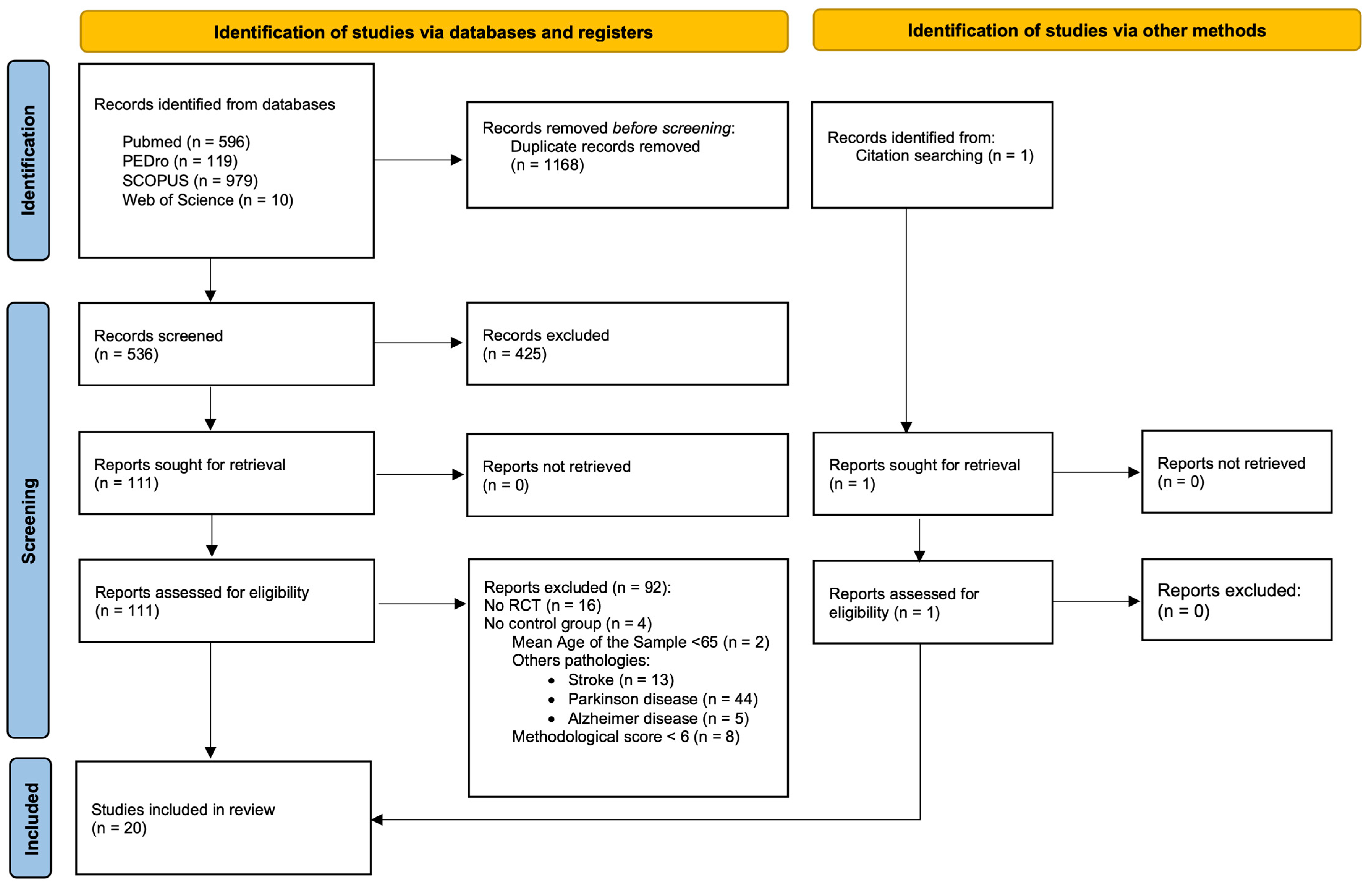
3.1. Study Slection
3.2. Methodological Quality Assessment
3.3. Characteristics of the Studies Included in the Review
3.4. Effect of the Intervention
3.4.1. Virtual Reality Therapy Compared to Usual Care or Minimal Intervention
3.4.2. Virtual Reality Therapy Compared to Balance Training
3.4.3. Virtual Reality Therapy Compared to Physical Exercise
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Harada, C.N.; Natelson Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Gerson, L.W.; Jarjoura, D.; McCord, G. Risk of imbalance in elderly people with impaired hearing or vision. Age Ageing 1989, 18, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; LeValley, A.; Hall, C.B.; Katz, M.J.; Ambrose, A.F.; Lipton, R.B. Epidemiology of gait disorders in community-residing older adults. J. Am. Geriatr. Soc. 2006, 54, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Hauer, K.; Lamb, S.E.; Jorstad, E.C.; Todd, C.; Becker, C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing 2006, 35, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [CrossRef] [PubMed]
- Prudham, D.; Evans, J.G. Factors associated with falls in the elderly: A community study. Age Ageing 1981, 10, 141–146. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P. Protocol for disseminating an evidence-based fall prevention program in community senior centers: Evaluation of translatability and public health impact via a single group pre-post study. Implement. Sci. 2014, 9, 63. [Google Scholar] [CrossRef]
- Goodwin, V.A.; Abbott, R.A.; Whear, R.; Bethel, A.; Ukoumunne, O.C.; Thompson-Coon, J.; Stein, K. Multiple component interventions for preventing falls and fall-related injuries among older people: Systematic review and meta-analysis. BMC Geriatr. 2014, 14, 15. [Google Scholar] [CrossRef]
- Vieira, E.R.; Palmer, R.C.; Chaves, P.H.M. Prevention of falls in older people living in the community. BMJ 2016, 353, i1419. [Google Scholar] [CrossRef]
- Shubert, T.E. Evidence-based exercise prescription for balance and falls prevention: A current review of the literature. J. Geriatr. Phys. Ther. 2011, 34, 100–108. [Google Scholar] [CrossRef]
- American College of Sports Medicine Physical activity programs and behavior counseling in older adult populations. Med. Sci. Sports Exerc. 2004, 36, 1997–2003. [CrossRef] [PubMed]
- Kobayashi, R.; Nakadaira, H.; Ishigami, K.; Muto, K.; Anesaki, S.; Yamamoto, M. Effects of physical exercise on fall risk factors in elderly at home in intervention trial. Environ. Health Prev. Med. 2006, 11, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Rydwik, E.; Frändin, K.; Akner, G. Effects of physical training on physical performance in institutionalised elderly patients (70+) with multiple diagnoses. Age Ageing 2004, 33, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Schlicht, J.; Camaione, D.N.; Owen, S.V. Effect of intense strength training on standing balance, walking speed, and sit-to-stand performance in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M281-6. [Google Scholar] [CrossRef] [PubMed]
- Shigematsu, R.; Chang, M.; Yabushita, N.; Sakai, T.; Nakagaichi, M.; Nho, H.; Tanaka, K. Dance-based aerobic exercise may improve indices of falling risk in older women. Age Ageing 2002, 31, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Lomas-Vega, R.; Obrero-Gaitán, E.; Molina-Ortega, F.J.; Del-Pino-Casado, R. Tai Chi for Risk of Falls. A Meta-analysis. J. Am. Geriatr. Soc. 2017, 65, 2037–2043. [Google Scholar] [CrossRef] [PubMed]
- Hiroyuki, S.; Uchiyama, Y.; Kakurai, S. Specific effects of balance and gait exercises on physical function among the frail elderly. Clin. Rehabil. 2003, 17, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, D.; Trakarnratanakul, N.; Smyth, B.; Caulfield, B. Effects of a wobble board-based therapeutic exergaming system for balance training on dynamic postural stability and intrinsic motivation levels. J. Orthop. Sports Phys. Ther. 2010, 40, 11–19. [Google Scholar] [CrossRef]
- Day, L.; Hill, K.D.; Stathakis, V.Z.; Flicker, L.; Segal, L.; Cicuttini, F.; Jolley, D. Impact of tai-chi on falls among preclinically disabled older people. A randomized controlled trial. J. Am. Med. Dir. Assoc. 2015, 16, 420–426. [Google Scholar] [CrossRef]
- Lee, H.-C.; Chang, K.-C.; Tsauo, J.-Y.; Hung, J.-W.; Huang, Y.-C.; Lin, S.-I. Effects of a multifactorial fall prevention program on fall incidence and physical function in community-dwelling older adults with risk of falls. Arch. Phys. Med. Rehabil. 2013, 94, 606–615.e1. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.J.; Robertson, M.C.; La Grow, S.J.; Kerse, N.M.; Sanderson, G.F.; Jacobs, R.J.; Sharp, D.M.; Hale, L.A. Randomised controlled trial of prevention of falls in people aged > or =75 with severe visual impairment: The VIP trial. BMJ 2005, 331, 817. [Google Scholar] [CrossRef] [PubMed]
- Van Diest, M.; Lamoth, C.J.; Stegenga, J.; Verkerke, G.J.; Postema, K. Exergaming for balance training of elderly: State of the art and future developments. J. Neuroeng. Rehabil. 2013, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Rizzo, A.A. The application of virtual reality technology in rehabilitation. Rehabil. Psychol. 2001, 46, 296–311. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Bredin, S.S.D.; Horita, L.T.L.; Zbogar, D.; Scott, J.M.; Esch, B.T.A.; Rhodes, R.E. The health benefits of interactive video game exercise. Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metab. 2007, 32, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Merians, A.S.; Jack, D.; Boian, R.; Tremaine, M.; Burdea, G.C.; Adamovich, S.V.; Recce, M.; Poizner, H. Virtual reality-augmented rehabilitation for patients following stroke. Phys. Ther. 2002, 82, 898–915. [Google Scholar] [CrossRef] [PubMed]
- Hung, J.-W.; Chou, C.-X.; Hsieh, Y.-W.; Wu, W.-C.; Yu, M.-Y.; Chen, P.-C.; Chang, H.-F.; Ding, S.-E. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch. Phys. Med. Rehabil. 2014, 95, 1629–1637. [Google Scholar] [CrossRef]
- Lange, B.S.; Requejo, P.; Flynn, S.M.; Rizzo, A.A.; Valero-Cuevas, F.J.; Baker, L.; Winstein, C. The potential of virtual reality and gaming to assist successful aging with disability. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 339–356. [Google Scholar] [CrossRef]
- Levac, D.E.; Sveistrup, H.; Weiss, P.L.; Keshner, E.A.; Levin, M.F. Virtual Reality for Physical and Motor Rehabilitation; Weiss, P.L., Keshner, E.A., Levin, M.F., Eds.; Springer: New York, NY, USA, 2014. [Google Scholar]
- Levin, M.F.; Demers, M. Motor learning in neurological rehabilitation. Disabil. Rehabil. 2021, 43, 3445–3453. [Google Scholar] [CrossRef]
- Holden, M.K. Virtual environments for motor rehabilitation: Review. Cyberpsychology Behav. 2005, 8, 187–189. [Google Scholar] [CrossRef]
- Bamidis, P.D.; Vivas, A.B.; Styliadis, C.; Frantzidis, C.; Klados, M.; Schlee, W.; Siountas, A.; Papageorgiou, S.G. A review of physical and cognitive interventions in aging. Neurosci. Biobehav. Rev. 2014, 44, 206–220. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0. [Update March 2011]; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Moseley, A.M.; Herbert, R.D.; Sherrington, C.; Maher, C.G. Evidence for physiotherapy practice: A survey of the Physiotherapy Evidence Database (PEDro). Aust. J. Physiother. 2002, 48, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Adcock, M.; Fankhauser, M.; Post, J.; Lutz, K.; Zizlsperger, L.; Luft, A.R.; Guimarães, V.; Schättin, A.; de Bruin, E.D. Effects of an In-home Multicomponent Exergame Training on Physical Functions, Cognition, and Brain Volume of Older Adults: A Randomized Controlled Trial. Front. Med. 2020, 6, 321. [Google Scholar] [CrossRef] [PubMed]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and Effects of an Immersive Virtual Reality Exergame Program on Physical Functions in Institutionalized Older Adults: A Randomized Clinical Trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef]
- Delbroek, T.; Vermeylen, W.; Spildooren, J. The effect of cognitive-motor dual task training with the biorescue force platform on cognition, balance and dual task performance in institutionalized older adults: A randomized controlled trial. J. Phys. Ther. Sci. 2017, 29, 1137–1143. [Google Scholar] [CrossRef]
- Karahan, A.Y.; Tok, F.; Taşkın, H.; Kuçuksaraç, S.; Başaran, A.; Yıldırım, P. Effects of Exergames on Balance, Functional Mobility, and Quality of Life of Geriatrics Versus Home Exercise Programme: Randomized Controlled Study. Cent. Eur. J. Public Health 2015, 23, S14–S18. [Google Scholar] [CrossRef]
- Lee, Y.; Choi, W.; Lee, K.; Song, C.; Lee, S. Virtual Reality Training With Three-Dimensional Video Games Improves Postural Balance and Lower Extremity Strength in Community-Dwelling Older Adults. J. Aging Phys. Act. 2017, 25, 621–627. [Google Scholar] [CrossRef]
- Park, J.; Yim, J. A New Approach to Improve Cognition, Muscle Strength, and Postural Balance in Community-Dwelling Elderly with a 3-D Virtual Reality Kayak Program. Tohoku J. Exp. Med. 2016, 238, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Kuroki, K.; Saiki, S.; Nagatomi, R. Improving Walking, Muscle Strength, and Balance in the Elderly with an Exergame Using Kinect: A Randomized Controlled Trial. Games Health J. 2015, 4, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-M.; Chen Hsieh, J.S.; Chen, Y.-C.; Yang, S.-Y.; Lin, H.-C.K. Effects of Kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine 2020, 99, e21228. [Google Scholar] [CrossRef] [PubMed]
- Yeşilyaprak; Sevgi, S.; Yıldırım, M.Ş.; Tomruk, M.; Ertekin, Ö.; Algun, Z.C. Comparison of the effects of virtual reality-based balance exercises and conventional exercises on balance and fall risk in older adults living in nursing homes in Turkey. Physiother. Theory Pract. 2016, 32, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of Exergaming Training in Reducing Risk and Incidence of Falls in Frail Older Adults with a History of Falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Virtual reality gait training to promote balance and gait among older people: A randomized clinical trial. Geriatrics 2021, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Bacha, J.M.; Gomes, G.C.V.; De Freitas, T.B.; Viveiro, L.A.P.; Da Silva, K.G.; Bueno, G.C.; Varise, E.M.; Torriani-Pasin, C.; Alonso, A.C.; Luna, N.M.S.; et al. Effects of kinect adventures games versus conventional physical therapy on postural control in elderly people: A randomized controlled trial. Games Health J. 2018, 7, 24–36. [Google Scholar] [CrossRef]
- Tsang, W.W.N.; Fu, A.S.N. Virtual reality exercise to improve balance control in older adults at risk of falling. Hong Kong Med. J. Xianggang Yi Xue Za Zhi 2016, 22 (Suppl. S2), S19–S22. [Google Scholar]
- Benitez-Lugo, M.L.; Suárez-Serrano, C.; Galvao-Carmona, A.; Vazquez-Marrufo, M.; Chamorro-Moriana, G. Effectiveness of feedback-based technology on physical and cognitive abilities in the elderly. Front. Aging Neurosci. 2022, 14, 1050518. [Google Scholar] [CrossRef]
- Gallardo-Meza, C.; Simon, K.; Bustamante-Ara, N.; Ramirez-Campillo, R.; García-Pinillos, F.; Keogh, J.W.L.; Izquierdo, M. Effects of 4 Weeks of Active Exergames Training on Muscular Fitness in Elderly Women. J. Strength Cond. Res. 2022, 36, 427–432. [Google Scholar] [CrossRef]
- Gomes, G.C.V.; do Socorro Simões, M.; Lin, S.M.; Bacha, J.M.R.; Viveiro, L.A.P.; Varise, E.M.; Junior, N.C.; Lange, B.; Jacob Filho, W.; Pompeu, J.E. Feasibility, safety, acceptability, and functional outcomes of playing Nintendo Wii Fit PlusTM for frail older adults: A randomized feasibility clinical trial. Maturitas 2018, 118, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Khushnood, K.; Sultan, N.; Altaf, S.; Qureshi, S.; Mehmood, R.; Awan, M.M.A. Effects of Wii Fit exer-gaming on balance and gait in elderly population: A randomized control trial. J. Pak. Med. Assoc. 2021, 71, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Cho, S.H. Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina 2022, 58, 1545. [Google Scholar] [CrossRef] [PubMed]
- Lima Rebêlo, F.; de Souza Silva, L.F.; Doná, F.; Sales Barreto, A.; de Souza Siqueira Quintans, J. Immersive virtual reality is effective in the rehabilitation of older adults with balance disorders: A randomized clinical trial. Exp. Gerontol. 2021, 149, 111308. [Google Scholar] [CrossRef] [PubMed]
- Szturm, T.; Betker, A.L.; Moussavi, Z.; Desai, A.; Goodman, V. Effects of an interactive computer game exercise regimen on balance impairment in frail community-dwelling older adults: A randomized controlled trial. Phys. Ther. 2011, 91, 1460–1462. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, S.I.; McAvay, G.; Ning, Y.; Allore, H.G.; Newman, A.B.; Gill, T.M. Geriatric impairments and disability: The cardiovascular health study. J. Am. Geriatr. Soc. 2010, 58, 1686–1692. [Google Scholar] [CrossRef] [PubMed]
- Tahmosybayat, R.; Baker, K.; Godfrey, A.; Caplan, N.; Barry, G. Movements of older adults during exergaming interventions that are associated with the Systems Framework for Postural Control: A systematic review. Maturitas 2018, 111, 90–99. [Google Scholar] [CrossRef]
- Galna, B.; Jackson, D.; Schofield, G.; McNaney, R.; Webster, M.; Barry, G.; Mhiripiri, D.; Balaam, M.; Olivier, P.; Rochester, L. Retraining function in people with Parkinson’s disease using the Microsoft kinect: Game design and pilot testing. J. Neuroeng. Rehabil. 2014, 11, 60. [Google Scholar] [CrossRef]
- Pompeu, J.E.; Mendes, F.A.D.S.; Silva, K.G.D.; Lobo, A.M.; Oliveira, T.D.P.; Zomignani, A.P.; Piemonte, M.E.P. Effect of Nintendo Wii™-Based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: A randomised clinical trial. Physiotherapy 2012, 98, 196–204. [Google Scholar] [CrossRef]
- Daniel, K. Wii-hab for pre-frail older adults. Rehabil. Nurs. 2012, 37, 195–201. [Google Scholar] [CrossRef]
- Teixeira, L.E.P.P.; Silva, K.N.G.; Imoto, A.M.; Teixeira, T.J.P.; Kayo, A.H.; Montenegro-Rodrigues, R.; Peccin, M.S.; Trevisani, V.F.M. Progressive load training for the quadriceps muscle associated with proprioception exercises for the prevention of falls in postmenopausal women with osteoporosis: A randomized controlled trial. Osteoporos. Int. 2010, 21, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Muehlbauer, T.; Gruber, M. A qualitative review of balance and strength performance in healthy older adults: Impact for testing and training. J. Aging Res. 2012, 2012, 708905. [Google Scholar] [CrossRef] [PubMed]
- Madureira, M.M.; Takayama, L.; Gallinaro, A.L.; Caparbo, V.F.; Costa, R.A.; Pereira, R.M.R. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: A randomized controlled trial. Osteoporos. Int. 2007, 18, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Kristjansson, E.; Treleaven, J. Sensorimotor function and dizziness in neck pain: Implications for assessment and management. J. Orthop. Sports Phys. Ther. 2009, 39, 364–377. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.; Kraemer, T. Clinical use of Nintendo Wii bowling simulation to decrease fall risk in an elderly resident of a nursing home: A case report. J. Geriatr. Phys. Ther. 2009, 32, 174–180. [Google Scholar] [CrossRef]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 2013, 8, 257–263. [Google Scholar] [CrossRef]
- Kim, J.; Son, J.; Ko, N.; Yoon, B. Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: A pilot study. Arch. Phys. Med. Rehabil. 2013, 94, 937–943. [Google Scholar] [CrossRef]
- Lai, C.-H.; Peng, C.-W.; Chen, Y.-L.; Huang, C.-P.; Hsiao, Y.-L.; Chen, S.-C. Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture 2013, 37, 511–515. [Google Scholar] [CrossRef]
- Duncan, P.W.; Weiner, D.K.; Chandler, J.; Studenski, S. Functional reach: A new clinical measure of balance. J. Gerontol. 1990, 45, M192-7. [Google Scholar] [CrossRef]
- Song, Q.; Zhang, X.; Mao, M.; Sun, W.; Zhang, C.; Chen, Y.; Li, L. Relationship of proprioception, cutaneous sensitivity, and muscle strength with the balance control among older adults. J. Sport Health Sci. 2021, 10, 585–593. [Google Scholar] [CrossRef]
- Tsang, W.W.N.; Hui-Chan, C.W.Y. Effects of exercise on joint sense and balance in elderly men: Tai Chi versus golf. Med. Sci. Sports Exerc. 2004, 36, 658–667. [Google Scholar] [CrossRef]
- Van Diest, M.; Stegenga, J.; Wörtche, H.J.; Postema, K.; Verkerke, G.J.; Lamoth, C.J.C. Suitability of Kinect for measuring whole body movement patterns during exergaming. J. Biomech. 2014, 47, 2925–2932. [Google Scholar] [CrossRef]
- Clark, R.A.; Pua, Y.-H.; Fortin, K.; Ritchie, C.; Webster, K.E.; Denehy, L.; Bryant, A.L. Validity of the Microsoft Kinect for assessment of postural control. Gait Posture 2012, 36, 372–377. [Google Scholar] [CrossRef]
| Database | Search Strategy |
|---|---|
| PubMed | (aged[mh] or aged[tiab] or aged, 80 and over[mh] or aged, 80 and over[tiab] or frail elderly[mh] or frail elderly[tiab] or old* adult*[tiab] or elderly[tiab] or ancient*[tiab]) AND (virtual reality[mh] OR virtual reality[tiab] OR virtual reality exposure therapy[mh] OR virtual reality exposure therapy[tiab] OR exergam*[tiab] or video games [mh] or video-gam*[tiab]) AND (postural balance[mh] or postural balance[tiab] or balance[mh] or balance[tiab] or balance*[tiab] or balance disorder*[tiab] or equilibrium[tiab]) |
| SCOPUS | [TITLE-ABS-KEY (“aged” OR “elderly” OR “older adult”) AND TITLE-ABS-KEY (“virtual reality” OR “video games” OR “exergames”) AND TITLE-ABS-KEY (“postural balance” OR “balance” OR “balance disorders”)] |
| Web of Science | TOPIC: (*aged* OR *elderly* OR *frail elderly* OR *older adult*) AND TOPIC: (*virtual reality* OR *exergame* OR *video games*) AND TOPIC: (*postural balance* OR *balance* OR *balance disorders*) |
| PEDro | aged AND virtual reality AND balance aged AND exergame AND balance aged AND video games AND balance older adults AND virtual reality AND balance older adults AND exergame AND balance older adults AND video game AND balance elderly AND virtual reality AND balance elderly AND exergame AND balance elderly AND video games AND balance |
| Study | I1 | I2 | I3 | I4 | I5 | I6 | I7 | I8 | I9 | I10 | I11 | Total | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adcock et al., 2021 [38] | Y | Y | Y | Y | N | N | N | Y | N | Y | Y | 6/10 | Good |
| Benítez-Lugo et al., 2022 [51] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 | Good |
| Campo-Prieto et al., 2022 [39] | Y | Y | Y | Y | N | N | N | Y | Y | Y | N | 6/10 | Good |
| Delbroek et al., 2017 [40] | Y | Y | Y | Y | N | N | Y | Y | Y | N | N | 6/10 | Good |
| Fu et al., 2015 [47] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | N | 7/10 | Good |
| Gallardo-Meza et al., 2022 [52] | Y | Y | Y | Y | N | Y | Y | Y | N | Y | Y | 8/10 | Good |
| Gomes et al., 2018 [53] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 | Good |
| Karahan et al., 2015 [41] | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | 6/10 | Good |
| Khusnood, K. et al., 2021 [54] | Y | Y | Y | N | Y | Y | Y | Y | N | Y | Y | 8/10 | Good |
| Kim, S.H. et al., 2022 [55] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 | Good |
| Lee, K. et al., 2021 [48] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | N | 7/10 | Good |
| Lee, Y. et al., 2017 [42] | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | 6/10 | Good |
| Lima-Revêlo et al., 2021 [56] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 | Good |
| Park et al., 2016 [43] | Y | Y | Y | Y | N | N | N | Y | Y | Y | N | 6/10 | Good |
| Ribeiro-Bacha et al., 2018 [49] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 | Good |
| Sato et al., 2015 [44] | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | 6/10 | Good |
| Szturm et al., 2011 [57] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 | Good |
| Tsang et al., 2020 [50] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7/10 | Good |
| Yang et al., 2020 [45] | Y | Y | N | Y | N | N | Y | Y | Y | Y | N | 6/10 | Good |
| Yeşilyaprak et al., 2016 [46] | Y | Y | Y | Y | N | N | N | Y | N | Y | Y | 6/10 | Good |
| Study | Participants | EG Sample Characteristics | CG Sample Characteristics |
|---|---|---|---|
| Adcock, M. et al., 2021 [38] Design: RCT | 31 Older adults (16F/15M) | 15 Subjects (77 ± 6.4 year; 10F/5M) | 16 patients (70.9 ± 5.0 year; 6F/10M) |
| Benítez-Lugo, M.L. et al., 2022 [51] Design: RCT | 46 Older adults (32F/14M) | 26 Subjects (72.19 ± 4.79 year; 20F/6M) | 20 Subjects (73.00 ± 7.4 year; 12F/8M) |
| Campo-Prieto, P. et al., 2022 [39] Design: RCT | 24 Older adults (21F/3M) | 13 Subjects (85.08 ± 8.48 year; 11F/2M) | 11 Subjects (84.82 ± 8.10 year; 10F/1M) |
| Delbroek, T. et al., 2017 [40] Design: RCT | 20 Older adults (13F/5M) | 10 Subjects (86.9 ± 5.6 year; 2F/8M) | 10 Subjects (87.5 ± 6.6 year; 5F/5M) |
| Fu, A.S. et al., 2015 [47] Design: RCT | 60 Older adults (39F/21M) | 30 Subjects (82.4 ± 3.8 year; 20F/10M) | 30 Subjects (82.3 ± 4.3 year; 19F/11M) |
| Gallardo-Meza, C. et al., 2022 [52] Design: RCT | 72 Older women | 35 Subjects (69.2 ± 3.3 year; 35F/0M) | 37 Subjects (68.1 ± 3.7year; 37F/0M) |
| Gomes, G.C.V. et al., 2018 [53] Design: RCT | 30 Older adults (Gender not reported) | 15 Subjects (83 ± 5.87 year; Gender not reported) | 15 Subjects (85 ± 6.19 year; Gender not reported) |
| Karahan, A.Y. et al., 2015 [41] Design: RCT | 90 Older adults (39F/21M) | 48 Subjects (71.3 ± 6.1 year; 21F/27M) | 42 Subjects (71.5 ± 4.7 year; 18F/24M) |
| Khusnood, K. et al., 2021 [54] Design: RCT | 83 Older adults (Gender not reported) | 42 Subjects (65 ± 3.0 year; Gender not reported) | 41 Subjects (66.5 ± 4.6 year; Gender not reported) |
| Kim, S.H. et al., 2022 [55] Design: RCT | 34 Older adults (39F/21M) | 12 Subjects (75.75 ± 10.15 year; 21F/27M) | 12 Subjects (80.75 ± 6.03 year; 21F/27M) |
| 10 Subjects (83.10 ± 5.24 year; 21F/27M) | |||
| Lee, K. et al., 2021 [48] Design: RCT | 56 Older adults (39F/21M) | 28 Subjects (81.01 ± 6.89 year; 12F/16M) | 28 Subjects (79.47 ± 6.15 year; 13F/15M) |
| Lee, Y. et al., 2017 [42] Design: RCT | 40 Older adults (Gender not reported) | 21 Subjects (76.15 ± 4.55 year; 12F/9M) | 19 Subjects (75.71 ± 4.91 year; 11F/8M) |
| Lima-Revêlo, F. et al., 2021 [56] Design: RCT | 37 Older adults (31F/6M) | 17 Subjects (69.25 ± 5.67 year; 16F/4M) | 20 Subjects (71.41 ± 5.94 year; 15F/2M) |
| Park, J. et al., 2016 [43] Design: RCT | 72 Older adults (68F/4M) | 36 Subjects (72.97 ± 2.98 year; 33F/3M) | 36 Subjects (74.11 ± 2.88 year; 35F/1M) |
| Ribeiro-Bacha, J.M. et al., 2018 [49] Design: RCT | 46 Older adults (34F/12M) | 23 Subjects (66.5 year; 19F/4M) | 23 Subjects (71.0 year; 15F/8M) |
| Sato, K. et al., 2015 [44] Design: RCT | 54 Older adults (43F/11M) | 28 Subjects (70.07 ± 5.35 year; 22F/6M) | 26 Subjects (68.50 ± 5.47 year; 21F/5M) |
| Szturm, T. et al., 2011 [57] Design: RCT | 27 Older adults (19F/8M) | 13 Subjects (80.5 ± 6 year; 10F/3M) | 14 Subjects (81 ± 7 year; 9F/5M) |
| Tsang, W.W.N. et al., 2020 [50] Design: RCT | 79 Older adults (48F/31M) | 39 Subjects (82.3 ± 3.8 year; 23F/16M) | 40 Subjects (82.0 ± 4.3 year; 25F/15M) |
| Yang, C.M. et al., 2020 [45] Design: RCT | 20 Older adults (18F/2M) | 10 Subjects (69.71 year; 9F/1M) | 10 Subjects (67.54 year; 9F/1M) |
| Yeşilyaprak, S.S. et al., 2016 [46] Design: RCT | 18 Older adults (5F/13M) | 7 Subjects (70.1 ± 4.0 year; 3F/4M) | 11 Subjects (73.1 ± 4.5 year; 2F/9M) |
| Study | EG Intervention | CG Intervention | Assessments | Variables | Tests | Outcomes |
|---|---|---|---|---|---|---|
| Adcock, M. et al., 2021 [38] | 48 sessions. Three 30–40 min sessions per week for 16 weeks. Strength, balance, and cognitive training through Active@ home exergames. | Normal daily activity | Patients were assessed preintervention and after intervention. | Balance | SPPB | At post treatment improvements in WMS-R forward span score (F = 8.504, p = 0.004, ηp2 = 0.04) and WMS-R backward span score (F = 5.872, p = 0.015, ηp2 = 0.02) and no significant improvements in balance (p > 0.05) or gait (p > 0.05) at post treatment were observed. |
| Gait | Physilog® 5. | |||||
| Lower body strength and aerobic endurance | SFT | |||||
| Cognitive Functions | VST | |||||
| WMS-R | ||||||
| TMT | ||||||
| Benítez-Lugo, M.L. et al., 2022 [51] | 16 sessions. Two 30 min sessions per week for 8 weeks. Wii Fit exercise program for Nintendo Wii, using the Wii Balance Board platform. | Usual care (memory workshops and joint mobility workshops in the center). | Patients were assessed pre intervention and after intervention | Balance | BBS | EG showed greater improvements in terms of balance, gait, and fall risk (BBS [p = 0.001]; TUG [p = 0.001]; Tinetti [p = 0.001]), attention, and cognitive status (Oddball [p = 0.003]; MMSE [p = 0.025]). [p = 0.001]) |
| Tinetti test | ||||||
| Gait | TUG | |||||
| Tinetti test | ||||||
| Risk of fall | Tinetti test | |||||
| Attention | ANT-ELDERLY | |||||
| Oddball Test | ||||||
| Cognitive Status | MMSE | |||||
| Campo-Prieto, P. et al., 2022 [39] | 30 sessions. Three 6 min sessions per week for 10 weeks. Exercise-based boxing in a virtual gym space while wearing immersive virtual reality goggles. | Usual care (memory workshops and occupational therapy). | Patients were assessed pre intervention, after intervention, and at 14 weeks. | Balance | Tinetti test | EG showed greater improvements in terms of balance, gait, and lower limb function, both at post treatment (Tinetti balance [p < 0.005]; Tinetti gait [p < 0.005]; Tinetti total [p < 0.005]; TUG [p < 0.005]; FTSTS [p < 0.005]) and at follow-up (Tinetti balance [p < 0.005]; Tinetti gait [p < 0.005]; Tinetti total [p < 0.005]. |
| Gait | Tinetti test | |||||
| Lower limb function | TUG | |||||
| FTSTS | ||||||
| Handgrip Strength | Dynamometer | |||||
| QoL | SF-12 | |||||
| Delbroek, T. et al., 2017 [40] | 12 sessions. Two 18–30 min sessions per week for 6 weeks. Training program with Bio Rescue. This is a virtual reality device for cognitive-motor training of dual tasks. | Usual care in the nursing home if applicable. | Patients were assessed pre intervention and after intervention | Balance | Tinetti test | EG showed greater improvements in three gait domains, including a reduction in total ambulation time (p = 0.02), sitting transition (p = 0.02), and gait time before turning (p = 0.02). |
| Gait | TUG | |||||
| Cognitive Functions | MoCA | |||||
| Gallardo-Meza, C. et al., 2022 [52] | Eight sessions. Two sessions per week for 4 weeks. Active exergames training program (Nintendo Wii, including the Wii Fit Plus, the Wii Balance board, and the Wii Nunchuk). | Habitual weekly physical activity levels. | Patients were assessed pre intervention and after intervention | Balance | One-leg stance test | EG showed greater improvements in strength, with a Δ75.5% increase (d = 0.89) in right leg static balance, a Δ33.7% increase (d = 0.57) in left leg static balance, a Δ14.8% increase (d = 0.85) in timed stand-and-walk test, and a Δ83.8% increase (d = 1.62) in five-repetition sit-to-stand test. |
| Gait | TUG | |||||
| Lower limb strength | FTSTS velocity test | |||||
| Gomes, G.C.V. et al., 2018 [53] | 14 sessions. Two 50 min sessions per week for 7 weeks. Exercise program with Nintendo Wii fit plus adapted to the needs, supervised by a physiotherapist. | World Health Organization guidelines described the benefits and risks of physical activity. | Patients were assessed pre intervention, after intervention, and at 1 month after treatment. | Balance | Mini-BEST test | EG showed greater improvements in static balance, measured by the Mini-BEST test (F = 6.060; p = 0.004; ES = 0.016), and gait, measured by the FGA (F = 3.794; p = 0.028; ES = 0.014), than the CG. |
| Gait | FGA | |||||
| Fear of Falling | FES-I | |||||
| Cognitive functions | MoCA | |||||
| Mood | GDS-15 | |||||
| Kim, S.H. et al., 2022 [55] | 18 sessions. Three 30 min sessions per week for 6 weeks. Wii Fit game program. | No intervention. | Patients were assessed pre intervention, after intervention, and at two weeks after treatment. | Balance | Personal measurement | EG showed greater improvements in OE balance sensation compared to the CG after treatment (p = 0.020; d = 1.08). |
| Body center movement area | Gaitview AFA-50 system | |||||
| 18 sessions. Three 20 min sessions per week for 6 weeks. Motor imagery training | Fear of falling | Tinetti test | ||||
| BBS | ||||||
| Lee, Y. et al., 2017 [42] | Virtual reality training with 3D video games. | Fall prevention education program. | Patients were assessed preintervention and after-intervention. | Static Balance | Stabilometric platform | EG showed greater improvements in medio-lateral sway (OE [p = 0.025], CE [p = 0.010]), anterior-posterior sway (OE [p = 0.018], CE [p = 0.017]), and travel speed (OE [p = 0.011], CE [p = 0.010]). In monopodal balance, significant improvements in antero-posterior sway (p = 0.017) and velocity of displacement (p = 0.010), for both OE (p = 0.008) and CE (p = 0.035), dynamic balance (BBS [p < 0.001], FRT [p < 0.001], and TUG [p < 0.001]) and lower limb strength (p < 0.001). |
| One-leg stance test | ||||||
| Dynamic Balance | BBS | |||||
| TUG | ||||||
| Functional reach test | ||||||
| Lower body strength | FTSTS | |||||
| Sato, K. et al., 2015 [44] | Therapy with Kinect and Kinect SDK version 1.5 and Unity version 3.4.2. | Normal daily activity. | Patients were assessed pre intervention and after intervention. | Balance | BBS | Within-group statistical analysis revealed improvements in EG for balance (p < 0.01), stability(p < 0.01), and lower limb strength (p < 0.01), while CG showed no differences between pre- and post-assessments. In addition, gait analysis showed a decrease in double stance time in EG (p = 0.04). |
| Gait | 3D motion analysis system Cortex 2 | |||||
| Stability | FRT | |||||
| Lower limb strength | 30-s Chair Stand Test |
| Study | EG Intervention | CG Intervention | Assessments | Variable | Test | Outcomes |
|---|---|---|---|---|---|---|
| Fu, A.S. et al., 2015 [47] | 18 sessions. Three 60-min sessions per week for 6 weeks. Balance training using a Nintendo’s Wii Fit balance board. | 18 sessions. Three 60-min sessions per week for 6 weeks. Conventional balance training. | Patients were assessed pre intervention and after intervention. | Falls | Fall incidence | EG showed greater improvements compared to CG in terms of muscle strength (p < 0.001), faster reaction times (p < 0.001), and less body sway (p = 0.013). |
| Risk of fall | PPA | |||||
| Postural Sway | Sway meter recording displacements of the body | |||||
| Quadriceps Strength | Kilograms | |||||
| Khusnood, K. et al., 2021 [54] | 16 sessions. Two 30-min sessions per week for 8 weeks. Exergaming with the Wii fit. | 16 sessions. Twice a week for 8 weeks. Balance exercise. | Patients were assessed pre intervention, after intervention, and at 8 weeks after treatment. | Balance | BBS | EG showed greater improvements compared to CG in terms of gait (variability [p < 0.001], alertness [p < 0.001], sway [p < 0.001], hip range of motion [p < 0.001], and leg-shoulder synchrony [p < 0.001]). |
| Gait | GARS-M | |||||
| Lima-Revêlo, F. et al., 2021 [56] | 16 sessions. Two 60-min sessions per week for 6 weeks. Immersive Virtual Reality program through Oculus rift device (Menlo Park, CA, USA). | 16 sessions. Two 60-min sessions per week for 6 weeks. Balance exercise. | Patients were assessed pre intervention, after intervention, and at 1 month after treatment. | Static Balance | CTSIB | Only the experimental group exhibited increased mobility (TUG) and decreased dizziness (DHI). |
| Gait | TUG | |||||
| DGI | ||||||
| Stability | FRT | |||||
| Fear of Falling | FES-I | |||||
| Dizziness | DHI | |||||
| Szturm, T. et al., 2011 [57] | 16 sessions. Two 30-min sessions per week for 8 weeks. Dynamic balance exercise coupled with computer games. | 16 sessions. Two 30-min sessions per week for 8 weeks. Conventional balance training. | Patients were assessed pre intervention and after intervention. | Static Balance | BBS | EG showed greater improvements compared to CG in change scores for the BBS (p = 0.001), LOB counts (p = 0.007), and ABC (p = 0.020) compared to the control group. |
| Dynamic Balance | CTSIB | |||||
| Gait | TUG | |||||
| GaitRite Instrumented carpet System | ||||||
| Fear of Falling | ABC | |||||
| Tsang, W.W.N. et al., 2020 [50] | 18 sessions. Three 60-min sessions per week for 6 weeks. Wii Fit balance training. | 18 sessions. Three 60-min sessions per week for 6 weeks. Conventional balance training. | Patients were assessed pre intervention and after intervention. | Static Balance | BBS | EG showed greater improvements compared to CG in balance (p < 0.001), end point of excursion (anterior [p < 0.001], posterior [p = 0.001], left [p = 0.048], and right [p = 0.007]) and maximum excursion (anterior [p < 0.001], posterior [p < 0.001], left [p = 0.011], and right [p = 0.001]). |
| Dynamic Balance | TUG | |||||
| Stability limits | Limits of stability test | |||||
| Yeşilyaprak, S.S. et al., 2016 [46] | 18 sessions. Three 60-min sessions per week for 6 weeks. Balance training with the NIRVANA Interactive Virtual Reality System. | 18 sessions. Three 60-min sessions per week for 6 weeks. Conventional balance training. | Patients were assessed pre intervention and after intervention. | Static Balance | BBS | The within-group analysis showed improvements in both groups in both static (EG BBS p < 0.01; CG BBS p < 0.01) and dynamic balance (EG TUG p = 0.01; CG TUG p = 0.04). |
| One-leg stance test | ||||||
| Tandem stance test | ||||||
| Dynamic Balance | TUG | |||||
| Fear of Falling | FES-I |
| Study | EG Intervention | CG Intervention | Assessments | Variables | Tests | Outcomes |
|---|---|---|---|---|---|---|
| Karahan, A.Y. et al., 2015 [41] | 30 sessions. Five 30-min sessions per week for 6 weeks. Game set comprising the Xbox 360 Kinect game (Kinect Adventures, Kinect Sports, and Kinect Sports Season two). | 30 sessions. Five 30-min sessions per week for 6 weeks. Balance training. | Patients were assessed before and after the intervention. | Balance | BBS | EG showed greater improvements compared to CG in BBS (p < 0.001). In addition, within-group analysis showed EG group improvements in TUG and SF-36 (all p < 0.05) |
| Gait | TUG | |||||
| QoL | SF-36 | |||||
| Lee, K. et al., 2021 [48] | 20 sessions. Five 50-min sessions per week for 4 weeks. Virtual reality gait training. | 20 sessions. Five 50-min sessions per week for 4 weeks. Standard treadmill training without virtual reality. | Patients were assessed before and after the intervention. | Balance | One-leg stance test | EG showed greater improvements compared to CG in single-leg balance (t = 6.240, p < 0.001) and dynamic balance (t = 3.339, p = 0.002), static stride (t = 2.136, p = 0.037), step length (t = 2.136, p = 0.037), and step width (t = 2.364, p = 0.022). |
| BBS | ||||||
| Gait | TUG | |||||
| OptoGait | ||||||
| Stability | FRT | |||||
| Park, J. et al., 2016 [43] | 12 sessions. Two 50-min sessions per week for 6 weeks. 30 min of conventional exercise and 20 min of virtual training in Kayak (using a 3-D projector and 3-D images). | 12 sessions. Two 30-min sessions per week for 6 weeks. Conventional exercise. | Patients were assessed before and after the intervention. | Balance | Stabilometric platform | EG showed greater improvements compared to CG in all balance parameters, including OE (t = 4.367; p = 0.000) and CE (t = 4. 367; p = 0.000), upper limb strength (ACT; t = 6.896; p = 0.000), grip strength for the right hand (t = 4.367; p = 0.000) and left hand (t = 5.836; p = 0.000), and cognitive function (t = 5.475; p = 0.000). |
| Upper limb muscle strength | Dynamometer | |||||
| ACT | ||||||
| Cognitive Functions | MoCA | |||||
| Ribeiro-Bacha, J.M. et al., 2018 [49] | 14 sessions. Two 60-min sessions per week for 7 weeks. Therapy with Xbox Kinect Adventures games. | 14 sessions. Two 60-min sessions per week for 7 weeks. Training program in small groups supervised by a physiotherapist. | Patients were assessed before and after the intervention. In addition, a follow-up assessment was performed at 4 weeks after treatment. | Balance | Mini-BESTest | Significant intragroup improvements in gait were found at the end of treatment in both the EG and CG (EG [p < 0.05] and CG [p < 0.005]), and these improvements were maintained over time. |
| Gait | FGA | |||||
| Cognitive Functions | MoCA | |||||
| Yang, C.M. et al., 2020 [45] | 10 sessions. Two 45-min sessions per week for 5 weeks. Exercise with the Microsoft Kinect for Xbox 360 device (Microsoft, Washington, DC, USA), using “Your Shape: Fitness Evolved II” game software. | 10 sessions. Two 45-min sessions per week for 5 weeks. Physical exercise program specifically designed to prevent falls in elderly women. | Patients were assessed before and after the intervention. | Balance | TUG | EG showed greater improvements compared to CG in dynamic balance (z = −2.307; p = 0.021). Both groups showed intragroup differences in the 30-s CST the FRT and OLS with OE. In addition, EG showed improvements one-leg standing test with CE (z = −2.803; p = 0.005) and the timed up and go test (z = −2.803; p = 0.005). |
| FRT | ||||||
| One-leg stance test | ||||||
| Lower limb strength | 30-s Chair Stand Test |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Almagro, D.; Achalandabaso-Ochoa, A.; Ibáñez-Vera, A.J.; Góngora-Rodríguez, J.; Rodríguez-Huguet, M. Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review. Healthcare 2024, 12, 158. https://doi.org/10.3390/healthcare12020158
Rodríguez-Almagro D, Achalandabaso-Ochoa A, Ibáñez-Vera AJ, Góngora-Rodríguez J, Rodríguez-Huguet M. Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review. Healthcare. 2024; 12(2):158. https://doi.org/10.3390/healthcare12020158
Chicago/Turabian StyleRodríguez-Almagro, Daniel, Alexander Achalandabaso-Ochoa, Alfonso Javier Ibáñez-Vera, Jorge Góngora-Rodríguez, and Manuel Rodríguez-Huguet. 2024. "Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review" Healthcare 12, no. 2: 158. https://doi.org/10.3390/healthcare12020158
APA StyleRodríguez-Almagro, D., Achalandabaso-Ochoa, A., Ibáñez-Vera, A. J., Góngora-Rodríguez, J., & Rodríguez-Huguet, M. (2024). Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review. Healthcare, 12(2), 158. https://doi.org/10.3390/healthcare12020158








