Tackling Shift Work: Cardiovascular Health in the Auto Industry
Abstract
1. Introduction
1.1. Purpose and Significance
1.2. Current State of Research
2. Materials and Methods
2.1. Study Setting and Enterprise Selection
2.2. Data Collection
2.3. Study Population and Design
2.4. Shift Work Definitions and Schedules
2.5. Definition of Seniority in Work
2.6. Statistical Analysis
3. Results
3.1. Demographic Distribution and Occupational Characteristics
3.2. Age Distribution and Shift Work Patterns
3.3. Cardiovascular Disease (CVD) Prevalence
3.4. Cardiovascular Risk Factors
- Overall CVD Incidence
- 2.
- Gender and CVD
- 3.
- Age and CVD
- 4.
- Seniority in Work and CVD
- 5.
- Type of Work and CVD
- 6.
- Working Program and CVD
- Gender and Shift Work
- 2.
- Age and Shift Work
- 3.
- Seniority in Work and Shift Work
- 4.
- Type of Work and Shift Work
- Overall Night Shift and CVD Incidence
- 2.
- Gender-Specific Night Shift and CVD Incidence
4. Discussion
4.1. Gender Distribution and Occupational Roles
4.2. Age Distribution and Shift Work Patterns
4.3. Shift Work and Cardiovascular Health
4.4. Cardiovascular Disease Prevalence and Risk Factors
4.5. Occupational Role and CVD Incidence
4.6. Seniority in Work and CVD
4.7. Potential Long-Term Implications:
4.8. Addressing Cardiovascular Health
Potential Mechanisms:
4.9. Importance of Cardiovascular Health in the Context of Shift Work
4.10. Strategic Interventions
- Promoting Healthy Lifestyle Behaviors:
- -
- Encourage shift workers to engage in regular physical activity, even if it means adjusting workout schedules to fit their shift patterns. Providing access to on-site fitness facilities or partnerships with local gyms can facilitate this.
- -
- Educate employees about the importance of maintaining a balanced diet despite working non-standard shifts. Offering healthy food options during overnight shifts and providing nutritional resources can help support healthy eating habits [36].
- -
- Promote strategies for stress management and relaxation techniques, such as mindfulness training, yoga classes, or access to counseling services to help employees cope with the stress associated with their work schedules [45].
- Sleep Hygiene and Management:
- -
- Provide education on good sleep hygiene practices for shift workers, including creating a conducive sleep environment, maintaining consistent sleep schedules, and minimizing disruptions during sleep hours [46].
- -
- Consider implementing policies that allow for adequate time for sleep between shift rotations and provide guidance on how to optimize sleep quality and duration [46].
- Flexible Scheduling and Shift Design:
- -
- Explore opportunities for flexible scheduling, such as compressed workweeks or allowing employees to have a say in their shift preferences where possible. This can help reduce the frequency of rotating shifts, which can be particularly disruptive to circadian rhythms.
- -
- Consider aligning shift rotations in a forward-rotating manner (morning, evening, night shifts) to allow the body’s internal clock to adjust more effectively, rather than rotating shifts in a reverse order [47].
- Cardiovascular Risk Assessments and Monitoring:
- -
- Offer regular cardiovascular risk assessments, including screenings for blood pressure, cholesterol levels, and weight management programs, to help identify and manage potential risk factors early on [48].
- -
- Provide access to occupational health services that specifically address the unique needs and risk factors faced by shift workers, including cardiovascular risk factors [49].
- Employee Assistance Programs and Resources:
- -
- Establish access to employee assistance programs that offer support for mental health, stress management, and coping with the challenges associated with shift work [50].
- -
- Provide access to resources such as financial planning assistance, legal services, and support for family-related issues to help alleviate potential stressors that can impact cardiovascular health.
- Worksite Health Promotion Initiatives:
- -
- Implement worksite health promotion initiatives that focus on cardiovascular health, such as organizing health fairs, offering smoking cessation programs, and providing access to flu shots and other preventive healthcare services.
- -
- Foster a workplace culture that values and prioritizes employee well-being, providing opportunities for physical activity, healthy eating options, and wellness challenges to engage shift workers in positive health behaviors.
- Education and Training:
- -
- Offer educational programs on cardiovascular health, addressing topics such as the impact of shift work on cardiovascular function, the importance of stress management, and strategies for maintaining a healthy lifestyle despite non-traditional work schedules [44].
- -
- Provide training for managers and supervisors on recognizing signs of fatigue, stress, and potential health issues in shift workers, while also promoting supportive and flexible leadership practices.
- Access to Healthcare and Preventive Services:
- -
- Ensure that shift workers have access to healthcare services outside of standard business hours. This might include accommodating alternate appointment times with healthcare providers or offering telemedicine options for remote consultations.
- -
- Provide information about the availability of community health resources, such as local clinics and support groups, to supplement access to healthcare services.
- Supportive Organizational Policies:
- -
- Establish policies that promote a healthy work–life balance, including measures to limit excessive overtime, provide adequate rest periods between shifts, and consider shift preferences when feasible.
- -
- Recognize the unique challenges faced by shift workers and create a supportive work environment that fosters open communication, active listening, and responsive action to address employee concerns related to their work schedules.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Travill, A.L.; Soeker, F.; Overmeyer, D.; Rickers, F. Cardiovascular and metabolic risk factors of shift workers within the automotive industry. Health SA 2019, 24, 1227. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.J.; Cheng, Y. Night shift and rotating shift in association with sleep problems, burnout and minor mental disorder in male and female employees. Occup. Environ. Med. 2017, 74, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Peterson, S.A.; Wolkow, A.P.; Lockley, S.W.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Czeisler, C.A.; Rajaratnam, S.M.W.; Barger, L.K. Associations between shift work characteristics, shift work schedules, sleep and burnout in North American police officers: A cross-sectional study. BMJ Open 2019, 9, e030302. [Google Scholar] [CrossRef]
- Gu, H.; Lee, J.; Hwang, Y.; Kim, J.; Lee, S.; Kim, S.J. Job burnout among workers with different shift regularity: Interactive factors between sleep, depression, and work environment. Front. Public Health 2023, 11, 1131048. [Google Scholar] [CrossRef]
- Hemmer, A.; Mareschal, J.; Dibner, C.; Pralong, J.A.; Dorribo, V.; Perrig, S.; Genton, L.; Pichard, C.; Collet, T.-H. The Effects of Shift Work on Cardio-Metabolic Diseases and Eating Patterns. Nutrients 2021, 13, 4178. [Google Scholar] [CrossRef]
- Lopez-Santamarina, A.; Mondragon, A.d.C.; Cardelle-Cobas, A.; Santos, E.M.; Porto-Arias, J.J.; Cepeda, A.; Miranda, J.M. Effects of Unconventional Work and Shift Work on the Human Gut Microbiota and the Potential of Probiotics to Restore Dysbiosis. Nutrients 2023, 15, 3070. [Google Scholar] [CrossRef]
- Xue, J.; Wang, H.; Chen, M.; Ding, X.; Zhu, M. Signifying the Relationship Between Psychological Factors and Turnover Intension: The Mediating Role of Work-Related Stress and Moderating Role of Job Satisfaction. Front. Psychol. 2022, 13, 847948. [Google Scholar] [CrossRef] [PubMed]
- Boini, S.; Bourgkard, E.; Ferrières, J.; Esquirol, Y. What do we know about the effect of night-shift work on cardiovascular risk factors? An umbrella review. Front. Public Health 2022, 10, 1034195. [Google Scholar] [CrossRef]
- Bøggild, H.; Knutsson, A. Shift work, risk factors and cardiovascular disease. Scand. J. Work Environ. Health 1999, 25, 85–99. [Google Scholar] [CrossRef]
- Ohlander, J.; Keskin, M.C.; Stork, J.; Radon, K. Shift work and hypertension: Prevalence and analysis of disease pathways in a German car manufacturing company. Am. J. Ind. Med. 2015, 58, 549–560. [Google Scholar] [CrossRef]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef]
- Pereira, H.; Fehér, G.; Tibold, A.; Monteiro, S.; Costa, V.; Esgalhado, G. The Impact of Shift Work on Occupational Health Indicators among Professionally Active Adults: A Comparative Study. Int. J. Environ. Res. Public Health 2021, 18, 11290. [Google Scholar] [CrossRef] [PubMed]
- Nena, E.; Katsaouni, M.; Steiropoulos, P.; Theodorou, E.; Constantinidis, T.C.; Tripsianis, G. Effect of Shift Work on Sleep, Health, and Quality of Life of Health-care Workers. Indian J. Occup. Environ. Med. 2018, 22, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Kalkanis, A.; Demolder, S.; Papadopoulos, D.; Testelmans, D.; Buyse, B. Recovery from shift work. Front. Neurol. 2023, 14, 1270043. [Google Scholar] [CrossRef] [PubMed]
- Barth, J.; Greene, J.A.; Goldstein, J.; Sibley, A. Adverse Health Effects Related to Shift Work Patterns and Work Schedule Tolerance in Emergency Medical Services Personnel: A Scoping Review. Cureus 2022, 14, e23730. [Google Scholar] [CrossRef] [PubMed]
- Sagetha, J.; Preeti, P.; Rex Vijay, V. Assessment of Sleep Quality Among Shift Workers in the Automobile Industry in Kanchipuram, Tamil Nadu. J. Chem. Health Risks 2024, 14, 3394–3403, ISSN:2251-6727. Available online: https://jchr.org/index.php/JCHR/article/view/4193 (accessed on 18 May 2024).
- Kawada, T.; Shimizu, T.; Kuratomi, Y.; Suto, S.; Kanai, T.; Nishime, A.; Nakano, N. Monitoring of the sleep patterns of shift workers in the automotive industry. Work 2011, 38, 163–167. [Google Scholar] [CrossRef]
- Smith, P.M.; Saunders, R.; Lifshen, M.; Black, O.; Lay, M.; Breslin, F.C.; LaMontagne, A.D.; Tompa, E. The development of a conceptual model and self-reported measure of occupational health and safety vulnerability. Accid. Anal. Prev. 2015, 82, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Huxley, R.R.; Ansary-Moghaddam, A.; Clifton, P.; Czernichow, S.; Parr, C.L.; Woodward, M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: A quantitative overview of the epidemiological evidence. Int. J. Cancer 2009, 125, 171–180. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322, Erratum in Circulation 2015, 131, e535; Erratum in Circulation 2016, 133, e417. [Google Scholar] [CrossRef] [PubMed]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA 2016, 315, 1726–1734. [Google Scholar] [CrossRef]
- Knutsson, A. Health disorders of shift workers. Occup. Med. 2003, 53, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528, Erratum in Circulation 2020, 141, e33. [Google Scholar] [CrossRef]
- Holtermann, A.; Hansen, J.V.; Burr, H.; Søgaard, K.; Sjøgaard, G. The health paradox of occupational and leisure-time physical activity. Br. J. Sports Med. 2012, 46, 291–295. [Google Scholar] [CrossRef]
- Thorp, A.A.; Owen, N.; Neuhaus, M.; Dunstan, D.W. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am. J. Prev. Med. 2011, 41, 207–215. [Google Scholar] [CrossRef]
- Kivimäki, M.; Nyberg, S.T.; Batty, G.D.; Fransson, E.I.; Heikkilä, K.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. Lancet 2012, 380, 1491–1497. [Google Scholar] [CrossRef]
- Skogstad, M.; Goffeng, E.; Skare, Ø.; Zardin, E. The Prolonged Effect of Shift Work and the Impact of Reducing the Number of Nightshifts on Arterial Stiffness-A 4-Year Follow-Up Study. J. Cardiovasc. Dev. Dis. 2023, 10, 70. [Google Scholar] [CrossRef]
- Wong, R.; Crane, A.; Sheth, J.; Mayrovitz, H.N. Shift Work as a Cardiovascular Disease Risk Factor: A Narrative Review. Cureus 2023, 15, e41186. [Google Scholar] [CrossRef]
- Yang, L.; Luo, Y.; He, L.; Yin, J.; Li, T.; Liu, S.; Li, D.; Cheng, X.; Bai, Y. Shift Work and the Risk of Cardiometabolic Multimorbidity Among Patients With Hypertension: A Prospective Cohort Study of UK Biobank. J. Am. Heart Assoc. 2022, 11, e025936. [Google Scholar] [CrossRef]
- Ljevak, I.; Vasilj, I.; Ćurlin, M.; Šaravanja, N.; Meštrović, T.; Šimić, J.; Neuberg, M. The Impact of Shift Work on Psychosocial Functioning and Quality of Life Among Hospital-Employed Nurses: A Cross-Sectional Comparative Study. Psychiatr. Danub. 2020, 32 (Suppl. S2), 262–268. [Google Scholar] [PubMed]
- Boivin, D.B.; Boudreau, P.; Kosmadopoulos, A. Disturbance of the Circadian System in Shift Work and Its Health Impact. J. Biol. Rhythms. 2022, 37, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Hoshide, S.; Kario, K. Sleep duration as a risk factor for cardiovascular disease—A review of the recent literature. Curr. Cardiol. Rev. 2010, 6, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Zuraikat, F.M.; Makarem, N.; Redline, S.; Aggarwal, B.; Jelic, S.; St-Onge, M.P. Sleep Regularity and Cardiometabolic Heath: Is Variability in Sleep Patterns a Risk Factor for Excess Adiposity and Glycemic Dysregulation? Curr. Diab. Rep. 2020, 20, 38. [Google Scholar] [CrossRef] [PubMed]
- Mentzelou, M.; Papadopoulou, S.K.; Papandreou, D.; Spanoudaki, M.; Dakanalis, A.; Vasios, G.K.; Voulgaridou, G.; Pavlidou, E.; Mantzorou, M.; Giaginis, C. Evaluating the Relationship between Circadian Rhythms and Sleep, Metabolic and Cardiovascular Disorders: Current Clinical Evidence in Human Studies. Metabolites 2023, 13, 370. [Google Scholar] [CrossRef] [PubMed]
- Bucher Della Torre, S.; Wild, P.; Dorribo, V.; Danuser, B.; Amati, F. Energy, Nutrient and Food Intakes of Male Shift Workers Vary According to the Schedule Type but Not the Number of Nights Worked. Nutrients 2020, 12, 919. [Google Scholar] [CrossRef] [PubMed]
- Sara, J.D.; Prasad, M.; Eleid, M.F.; Zhang, M.; Widmer, R.J.; Lerman, A. Association Between Work-Related Stress and Coronary Heart Disease: A Review of Prospective Studies Through the Job Strain, Effort-Reward Balance, and Organizational Justice Models. J. Am. Heart Assoc. 2018, 7, e008073. [Google Scholar] [CrossRef]
- Vancheri, F.; Longo, G.; Vancheri, E.; Henein, M.Y. Mental Stress and Cardiovascular Health-Part I. J. Clin. Med. 2022, 11, 3353. [Google Scholar] [CrossRef] [PubMed]
- AbdulRaheem, Y. Unveiling the Significance and Challenges of Integrating Prevention Levels in Healthcare Practice. J. Prim. Care Community Health 2023, 14, 21501319231186500. [Google Scholar] [CrossRef] [PubMed]
- Bays, H.E.; Taub, P.R.; Epstein, E.; Michos, E.D.; Ferraro, R.A.; Bailey, A.L.; Kelli, H.M.; Ferdinand, K.C.; Echols, M.R.; Weintraub, H.; et al. Ten things to know about ten cardiovascular disease risk factors. Am. J. Prev. Cardiol. 2021, 5, 100149. [Google Scholar] [CrossRef]
- Lunde, L.K.; Skare, Ø.; Mamen, A.; Sirnes, P.A.; Aass, H.C.D.; Øvstebø, R.; Goffeng, E.; Matre, D.; Nielsen, P.; Heglum, H.S.A.; et al. Cardiovascular Health Effects of Shift Work with Long Working Hours and Night Shifts: Study Protocol for a Three-Year Prospective Follow-Up Study on Industrial Workers. Int. J. Environ. Res. Public Health 2020, 17, 589. [Google Scholar] [CrossRef] [PubMed]
- Rippe, J.M. Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease. Am. J. Lifestyle Med. 2018, 13, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Costa, G. The impact of shift and night work on health. Appl. Ergon. 1996, 27, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Ghodeshwar, G.K.; Dube, A.; Khobragade, D. Impact of Lifestyle Modifications on Cardiovascular Health: A Narrative Review. Cureus 2023, 15, e42616. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.; Pignata, S.; Bezak, E.; Tie, M.; Childs, J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: A systematic review. BMJ Open 2023, 13, e071203. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.sleephealthfoundation.org.au/sleep-topics/healthy-sleep-practices-for-shift-workers (accessed on 18 May 2024).
- Shon, Y.; Ryu, S.; Suh, B.S.; Kim, S.G.; Kim, W.S.; Son, H.S.; Kim, H.Y.; Jeong, H.S. Comparison of sleep quality based on direction of shift rotation in electronics workers. Ann. Occup. Environ. Med. 2016, 28, 37. [Google Scholar] [CrossRef] [PubMed]
- WHO CVD-Risk Management Package for Low- and Medium-Resource Settings. Available online: https://iris.who.int/bitstream/handle/10665/42621/9241545852.pdf (accessed on 18 May 2024).
- Thomas, C.; Power, C. Shift work and risk factors for cardiovascular disease: A study at age 45 years in the 1958 British birth cohort. Eur. J. Epidemiol. 2010, 25, 305–314. [Google Scholar] [CrossRef]
- Heo, S.; Cho, Y.; Jeon, M.J. Association between working evening shifts and mental health among Korean employees: Data from the 5th Korean Working Conditions Survey. Ann. Occup. Environ. Med. 2022, 34, e36. [Google Scholar] [CrossRef]
| Parameters | N | % | Parameters | N | % |
|---|---|---|---|---|---|
| Gender | Type of work | ||||
| Male | 3713 | 79.3 | Physical | 4128 | 88.1 |
| Female | 970 | 20.7 | Sedentary | 555 | 11.9 |
| Age | Working program | ||||
| Average (years ± SD) | 37.78 ± 9.17 | Night shift | 3802 | 81.2 | |
| Age < 50 years | 4173 | 89.1 | Day shift | 881 | 18.8 |
| Age 50–65 years | 510 | 10.9 | |||
| Group age | Cardiovascular disease (CVD) | ||||
| 18–19 | 58 | 1.2 | All CVDs | 187 | 4 |
| 20–29 | 882 | 18.8 | Hypertension | 181 | 3.9 |
| 30–39 | 1748 | 37.3 | Rhythm disorders | 24 | 0.5 |
| 40–49 | 1485 | 31.7 | Atrial fibrillation | 11 | 0.2 |
| 50–59 | 495 | 10.6 | Heart failure | 25 | 0.5 |
| 60–65 | 15 | 0.3 | Myocardial infarction | 9 | 0.2 |
| Seniority in work | Risk Factors | ||||
| Average (years ± SD) | 7.82 ± 5.69 | Diabetes | 177 | 3.8 | |
| <0–10 years | 2964 | 63.3 | Dyslipidemia | 10 | 0.02 |
| >10 years | 1718 | 36.7 | Obesity | 217 | 4.6 |
| Parametrs | CVD | No CVD | Total | Risk | ||
|---|---|---|---|---|---|---|
| N (%) | N (%) | N | OR /Differences | IC95% | p | |
| All | 187 (4.0) | 4496 (96.0) | 4683 | |||
| Gender | ||||||
| Male * | 159 (2.9) | 3554 (97.1) | 3713 | 1.51 | 1.01–2.26 | 0.048 |
| Female | 28 (4.3) | 942 (95.7) | 970 | |||
| Age | ||||||
| Average age | 48.18 ± 6.96 | 37.35 ± 8.99 | −10.84 y | −12.27–9.41 | <0.001 | |
| <50 years | 104 (2.5) | 4069 (97.5) | 4173 | 7.61 | 5.65–10.42 | <0.001 |
| 50–65 * years | 83 (16.3) | 427 (83.7) | 510 | |||
| Seniority in work | ||||||
| Years | 11.37 ± 5.07 | 7.67 ± 5.67 | −3.7 y | −4.52–(−2.87) | <0.001 | |
| 0–10 years | 67 (2.3) | 2897 (97.7) | 2964 | 3.25 | 2.39–4.41 | <0.001 |
| >10 years * | 120 (7.0) | 1598 (93.0) | 1718 | |||
| Type of work | ||||||
| Physically * | 177 (4.3) | 3951 (95.7) | 4128 | 2.44 | 1.28–4.65 | 0.007 |
| Sedentary | 10 (1.8) | 545 (98.2) | 555 | |||
| Working program | ||||||
| Night shif t * | 164 (4.3) | 3638 (95.7) | 3802 | 1.682 | 1.08–2.62 | 0.021 |
| Day shift | 23 (2.6) | 858 (97.4) | 881 | |||
| Parameters | Night Shift with CVD | Day Shift with CVD | Total | Risk | ||
|---|---|---|---|---|---|---|
| N % | N % | N | OR /Differences | IC95% | p | |
| Gender | ||||||
| Male | 139 4.5 | 20 3.0 | 159 | 1.52 | 1.04–2.44 | 0.046 |
| Female | 25 3.4% | 3 1.3% | 28 | 2.55 | 0.76–8.54 | 0.127 |
| Age | ||||||
| Average age (years ± SD) | 37.76 ± 9.29 | 37.86 ± 8.62 | 0.1 | −0.57–0.77 | 0.77 | |
| <50 years | 91 2.7% | 13 1.6% | 104 | 1.67 | 0.93–3.01 | 0.085 |
| 50–65 years | 73 17.1% | 10 12.0% | 83 | 1.51 | 0.74–3.05 | 0.257 |
| Seniority in work | ||||||
| Years | 7.59 ± 5.57 | 8.8 ± 6.1 | 1.21 y | 0.79–1.63 | <0.001 | |
| 0–10 years | 63 2.5% | 4 0.8% | 67 | 3.16 | 1.14–8.72 | 0.026 |
| >10 years | 101 7.6% | 19 4.8% | 120 | 1.62 | 1.05–2.53 | 0.042 |
| Type of work | ||||||
| Physical | 162 4.3% | 15 4.2% | 177 | 1.02 | 0.59–1.75 | 0.94 |
| Sedentary | 8 6.7% | 2 1.5% | 10 | 4.62 | 1.03–20.76 | 0.04 |
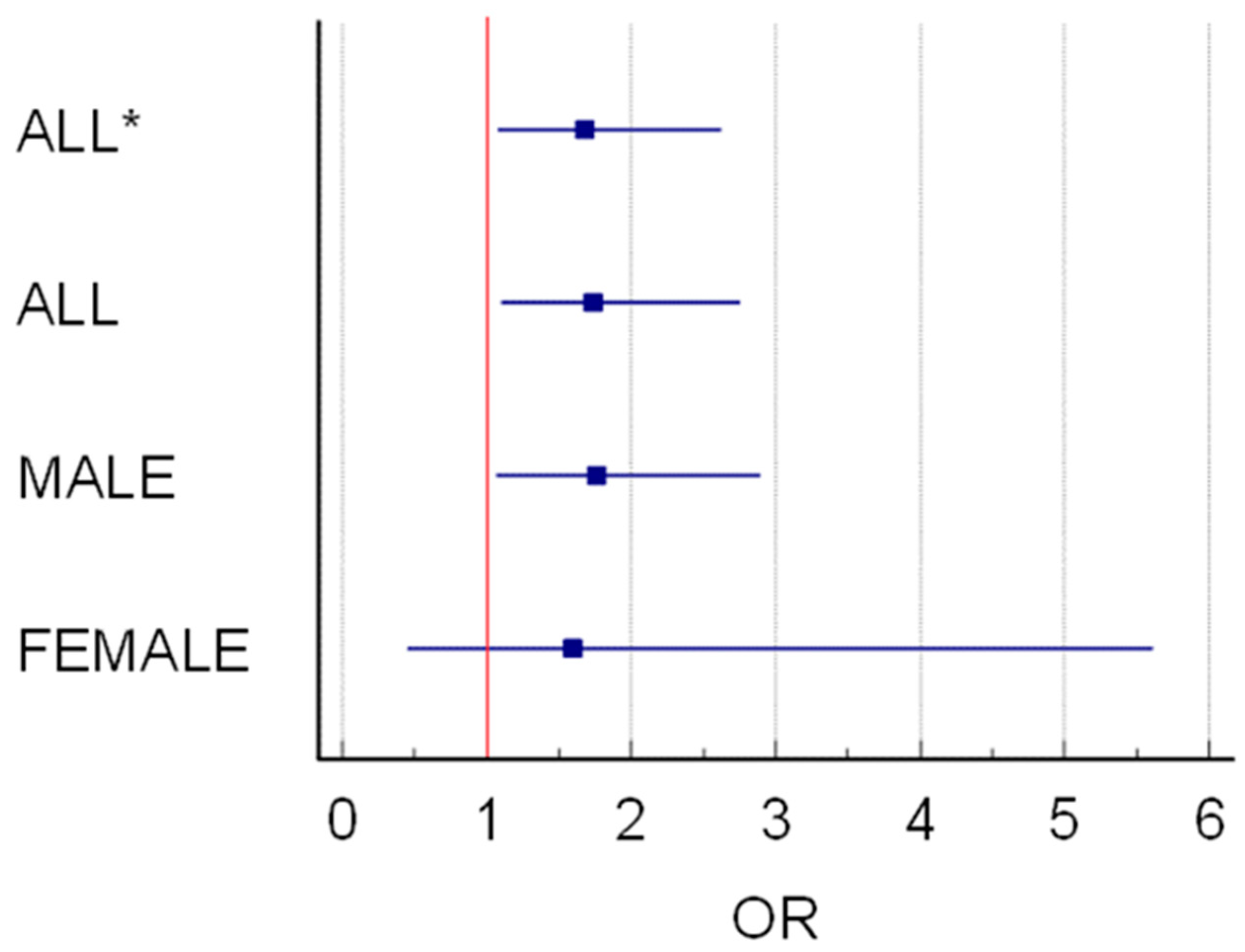
| Odds Ratio | 95% CI | Regression Coefficients | Std. Error | p | |
|---|---|---|---|---|---|
| Night Shift | |||||
| ALL * | 1.68 | 1.08 to 2.62 | 0.52 | 0.23 | 0.021 |
| ALL | 1.74 | 1.09–2.75 | 0.55 | 0.24 | 0.019 |
| MALE | 1.75 | 1.07 to 2.89 | 0.56 | 0.25 | 0.026 |
| FEMALE | 1.59 | 0.45 to 5.61 | 0.46 | 0.64 | 0.47 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bunescu, M.G.; Gheorman, V.; Marcu, I.R.; Lungulescu, C.V.; Dinescu, V.C. Tackling Shift Work: Cardiovascular Health in the Auto Industry. Healthcare 2024, 12, 1097. https://doi.org/10.3390/healthcare12111097
Bunescu MG, Gheorman V, Marcu IR, Lungulescu CV, Dinescu VC. Tackling Shift Work: Cardiovascular Health in the Auto Industry. Healthcare. 2024; 12(11):1097. https://doi.org/10.3390/healthcare12111097
Chicago/Turabian StyleBunescu, Marius Gabriel, Veronica Gheorman, Iulia Rahela Marcu, Cristian Virgil Lungulescu, and Venera Cristina Dinescu. 2024. "Tackling Shift Work: Cardiovascular Health in the Auto Industry" Healthcare 12, no. 11: 1097. https://doi.org/10.3390/healthcare12111097
APA StyleBunescu, M. G., Gheorman, V., Marcu, I. R., Lungulescu, C. V., & Dinescu, V. C. (2024). Tackling Shift Work: Cardiovascular Health in the Auto Industry. Healthcare, 12(11), 1097. https://doi.org/10.3390/healthcare12111097





