Exploring Factors Influencing Caregiver Burden: A Systematic Review of Family Caregivers of Older Adults with Chronic Illness in Local Communities
Abstract
1. Introduction
Purpose of the Present Study
- (1)
- To identify characteristics of chronically ill community-dwelling older adults and their family caregivers’ burden through a systematic review.
- (2)
- To identify factors affecting caregiving burden of family caregivers of community-dwelling older adults with chronic diseases through a systematic review.
2. Methods
2.1. Research Design
2.2. Data Sources
2.3. Inclusion and Exclusion Criteria
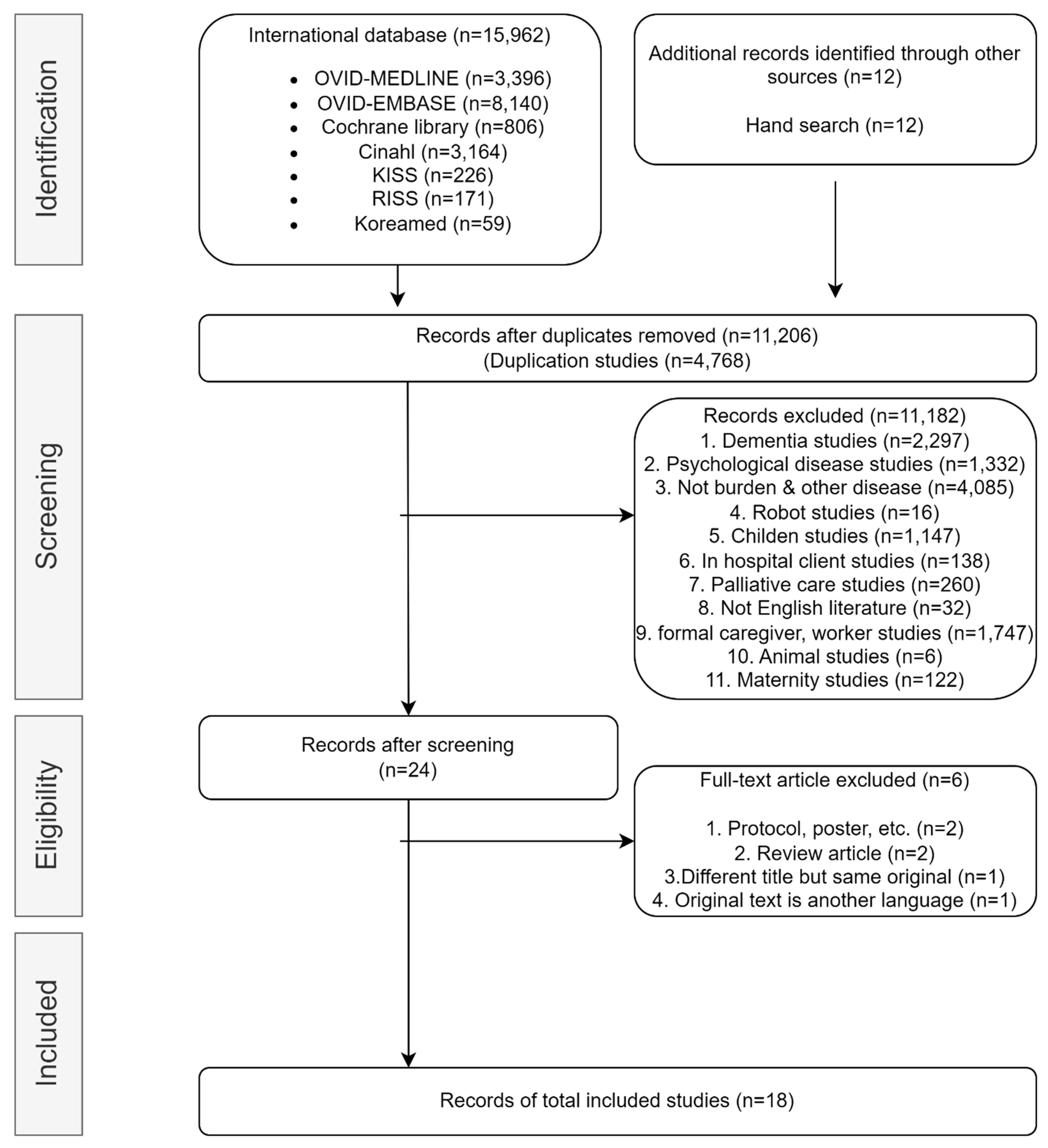
2.4. Selection Process and Data Extraction
3. Results
3.1. Selected Documents
3.2. General Characteristics of Selected Studies
3.3. Key Elements Identified through Selected Studies
3.3.1. Family Caregiver Burden Assessment Tool
3.3.2. Care Recipient Variables Affecting Caregiving Burden
3.3.3. Caregiver Variables That Affect Caregiving Burden
4. Discussion
4.1. Limitations
4.2. Implications for Practice and Suggestions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015; Available online: https://iris.who.int/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1 (accessed on 26 April 2023).
- Korean Statistical Information Service. 2023 Elderly Statistics. Available online: https://kostat.go.kr/board.es?mid=a10301010000&bid=10820&list_no=427252&act=view&mainXml=Y (accessed on 26 September 2023).
- Rechel, B.; Grundy, E.; Robine, J.M. Ageing in the European Union. Lancet 2013, 381, 1312–1322. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Current Status and Issues of Chronic Disease in 2023. Available online: https://www.kdca.go.kr/filepath/galleryDownload.es?bid=0003&list_no=146387&seq=1 (accessed on 26 December 2023).
- Kadambi, S.; Abdallah, M.; Loh, K.P. Multimorbidity, Function, and Cognition in Aging. Clin. Geriatr. Med. 2020, 36, 569–584. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, J.; Nicholas, S. Social support and depressive symptoms among family caregivers of older people with disabilities in four provinces of urban China: The mediating role of caregiver burden. BMC Geriatr. 2020, 20, 3. [Google Scholar] [CrossRef]
- Ornstein, K.; Gaugler, J.E. The problem with “problem behaviors”: A systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. Int. Psychogeriatr. 2012, 24, 1536–1552. [Google Scholar] [CrossRef]
- Cascella Carbó, G.F.; García-Orellán, R. Burden and Gender inequalities around Informal Care. Investig. Educ. Enferm. 2020, 38, e05. [Google Scholar] [CrossRef]
- Kavga, A.; Kalemikerakis, I.; Faros, A. The Effects of Patients’ and Caregivers’ Characteristics on the Burden of Families Caring for Stroke Survivors. Int. J. Environ. Res. Public Health. 2021, 18, 7298. [Google Scholar] [CrossRef]
- Jone, M. Effects of the Characteristics of the Elderly and Family Caregivers on the Caregiving Stresses. Korea Contents Assoc. 2014, 14, 274–282. [Google Scholar]
- Yu, S.Y. Analysis of Research Trends about Burden of Caring for Senile Dementia Patients in Korea. Health Welf. 2018, 20, 29–54. [Google Scholar]
- Zhang, S.; Xu, M.; Liu, Z.J.; Feng, J.; Ma, Y. Neuropsychiatric issues after stroke: Clinical significance and therapeutic implications. World J. Psychiatry 2020, 10, 125–138. [Google Scholar] [CrossRef]
- Mlenzana, N.B.; Frantz, J.M.; Rhoda, A.J.; Eide, A.H. Barriers to and facilitators of rehabilitation services for people with physical disabilities: A systematic review. Afr. J. Disabil. 2013, 2, a22. [Google Scholar] [CrossRef]
- Ko, Y.; Yu, S. Core nursing competency assessment tool for graduates of outcome-based nursing education in South Korea: A validation study. Jpn. J. Nurs. Sci. 2019, 16, 155–171. [Google Scholar] [CrossRef]
- Lu, N.; Liu, J.; Lou, V.W. Caring for frail elders with musculoskeletal conditions and family caregivers’ subjective well-being: The role of multidimensional caregiver burden. Arch. Gerontol. Geriatr. 2015, 61, 411–418. [Google Scholar] [CrossRef]
- Kristianingrum, N.D.; Ramadhani, D.A.; Hayati, Y.S.; Setyoadi, S. Correlation between the burden of family caregivers and health status of people with diabetes mellitus. J. Public Health Res. 2021, 10, 2227. [Google Scholar] [CrossRef]
- Rodríguez-González, A.M.; Rodríguez-Míguez, E.; Claveria, A. Determinants of caregiving burden among informal caregivers of adult care recipients with chronic illness. J. Clin. Nurs. 2021, 30, 1335–1346. [Google Scholar] [CrossRef]
- Faison, K.J.; Faria, S.H.; Frank, D. Caregivers of chronically ill elderly: Perceived burden. J. Community Health Nurs. 1999, 16, 243–253. [Google Scholar] [CrossRef]
- Schandl, A.; Ringborg, C.; Mälberg, K.; Johar, A.; Lagergren, P. Caregiver burden and health-related quality of life among family caregivers of oesophageal cancer patients: A prospective nationwide cohort study. Acta Oncol. 2022, 61, 1186–1191. [Google Scholar] [CrossRef]
- Schwartz, K.; Beebe-Dimmer, J.; Hastert, T.A.; Ruterbusch, J.J.; Mantey, J.; Harper, F.; Thompson, H.; Pandolfi, S.; Schwartz, A.G. Caregiving burden among informal caregivers of African American cancer survivors. J. Cancer Surviv. 2021, 15, 630–640. [Google Scholar] [CrossRef]
- Hooley, P.J.; Butler, G.; Howlett, J.G. The relationship of quality of life, depression, and caregiver burden in outpatients with congestive heart failure. Congest. Heart Fail. 2005, 11, 303–310. [Google Scholar] [CrossRef]
- Unnikrishnan, B.; Rathi, P.; Saxena, P.U.P.; Aggarwal, A.; Shekhar, S.; Bansal, S.; Naidu, B.V.; Menon, S. Psychosocial burden among informal caregivers of adult cancer patients attending a tertiary care cancer center in coastal south India. Sage Open 2019, 9, 2158244019876287. [Google Scholar] [CrossRef]
- Iecovich, E. Caregiving burden, community services, and quality of life of primary caregivers of frail elderly persons. J. Appl. Gerontol. 2008, 27, 309–330. [Google Scholar] [CrossRef]
- Alshammari, S.A.; Alzahrani, A.A.; Alabduljabbar, K.A.; Aldaghri, A.; Alhusainy, Y.; Khan, M.; Alshuwaier, R.; Kariz, I.N. The burden perceived by informal caregivers of the elderly in Saudi Arabia. J. Fam. Community Med. 2017, 24, 145–150. [Google Scholar] [CrossRef]
- Brinda, E.M.; Rajkumar, A.P.; Enemark, U.; Attermann, J.; Jacob, K.S. Cost and burden of informal caregiving of dependent older people in a rural Indian community. BMC Health Serv. Res. 2014, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Glass, G.; Chua, K.C.; Ali, N.; Lim, W.S. Relationship between Mastery and Caregiving Competence in Protecting against Burden, Anxiety and Depression among Caregivers of Frail Older Adults. J. Nutr. Health Aging 2018, 22, 1238–1245. [Google Scholar] [CrossRef]
- Chen, M.C.; Chen, K.M.; Chu, T.P. Caregiver burden, health status, and learned resourcefulness of older caregivers. West. J. Nurs. Res. 2015, 37, 767–780. [Google Scholar] [CrossRef]
- Choi, J.Y.; Sok, S.R. Relationships among family support, health status, burnout, and the burden of the family caregiver caring for Korean older adults. J. Hosp. Palliat. Nurs. 2012, 14, E1–E8. [Google Scholar] [CrossRef]
- Freeman, S.; Kurosawa, H.; Ebihara, S.; Kohzuki, M. Caregiving burden for the oldest old: A population based study of centenarian caregivers in Northern Japan. Arch. Gerontol. Geriatr. 2010, 50, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Limpawattana, P.; Theeranut, A.; Chindaprasirt, J.; Sawanyawisuth, K.; Pimporm, J. Caregivers burden of older adults with chronic illnesses in the community: A cross-sectional study. J. Community Health 2013, 38, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Ong, H.L.; Vaingankar, J.A.; Abdin, E.; Sambasivam, R.; Fauziana, R.; Tan, M.-E.; Chong, S.A.; Goveas, R.R.; Chiam, P.C.; Subramaniam, M. Resilience and burden in caregivers of older adults: Moderating and mediating effects of perceived social support. BMC Psychiatry 2018, 18, 27. [Google Scholar] [CrossRef]
- Sabzwari, S.; Badini, A.M.; Fatmi, Z.; Jamali, T.; Shah, S. Burden and associated factors for caregivers of the elderly in a developing country. East. Mediterr. Health J. 2016, 22, 394–403. [Google Scholar] [CrossRef]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Zarit Burden Interview. Gerontologist 1980, 41, 652–657. [Google Scholar]
- Kwon, J.D. The Determinant Model of Caregiver Burden In Caring for the Demented Elderly in Korea. Health Soc. Welf. Rev. 1994, 14, 1–16. [Google Scholar]
- Kim, M.J. Associated Factors Caused by Falls of Older People in Community-Dwelling. Unpublished Master’s Dissertation, Ewha Womans University, Seoul, Republic of Korea, 2004. [Google Scholar]
- Ma, B.S. A Study on the People in Charge of the Demented: Especially People in the Day Care Center or Short Stay Service. Unpublished Master’s Thesis, Ewha Womans University, Seoul, Republic of Korea, 1998. [Google Scholar]
- Rhee, K.O. A study on caregiving burden among family caregivers of impaired elderly. J. Korean Gerontol. Soc. 2000, 20, 215–228. [Google Scholar]
- Yoon, H.S.; Ryu, S.H. Factors Associated with Family Caregivers’ Burden of Frail Elders-Comparing Spouse with Adult Children. Korean Gerontol. Soc. 2007, 27, 195–211. [Google Scholar]
- Kim, H.M. A Study on the Burden of the People Supporting the Dementia Elderly-Since Operation of the Dementia Elderly Daycare Centers. Unpublished Master’s Thesis, MYONGJI University, Seoul, Republic of Korea, 2005. [Google Scholar]
- Hong, D.I. A study on the Caregiving Burden of Elderly Primary Caregivers Using Day Shelters. Unpublished Master’s Thesis, Pyeongtaek University, Pyeongtaek, Republic of Korea, 2002. [Google Scholar]
- Yoon, H.S. Who Care for the Elderly? Family Responsibility vs. Social Responsibility. Korean J. Fam. Law 2000, 14, 201–226. [Google Scholar]
- Cohen, S.; Doyle, W.J.; Skoner, D.P.; Rabin, B.S.; Gwaltney, J.M., Jr. Social ties and susceptibility to the common cold. JAMA 1997, 277, 1940–1944. [Google Scholar] [CrossRef] [PubMed]
- Williamson, G.M.; Schulz, R. Coping with specific stressors in Alzheimer’s disease caregiving. Gerontologist 1993, 33, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.A. Discussion on “How to Institutionalize the Training and Education of Care Managers and Care Workers in the Elderly Care Insurance System”; Korean Academy of Care Work: Seoul, Republic of Korea, 2006; pp. 156–162. [Google Scholar]
- Woo, K.H. The Subjective Experience of Caregiving and Social Support for Family Caregivers of the Elderly with Dementia. Korean J. Soc. Welf. Stud. 1997, 10, 383–413. [Google Scholar]
- Yoon, H.S.; Cha, H.B.; Cho, S.H. The Impact of Social Support on the Family Caregivers’ Burden and Depression. Korean Gerontol. Soc. 2000, 20, 1–19. [Google Scholar]
- Yang, O.N. A Study on Stress of the Aged and Their Supporters and Coping strategies. Unpublished Master’s Thesis, Ewha Womans University, Seoul, Republic of Korea, 1995. [Google Scholar]
- Lee, Y.O. Factors Affecting Caregiving Burden for Elderly Caregivers of Stroke Survivors. Unpublished Master’s Thesis, Daejeon University, Daejeon, Republic of Korea, 2002. [Google Scholar]
- Lee, H.J. Influencing Factors and Caregiving burden among primary caregiver for Demented Elderly. Korean J. Care Work. 2006, 2, 33–60. [Google Scholar]
- Kim, J.M.; Shin, L.S.; Yoon, J.S. Determinants of Care Burden of Caregiver in Patients with Dementia. J. Korean Neuropsychiatr. Assoc. 2002, 40, 1106–1113. [Google Scholar]
- Lee, Y.M.; Yoo, I.Y. Care Burden, Depression and Social Welfare Service Utilization among Family Caregiver for Demented Elderly. Korean Gerontol. Soc. 2005, 25, 111–121. [Google Scholar]
- Kim, Y.J.; Choi, H.K. A Study on the burden, gratification, and family support of in-home dementia caregiver. Korean Gerontol. Soc. 1993, 13, 63–83. [Google Scholar]
- Park, J.H.; Lee, Y.R. Causes and Treatment of Dementia; Hakmunsa: Seoul, Republic of Korea, 1997. [Google Scholar]
- Lee, H.J. Factors affecting family caregivers’ health related behavior change to the elderly with chronic diseases. Korean J. Fam. Soc. Work 2007, 19, 29–53. [Google Scholar]
- Kim, E.K.; Park, H.O. Factors associated with Burden of Family Caregivers of Home-Dwelling Elderly People with Dementia: A Systematic Review and Meta-Analysis. Korean J. Adult Nurs. 2019, 31, 351–364. [Google Scholar] [CrossRef]
| No. | Author/Year | Methodological Variables | Content-Specific Variables | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Care Recipient Variables | Caregiver Variables | |||||||||
| Design | Location and Sample Size (n) | Burden Measurement | Chronic Illness/Disability State among Surveyed Older Adults | Mean Age | % of Female | Dominant Relationship with Older Adults | Mean Age | Average Care Duration | ||
| 1 | Lu et al., 2015 [15] | Cross-sectional | China n = 494 older adult–caregiver dyads | 24-item Chinese Caregiver Burden Inventory Approach: Self-administered questionnaire | Musculoskeletal condition/more than two-thirds of the older adults needed assistance to complete more than two out of ten activities of daily living or equivalent (70.6%) | 83.393 | 51.4% | Children/son-in-law/daughter-in-law: 71.9% | 62.645 | - |
| 2 | Kristaningrum et al., 2021 [16] | Cross- sectional | Indonesia n = 327 DM patients and their families | ZBI Approach: Self-administered questionnaire | Diabetes mellitus | 45–65 | 48.6% | Child: 47.1% | <45 | - |
| 3 | Roudriguez-Gonzalez et al., 2021 [17] | Cross- sectional | Spain n = 148 care recipients, 135 caregivers | Zarit Burden Interview Approach: Self-administered questionnaire | Chronic illness/ADL mean | ≥80 | 91.1% | - | 55–64 | ≥6 years |
| 4 | Faison et al., 1999 [18] | Cross- sectional | USA n = 88 caregivers of older chronically ill persons | BI(Burden Interview) Approach: Self-administered questionnaire | CVD, neurological disorder, psychiatric disease, dementia, Endocrine disorder, etc. | - | 77% | Daughters: 54.5% | 53.5 | >5 years |
| 5 | Schandl et al., 2022 [19] | Cross- sectional | Sweden n = 319 family caregivers | The Caregiver Burden Scale Approach: Self-administered questionnaire | Esophageal cancer (adenoCa.) | 67 | 86% | Spouse: 83% | 66 | - |
| 6 | Schwartz et al., 2020 [20] | Cross- sectional | USA n = 560 informal caregivers | the 22-item Zarit Burden Interview Approach: Self-administered questionnaire | Cancer/ADL mean 2.8, IADL mean 5.0 | - | 77% | Spouse/significant other: 42% | 52.6 | - |
| 7 | Hooley et al., 2005 [21] | Cross- sectional | Canada n = 50 patients and 50 primary caregivers | ZCB (Zarit Caregiver Burden) Approach: Self-administered questionnaire | CHF, HTN, DM, MI | 72 ± 11 | 80% | Spouse: 66% | 61 ± 14 | - |
| 8 | Unnikrishnan et al., 2019 [22] | Cross- sectional | India n = 205 caregivers of patients with cancer | ZBI (Zarit Burden Interview) Approach: Self-administered questionnaire | Cancer | 52.6 | 48% | Children: 38% | 42.4 | <6 months |
| 9 | Iecovich, 2008 [23] | Cross- sectional | Israel n = 114 primary caregivers | Zarit scale Approach: face-to-face interview | Frail older people | 79.58 | 67.5% | Adult child: 70.3% | 52.89 | 5.42 years |
| 10 | Alshammari et al., 2017 [24] | Cross- sectional | Saudi Arabia n = 315 informal caregivers | ZBI-22 Approach: Self-administered questionnaire | Chronic problems or disabilities, cognitive impairment, and senility | 70–80 | 52.7% | Children: 69.8% | 18~27 (43.8%) | |
| 11 | Brinda et al., 2014 [25] | Cross- sectional | India n = 85 primary caregivers who provided assistance for ADL and accompanied their older care recipients to health facilities | ZBI-22 Approach: Self-administered questionnaire | Stroke, dementia, falls, incontinence WHODAS II mean score: 35.2 ± 13.5 | 74.3 ± 6.7 | 80% | Co-residence 87.1% | 44.2 ± 14.1 | 38.6 h/week |
| 12 | Chan et al., 2018 [26] | Cross- sectional | Singapore n = 274 patient–caregiver dyads | ZBI-22 Approach: Self-administered questionnaire | BI means: 19.48 ± 5.59 Dementia: 50.4% NPI-Q mean: 7.37 ± 6.59 | 85.29 ± 8 | 65% | Children: 70.8% | 59.1 ± 10.5 | 88.96 ± 66.13 h/week |
| 13 | Chen et al., 2015 [27] | Cross- sectional | Taiwan n = 108 caregivers of disabled older adults who received home care services with intact cognition | Caregiver Burden Scale Approach: Self-administered questionnaire | Total dependence on caregivers: 63.89% ± 25.88 BI score of >/=60:19.86 | 80.53 ± 7.17 | 65.74% | Spouse: 81.48% | 74.03 ± 6.02 | 17.50 ± 7.52 h/day |
| 14 | Choi et al., 2012 [28] | Cross- sectional | South Korea n = 267 caregivers | Burden Scale Approach: Self-administered questionnaire | Arthritis, hypertension, diabetes mellitus, dementia, stroke, cancer, heart disease | - | 62.5% | Children: 47.4% | - | >10 years (40.5%) |
| 15 | Freeman et al., 2010 [29] | Cross- sectional | Japan n = 160 older adults and 84 caregivers | Japan-ZBI (J-ZBI) Burden Index of Care (BIC) Approach: Self-administered questionnaire | BI mean scores 80–89 years: 86.7 ± 27.0 90–99 years: 63.5 ± 31.2 100 + years: 44.2 ± 33.9 | 95.35 ± 7.15 | 88.09% | Children: 54.4% | 63.7 ± 12.75 | 8.5 ± 7.8 h/day |
| 16 | Limpawattana et al., 2013 [30] | Cross- sectional | Taiwan n = 150 informal caregivers | ZBI-22 Approach: Self-administered questionnaire | Hypertension, diabetes, gastric disease, musculoskeletal disease, eye disease, respiration trace disease, and stroke | - | 80.67% | Children: 48.67% | 51.2 ± 13.7 | 60 month |
| 17 | Ong et al., 2018 [31] | Cross- sectional | Singapore n = 285 caregivers | ZBI-22 Approach: Self-administered questionnaire | Hypertension, hyperlipidemia, diabetes mellitus, mental illnesses including dementia | >60 | 64.6% | Children: 78.6% | 40–65 | - |
| 18 | Sabzwari et al., 2016 [32] | Cross- sectional | Pakistan n = 350 caregivers | Perceived Caregiver Burden Scale Approach: Self-administered questionnaire | Arthritis, hypertension, diabetes, memory, and agitation requires assistance: 45.7% With an assisted device: 13.7% Bedridden: 3.4% | 71.1 ± 10.1 | 68.9% | Daughter in law 34% | - | 47.23 ± 15.5 years |
| Name of the Assessment Tool | Mean Range in Selected Studies | Range of Scale | Interpretation of Scores | Summary of Findings |
|---|---|---|---|---|
| Zarit Burden Inventory Japanese version of Zarit Burden Interview (J-ZBI) | 24.09 | 0–88 | 0–20: no or little burden 21–40: little to moderate burden 41–60: moderate to severe burden 61–88: severe burden | Little to moderate burden |
| Short version of the Zarit Burden Interview | 29.42 | 12–60 | Moderate level of burden | |
| ZBI’s short version for palliative care | 19.6 | 7–35 | 17 or more points: “severely” burdened | Higher scores correspond to a greater caregiving burden |
| 24-item Chinese Caregiving Burden Inventory | 24.85 | 0–96 | Higher scores indicate a higher degree of burden | High score indicates a high level of burden |
| Caregiver Burden Scale | 25.13 | 0–60 | Resulting scores were used to represent the level of burden. Compared with low caregiver burden, high to moderate burden was associated with reductions in all HRQL aspects. | |
| Caregiver Burden Scale | ≥2 | 1–3.99 | 1.00–1.99: low burden 2.00–2.99: moderate burden 3.00–3.99: high burden | High to moderate caregiver burden |
| Personal Variables | ||
|---|---|---|
| Age | Freeman, 2008 [29] | Care recipient age increases, and it becomes a heavier burden on their caregivers. |
| Functional ability (ADL/IADL, BI) | Lu, 2015 [15] | Functional health was associated with all five dimensions of burden. |
| Roudriguez-Gonzalez, 2021 [17] | Burden severity increases significantly with the level of dependence. | |
| Faison, 1999 [18] | Increases in ADL were associated with increases in caregiver burden. | |
| Schwartz, 2020 [20] | ADLs associated with high CGB included feeding and toileting. | |
| Brinda, 2014 [25] | The dependent older people and the time spent on ADL increased the burden on caregivers. | |
| Sabzwari, 2016 [32] | The higher the physical and cognitive dependence, the greater the burden on the caregiver. | |
| Chronic illnesses | Roudriguez-Gonzalez, 2021 [17] | Care related to incontinence has the greatest effect on burden. |
| Faison, 1999 [18] | A significant correlation was observed between incontinence and caregiver burden. | |
| Hooley, 2005 [21] Brinda, 2014 [25] Sabzwari, 2016 [32] | Increased caregiver burden is associated with disease burden. CVD, Parkinsonism, higher disability, and urinary incontinence significantly worsened the burden. Stroke was significantly associated with perceived caregiver burden. | |
| Behavioral problem Cognition/Mental disorder | Lu, 2015 [15] Roudriguez-Gonzalez, 2021 [17] Sabzwari, 2016 [32] Lu, 2015 [15] Hooley, 2005 [21] Sabzwari, 2016 [32] | Behavioral problems seemed to be the most demanding stressor of caregiver burden. Burdens are aggravated when the patient has behavioral problems. The behavioral problem of the older people was a predictor of increasing the burden on caregivers. Caregiver’s cognitive status affects different dimensions of caregiver burden. Caregiver burden and patient depression score were significantly correlated. Older people with difficulty sleeping were predictors of a higher caregiver burden. |
| Personal Variables | ||
|---|---|---|
| Age | Schandl, 2022 [19] | Younger family caregivers were more likely to have a higher burden on caregivers. |
| Unnikrishnan, 2019 [22] | Caregivers of patients who were of older age had moderate to severe burden. | |
| Limpawattana, 2013 [30] | The age of caregivers had a positive relationship with ZBI scores. | |
| Sex | Unnikrishnan, 2019 [22] | Female caregivers had moderate to severe burden. |
| Freeman, 2008 [29] | Male caregivers experienced lower levels of burden compared to female caregivers. | |
| Marital status | Schwartz, 2020 [20] | Variables associated with high CGBs included married people. |
| Relation | Faison, 1999 [18] | Sons reported significantly less burden than did either daughters or others. |
| Freeman, 2008 [29] | Male caregivers, who are biological children, experienced lower burdens than female caregivers. | |
| Education | Lu, 2015 [15] | The higher the level of education, the higher the level of developmental burden. |
| Schwartz, 2020 [20] | High CGBs have been reported at educational levels above 4-year college degrees. | |
| Duration of caregiving | Lu, 2015 [15] | Shorter informal care hours were associated with lower levels of physical burden. |
| Brinda, 2014 [25] | Time spent on helping ADL and on supervision increased the caregiver’s burden. | |
| Limpawattana, 2013 [30] | Duration of care had a positive relationship with ZBI scores. | |
| Health status | Roudriguez-Gonzalez, 2021 [17] | Poor caregiver health also contributes to burden levels. |
| Schwartz, 2020 [20] | Self-reported poor health was reported as a high CGB. | |
| Hooley, 2005 [21] | ZBI scores were associated with an increased number of medications and comorbidities. | |
| Chen, 2015 [27] | Lower physical health and higher caregiver burden scores. | |
| Choi, 2010 [28] | There were significant correlations between health status and the burden of the family caregiver. | |
| Limpawattana, 2013 [30] | Self-reported health status had a positive relationship with ZBI scores. | |
| Employment status | Roudriguez-Gonzalez, 2021 [17] | Not being retired also contributes to burden levels. |
| Unnikrishnan, 2019 [22] | Caregivers of patients who were unemployed had moderate to severe burden. | |
| Freeman, 2008 [29] | Employed caregivers experienced less burden than unemployed caregivers. | |
| Income | Schwartz, 2020 [20] | Higher income levels were reported as higher CGBs. |
| Hooley, 2005 [21] | Caregivers with lower income had higher caregiver burden ZCB scores. | |
| Limpawattana, 2013 [30] | Self-reported income had a negative relationship with ZBI scores. | |
| Sabzwari, 2016 [32] | Financial impact had a strong correlation with perceived caregiver burden. | |
| Support (family, social) | Iecovich, 2008 [23] | Caregiver burden increased according to the availability of formal community-based services. |
| Choi, 2010 [28] | There were significant correlations between family support and caregiving burden. | |
| Ong, 2018 [31] | Caregivers with a higher level of social support experience a lower level of burden. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.Y.; Lee, S.H.; Yu, S. Exploring Factors Influencing Caregiver Burden: A Systematic Review of Family Caregivers of Older Adults with Chronic Illness in Local Communities. Healthcare 2024, 12, 1002. https://doi.org/10.3390/healthcare12101002
Choi JY, Lee SH, Yu S. Exploring Factors Influencing Caregiver Burden: A Systematic Review of Family Caregivers of Older Adults with Chronic Illness in Local Communities. Healthcare. 2024; 12(10):1002. https://doi.org/10.3390/healthcare12101002
Chicago/Turabian StyleChoi, Jin Young, Seon Heui Lee, and Soyoung Yu. 2024. "Exploring Factors Influencing Caregiver Burden: A Systematic Review of Family Caregivers of Older Adults with Chronic Illness in Local Communities" Healthcare 12, no. 10: 1002. https://doi.org/10.3390/healthcare12101002
APA StyleChoi, J. Y., Lee, S. H., & Yu, S. (2024). Exploring Factors Influencing Caregiver Burden: A Systematic Review of Family Caregivers of Older Adults with Chronic Illness in Local Communities. Healthcare, 12(10), 1002. https://doi.org/10.3390/healthcare12101002






