Determinants of Working Practice Location for Clinicians According to High School, Medical School, and Resident Training Locations in Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
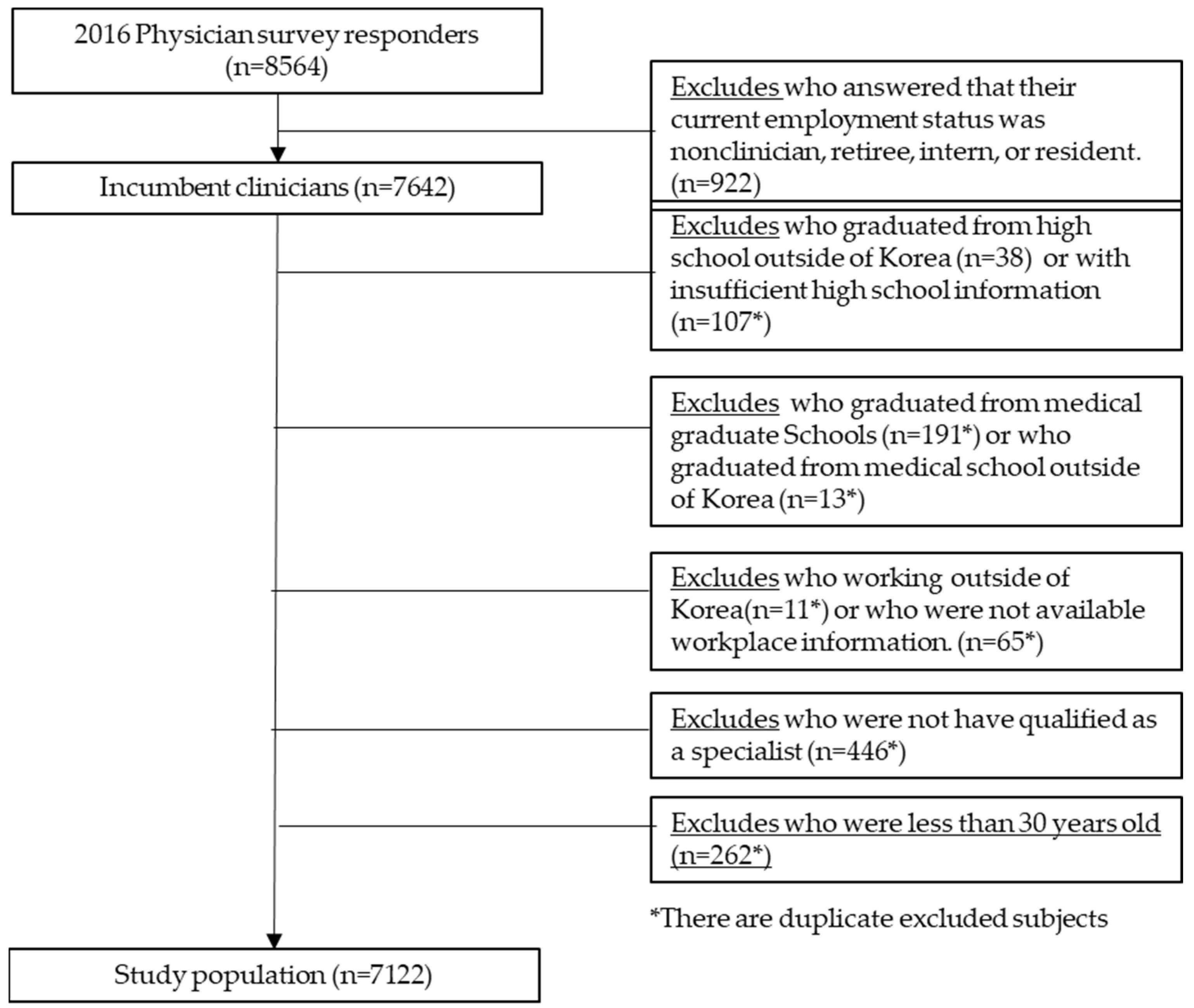
2.2. Selection of Study Population
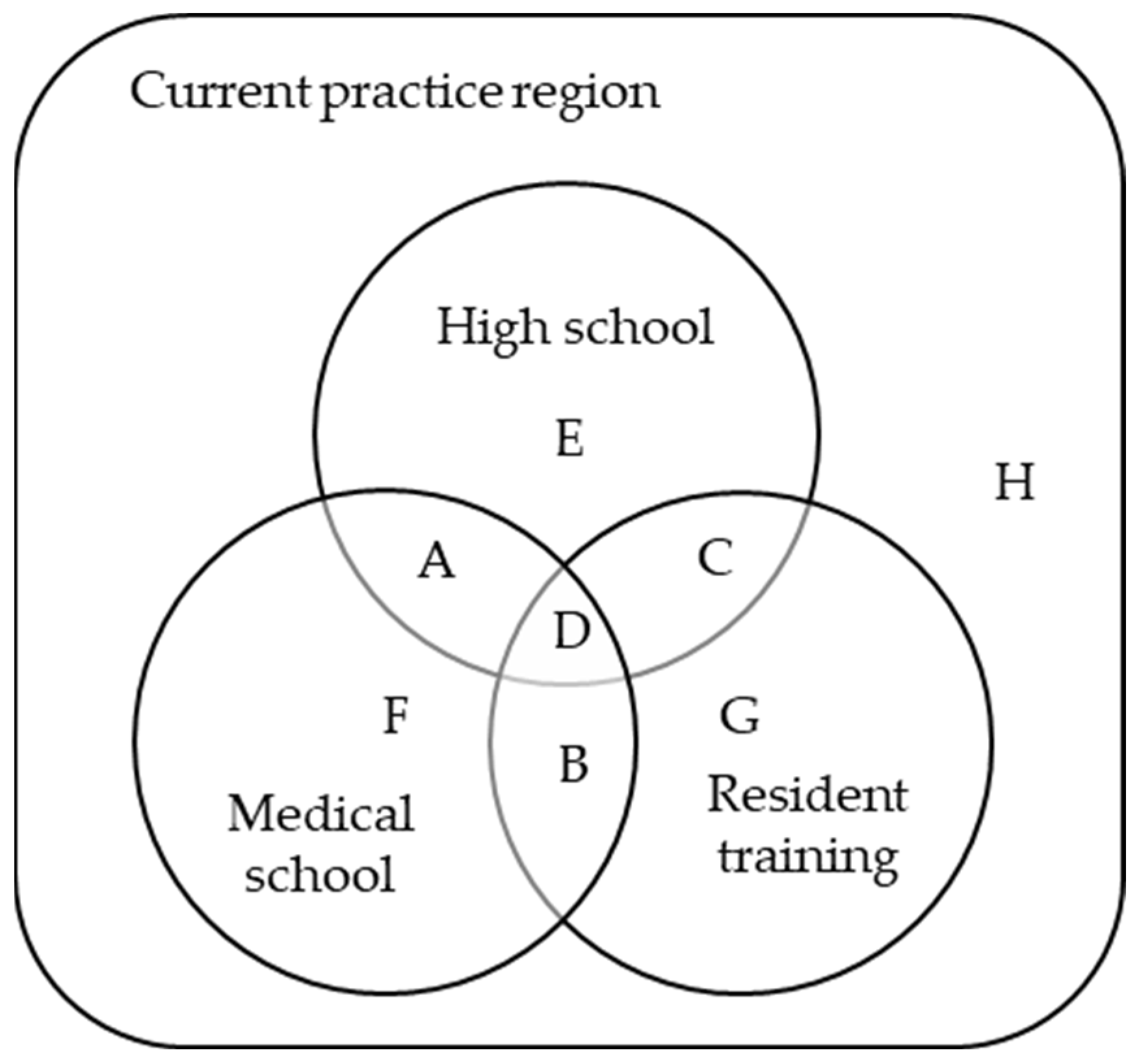
2.3. Variables
2.4. Data Analysis
2.5. Ethics Statement
3. Results
3.1. Proportions of Each Subgroup in Metropolitan and Non-Metropolitan Regions
3.2. Relations between Subgroups and Sociodemographic Characteristics
3.3. Retention Rates in Metropolitan and Non-Metropolitan Regions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ono, T.; Schoenstein, M.; Buchan, J. Geographic Imbalances in Doctor Supply and Policy Responses (Presentation). OECD Health Work. Pap. 2014, 69, 1–65. [Google Scholar]
- 46.4% of Medical School Freshmen This Year Are from the Metropolitan Area. 7 Medical Schools Didn’t Fill Local Talent Quota. Available online: https://m.medigatenews.com/news/1818231323 (accessed on 11 March 2023).
- [2022 Health and Welfare Committee National Audit] This Year, the Vacancy Rate of Doctors at Local Medical Centers Doubled Compared to 2018. Available online: http://www.newsmp.com/news/articleView.html?idxno=227004 (accessed on 11 March 2023).
- Kim, C.-Y.; Yoon, S.; Lee, J.S.; Kim, Y.-I. Individual Factors Influencing the Location Decisions of Practicing Physicians. Korean J. Health Policy Adm. 1999, 9, 21–32. [Google Scholar]
- Keley, E.T.; Ravaghi, H.; Salehi, M.; Nasiripour, A.A.; Abdi, Z.; Meshkini, A. Relationship between Per sonal Characteristics of Specialist Physicians and Choice of Practice Location in Iran. Rural. Remote Health 2016, 16, 1–11. [Google Scholar] [CrossRef]
- Patterson, D.G.; Andrilla, C.H.A.; Larson, E.H. Graduates of Rural-Centric Family Medicine Residencies: Determinants of Rural and Urban Practice. Policy Brief 2016, 159, 1–10. [Google Scholar]
- Mohammadiaghdam, N.; Doshmangir, L.; Babaie, J.; Khabiri, R.; Ponnet, K. Determining Factors in the Retention of Physicians in Rural and Underdeveloped Areas: A Systematic Review. BMC Fam. Pract. 2020, 21, 216. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; O’Sullivan, B.G. Increasing Doctors Working in Specific Rural Regions through Selection from and Training in the Same Region: National Evidence from Australia. Hum. Resour. Health 2021, 19, 132. [Google Scholar] [CrossRef] [PubMed]
- Kim, K. Factors Associated with Practice Locations of Active Specialist Physicians in Korea: Focusing on Their Hometown, Medical Education and Residency Training Locations. Health Serv. Manag. Rev. 2021, 15, 13–23. [Google Scholar] [CrossRef]
- Korean Physician Survey (KPS). Available online: https://rihp.re.kr/eng/doctor/introduce.php (accessed on 11 March 2023).
- Enforcement Decree of the Act on Fostering Local Universities and Talents. Available online: https://www.law.go.kr/%EB%B2%95%EB%A0%B9/%EC%A7%80%EB%B0%A9%EB%8C%80%ED%95%99%20%EB%B0%8F%20%EC%A7%80%EC%97%AD%EA%B7%A0%ED%98%95%EC%9D%B8%EC%9E%AC%20%EC%9C%A1%EC%84%B1%EC%97%90%20%EA%B4%80%ED%95%9C%20%EB%B2%95%EB%A5%A0%20%EC%8B%9C%ED%96%89%EB%A0%B9 (accessed on 1 March 2023).
- Kim, K.H.; Lim, S.M.; Park, J.H.; Lim, J.Y. A Study on the Working Status of Doctors by Region and Ways to Maintain Incentives; Korean Medical Association, Research Institute for Healthcare Policy: Seoul, Korea, 2022. [Google Scholar]
- Programs for Rural Physicians|Doctors of BC. Available online: https://www.doctorsofbc.ca/managing-your-practice/practice-supports/programs-rural-physicians (accessed on 1 March 2023).
- Workforce Incentive Program Guidelines|Australian Government Department of Health and Aged Care. Available online: https://www.health.gov.au/resources/publications/workforce-incentive-program-guidelines?language=en (accessed on 1 March 2023).
| Current Practice Region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Metro | Non-Metro (6 Regions Subtotal) | Chung Cheong | Jeolla | Gangwon | Daegu/ Gyeongbuk | Busan/ Ulsan/ Gyeongnam | Jeju | |||
| Subgroup | A | n | 15 | 296 | 66 | 97 | 8 | 50 | 73 | 2 |
| % | 0.4 | 8.2 | 9.3 | 12.7 | 4.1 | 6.6 | 6.6 | 2.2 | ||
| B | n | 548 | 175 | 64 | 23 | 27 | 26 | 35 | 0 | |
| % | 15.7 | 4.8 | 9.0 | 3.0 | 13.9 | 3.4 | 3.2 | 0.0 | ||
| C | n | 409 | 52 | 6 | 4 | 1 | 10 | 31 | 0 | |
| % | 11.7 | 1.4 | 0.8 | 0.5 | 0.5 | 1.3 | 2.8 | 0.0 | ||
| D | n | 1611 | 1917 | 213 | 550 | 23 | 519 | 612 | 0 | |
| % | 46.1 | 52.9 | 30.0 | 72.0 | 11.9 | 68.2 | 55.4 | 0.0 | ||
| E | n | 90 | 182 | 32 | 29 | 10 | 26 | 68 | 17 | |
| % | 2.6 | 5.0 | 4.5 | 3.8 | 5.2 | 3.4 | 6.2 | 18.9 | ||
| F | n | 8 | 67 | 33 | 6 | 14 | 3 | 11 | 0 | |
| % | 0.2 | 1.8 | 4.6 | 0.8 | 7.2 | 0.4 | 1.0 | 0.0 | ||
| G | n | 603 | 87 | 19 | 1 | 9 | 8 | 49 | 1 | |
| % | 17.2 | 2.4 | 2.7 | 0.1 | 4.6 | 1.1 | 4.4 | 1.1 | ||
| H | n | 213 | 849 | 278 | 54 | 102 | 119 | 226 | 70 | |
| % | 6.1 | 23.4 | 39.1 | 7.1 | 52.6 | 15.6 | 20.5 | 77.8 | ||
| Total | 3497 | 3625 | 711 | 764 | 194 | 761 | 1105 | 90 | ||
| Current Practice Region | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Metropolitan | Chungcheong | Jeolla | Gangwon | Daegu/ Gyeongbuk | Busan/ Ulsan/ Gyeongnam | Jeju | |||||||||
| R | SP/S | R | SP/S | R | SP/S | R | SP/S | R | SP/S | R | SP/S | R | SP/S | ||
| Subgroup | A | 46.9 | 15/32 | 40 | 66/165 | 24 | 97/405 | 25.8 | 8/31 | 26.9 | 50/186 | 36.9 | 73/198 | 50 | 2/4 |
| B | 71.6 | 548/765 | 58.2 | 64/110 | 57.5 | 23/40 | 26.7 | 27/101 | 52 | 26/50 | 83.3 | 35/42 | 0 | 0 | |
| C | 77 | 409/531 | 66.7 | 6/9 | 57.1 | 4/7 | 100 | 1/1 | 71.4 | 10/14 | 86.1 | 31/36 | 0 | 0 | |
| D | 84.3 | 1611/1912 | 86.2 | 213/247 | 79.9 | 550/688 | 56.1 | 23/41 | 81.6 | 519/636 | 93.3 | 612/656 | 0 | 0/2 | |
| E | 39.1 | 90/230 | 17.9 | 32/179 | 9.8 | 29/295 | 20.8 | 10/48 | 14.3 | 26/182 | 20.9 | 68/326 | 27.9 | 17/61 | |
| F | 22.9 | 8/35 | 12.6 | 33/262 | 5.7 | 6/106 | 5.5 | 14/257 | 5.1 | 3/59 | 12.8 | 11/86 | 0 | 0/6 | |
| G | 58.9 | 603/1023 | 40.4 | 19/47 | 11.1 | 1/9 | 29.0 | 9/31 | 30.8 | 8/26 | 51 | 49/96 | 50 | 1/2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, K.; Kim, H.; Lee, J.; Shin, J.; Park, A. Determinants of Working Practice Location for Clinicians According to High School, Medical School, and Resident Training Locations in Korea. Healthcare 2023, 11, 1203. https://doi.org/10.3390/healthcare11091203
Park K, Kim H, Lee J, Shin J, Park A. Determinants of Working Practice Location for Clinicians According to High School, Medical School, and Resident Training Locations in Korea. Healthcare. 2023; 11(9):1203. https://doi.org/10.3390/healthcare11091203
Chicago/Turabian StylePark, Kyungah, Hyeongsu Kim, Jeehye Lee, Jinyoung Shin, and AhHyun Park. 2023. "Determinants of Working Practice Location for Clinicians According to High School, Medical School, and Resident Training Locations in Korea" Healthcare 11, no. 9: 1203. https://doi.org/10.3390/healthcare11091203
APA StylePark, K., Kim, H., Lee, J., Shin, J., & Park, A. (2023). Determinants of Working Practice Location for Clinicians According to High School, Medical School, and Resident Training Locations in Korea. Healthcare, 11(9), 1203. https://doi.org/10.3390/healthcare11091203








