Effects of Yoga for Coping with Premenstrual Symptoms in Taiwan—A Cluster Randomized Study
Abstract
1. Introduction
2. Materials and Methods
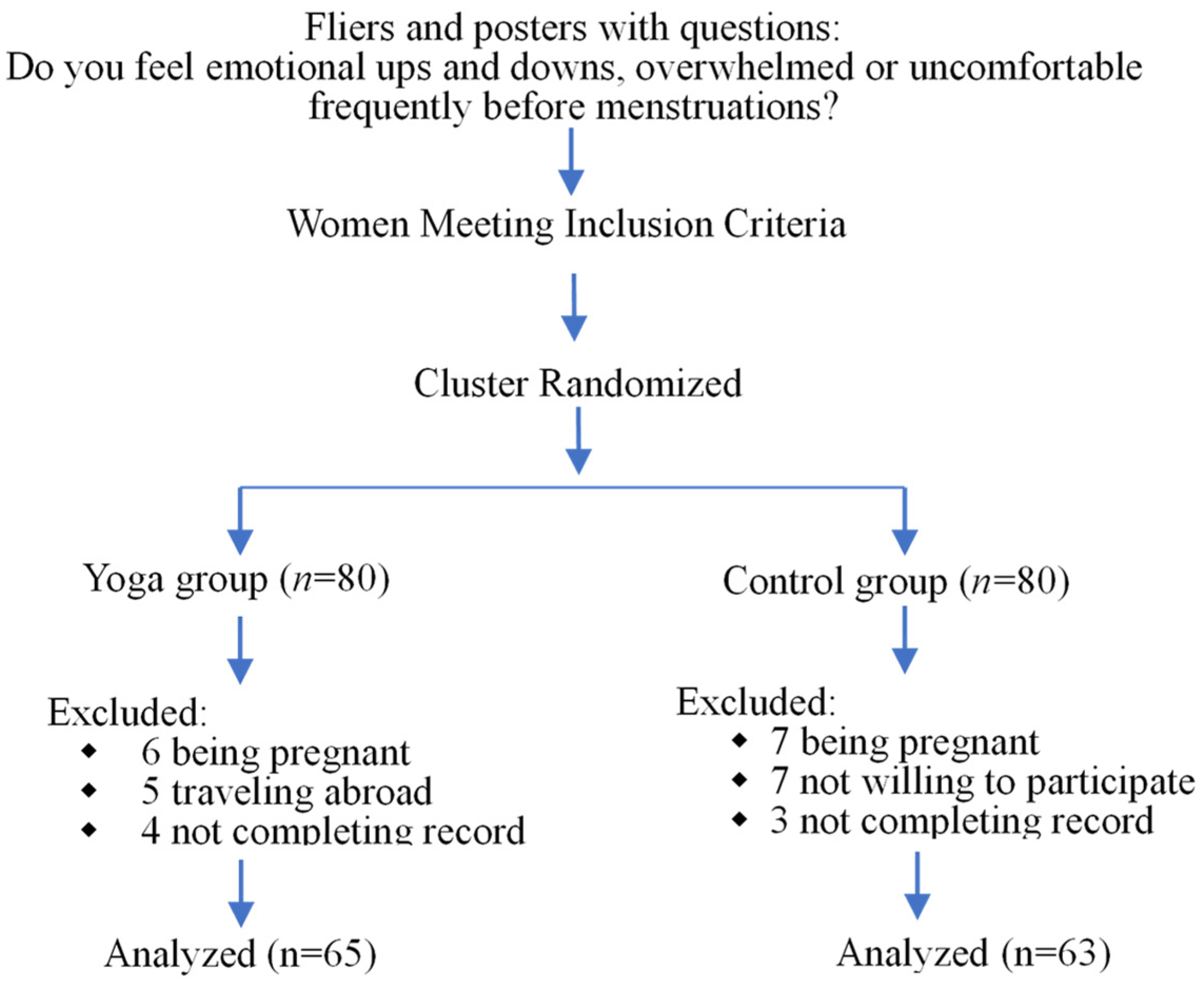
2.1. Study Design and Sample
2.2. Measures
2.3. Intervention
- ◆ Five minutes for warming up from head to belly.
- ◆ Twenty minutes of asana practice, including Surya Namaskar (sun salutation), Supta Baddha Konasana (reclining bound angle pose), Supta Padangusthasana (reclining hand-to-big-toe pose), Upavistha Konasana (seated wide-angle pose), and Psrsva Virasana (side twisted hero pose).
- ◆ Five minutes of Ardha Padmasana (half lotus pose).
2.4. Data Collection and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yonkers, K.A.; O’Brien, P.S.; Eriksson, E. Premenstrual syndrome. Lancet 2008, 371, 1200–1210. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.S.; Ruderman, Y.; Frye, C.; Homanics, G.; Yuan, M. Steroid withdrawal in the mouse results in anxiogenic effects of 3α,5β-THP: A possible model of premenstrual dysphoric disorder. Psychopharmacology 2005, 186, 323–333. [Google Scholar] [CrossRef]
- Björn, I.; Sundström-Poromaa, I.; Bixo, M.; Nyberg, S.; Bäckström, G.; Bäckström, T. Increase of Estrogen Dose Deteriorates Mood during Progestin Phase in Sequential Hormonal Therapy. J. Clin. Endocrinol. Metab. 2003, 88, 2026–2030. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-J.; Park, Y.-J. Menstrual Cycle Characteristics and Premenstrual Syndrome Prevalence Based on the Daily Record of Severity of Problems in Korean Young Adult Women. J. Korean Acad. Nurs. 2020, 50, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Steiner, M. Premenstrual syndrome and premenstrual dysphoric disorder: Guidelines for management. J. Psychiatry Neurosci. 2000, 25, 459–468. [Google Scholar]
- Direkvand-Moghadam, A.; Sayehmiri, K.; Delpisheh, A.; Sattar, K. Epidemiology of premenstrual syndrome (PMS)-A systematic review and meta-analysis study. J. Clin. Diagn. Res. 2014, 8, 106–109. [Google Scholar] [CrossRef]
- Potter, J.; Bouyer, J.; Trussell, J.; Moreau, C. Premenstrual Syndrome Prevalence and Fluctuation over Time: Results from a French Population-Based Survey. J. Women’s Health 2009, 18, 31–39. [Google Scholar] [CrossRef]
- Dennerstein, L.; Lehert, P.; Bäckström, T.C.; Heinemann, K. The effect of premenstrual symptoms on activities of daily life. Fertil. Steril. 2010, 94, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Woods, N.F.; Taylor, D.; Mitchell, E.S.; Lentz, M.J.; Johnson, J.L.; Relyea, M.J. Perimenstrual Symptoms and Health-Seeking Behavior. West. J. Nurs. Res. 1992, 14, 418–443. [Google Scholar] [CrossRef]
- Hardy, C.; Hunter, M.S. Premenstrual Symptoms and Work: Exploring Female Staff Experiences and Recommendations for Workplaces. Int. J. Environ. Res. Public Health 2021, 18, 3647. [Google Scholar] [CrossRef]
- Al-Shahrani, A.M.; Miskeen, E.; Shroff, F.; Elnour, S.; Algahtani, R.; Youssry, I.; Ahmed, S. Premenstrual Syndrome and Its Impact on the Quality of Life of Female Medical Students at Bisha University, Saudi Arabia. J. Multidiscip. Health 2021, 14, 2373–2379. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.A.; Minh, T.D.; Filonenko, A.; Uhl-Hochgräber, K. Explorative Evaluation of the Impact of Premenstrual Disorder on Daily Functioning and Quality of Life. Patient 2010, 3, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Tutty, L.M.; Barry, L.; Nixon, K.L. “Mommy’s Having a Bad Day”: The Impact of Premenstrual Symptoms on Mothering. Women’s Reprod. Health 2021, 9, 81–99. [Google Scholar] [CrossRef]
- Siminiuc, R.; Ţurcanu, D. Impact of nutritional diet therapy on premenstrual syndrome. Front. Nutr. 2023, 10, 1079417. [Google Scholar] [CrossRef] [PubMed]
- Heidari, H.; Amani, R.; Feizi, A.; Askari, G.; Kohan, S.; Tavasoli, P. Vitamin D Supplementation for Premenstrual Syndrome-Related inflammation and antioxidant markers in students with vitamin D deficient: A randomized clinical trial. Sci. Rep. 2019, 9, 14939. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H.; Kim, D.I.; Choi, M.-S. Effects and treatment methods of acupuncture and herbal medicine for premenstrual syndrome/premenstrual dysphoric disorder: Systematic review. BMC Complement. Altern. Med. 2014, 14, 11. [Google Scholar] [CrossRef]
- Panahi, F.; Faramarzi, M. The Effects of Mindfulness-Based Cognitive Therapy on Depression and Anxiety in Women with Premenstrual Syndrome. Depression Res. Treat. 2016, 2016, 9816481. [Google Scholar] [CrossRef]
- Carlini, S.V.; di Scalea, T.L.; McNally, S.T.; Lester, J.; Deligiannidis, K.M. Management of Premenstrual Dysphoric Disorder: A Scoping Review. Int. J. Women’s Health 2022, 14, 1783–1801. [Google Scholar] [CrossRef]
- Asadi, D.M.; Tajrishi, K.Z.; Gharaei, B. Mindfulness Training Intervention with the Persian Version of the Mindfulness Training Mobile App for Premenstrual Syndrome: A Randomized Controlled Trial. Front. Psychiatry 2022, 13, 922360. [Google Scholar] [CrossRef]
- Prior, J.C.; Vigna, Y. Conditioning exercise and premenstrual symptoms. J. Reprod. Med. 1987, 32, 423–428. [Google Scholar]
- Mohebbi Dehnavi, Z.; Jafarnejad, F.; Goghary, S.S. The effect of 8 weeks aerobic exercise on severity of physical symptoms of premenstrual syndrome: A clinical trial study. BMC Women’s Health 2018, 18, 80. [Google Scholar] [CrossRef] [PubMed]
- Yesildere Saglam, H.; Orsal, O. Effect of exercise on premenstrual symptoms: A systematic review. Complement. Ther. Med. 2020, 48, 102272. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.; Jolly, K.; Jones, L.; Matthewman, G.; Zanganeh, M.; Daley, A. Exercise for premenstrual syndrome: A systematic review and meta-analysis of randomised controlled trials. BJGP Open 2020, 4, 20X101032. [Google Scholar] [CrossRef] [PubMed]
- Gannon, L. The potential role of exercise in the alleviation of menstrual disorders and menopausal symptoms: A theoretical syn-thesis of recent research. Women Health 1988, 14, 105–127. [Google Scholar] [CrossRef] [PubMed]
- Prior, J.C.; Vigna, Y.; Alojada, N. Conditioning exercise decreases premenstrual symptoms. A prospective controlled three month trial. Eur. J. Appl. Physiol. Occup. Physiol. 1986, 55, 349–355. [Google Scholar] [CrossRef]
- El-Lithy, A.; El-Mazny, A.; Sabbour, A.; El-Deeb, A. Effect of aerobic exercise on premenstrual symptoms, haematological and hormonal parameters in young women. J. Obstet. Gynaecol. 2015, 35, 389–392. [Google Scholar] [CrossRef]
- Aganoff, J.A.; Boyle, G.J. Aerobic exercise, mood states and menstrual cycle symptoms. J. Psychosom. Res. 1994, 38, 183–192. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists (ACOG). Gynecologic Problems: Premenstrual Syndrome. ACOG. 2015. Available online: http://www.acog.org/Patients/FAQs/Premenstrual-Syndrome-PMS (accessed on 20 October 2015).
- National Health Service (NHS). Premenstrual syndrome (PMS)—Treatment, GOV UK. NHS. 2015. Available online: http://www.nhs.uk/Conditions/Premenstrual-syndrome/Pages/Treatment.aspx (accessed on 15 November 2015).
- Raub, J.A. Psychophysiologic Effects of Hatha Yoga on Musculoskeletal and Cardiopulmonary Function: A Literature Review. J. Altern. Complement. Med. 2002, 8, 797–812. [Google Scholar] [CrossRef]
- Sherman, K.J. Guidelines for Developing Yoga Interventions for Randomized Trials. Evid. Based Complement. Altern. Med. 2012, 2012, 143271. [Google Scholar] [CrossRef]
- Wu, W.-L.; Lin, T.-Y.; Chu, I.-H.; Liang, J.-M. The Acute Effects of Yoga on Cognitive Measures for Women with Premenstrual Syndrome. J. Altern. Complement. Med. 2015, 21, 364–369. [Google Scholar] [CrossRef]
- Wang, W.-L.; Chen, K.-H.; Pan, Y.-C.; Yang, S.-N.; Chan, Y.-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry 2020, 20, 195. [Google Scholar] [CrossRef] [PubMed]
- Woodyard, C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int. J. Yoga 2011, 4, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Ciezar-Andersen, S.D.; Hayden, K.A.; King-Shier, K.M. A systematic review of yoga interventions for helping health professionals and students. Complement. Ther. Med. 2021, 58, 102704. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lauche, R.; Dobos, G. Characteristics of randomized controlled trials of yoga: A bibliometric analysis. BMC Complement. Altern. Med. 2014, 14, 328. [Google Scholar] [CrossRef]
- Moran, S.; Jäger, N.; Schnädelbach, H.; Glover, K. ExoPranayama: A biofeedback-driven actuated environment for supporting yoga breathing practices. Pers. Ubiquitous Comput. 2016, 20, 261–275. [Google Scholar] [CrossRef]
- Sharma, V.K.; Trakroo, M.; Subramaniam, V.; Sahai, A.; Bhavanani, A.B.; Rajajeyakumar, M. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int. J. Yoga 2013, 6, 104–110. [Google Scholar] [CrossRef]
- Ma, X.; Yue, Z.-Q.; Gong, Z.-Q.; Zhang, H.; Duan, N.-Y.; Shi, Y.-T.; Wei, G.-X.; Li, Y.-F. The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front. Psychol. 2017, 8, 874. [Google Scholar] [CrossRef]
- Hamasaki, H. Effects of Diaphragmatic Breathing on Health: A Narrative Review. Medicines 2020, 7, 65. [Google Scholar] [CrossRef]
- Desai, R.; Tailor, A.; Bhatt, T. Effects of yoga on brain waves and structural activation: A review. Complement. Ther. Clin. Pr. 2015, 21, 112–118. [Google Scholar] [CrossRef]
- Yamamoto-Morimoto, K.; Horibe, S.; Takao, R.; Anami, K. Positive Effects of Yoga on Physical and Respiratory Functions in Healthy Inactive Middle-Aged People. Int. J. Yoga 2019, 12, 62–67. [Google Scholar] [CrossRef]
- Srinivasan, T. Dynamic and static asana practices. Int. J. Yoga 2016, 9, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Field, T. Yoga clinical research review. Complement. Ther. Clin. Pract. 2011, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cahn, B.R.; Goodman, M.S.; Peterson, C.T.; Maturi, R.; Mills, P.J. Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Front. Hum. Neurosci. 2017, 11, 315. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, M.; Jain, A.; Agarwal, P.; Joshi, S.D.; Parvez, S. Role of Yoga and Meditation as Complimentary Therapeutic Regime for Stress-Related Neuropsychiatric Disorders: Utilization of Brain Waves Activity as Novel Tool. J. Evid.-Based Integr. Med. 2020, 25, 2515690X20949451. [Google Scholar] [CrossRef]
- Tsai, S.-Y. Effect of Yoga Exercise on Premenstrual Symptoms among Female Employees in Taiwan. Int. J. Environ. Res. Public Health 2016, 13, 721. [Google Scholar] [CrossRef]
- Borenstein, J.E.; Dean, B.B.; Yonkers, K.A.; Endicott, J. Using the Daily Record of Severity of Problems as a Screening Instrument for Premenstrual Syndrome. Obstet. Gynecol. 2007, 109, 1068–1075. [Google Scholar] [CrossRef]
- Wu, L.; He, Z.; Zhao, H.; Ma, D.; Zhang, S.; Deng, H.; Liang, T. Chinese version of Daily Record of Severity of Problems: Reliability and validity. J. Adv. Nurs. 2012, 69, 449–456. [Google Scholar] [CrossRef]
- Zhang, H.; Zhu, M.; Song, Y.; Kong, M. Baduanjin exercise improved premenstrual syndrome symptoms in Macau women. J. Tradit. Chin. Med. 2014, 34, 460–464. [Google Scholar] [CrossRef]
- Endicott, J.; Nee, J.; Harrison, W. Daily Record of Severity of Problems (DRSP): Reliability and validity. Arch. Women’s Ment. Health 2005, 9, 41–49. [Google Scholar] [CrossRef]
- Long, R.; Macivor, C. The Key Muscles of Yoga: Scientific Keys; BandhaYoga: Baldwinsville, NY, USA, 2009; Volume 1. [Google Scholar]
- Long, R.; Macivor, C. The Key Poses of Yoga: Scientific Keys; BandhaYoga: Baldwinsville, NY, USA, 2009; Volume 2. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 21.0; IBM Corp.: Armonk, NY, USA, 2012. [Google Scholar]
- Ross, A.; Thomas, S. The Health Benefits of Yoga and Exercise: A Review of Comparison Studies. J. Altern. Complement. Med. 2010, 16, 3–12. [Google Scholar] [CrossRef]
- Steege, J.F.; Blumenthal, J.A. The effects of aerobic exercise on premenstrual symptoms in middle-aged women: A preliminary study. J. Psychosom. Res. 1993, 37, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Dutta, A.; Aruchunan, M.; Mukherjee, A.; Metri, K.G.; Ghosh, K.; Basu-Ray, I. A Comprehensive Review of Yoga Research in 2020. J. Integr. Complement. Med. 2022, 28, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Nyer, M.; Hopkins, L.B.; Farabaugh, A.; Nauphal, M.; Parkin, S.; McKee, M.M.; Miller, K.K.; Streeter, C.; Uebelacker, L.A.; Fava, M.; et al. Community-Delivered Heated Hatha Yoga as a Treatment for Depressive Symptoms: An Uncontrolled Pilot Study. J. Altern. Complement. Med. 2019, 25, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Ghaffarilaleh, G.; Ghaffarilaleh, V.; Sanamno, Z.; Kamalifard, M. Yoga positively affected depression and blood pressure in women with premenstrual syndrome in a randomized controlled clinical trial. Complement. Ther. Clin. Pract. 2018, 34, 87–92. [Google Scholar] [CrossRef]
- Simsek Kucukkelepce, D.; Unver, H.; Nacar, G.; Tashan, S.T. The effects of acupressure and yoga for coping with premenstrual syndromes on premenstrual symptoms and quality of life. Complement. Ther. Clin. Pract. 2020, 42, 101282. [Google Scholar] [CrossRef] [PubMed]
- Kanojia, S.; Sharma, V.K.; Gandhi, A.; Kapoor, R.; Kukreja, A.; Subramanian, S.K. Effect of Yoga on Autonomic Functions and Psychological Status During Both Phases of Menstrual Cycle in Young Healthy Females. J. Clin. Diagn. Res. 2013, 7, 2133–2139. [Google Scholar] [CrossRef]
- Ghaffarilaleh, G.; Ghaffarilaleh, V.; Sanamno, Z.; Kamalifard, M. Yoga improves anxiety and vital signs of women with pre-menstrual syndrome. J. Dep. Anxiety 2019, 8, 342. [Google Scholar] [CrossRef]
- GhaffariLaleh, G.; Ghaffarilaleh, V.; Sanamno, Z.; Kamalifard, M.; Alibaf, L. Effects of Yoga on Quality of Sleep of Women With Premenstrual Syndrome. Altern Health Med. 2019, 25, 40–47. [Google Scholar]
- Taspinar, B.; Aslan, U.B.; Agbuga, B.; Taspinar, F. A comparison of the effects of hatha yoga and resistance exercise on mental health and well-being in sedentary adults: A pilot study. Complement. Ther. Med. 2014, 22, 433–440. [Google Scholar] [CrossRef]
- Rakhshani, A.; Maharana, S.; Raghuram, N.; Nagendra, H.R.; Venkatram, P. Effects of integrated yoga on quality of life and interpersonal relationship of pregnant women. Qual. Life Res. 2010, 19, 1447–1455. [Google Scholar] [CrossRef]
- Yilmaz-Akyuz, E.; Aydin-Kartal, Y. The effect of diet and aerobic exercise on Premenstrual Syndrome: Randomized controlled trial. Rev. De Nutr. 2019, 32, e180246. [Google Scholar] [CrossRef]
- Ravichandran, H.; Janakiraman, B. Effect of Aerobic Exercises in Improving Premenstrual Symptoms Among Healthy Women: A Systematic Review of Randomized Controlled Trials. Int. J. Women’s Health 2022, 14, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Çitil, E.T.; Kaya, N. Effect of pilates exercises on premenstrual syndrome symptoms: A quasi-experimental study. Complement. Ther. Med. 2020, 57, 102623. [Google Scholar] [CrossRef] [PubMed]
- Yonkers, K.A.; Cameron, B.; Gueorguieva, R.; Altemus, M.; Kornstein, S.G. The Influence of Cyclic Hormonal Contraception on Expression of Premenstrual Syndrome. J. Women’s Health 2017, 26, 321–328. [Google Scholar] [CrossRef]
- Sherman, K.J.; Cherkin, D.C.; Erro, J.; Miglioretti, D.L.; Deyo, R.A. Comparing Yoga, Exercise, and a Self-Care Book for Chronic Low Back Pain: A randomized, controlled trial. Ann. Intern. Med. 2005, 143, 849–856. [Google Scholar] [CrossRef]
- Halpern, J.; Cohen, M.; Kennedy, G.; Reece, J.; Cahan, C.; Baharav, A. Yoga for improving sleep quality and quality of life for older adults. Altern. Ther. Health Med. 2014, 20, 37–46. [Google Scholar]
- Ohlsson Nevo, E.; Arvidsson-Lindvall, M.; Börjeson, S.H.; Hagberg, L.; Hörnqvist, E.H.; Valachis, A.; Wickberg, Å.; Duberg, A. Digitally distributed Yoga Intervention in Breast Cancer Rehabilitation (DigiYoga CaRe): Protocol for a randomised controlled trial. BMJ Open 2022, 12, e065939. [Google Scholar] [CrossRef]
- Oates, J. The Effect of Yoga on Menstrual Disorders: A Systematic Review. J. Altern. Complement. Med. 2017, 23, 407–417. [Google Scholar] [CrossRef]
- Ikeda, Y.; Egawa, M.; Okamoto, K.; Mandai, M.; Takahashi, Y.; Nakayama, T. The reliability and validity of the Japanese version of the Daily Record of Severity of Problems (J-DRSP) and De-velopment of a Short-Form version (J-DRSP (SF)) to assess symptoms of premenstrual syndrome among Japanese women. BioPsychoSocial Med. 2021, 15, 6. [Google Scholar] [CrossRef]
| Characteristics | Yoga Group (n = 65) | Control Group (n = 63) | t/χ2 | p | ||
|---|---|---|---|---|---|---|
| M ± SD/n (%) | M ± SD/n (%) | |||||
| Physical exercise (exercise habit) | 0.76 | 0.38 | ||||
| Yes | 27 | (41.54) | 31 | (49.21) | ||
| No | 38 | (58.46) | 32 | (50.79) | ||
| Days of bleeding during menses | 5.55 | ±1.24 | 5.62 | ±1.17 | −0.31 | 0.76 |
| Menstruation amount | 1.48 | 0.48 | ||||
| Little | 0 | (0.00) | 1 | (1.59) | ||
| Moderate | 59 | (90.77) | 54 | (85.71) | ||
| Heavy | 6 | (9.23) | 8 | (12.70) | ||
| Pre-menstrual pain | 0.47 | 0.49 | ||||
| Yes | 45 | (69.23) | 40 | (63.49) | ||
| No | 20 | (30.77) | 23 | (36.51) | ||
| Menstrual pain | 2.70 | 0.44 | ||||
| No | 14 | (21.54) | 15 | (23.81) | ||
| Rarely | 15 | (23.08) | 14 | (22.22) | ||
| Sometimes | 21 | (32.31) | 26 | (41.27) | ||
| Regularly | 15 | (23.08) | 8 | (12.70) | ||
| Variable | Baseline | p | After Intervention | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yoga (n = 65) | Control (n = 63) | Yoga (n = 65) | Control (n = 63) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Depressive symptoms | 52.90 | 22.48 | 46.90 | 17.56 | 0.23 | 39.49 | 7.90 | 49.17 | 14.56 | 0.00 *** |
| Depressed/sad/blue | 9.20 | 4.68 | 7.55 | 4.37 | 0.13 | 6.49 | 2.01 | 7.11 | 3.90 | 0.26 |
| Hopeless | 6.38 | 3.23 | 6.00 | 2.49 | 0.59 | 5.48 | 1.00 | 5.94 | 2.24 | 0.14 |
| Worthless/guilty | 6.73 | 3.69 | 6.10 | 2.30 | 0.41 | 5.52 | 1.03 | 6.11 | 2.66 | 0.11 |
| Slept more | 11.35 | 5.97 | 10.77 | 5.62 | 0.68 | 8.25 | 3.29 | 11.70 | 4.51 | 0.00 *** |
| Trouble sleeping | 10.13 | 6.03 | 7.94 | 4.43 | 0.09 | 6.97 | 2.77 | 8.16 | 4.31 | 0.07 |
| Overwhelmed, can’t cope | 9.23 | 4.81 | 8.48 | 3.55 | 0.47 | 6.78 | 2.31 | 10.16 | 4.00 | 0.00 *** |
| Physical symptoms | 43.83 | 20.98 | 39.97 | 14.65 | 0.39 | 30.37 | 8.62 | 40.84 | 11.32 | 0.00 *** |
| Breast tenderness | 11.60 | 6.57 | 10.97 | 4.51 | 0.65 | 7.82 | 3.05 | 11.60 | 4.77 | 0.00 *** |
| Breast swelling/“bloated” | 12.15 | 6.90 | 11.87 | 4.30 | 0.84 | 8.14 | 3.05 | 12.40 | 4.52 | 0.00 *** |
| Headache | 9.70 | 5.92 | 8.71 | 4.27 | 0.43 | 6.55 | 1.86 | 8.43 | 2.73 | 0.00 *** |
| Joint or muscle pain | 10.38 | 5.77 | 8.45 | 4.49 | 0.13 | 7.86 | 2.87 | 8.41 | 3.80 | 0.36 |
| Anger/irritability | 15.95 | 6.98 | 15.23 | 4.72 | 0.62 | 12.52 | 3.01 | 16.22 | 5.44 | 0.00 *** |
| Angry, irritable | 8.70 | 4.29 | 8.23 | 3.01 | 0.60 | 6.68 | 2.31 | 8.98 | 3.29 | 0.00 *** |
| Conflicts with people | 7.33 | 3.50 | 7.00 | 2.61 | 0.64 | 5.85 | 1.19 | 7.24 | 3.00 | 0.00 *** |
| Other disturbances | ||||||||||
| Anxiety | 9.05 | 3.88 | 7.52 | 3.37 | 0.08 | 6.60 | 1.77 | 8.49 | 3.20 | 0.00 *** |
| Mood swings | 8.93 | 4.20 | 7.81 | 3.25 | 0.22 | 6.31 | 1.82 | 8.46 | 3.01 | 0.00 *** |
| Sensitive to rejection | 7.53 | 3.69 | 6.84 | 3.18 | 0.41 | 5.98 | 1.69 | 7.40 | 2.75 | 0.00 *** |
| Less interest | 8.92 | 4.34 | 7.84 | 3.06 | 0.23 | 6.97 | 1.88 | 8.87 | 3.21 | 0.00 *** |
| Difficulty concentrating | 9.28 | 4.56 | 7.87 | 3.17 | 0.15 | 7.08 | 2.22 | 8.98 | 3.18 | 0.00 *** |
| Fatigue | 11.95 | 6.11 | 11.32 | 3.93 | 0.62 | 8.03 | 3.13 | 12.54 | 3.95 | 0.00 *** |
| Increased appetite | 9.43 | 5.40 | 9.16 | 3.93 | 0.82 | 8.35 | 3.26 | 11.03 | 4.66 | 0.00 *** |
| Crave specific foods | 9.23 | 5.48 | 9.68 | 4.81 | 0.72 | 7.75 | 3.17 | 10.83 | 4.67 | 0.00 *** |
| Out of control | 8.23 | 3.94 | 8.03 | 3.19 | 0.83 | 6.38 | 1.35 | 10.17 | 3.56 | 0.00 *** |
| Impairment in functioning caused by the symptoms | ||||||||||
| Impaired work/daily routine | 10.48 | 5.75 | 8.68 | 3.54 | 0.13 | 7.11 | 2.48 | 9.57 | 3.49 | 0.00 *** |
| Impaired hobbies/social | 9.83 | 5.02 | 8.48 | 3.90 | 0.22 | 7.14 | 2.74 | 8.84 | 3.62 | 0.00 *** |
| Impaired relationships | 8.23 | 3.73 | 8.19 | 3.60 | 0.97 | 6.08 | 1.98 | 8.46 | 2.89 | 0.00 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, H.-C.; Cheng, Y.-C.; Yang, C.-H.; Tzeng, Y.-L.; Chen, C.-H. Effects of Yoga for Coping with Premenstrual Symptoms in Taiwan—A Cluster Randomized Study. Healthcare 2023, 11, 1193. https://doi.org/10.3390/healthcare11081193
Chang H-C, Cheng Y-C, Yang C-H, Tzeng Y-L, Chen C-H. Effects of Yoga for Coping with Premenstrual Symptoms in Taiwan—A Cluster Randomized Study. Healthcare. 2023; 11(8):1193. https://doi.org/10.3390/healthcare11081193
Chicago/Turabian StyleChang, Hsing-Chi, Yi-Chuan Cheng, Chi-Hsuan Yang, Ya-Ling Tzeng, and Chung-Hey Chen. 2023. "Effects of Yoga for Coping with Premenstrual Symptoms in Taiwan—A Cluster Randomized Study" Healthcare 11, no. 8: 1193. https://doi.org/10.3390/healthcare11081193
APA StyleChang, H.-C., Cheng, Y.-C., Yang, C.-H., Tzeng, Y.-L., & Chen, C.-H. (2023). Effects of Yoga for Coping with Premenstrual Symptoms in Taiwan—A Cluster Randomized Study. Healthcare, 11(8), 1193. https://doi.org/10.3390/healthcare11081193







