Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review
Abstract
1. Introduction
2. Methodology
2.1. Study Design
2.2. Sources of Information and Search Strategies
- Population: patients older than 18 years of age and with inflammation or pain lasting for more than 3 months.
- Intervention: reduction in the symptomology of pain or inflammation after a PBM intervention.
- Comparison: the use or not of PBM.
- Results: effectiveness of the PBM application strategies on chronic pain and inflammation.
2.2.1. PubMed
- Text accessibility: open-access or accessible to the University of Granada, Spain.
- Type of articles: RCTs and observational studies.
- Date of publication: 2017–2022.
- Species: human.
- Language: English.
2.2.2. ProQuest
- Text accessibility: open-access or accessible to the University of Granada, Spain.
- Type of articles: RCTs and observational studies.
- Date of publication: 2017–2022.
- Language: English.
2.2.3. Scopus
- Text accessibility: open-access or accessible to the University of Granada, Spain.
- Type of articles: articles.
- Subject: medicine and health professions.
- Date of publication: 2017–2022.
2.2.4. Web of Science
- Text accessibility: open-access or accessible to the University of Granada, Spain.
- Type of articles: articles (RCTs).
- Subject: medicine and health professions.
- Date of publication: 2017–2022.
2.2.5. PEDro
- Text accessibility: open-access or accessible to the University of Granada, Spain.
- Subject: chronic pain.
- Method: RCTs.
- Date of publication: 2017–2022.
2.3. Study Selection
2.3.1. Criteria for Inclusion
- Publication between January 2017 and May 2022.
- International publication in English and peer-reviewed.
- Designed as RCTs.
- Access to the complete text available.
- Conducted in humans over the age of 18.
- Suffer from acute pain or chronic pain.
- Suffer from some type of pathology that causes chronic pain.
- Suffer from edema/inflammation.
2.3.2. Exclusion Criteria
- Not meeting the inclusion criteria.
- Repeated in the databases.
- Does not assess chronic pain, inflammation or pathology or symptom prevention.
- Lack of PBMT implementation in people with pain or inflammation.
- No results were shown or no interpretation of the data.
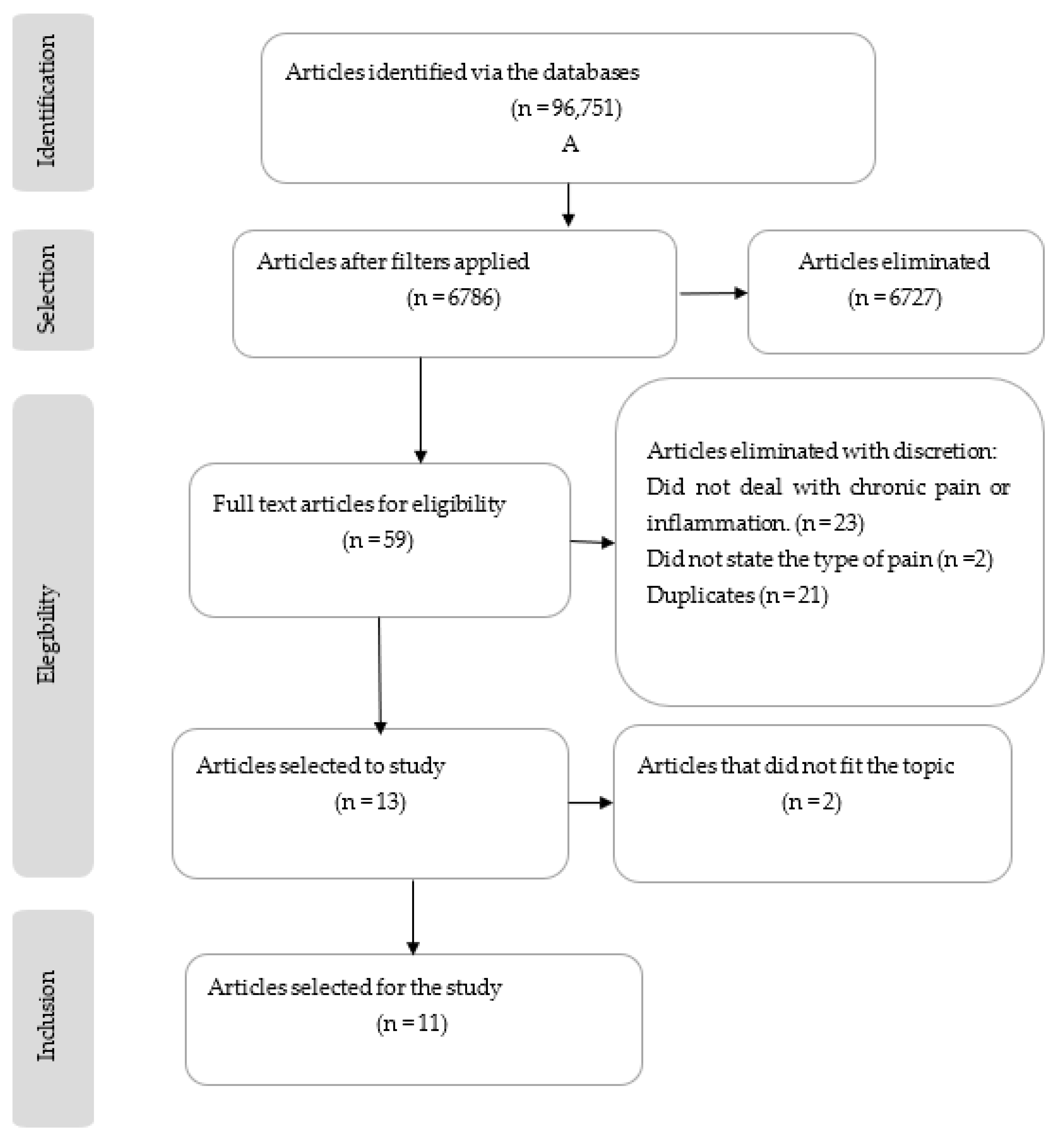
2.4. Article Selection
2.5. Methodological Quality Assessment of the RCTs
2.6. RCTs Qualitative Synthesis
2.7. Management of the Identified Literature
3. Results
3.1. Study Selection
3.2. Methodological Quality Evaluation
3.3. Study Characteristics
3.4. Methodological Quality of the Collected Literature
3.5. Effects of Photobiomodulation Therapy on Health Improvement and Chronic Pain
3.5.1. Chronic Pain
3.5.2. Inflammation
3.5.3. Acute Pain
3.6. Questionnaires and Scales Used in the Articles
4. Discussion
4.1. Chronic Nonspecific Low Back Pain
4.2. Fibromyalgia
4.3. Temporomandibular Pain and Dysfunction
4.4. Oral Pain and Inflammation
4.5. Post-Surgery Pain and Swelling
4.6. Strengths and Weaknesses of the Study
4.7. Prospective
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salehpour, F.; Mahmoudi, J.; Kamari, F.; Sadigh-Eteghad, S.; Rasta, S.H.; Hamblin, M.R. Brain Photobiomodulation Therapy: A Narrative Review. Mol. Neurobiol. 2018, 55, 6601–6636. [Google Scholar] [CrossRef]
- Karu, T.I.; Pyatibrat, L.V.; Kolyakov, S.F.; Afanasyeva, N.I. Absorption measurements of a cell monolayer relevant to phototherapy: Reduction of cytochrome c oxidase under near IR radiation. J. Photochem. Photobiol. B Biol. 2005, 81, 98–106. [Google Scholar] [CrossRef]
- Yeh, S.W.; Hong, C.H.; Shih, M.C.; Tam, K.W.; Huang, Y.H.; Kuan, Y.C. Low-level laser therapy for fibromyalgia: A systematic review and meta-analysis. Pain Physician 2019, 22, 241–254. [Google Scholar] [PubMed]
- Gur, A.; Karakoc, M.; Cevik, R.; Nas, K.; Sarac, A.J.; Karakoc, M. Efficacy of low power laser therapy and exercise on pain and functions in chronic low back pain. Lasers Surg. Med. 2003, 32, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Honda, Y.; Sakamoto, J.; Hamaue, Y.; Kataoka, H.; Kondo, Y.; Sasabe, R.; Goto, K.; Fukushima, T.; Oga, S.; Sasaki, R.; et al. Effects of Physical-Agent Pain Relief Modalities for Fibromyalgia Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Res. Manag. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Ledesma, S.; Carroll, J.; Burton, P.; Ana, G.-M. Short-Term Effects of Whole-Body Photobiomodulation on Pain, Quality of Life and Psychological Factors in a Population Suffering from Fibromyalgia: A Triple-Blinded Randomised Clinical Trial. Pain Ther. 2022, 12, 225–239. [Google Scholar] [CrossRef]
- Navarro-Ledesma, S.; Carroll, J.; González-Muñoz, A.; Pruimboom, L.; Burton, P. Changes in Circadian Variations in Blood Pressure, Pain Pressure Threshold and the Elasticity of Tissue after a Whole-Body Photobiomodulation Treatment in Patients with Fibromyalgia: A Tripled-Blinded Randomized Clinical Trial. Biomedicines 2022, 10, 2678. [Google Scholar] [CrossRef]
- Wickenheisser, V.A.; Zywot, E.M.; Rabjohns, E.M.; Lee, H.H.; Lawrence, D.S.; Tarrant, T.K. Laser Light Therapy in Inflammatory, Musculoskeletal, and Autoimmune Disease. Curr. Allergy Asthma Rep. 2019, 19, 37. [Google Scholar] [CrossRef] [PubMed]
- Schwan, J.; Sclafani, J.; Tawfik, V.L. Chronic Pain Management in the Elderly. Anesthesiol. Clin. 2019, 37, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef]
- Domenichiello, A.F.; Ramsden, C.E. The silent epidemic of chronic pain in older adults. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2019, 93, 284–290. [Google Scholar] [CrossRef]
- Kaushik, A.S.; Strath, L.J.; Sorge, R.E. Dietary Interventions for Treatment of Chronic Pain: Oxidative Stress and Inflammation. Pain Ther. 2020, 9, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Bosch-Capblanch, X.; Lavis, J.N.; Lewin, S.; Atun, R.; Røttingen, J.-A.; Dröschel, D.; Beck, L.; Abalos, E.; El-Jardali, F.; Gilson, L.; et al. Policy Forum Guidance for Evidence-Informed Policies about Health Systems: Rationale for and Challenges of Guidance Development. PLoS Med. 2012, 9, e1001185. [Google Scholar] [CrossRef] [PubMed]
- Clijsen, R.; Brunner, A.; Barbero, M.; Clarys, P.; Taeymans, J. Effects of low-level laser therapy on pain in patients with musculoskeletal disorders: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2017, 53, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Nunes, E.C.; Herkrath, F.J.; Suzuki, E.H.; Júnior, E.C.G.; Marques, A.A.F.; Júnior, E.C.S. Comparison of the effect of photobiomodulation therapy and Ibuprofen on postoperative pain after endodontic treatment: Randomized, controlled, clinical study. Lasers Med Sci. 2019, 35, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Langella, L.G.; Casalechi, H.L.; Tomazoni, S.S.; Johnson, D.S.; Albertini, R.; Pallotta, R.C.; Marcos, R.L.; Carvalho, P.D.T.C.D.; Leal-Junior, E.C.P. Photobiomodulation therapy (PBMT) on acute pain and inflammation in patients who underwent total hip arthroplasty-a randomized, triple-blind, placebo-controlled clinical trial. Lasers Med Sci. 2018, 33, 1933–1940. [Google Scholar] [CrossRef]
- Paolillo, F.R.; Paolillo, A.R.; João, J.P.; Frascá, D.; Duchêne, M.; João, H.A.; Bagnato, V.S. Ultrasound plus low-level laser therapy for knee osteoarthritis rehabilitation: A randomized, placebo-controlled trial. Rheumatol. Int. 2018, 38, 785–793. [Google Scholar] [CrossRef]
- Kholoosy, L.; Elyaspour, D.; Akhgari, M.R.; Razzaghi, Z.; Khodamardi, Z.; Bayat, M. Evaluation of the therapeutic effect of low level laser in controlling low back pain: A randomized controlled trial. J. Lasers Med. Sci. 2020, 11, 120–125. [Google Scholar] [CrossRef]
- da Silva, M.M.; Albertini, R.; Carvalho, P.D.T.C.D.; Leal-Junior, E.C.P.; Bussadori, S.K.; Vieira, S.S.; Bocalini, D.S.; de Oliveira, L.V.F.; Grandinetti, V.; Silva, J.A.; et al. Randomized, blinded, controlled trial on effectiveness of photobiomodulation therapy and exercise training in the fibromyalgia treatment. Lasers Med Sci. 2017, 33, 343–351. [Google Scholar] [CrossRef]
- de Souza, R.-C.-V.; de Sousa, E.-T.; Oliveira Scudine, K.-G.; Meira, U.-M.; de Oliveira Silva, E.-D.; Gomes, A.-C.-A.; Limeira-Junior, F.-d.A. Low-level laser therapy and anesthetic infiltration for orofacial pain in patients with fibromyalgia: A randomized clinical trial. Med. Oral Patol. Oral Y Cir. Bucal 2018, 23, e65–e71. [Google Scholar] [CrossRef] [PubMed]
- Tomazoni, S.S.; Costa, L.O.P.; Joensen, J.; Stausholm, M.B.; Naterstad, I.F.; Ernberg, M.; Leal-Junior, E.C.P.; Bjordal, J.M. Photobiomodulation Therapy is Able to Modulate PGE 2 Levels in Patients with Chronic Non-Specific Low Back Pain: A Randomized Placebo-Controlled Trial. Lasers Surg. Med. 2020, 53, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; McGrath, C.; Gu, M.; Jin, L.; Zhang, C.; Sum, F.H.K.M.H.; Wong, K.W.F.; Chau, A.C.M.; Yang, Y. Low-level laser-aided orthodontic treatment of periodontally compromised patients: A randomised controlled trial. Lasers Med Sci. 2019, 35, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Taradaj, J.; Rajfur, K.; Rajfur, J.; Ptaszkowski, K.; Ptaszkowska, L.; Sopel, M.; Rosińczuk, J.; Dymarek, R. Effect of laser treatment on postural control parameters in patients with chronic nonspecific low back pain: A randomized placebo-controlled trial. Braz. J. Med. Biol. Res. 2019, 52. [Google Scholar] [CrossRef]
- Liao, F.-Y.; Lin, C.-L.; Lo, S.-F.; Chang, C.-C.; Liao, W.-Y.; Chou, L.-W. Efficacy of Acupoints Dual-Frequency Low-Level Laser Therapy on Knee Osteoarthritis. Evid.-Based Complement. Altern. Med. 2020, 2020, 1–7. [Google Scholar] [CrossRef]
- Brochado, F.T.; De Jesus, L.H.; Carrard, V.C.; Freddo, A.L.; Chaves, K.D.; Martins, M.D. Comparative effectiveness of photobiomodulation and manual therapy alone or combined in TMD patients: A randomized clinical trial. Braz. Oral Res. 2018, 32, e50. [Google Scholar] [CrossRef]
- Sung, Y.-T.; Wu, J.-S. The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement. Behav. Res. Methods 2018, 50, 1694–1715. [Google Scholar] [CrossRef]
- Van Wilgen, C.P.; Vuijk, P.; Van Ittersum, M.W.; Nijs, J. Not throwing out the baby with the bathwater: Lessons from the Fibromyalgia Impact Questionnaire. Clin. Rheumatol. 2012, 32, 333–339. [Google Scholar] [CrossRef]
- Winocur, E.; Steinkeller-Dekel, M.; Reiter, S.; Eli, I. A retrospective analysis of temporomandibular findings among Israeli-born patients based on the RDC⁄TMD. J. Oral Rehabil. 2009, 36, 11–17. [Google Scholar] [CrossRef]
- Madan, J.; Khan, K.A.; Petrou, S.; Lamb, S.E. Can Mapping Algorithms Based on Raw Scores Overestimate QALYs Gained by Treatment? A Comparison of Mappings between the Roland-Morris Disability Questionnaire and the EQ-5D-3L Based on Raw and Differenced Score Data. Pharmacoeconomics 2017, 35, 549–559. [Google Scholar] [CrossRef]
- Primorac, D.; Molnar, V.; Rod, E.; Jeleč, Ž.; Čukelj, F.; Matišić, V.; Vrdoljak, T.; Hudetz, D.; Hajsok, H.; Borić, I. Knee Osteoarthritis: A Review of Pathogenesis and State-Of-The-Art Non-Operative Therapeutic Considerations. Genes 2020, 11, 854. [Google Scholar] [CrossRef]
- Oehlert, M.E.; Nelson, K.G.; King, N.; Reis, D.J.; Sumerall, S.; Neal, C.; Henry, P. Measurement-based care: Use of the beck anxiety inventory (BAI) in a veteran population. Psychol. Serv. 2020, 17, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.S.; Tomazoni, S.S.; Vanin, A.A.; Araujo, A.C.; De Medeiros, F.C.; Oshima, R.K.A.; Costa, L.O.P.; Costa, L.D.C.M. Management of Acute Low Back Pain in Emergency Departments in São Paulo, Brazil: A Descriptive, Cross-Sectional Analysis of Baseline Data from a Prospective Cohort Study. BMJ Open 2022, 12. [Google Scholar] [CrossRef]
- Thomsen, M.G.; Latifi, R.; Kallemose, T.; Barfod, K.W.; Husted, H.; Troelsen, A. Good validity and reliability of the forgotten joint score in evaluating the outcome of total knee arthroplasty. Acta Orthop. 2016, 87, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Ledesma, S.; Gonzalez-Muñoz, A.; Carroll, J.; Burton, P. Short- and Long-Term Effects of Whole-Body Photobiomodulation on Pain, Functionality, Tissue Quality, Central Sensitisation and Psychological Factors in a Population Suffering from Fibromyalgia: Protocol for a Triple-Blinded Randomised Clinical Trial. Ther. Adv. Chronic. Dis. 2022, 13, 204062232210780. [Google Scholar] [CrossRef]
- Mishra, R.; Drangsholt, M.T.; Leresche, L.; Kassebaum, N. Global Burden of Temporomandibular Disorder (Tmd): A Systematic Review of Tmd Prevalence and Incidence (1990–January 2019). 1990. Available online: https://digital.lib.washington.edu/researchworks/bitstream/handle/1773/45167/Mishra_washington_0250O_20844.pdf?sequence=1&isAllowed=y (accessed on 15 March 2023).
- Matsuda, M.; Huh, Y.; Ji, R.-R. Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. J. Anesth. 2018, 33, 131–139. [Google Scholar] [CrossRef]
- González-Muñoz, A.; Perez-Montilla, J.J.; Cuevas-Cervera, M.; Aguilar-García, M.; Aguilar-Nuñez, D.; Hamed-Hamed, D.; Pruimboom, L.; Navarro-Ledesma, S. Effects of Photobiomodulation in Sports Performance: A Literature Review. Appl. Sci. 2023, 13, 3147. [Google Scholar] [CrossRef]
| PubMed |
|
| ProQuest |
|
| Scopus |
|
| Web of Science |
|
| PEDro |
|
| Author, Year | 1 * | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eduardo C. et al., 2020 [16] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 9/10 Excellent |
| Luciana GL. et al., 2018 [17] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/10 Excellent |
| Fernanda R. et al., 2018 [18] | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 6/10 Good |
| Leyla K. et al., 2020 [19] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 6/10 Good |
| Mariana M. et al., 2018 [20] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/10 Excellent |
| De Souza R. et al., 2018 [21] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6/10 Good |
| Shaiane S. et al., 2021 [22] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 9/10 Excellent |
| Chong R. et al., 2020 [23] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/10 Excellent |
| Taradaj J. et al., 2019 [24] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9/10 Excellent |
| Fang-Yin L. et al., 2020 [25] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 8/10 Good |
| Author, Year | 2 | 3 | 5 | 6 | 7 | 8 | 9 | IVS |
|---|---|---|---|---|---|---|---|---|
| Eduardo C. et al., 2020 [16] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 6/7 High |
| Luciana GL. et al., 2018 [17] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7/7 High |
| Fernanda R. et al., 2018 [18] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 3/7 Limited |
| LeylaK. et al., 2020 [19] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 3/7 Limited |
| Mariana M. et al., 2018 [20] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7/7 High |
| De Souza R. et al., 2018 [21] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 4/7 Limited |
| Shaiane S. et al., 2021 [22] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 6/7 High |
| Chong R. et al., 2020 [23] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7/7 High |
| Taradaj J. et al., 2019 [24] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 6/7 High |
| Fang-Yin L. et al., 2020 [25] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 5/7 High |
| Fernanda T. et al., 2018 [26] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 4/7 Limited |
| Author, Year | Type of Study | Experimental Group | Control Group | Interventions | Variables | Results |
|---|---|---|---|---|---|---|
| Nunes EC. et al., 2020 [16] | Randomized Clinical Trial | 35 people with post endodontic surgery pain. Men: 16 Women: 19 Age range: 20.8–37.2 Chronic illness: No Post operative pain: 1.3–2.9 Treatment time: 39.2–54.2 | 35 people with post endodontic surgery pain. Men: 15 Women: 20 Age range:18.4–42.2 Chronic illness: No Post operative pain: 1.4–3.2 Treatment time: 49.9–39.3 | EG: Received PBMT at 4 points (attached to mucosa) after endodontic treatment. CG: Received endodontic treatment and prescribed ibuprofen 600 mg, to be taken every 12 h daily. Received sham PBMT. | Verbal rating scale (VPRS) with ibuprofen. Verbal rating scale (VPRS) with PBMT. Numerical rating scale (NPRS) with ibuprofen. Numerical rating scale (NPRS) with PBMT. | There is a significant decrease in pain in the first 24 h with PBMT compared to the administration of ibuprofen 600mg (p < 0.001). |
| Gonçalves Langella L. et al., 2018 [17] | Randomized Clinical Trial | 9 people in the post-surgical period of knee arthroplasty. | 9 people in the post-surgical period of knee arthroplasty. | EG: PBMT applied at 5 points along the scar of the operation. CG: Sham PBMT applied at 5 points along the scar of the operation. | Changes in color. Changes in IL-6. Changes in IL-8. Changes in TNF-α. | There was a significant change in the group treated with PBMT, with reduced pain and serum levels of proinflammatory cytokines (p < 0.05) (IL-6, IL-8, TNF-α). |
| Fernanda R. et al., 2018 [18] | Randomized Clinical Trial | Group US + LLLT: 14 Caucasian women with knee osteoarthritis. Age range: 77–67 Group US + ET + LLLT: 14 Caucasian women with knee osteoarthritis. Age range: 71–61 | 14 Caucasian women with knee osteoarthritis. Age range: 69–61. | EG1 US + LLLT: US and LLLT applied to 5 specific points on the knee. EG2 US + ET + LLLT: US and LLLT applied to 5 specific points on the knee. In addition, performance of guided therapeutic exercise. CG: sham US and LLLT applied to 5 specific points on the knee. Subjects were blinded. | Changes in pain pressure threshold. Changes in the number of squats Radiological Evaluation (K-L Scale) | There was a significant increase in the pain pressure threshold (p < 0.01). The number of squats was higher in the experimental groups after treatment when compared to the CG (p < 0.0001). There were no radiological findings that differed between any of the groups. (p > 0.05). |
| Leyla K. et al., 2020 [19] | Randomized Clinical Trial | 20 people with nonspecific chronic low back pain. Men: 7 Women: 13 Age range: 25–65 Average age: 47 | 20 people with nonspecific chronic low back pain. Men: 5 Women: 15 Age range: 28–69 Average age: 51 | EG: LLLT applied to the joint spaces of the spine (3 points per disc, 30 s each), adjacent paravertebral points, radiating pain zones, and tender and acupuncture points. CG: The same intervention as the experimental group but in the form of sham treatments. | Changes in pain intensity (VAS). Changes in the range of motion of the lumbar spine. Functional status of the patients (according to RMQ). Spinal tenderness. | Significant changes in pain, functional status (p < 0.001) and range of motion of the lumbar spine, with these benefits persisting during the 3-month treatment period (p < 0.001), unlike in the control group where there were only improvements during the first month. There were no significant differences between groups regarding spinal tenderness. |
| Mariana M. et al., 2017 [20] | Randomized Clinical Trial | PBMT group: Formed of 2 groups, each containing 20 people with FM. ET group: Formed of 2 groups, each containing 20 people with FM. PBMT + ET group: Formed of 2 groups, each containing 20 people with FM. Set 1: Investigates the immediate effect of a single PBMT/ET session on chronic pain condition Age: 32–38 BMI (Kg/m2): 21–31 Set 2: Investigates the long-term effect (10 weeks) on the chronic pain condition and other FM symptoms Age: 38–42 BMI(Kg/m2): 23–31 | Divided into 2 groups, each containing 20 people with FM. Set 1: Investigates the immediate effect of a single PBMT/ET session on chronic pain condition Age: 32–38 BMI (Kg/m2): 21–31 Set 2: Investigates the long-term effect (10 weeks) on the chronic pain condition and other FM symptoms Age: 38–42 BMI (Kg/m2): 23–31 | EG1 (Set 1): Only one PBMT session was performed. These patients were evaluated at baseline and after 24 h. EG2 (Set 2): PBMT was applied 30 min before each exercise session. Outcome parameters were assessed at baseline (before group draw) and 48 h after the last day of intervention. PBMT: Applied for 300 s at each of 10 sensitive pain points. ET: Consisted of aerobic exercises and stretching 2 times/week for 10 weeks. They also performed TMJ exercises. PBMT + ET: They performed a combination of both protocols. | Changes in pain threshold. Changes in pain intensity (VAS). FIQ score. Sleep score. Mouth opening. | Pain threshold did not significantly improve after an exercise session; however, differences were noticeable with a PBMT session. Set 2 of the PBMT group showed similar results to Set 1. In Set 1, no additional benefits of the PBMT + ET combination were detected. The PBMT and PBMT + ET groups showed significant pain reduction versus the ET group and CG (Set 2). Furthermore, both combined therapies reduced the number of tender points. PBMT + ET had a beneficial role in anxiety, depression, and fatigue. |
| De Souza R. et al., 2018 [21] | Randomized Clinical Trial | 66 people with FM. Age Range: 57.05–35.23 Average age: 46.14 (62 women and 4 men) Group A: 33 volunteers with FM and chronic pain. Group B: 33 volunteers with FM and chronic pain. | None. | 2 sessions/week for 6 weeks: Group A: GaAIAs diode laser irradiation for 40 s at each selected point. 780 nm wavelength. Power: 50 mW. Energy: 2 J. Point-skin distance: 1 cm. 1 session/week for 4 weeks: Group B: Anesthetic injection of 2% lidocaine without vasoconstrictor. Volume: 0.5 mL at each tender point. Stretching after infiltrations. | Intensity of orofacial pain (VAS). Tenderness in the facial muscles. Perception of efficacy and well-being of both treatments. | Significant decrease in pain (p = 0.0001), although without any noticeable difference between groups. There was a decrease in pain intensity in tender points with both treatments. All the muscles analyzed had a response except for the temporal post (p < 0.05). The perception of the patients and their well-being improved in both groups with a slight difference in favor of Group A. |
| Shaiane S. et al., 2021 [22] | Randomized Clinical Trial | 9 people with chronic nonspecific low back pain. Women: 5 Men: 4 Age range: 20.51–47.05 Average age: 33.78 | 9 people with chronic nonspecific low back pain. Women: 6 Men: 3 Age range: 19.63–44.23 Average age: 31.44 | EG: A single PBMT session was applied with the following parameters: Area: 4 cm2. Frequency: 3000Hz. Time: 3 min at each sensitive point. Total energy radiated at each point (between the spinous processes of T11 and T12, L2 and L3, L5 and S1 and in the same direction but laterally, 3 sites to the left and another 3 to the right): 24.30 J. CG: Received the same therapy, but in a simulated way, in a single session. | Changes in PGE2. Pain intensity. Changes in IL-6. Changes in TNF-α. | With PBMT, PGE2 decreased significantly (p = 0.04) compared to the placebo group. The same did not happen with pain intensity, IL-6 or TNF-α, which did not show significant changes in relation to the CG. |
| Chong R. et al., 2020 [23] | Randomized Clinical Trial | 27 people with orthodontic pain and periodontal inflammation. | 27 people with orthodontic pain and periodontal inflammation. | EG: For 6 months the use of PBMT on orthodontic pain and periodontal inflammation is examined. During the first 2 months the volunteers had braces/buccal tubes in the maxillary and/or mandibular dental arches, followed by thermal NiTi archwire treatment in the 3rd month. The teeth in the middle of the dental arch were treated with LLLT. With a quadrangular probe, the region was covered from the central incisor to the first molar. The probe was first directed at the level of the braces and the buccal gingival margin and then moved to the level of the buccal alveolar mucosa. Wavelength: 940 nm. Output power: 800 mW. Irradiation duration: 30 s. CG: Received the same treatment as the experimental group but with a sham LLLT. | Subjective pain assessment. Clinical periodontal status and supragingival bacterial load. FGC biomarkers associated with pain and inflammation. | In the comparison between groups, regarding subjective pain, the side irradiated with LLLT experienced less pain, but it was only significant at the 6- and 24 h intervals (p = 0.01) and marginally significant at the 3-day interval (p = 0.03). No differences were found between groups (p > 0.05). regarding the clinical periodontal status and the bacterial load. The LLLT group had significant improvements in both pain 1 h and 24 h later (p = 0.02) and gingival inflammation during the first 24 h (p = 0.00). |
| Taradaj J. et al., 2019 [24] | Randomized Clinical Trial | TLAI group: 18 people with nonspecific chronic low back pain. Men: 10 Women: 8 Age range: 29–58. Average age: 44 LLLT group: 16 people with nonspecific chronic low back pain. Men: 8 Women: 8 Age range: 29–53 Average age: 45.50 | TLAI group: 17 people with nonspecific chronic low back pain. Men: 9 Women: 8 Age range: 26–51. Average age: 45 LLLT group: 17 people with nonspecific chronic low back pain. Men: 9 Women: 8 Age range: 22–76 Average age: 52 | EG: TLAI group: Received 15 daily high-intensity laser irradiations for 3 weeks. Area: 6 × 5 cm lumbar area with a 30 cm2 punctual applicator. Wavelength: 1064nm. Energy: 60 J/cm2. Duration: 10 min. LLLT group: Received 15 daily high-intensity laser irradiations for 3 weeks. Area: Paraspinal region of the lower back. Wavelength: 785nm. Energy: 8 J/cm2. Duration: 8 min. CG: The placebo TLAI group and the placebo LLLT group both received sham irradiation treatments of their respective types of lasers. | Roll path. Roll path along the Y axis. Roll path along the X axis. Average speed. Average frequency. Rolling area results. Tests are performed with eyes closed and eyes open. | The only non-significant changes were seen in the average frequency (p = 0.77 (Open Eyes); p = 0.68 (Closed Eyes)). Improvements did occur but were only significant in the short term (after 3 weeks of therapy). Analysis 1 and 3 months after therapy, without continuing stabilization exercises, showed the parameters to deteriorate over time. Therefore, the changes are observed over a short period of time. |
| Fang-Yin L. et al., 2020 [25] | Randomized Clinical Trial | 16 people with knee osteoarthritis. Age range: 77.42–63.64. | 17 people with knee osteoarthritis. Age range: 76.64–62.82. | EG: Treated with LLLT 3 times a week for 4 weeks at points SP9, SP10 and EX.-LE2 on the knee. Wavelength: 780 nm (P: 50 mW) and 830 nm (P: 30 mW). Duration: 15 min CG: Receives the same treatment as the EG but in a simulated way. | Subjective pain assessment (VAS) (Static and in motion). Changes in the pain pressure threshold (over the goosefoot tendon). Knee OA severity index (Lequesne index). | For the EG, the conscious VAS to move the knees decreased each week, while in the CG it did not decrease significantly. The same thing happened with the knee at rest (p < 0.01, p < 0.0001). The pain pressure threshold improved significantly each week in the EG, while for the CG this threshold did not improve effectively (p < 0.001, p < 0.0001). The OA severity index also improved significantly for the EG (p < 0.0001, p < 0.001) |
| Fernanda T. et al., 2018 [26] | Randomized Clinical Trial | Groups made up of 41 patients with temporomandibular pain and dysfunction (TMD). PBMT group: 14 patients. Women: 14 Age range: 30–61.4 MT group: 13 patients. Men: 1 Women: 12 Age Range: 20.9–61.5 Combined therapies (CTs) group: 14 patients. Men:1 Women: 13 Age range: 32.1–61.9. | None. | PBMT group: PBMT applied 3 times a week for 4 weeks. Wavelength: 808 nm. Dot size: 0.03 cm2. Power: 100 mW. Irradiation: 133 J/cm2. Irradiation time: 40 sec/point (12 points). MT group: Received 3 weekly session on intra- and extra- oral masticatory muscles (temporal, masseter, medial pterygoid on both sides) and TMJ for 4 weeks. CTs group: They underwent the MT and PBMT protocols 3 times a week for 4 weeks. | Pain assessment (VAS). Beck anxiety inventory (BAI). TMD classification. Assessment of psychosocial aspects. | All subjects experienced a significant reduction in pain (p < 0.001) although not between groups. All groups showed a reduction in anxiety (PBMT: p = 0.02; MT: 0.03; CTs: p < 0.001). The classification of the TMD, based on Axis I, revealed that all patients were diagnosed with GI and GIII and presented a combination of both myogenic aspects. MT promotes improvement in 2 impairments, PBMT in 5 and CTs in 1 (p < 0.001). The evaluation of psychosocial aspects, comparing baseline and follow-up in all treatment groups, revealed that the treatment did not modify the intensity of chronic pain (p > 0.05). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Muñoz, A.; Cuevas-Cervera, M.; Pérez-Montilla, J.J.; Aguilar-Núñez, D.; Hamed-Hamed, D.; Aguilar-García, M.; Pruimboom, L.; Navarro-Ledesma, S. Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review. Healthcare 2023, 11, 938. https://doi.org/10.3390/healthcare11070938
González-Muñoz A, Cuevas-Cervera M, Pérez-Montilla JJ, Aguilar-Núñez D, Hamed-Hamed D, Aguilar-García M, Pruimboom L, Navarro-Ledesma S. Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review. Healthcare. 2023; 11(7):938. https://doi.org/10.3390/healthcare11070938
Chicago/Turabian StyleGonzález-Muñoz, Ana, María Cuevas-Cervera, José Javier Pérez-Montilla, Daniel Aguilar-Núñez, Dina Hamed-Hamed, María Aguilar-García, Leo Pruimboom, and Santiago Navarro-Ledesma. 2023. "Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review" Healthcare 11, no. 7: 938. https://doi.org/10.3390/healthcare11070938
APA StyleGonzález-Muñoz, A., Cuevas-Cervera, M., Pérez-Montilla, J. J., Aguilar-Núñez, D., Hamed-Hamed, D., Aguilar-García, M., Pruimboom, L., & Navarro-Ledesma, S. (2023). Efficacy of Photobiomodulation Therapy in the Treatment of Pain and Inflammation: A Literature Review. Healthcare, 11(7), 938. https://doi.org/10.3390/healthcare11070938







