Child and Adolescent Mental Health during the COVID-19 Pandemic: Challenges of Psychiatric Outpatient Clinics
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Statistical Analysis
3. Results
3.1. Sample Characteristics
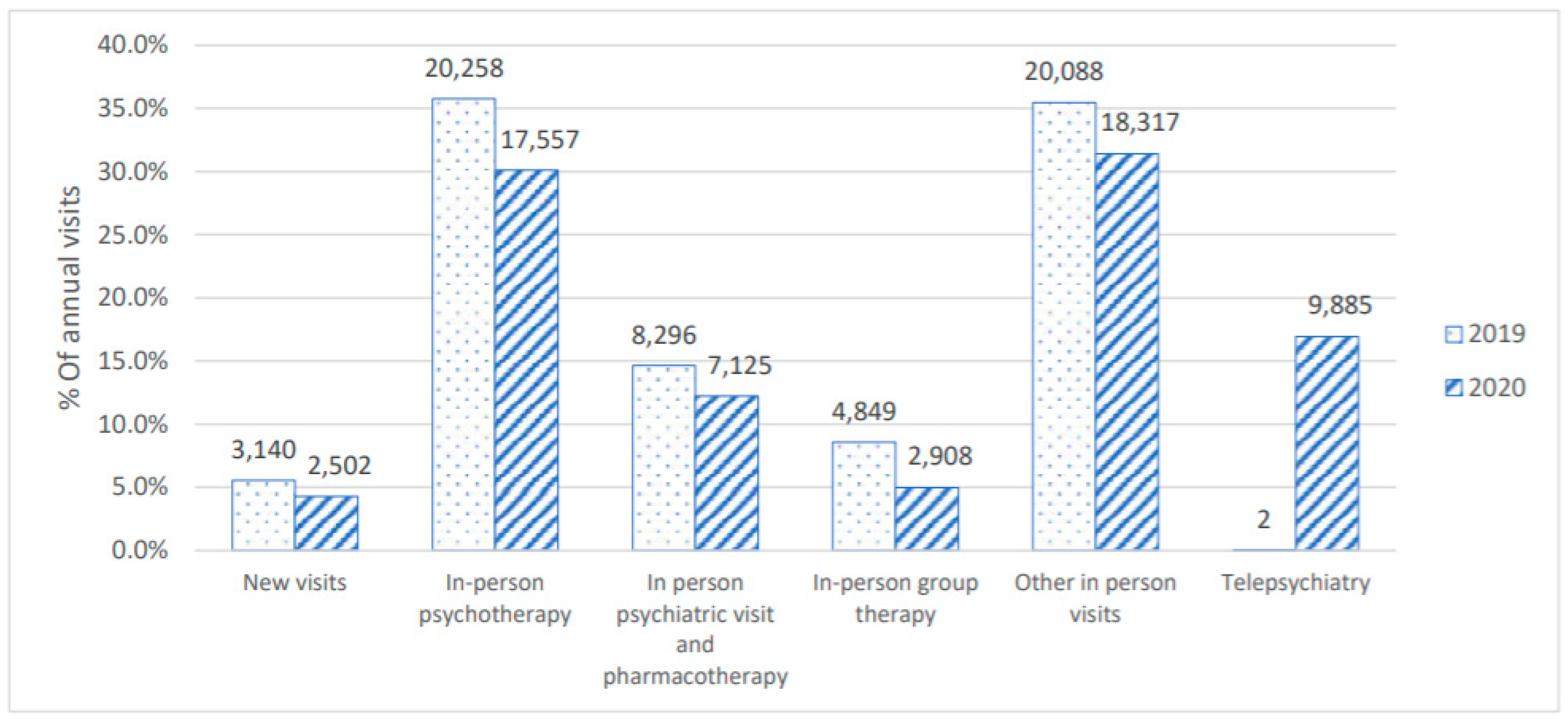
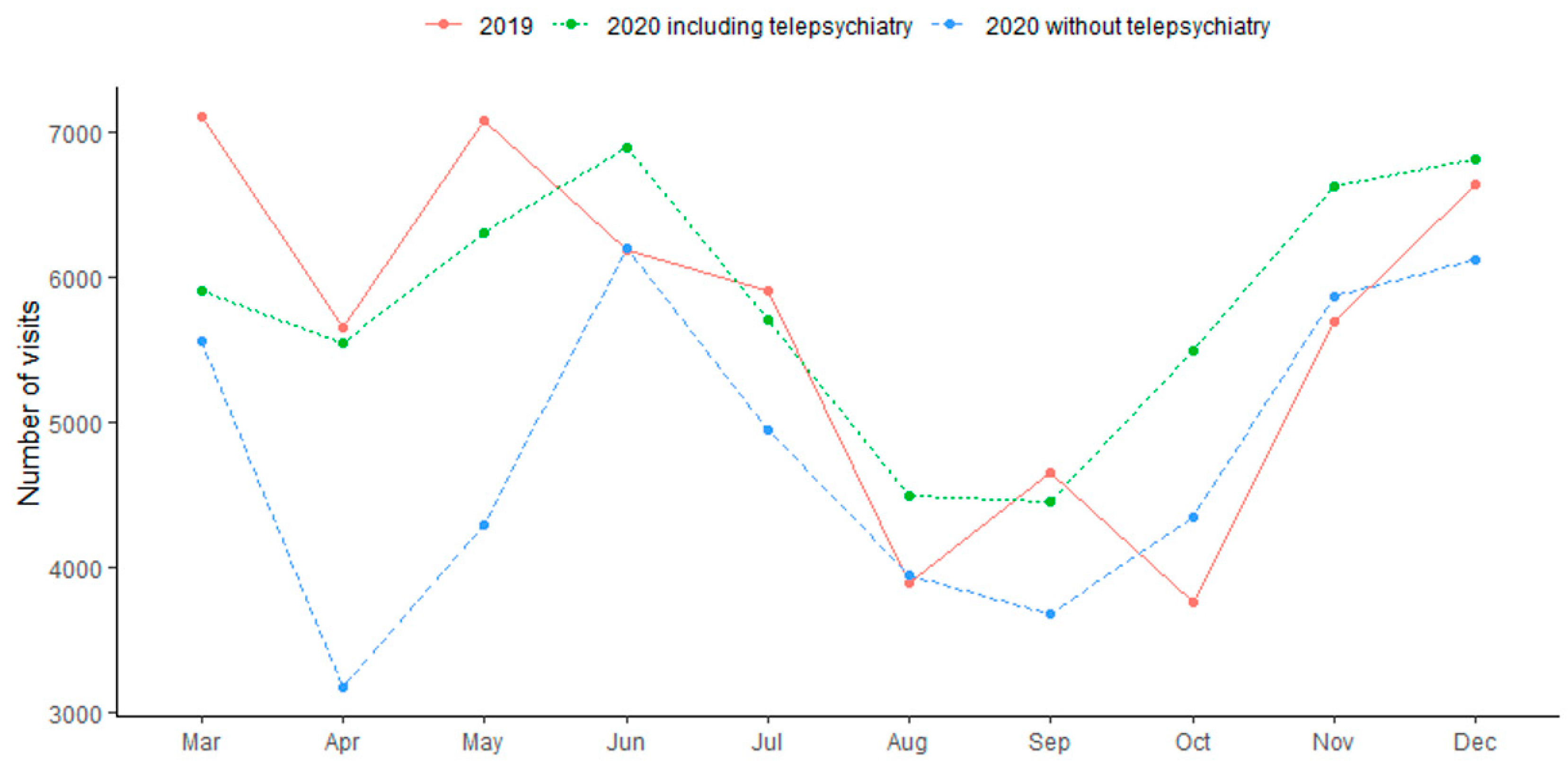
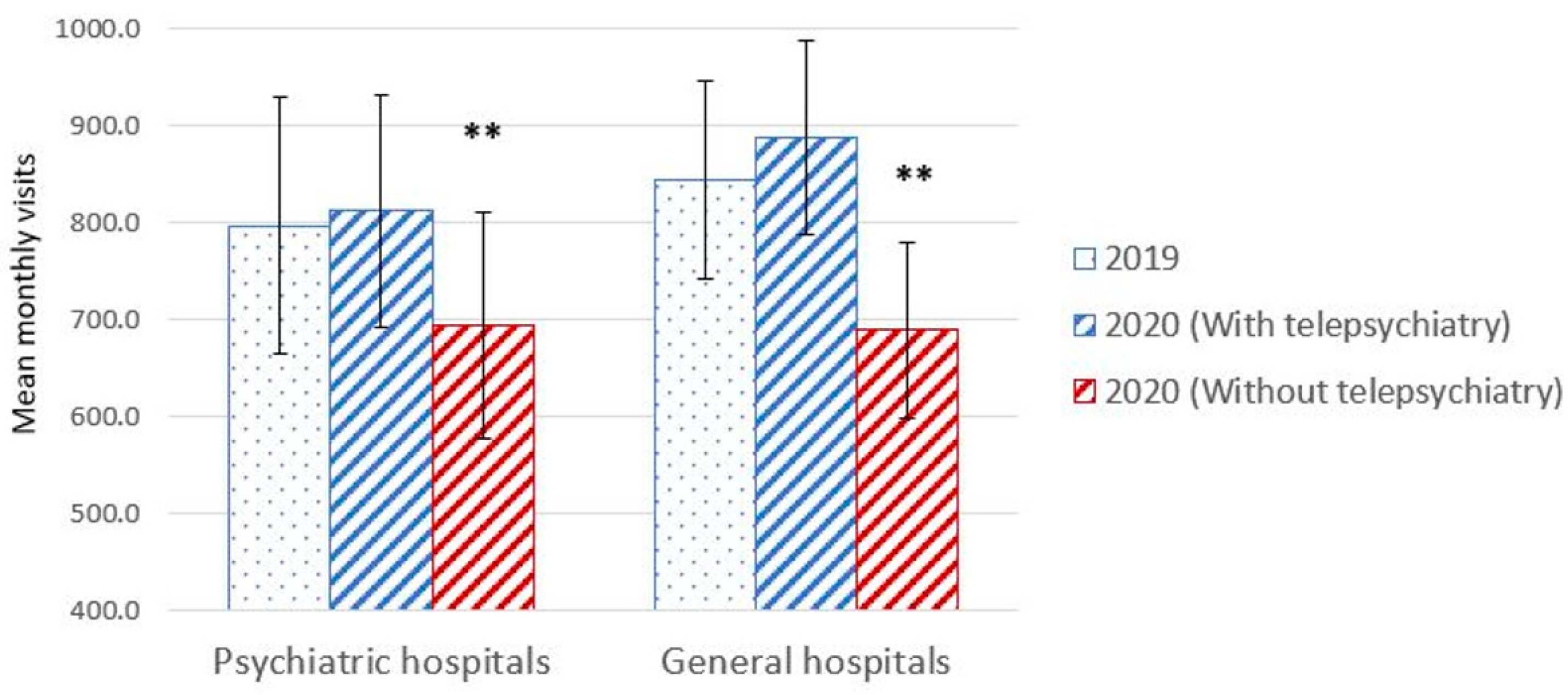
3.2. Type of Visits
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Geweniger, A.; Barth, M.; Haddad, A.D.; Högl, H.; Insan, S.; Mund, A.; Langer, T. Impact of the COVID-19 Pandemic on Mental Health Outcomes of Healthy Children, Children with Special Health Care Needs and Their Caregivers–Results of a Cross-Sectional Study. Front Pediatr. 2022, 10, 759066. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Saurabh, K.; Ranjan, S. Compliance and Psychological Impact of Quarantine in Children and Adolescents due to COVID-19 Pandemic. Indian J. Pediatr. 2020, 87, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Yeasmin, S.; Banik, R.; Hossain, S.; Hossain, M.N.; Mahumud, R.; Salma, N.; Hossain, M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: A cross-sectional study. Child. Youth Serv. Rev. 2020, 117, 105277. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898. [Google Scholar] [CrossRef]
- Gadermann, A.C.; Thomson, K.C.; Richardson, C.G.; Gagné, M.; Mcauliffe, C.; Hirani, S.; Jenkins, E.K. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: Findings from a national cross-sectional study. BMJ Open 2021, 11, e042871. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021, 31, 879–889. [Google Scholar] [CrossRef]
- Patrick, S.W.; Henkhaus, L.E.; Zickafoose, J.S.; Lovell, K.; Halvorson, A.; Loch, S.; Letterie, M.; Davis, M.M. Well-being of Parents and Children During the COVID-19 Pandemic: A National Survey. Pediatrics 2020, 146, e2020016824. [Google Scholar] [CrossRef]
- Gassman-Pines, A.; Ananat, E.O.; Fitz-Henley, J. COVID-19 and Parent-Child Psychological Well-being. Pediatrics 2020, 146, e2020007294. [Google Scholar] [CrossRef] [PubMed]
- Bilu, Y.; Flaks-Manov, N.; Bivas-Benita, M.; Akiva, P.; Kalkstein, N.; Yehezkelli, Y.; Mizrahi-Reuveni, M.; Ekka-Zohar, A.; Ben David, S.S.; Lerner, U.; et al. Data-driven assessment of adolescents’ mental health during the COVID-19 pandemic. Available online: https://pubmed.ncbi.nlm.nih.gov/36764609/ (accessed on 6 February 2023).
- Dror, C.; Hertz-Palmor, N.; Barzilai, Y.; Gila, S.; Tali, B.Z.; Alex, G.; Tal, L.; Maya, K.-L.; Talia, S.; Doron, G.; et al. Youth psychiatric hospitalization in Israel during COVID-19: A multi-center study. Int. J. Environ. Res. Public Health 2022, 19, 9870. [Google Scholar] [CrossRef]
- DeLaroche, A.M.; Rodean, J.; Aronson, P.L.; Fleegler, E.W.; Florin, T.A.; Goyal, M.; Hirsch, A.W.; Jain, S.; Kornblith, A.E.; Sills, M.R.; et al. Pediatric Emergency Department Visits at US Children’s Hospitals during the COVID-19 Pandemic. Pediatrics 2020, 147, e2020039628. [Google Scholar] [CrossRef]
- Krass, P.; Dalton, E.; Doupnik, S.K.; Esposito, J. US Pediatric Emergency Department Visits for Mental Health Conditions during the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, 8–11. [Google Scholar] [CrossRef]
- Dror, C.; Hertz-Palmor, N.; Yadan-Barzilai, Y.; Saker, T.; Kritchmann-Lupo, M.; Bloch, Y. Increase in referrals of children and adolescents to the psychiatric emergency room is evident only in the second year of the COVID-19 pandemic—Evaluating 9156 visits from 2010 through 2021 in a single psychiatric emergency room. Int. J. Environ. Res. Public Health 2022, 19, 8924. [Google Scholar] [CrossRef] [PubMed]
- Erez, G.; Yakubovich, S.; Sadeh, H.; Shoval, G.; Schoen, G.; Meiri, G.; Hertz-Palmor, N.; Bretler, T.; Bloch, Y. Pediatric psychiatric emergency rooms during COVID-19: A multi-center study. BMC Psychiatry 2021, 22, 828. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef] [PubMed]
- O’brien, M.; McNicholas, F. The use of telepsychiatry during COVID-19 and beyond. Ir. J. Psychol. Med. 2020, 37, 250–255. [Google Scholar] [CrossRef]
- Hubley, S.; Lynch, S.B.; Schneck, C.; Thomas, M.; Shore, J. Review of key telepsychiatry outcomes. World J. Psychiatry 2016, 6, 269–282. [Google Scholar] [CrossRef] [PubMed]
- Cowan, K.E.; McKean, A.J.; Gentry, M.T.; Hilty, D.M. Barriers to use of telepsychiatry: Clinicians as gatekeepers. Mayo Clin. Proc. 2019, 94, 2510–2523. [Google Scholar] [CrossRef]
- Schulz, T.; Long, K.; Kanhutu, K.; Bayrak, I.; Johnson, D.; Fazio, T. Telehealth during the coronavirus disease 2019 pandemic: Rapid expansion of telehealth outpatient use during a pandemic is possible if the program is previously established. J. Telemed. Telecare 2022, 28, 445–451. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J. Telepsychiatry: Learning from the pandemic. Br. J. Psychiatry 2022, 220, 257–261. [Google Scholar] [CrossRef]
- Perera, S.R.; Gambheera, H.; Williams, S.S. “Telepsychiatry” in the time of COVID-19: Overcoming the challenges. Indian J. Psychiatry 2020, 62 (Suppl. 3), S391–S394. [Google Scholar] [CrossRef] [PubMed]
- Saunders, N.R.; Kurdyak, P.; Stukel, T.A.; Strauss, R.; Fu, L.; Guan, J.; Fiksenbaum, L.; Cohen, E.; Toulany, A. Utilization of physician-based mental health care services among children and adolescents before and during the COVID-19 pandemic in Ontario, Canada. JAMA Pediatr. 2022, 176, e216298. [Google Scholar] [CrossRef] [PubMed]
- Ayraler Taner, H.; Akın Sarı, B.; Kaba, D. How did the COVID-19 pandemic affect child and adolescent psychiatry outpatient clinic admissions? A single-center, retrospective study. Clin. Child Psychol. Psychiatry 2022, 27, 824–835. [Google Scholar] [CrossRef]
- Saban, M.; Myers, V.; Shachar, T.; Miron, O.; Wilf-Miron, R.R. Effect of socioeconomic and ethnic characteristics on COVID-19 infection: The case of the ultra-orthodox and the Arab communities in Israel. J. Racial Ethn. Health Disparities 2022, 9, 581–588. [Google Scholar] [CrossRef]
- State Comptroller of Israel. Aspects of the Reform to Transfer Insurance Liability in Mental Health Care. 2022. Available online: https://www.mevaker.gov.il/sites/DigitalLibrary/Documents/2020/70b/70b-nagish/2020-70b-206-Mental-NAGISH.pdf?AspxAutoDetectCookieSupport=1 (accessed on 5 March 2023).
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Becker, L.A. Effect Size (ES). 2000. Available online: https://www.uv.es/~friasnav/EffectSizeBecker.pdf (accessed on 5 March 2023).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Sage: Thousand Oaks, CA, USA, 1997; (revised 31 December 1997). [Google Scholar]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 26. [Google Scholar] [CrossRef]
- Kassambara, A. Rstatix: Pipe-Friendly Framework for Basic Statistical Tests. R Package Version 0.7. 0. Computer Software. 2021. Available online: https://CRAN.R-project.org/package=rstatix (accessed on 5 March 2023).
- R Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2022. Available online: https://www.R-project.org/ (accessed on 5 March 2023).
- Meherali, S.; Punjani, N.; Louie-Poon, S.; Rahim, K.A.; Das, J.K.; Salam, R.A.; Lassi, Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: A rapid systematic review. Int. J. Environ. Res. Public Health 2021, 18, 3432. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- De Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-de-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-De-Araujo, E.; dos Santos, A.A.; Bomfim, P.O.-S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef]
- Imran, N.; Zeshan, M.; Pervaiz, Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak. J. Med Sci. 2020, 36, S67–S72. [Google Scholar] [CrossRef]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ Motivations to Engage in Social Distancing during the COVID-19 Pandemic: Associations with Mental and Social Health. J. Adolesc. Health 2020, 67, 179–185. Available online: https://pubmed.ncbi.nlm.nih.gov/32487491 (accessed on 5 March 2023). [CrossRef]
- Salmon, G.; James, A.; Cassidy, E.L.; Javaloyes, M.A. Bullying a review: Presentations to an adolescent psychiatric service and within a school for emotionally and behaviourally disturbed children. Clin. Child Psychol. Psychiatry 2000, 5, 563–579. [Google Scholar] [CrossRef]
- American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Telepsychiatry and AACAP Committee on Quality Issues. AACAP OFFICIAL ACTION Clinical Update: Telepsychiatry with Children and Adolescents American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Telepsychiatry and AACAP Committee on Quality Issues. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 875–893. [Google Scholar]
- Myers, K.; Nelson, E.L.; Rabinowitz, T.; Hilty, D.; Baker, D.; Barnwell, S.S.; Boyce, G.; Bufka, L.F.; Cain, S.; Chui, L.; et al. American Telemedicine Association Practice Guidelines for Telemental Health with Children and Adolescents. Telemed. E-Health 2017, 23, 779–804. [Google Scholar] [CrossRef]
- Kommu, J.V.S.; Sharma, E.; Ramtekkar, U. Telepsychiatry for Mental Health Service Delivery to Children and Adolescents. Indian J. Psychol Med. 2020, 42 (Suppl. 5), 46S–52S. [Google Scholar] [CrossRef] [PubMed]
- Myers, K.M.; Roth, D.E. Telepsychiatry with Children and Adolescents. Lewis’s Child Adolesc. Psychiatry 2018, 10, 885–896. [Google Scholar]
- Tandon, R. COVID-19 and mental health: Preserving humanity, maintaining sanity, and promoting health. Asian J. Psychiatr. 2020, 51, 102256. [Google Scholar] [CrossRef]
- Folk, J.B.; Schiel, M.A.; Oblath, R.; Feuer, V.; Sharma, A.; Khan, S.; Doan, B.; Kulkarni, C.; Ramtekkar, U.; Hawks, J.; et al. The Transition of Academic Mental Health Clinics to Telehealth during the COVID-19 Pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2021, 61, 277–290.e2. [Google Scholar] [CrossRef] [PubMed]
- Roesler, C. Tele-analysis: The use of media technology in psychotherapy and its impact on the therapeutic relationship. J. Anal. Psychol. 2017, 62, 372–394. [Google Scholar] [CrossRef] [PubMed]
- Titzler, I.; Saruhanjan, K.; Berking, M.; Riper, H.; Ebert, D.D. Barriers and facilitators for the implementation of blended psychotherapy for depression: A qualitative pilot study of therapists’ perspective. Internet Interv. 2018, 12, 150–164. [Google Scholar] [CrossRef]
- Békés, V.; Aafjes-van Doorn, K.; Luo, X.; Prout, T.A.; Hoffman, L. Psychotherapists’ Challenges with Online Therapy During COVID-19: Concerns about Connectedness Predict Therapists’ Negative View of Online Therapy and Its Perceived Efficacy Over Time. Front. Psychol. 2021, 12, 705699. [Google Scholar] [CrossRef] [PubMed]

| March–December 2019 Total = 56,663 N% | March–December 2020 Total = 58,294 N% | ||
|---|---|---|---|
| Gender Male (%) | 38,095 (67.27%) | 38,442 (65.95%) | |
| Female (%) | 18,538 (32.73%) | 19,852 (34.05%) | |
| Age groups | |||
| <12 | 20,310 | 10,968 (54.0%) | 9342 (46.0%) |
| >13 | 13,931 | 6421 (46.0%) | 7510 (54.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mosheva, M.; Barzilai, Y.; Hertz-Palmor, N.; Mekori-Domachevsky, E.; Avinir, A.; Erez, G.; Vardi, N.; Schoen, G.; Lahav, T.; Sadeh, H.; et al. Child and Adolescent Mental Health during the COVID-19 Pandemic: Challenges of Psychiatric Outpatient Clinics. Healthcare 2023, 11, 765. https://doi.org/10.3390/healthcare11050765
Mosheva M, Barzilai Y, Hertz-Palmor N, Mekori-Domachevsky E, Avinir A, Erez G, Vardi N, Schoen G, Lahav T, Sadeh H, et al. Child and Adolescent Mental Health during the COVID-19 Pandemic: Challenges of Psychiatric Outpatient Clinics. Healthcare. 2023; 11(5):765. https://doi.org/10.3390/healthcare11050765
Chicago/Turabian StyleMosheva, Mariela, Yael Barzilai, Nimrod Hertz-Palmor, Ehud Mekori-Domachevsky, Asia Avinir, Galit Erez, Noa Vardi, Gila Schoen, Tal Lahav, Hadar Sadeh, and et al. 2023. "Child and Adolescent Mental Health during the COVID-19 Pandemic: Challenges of Psychiatric Outpatient Clinics" Healthcare 11, no. 5: 765. https://doi.org/10.3390/healthcare11050765
APA StyleMosheva, M., Barzilai, Y., Hertz-Palmor, N., Mekori-Domachevsky, E., Avinir, A., Erez, G., Vardi, N., Schoen, G., Lahav, T., Sadeh, H., Rapaport, M., Dror, C., Gizunterman, A., Tsafrir, S., Gothelf, D., & Bloch, Y. (2023). Child and Adolescent Mental Health during the COVID-19 Pandemic: Challenges of Psychiatric Outpatient Clinics. Healthcare, 11(5), 765. https://doi.org/10.3390/healthcare11050765






