Morphological Characteristics of Proximal Ulna Fractures: A Proposal for a New Classification and Agreement for Validation
Abstract
1. Introduction
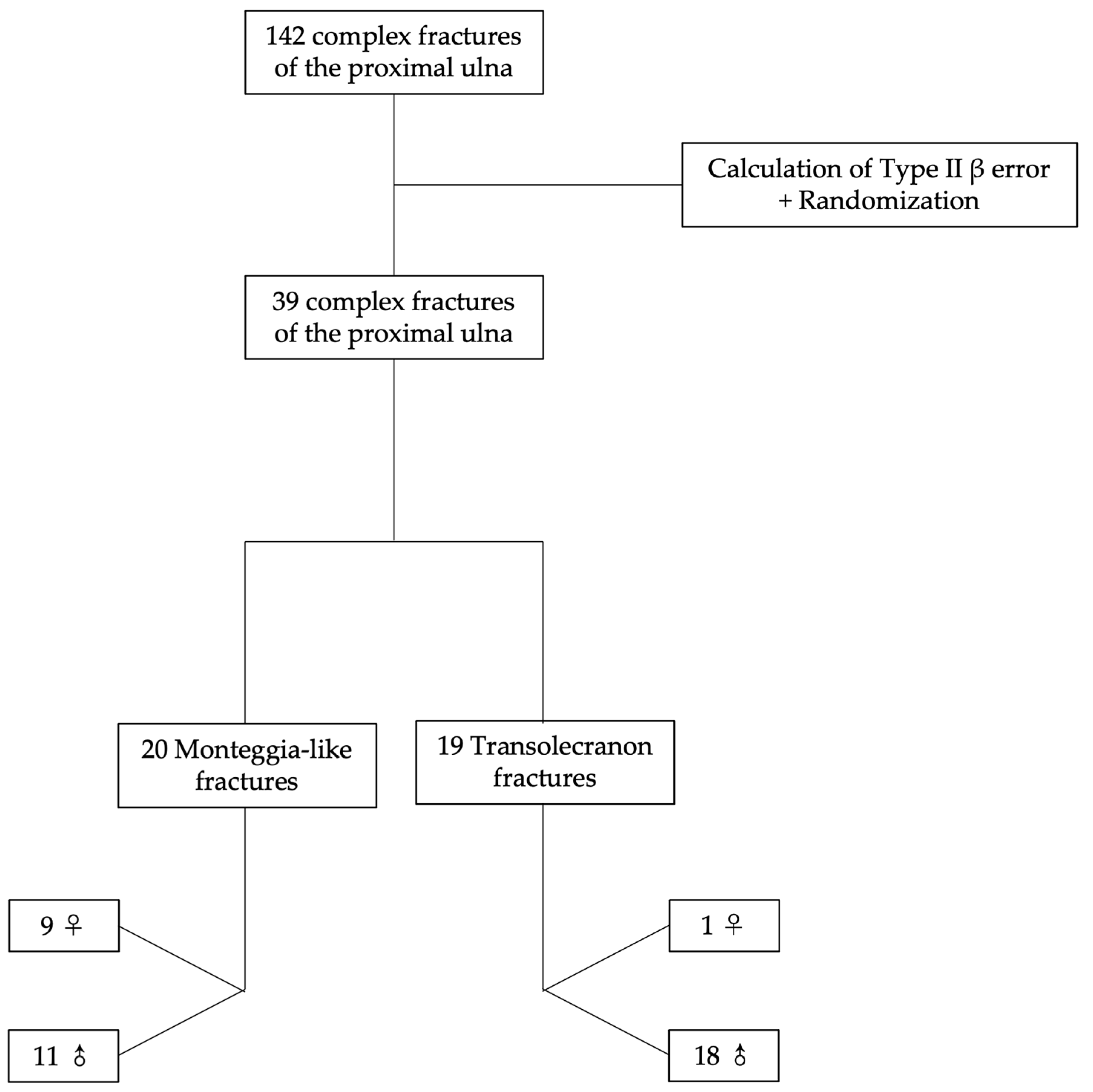
2. Materials and Methods
2.1. Patient Selection
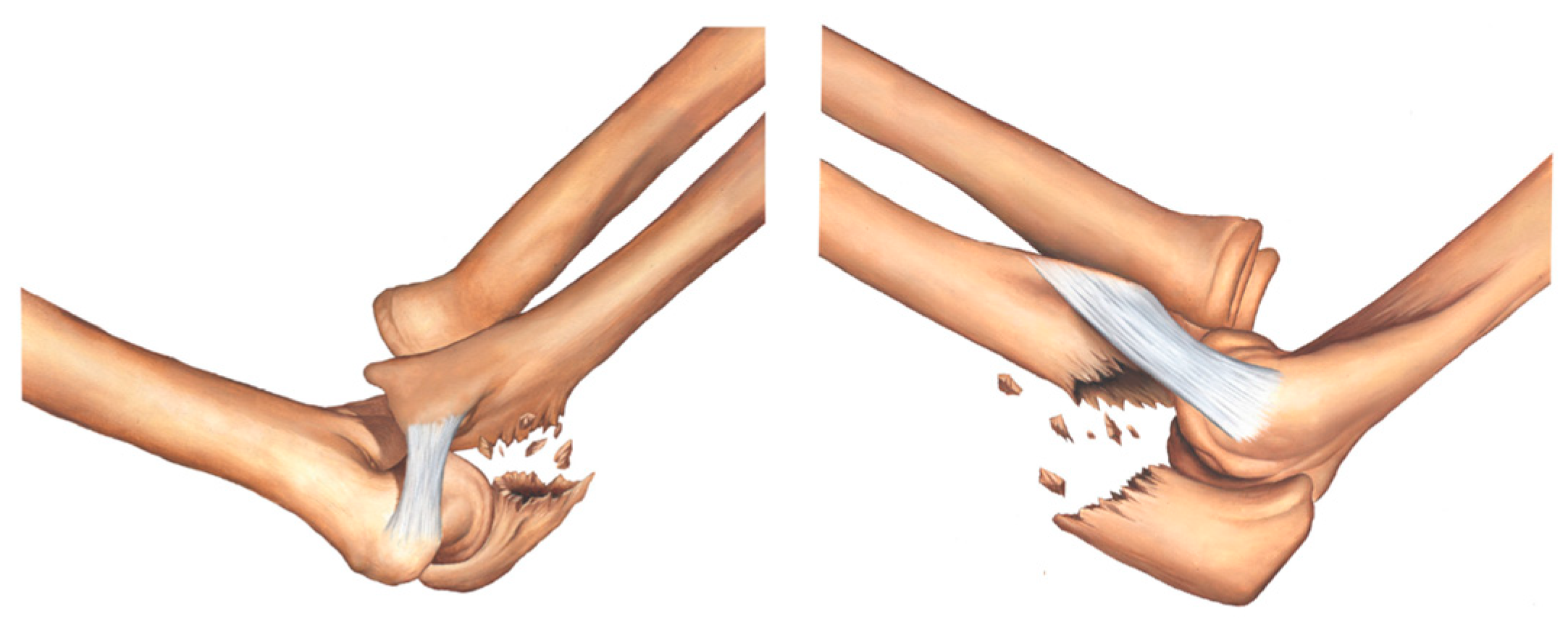
2.2. Classification
2.3. Validation
2.4. Statistical Analysis
3. Results
3.1. Intra-Rater Agreement
3.2. Inter-Rater Agreement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sahajpal, D.; Wright, T.W. Proximal ulna fractures. J. Hand. Surg. Am. 2009, 34, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.P. Revisiting the anatomy and biomechanics of the anconeus muscle and its role in elbow stability. Ann. Anat. 2013, 195, 365–370. [Google Scholar] [CrossRef]
- Sanchez-Sotelo, J.; Morrey, M. Complex elbow instability: Surgical management of elbow fracture dislocations. EFORT Open Rev. 2016, 1, 183–190. [Google Scholar] [CrossRef]
- An, K.N.; Morrey, B.F.; Chao, E.Y. The effect of partial removal of proximal ulna on elbow constraint. Clin. Orthop. Relat. Res. 1986, 270–279. [Google Scholar] [CrossRef]
- Bell, T.H.; Ferreira, L.M.; McDonald, C.P.; Johnson, J.A.; King, G.J. Contribution of the olecranon to elbow stability: An in vitro biomechanical study. J. Bone Jt. Surg. Am. 2010, 92, 949–957. [Google Scholar] [CrossRef]
- Closkey, R.F.; Goode, J.R.; Kirschenbaum, D.; Cody, R.P. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J. Bone Jt. Surg. Am. 2000, 82, 1749–1753. [Google Scholar] [CrossRef]
- Pollock, J.W.; Brownhill, J.; Ferreira, L.; McDonald, C.P.; Johnson, J.; King, G. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J. Bone Jt. Surg. Am. 2009, 91, 1448–1458. [Google Scholar] [CrossRef]
- Reichel, L.M.; Milam, G.S.; Hillin, C.D.; Reitman, C.A. Osteology of the coronoid process with clinical correlation to coronoid fractures in terrible triad injuries. J. Shoulder Elbow Surg 2013, 22, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Reichel, L.M.; Morales, O.A. Gross anatomy of the elbow capsule: A cadaveric study. J Hand Surg. Am. 2013, 38, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Ring, D.; Guss, D.; Jupiter, J.B. Reconstruction of the coronoid process using a fragment of discarded radial head. J. Hand Surg. Am. 2012, 37, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Sotelo, J.; O’Driscoll, S.W.; Morrey, B.F. Medial oblique compression fracture of the coronoid process of the ulna. J. Shoulder Elb. Surg 2005, 14, 60–64. [Google Scholar] [CrossRef]
- Sanchez-Sotelo, J.; O’Driscoll, S.W.; Morrey, B.F. Anteromedial fracture of the coronoid process of the ulna. J. Shoulder Elb. Surg 2006, 15, e5–e8. [Google Scholar] [CrossRef] [PubMed]
- Schneeberger, A.G.; Sadowski, M.M.; Jacob, H.A. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J. Bone Jt. Surg. Am. 2004, 86, 975–982. [Google Scholar] [CrossRef] [PubMed]
- von Ruden, C.; Woltmann, A.; Hierholzer, C.; Trentz, O.; Buhren, V. The pivotal role of the intermediate fragment in initial operative treatment of olecranon fractures. J. Orthop. Surg. Res. 2011, 6, 9. [Google Scholar] [CrossRef]
- Ring, D.; Jupiter, J.B. Fracture-dislocation of the elbow. Hand Clin. 2002, 18, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.C.; Singh, J.; Elvey, M.; Hamoodi, Z. Current concepts in elbow fracture dislocation. Shoulder Elb. 2021, 13, 451–458. [Google Scholar] [CrossRef]
- Doornberg, J.; Ring, D.; Jupiter, J.B. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin. Orthop. Relat. Res. 2004, 429, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Giannicola, G.; Greco, A.; Sacchetti, F.M.; Cinotti, G.; Nofroni, I.; Postacchini, F. Complex fracture-dislocations of the proximal ulna and radius in adults: A comprehensive classification. J. Shoulder Elb. Surg. 2011, 20, 1289–1299. [Google Scholar] [CrossRef]
- Jupiter, J.B.; Leibovic, S.J.; Ribbans, W.; Wilk, R.M. The posterior Monteggia lesion. J. Orthop. Trauma 1991, 5, 395–402. [Google Scholar] [CrossRef]
- Ring, D.; Jupiter, J.B.; Sanders, R.W.; Mast, J.; Simpson, N.S. Transolecranon fracture-dislocation of the elbow. J. Orthop. Trauma 1997, 11, 545–550. [Google Scholar] [CrossRef]
- Hamoodi, Z.; Singh, J.; Elvey, M.H.; Watts, A.C. Reliability and validity of the Wrightington classification of elbow fracture-dislocation. Bone Joint J. 2020, 102, 1041–1047. [Google Scholar] [CrossRef]
- de Haan, J.; Schep, N.W.; Eygendaal, D.; Kleinrensink, G.J.; Tuinebreijer, W.E.; den Hartog, D. Stability of the elbow joint: Relevant anatomy and clinical implications of in vitro biomechanical studies. Open Orthop. J. 2011, 5, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Regan, W.; Morrey, B. Fractures of the coronoid process of the ulna. J. Bone Jt. Surg. Am. 1989, 71, 1348–1354. [Google Scholar] [CrossRef]
- Jackson, J.D.; Steinmann, S.P. Radial head fractures. Hand Clin. 2007, 23, 185–193, vi. [Google Scholar] [CrossRef]
- O’Driscoll, S.W.; Jupiter, J.B.; Cohen, M.S.; Ring, D.; McKee, M.D. Difficult elbow fractures: Pearls and pitfalls. Instr. Course Lect. 2003, 52, 113–134. [Google Scholar]
- O’Driscoll, S.W.; Morrey, B.F.; Korinek, S.; An, K.N. Elbow subluxation and dislocation. A spectrum of instability. Clin. Orthop. Relat. Res. 1992, 186–197. [Google Scholar]
- Regan, W.D.; Korinek, S.L.; Morrey, B.F.; An, K.N. Biomechanical study of ligaments around the elbow joint. Clin. Orthop. Relat. Res 1991, 170–179. [Google Scholar] [CrossRef]
- Ring, D.; Jupiter, J.B. Fracture-dislocation of the elbow. J. Bone Jt. Surg. Am. 1998, 80, 566–580. [Google Scholar] [CrossRef]
- Chick, G.; Nordin, J.Y. Fractures complexes de l’extrémité supérieure des deux os de l’avant-bras chez l’adulte: Proposition d’une nouvelle classification. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2001, 87, 765–772. [Google Scholar] [PubMed]
- Egol, K.A.; Tejwani, N.C.; Bazzi, J.; Susarla, A.; Koval, K.J. Does a Monteggia variant lesion result in a poor functional outcome?: A retrospective study. Clin. Orthop. Relat. Res. 2005, 438, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Xiao, R.C.; Chan, J.J.; Cirino, C.M.; Kim, J.M. Surgical management of complex adult Monteggia fractures. J. Hand Surg. Am. 2021, 46, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Melamed, E.; Danna, N.; Debkowska, M.; Karia, R.; Liporace, F.; Capo, J.T. Complex proximal ulna fractures: Outcomes of surgical treatment. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Midtgaard, K.S.; Nolte, P.C.; Miles, J.W.; Tanghe, K.K.; Peebles, L.A.; Provencher, M.T.; Adolfsson, L. Biomechanical significance of the collateral ligaments in transolecranon fracture dislocations. J. Shoulder Elbow Surg. 2021, 30, 1245–1250. [Google Scholar] [CrossRef]
- Kfuri, M.; Schatzker, J. Revisiting the Schatzker classification of tibial plateau fractures. Injury 2018, 49, 2252–2263. [Google Scholar] [CrossRef] [PubMed]
- Park, S.G.; Ko, Y.J. Medial buttress plating for humerus fractures with unstable medial column. J. Orthop. Trauma 2019, 33, e352–e359. [Google Scholar] [CrossRef]
- Rikli, D.A.; Babst, R.; Jupiter, J.B. Distale Radiusfraktur: Neue Konzepte als Basis für die operative Therapie. Handchir. Mikrochir. Plast. Chir. 2007, 39, 2–8. [Google Scholar] [CrossRef]
- Sameer, M.; Bassetty, K.C.; Singaravadivelu, V. Fixation of tibial pilon fractures based on column concept: A prospective study. Acta Orthop. Belg. 2017, 83, 568–573. [Google Scholar]
- Zhang, R.; Yin, Y.; Li, A.; Wang, Z.; Hou, Z.; Zhuang, Y.; Fan, S.; Wu, Z.; Yi, C.; Lyu, G.; et al. Three-column classification for acetabular fractures: Introduction and reproducibility assessment. J. Bone Jt. Surg. Am. 2019, 101, 2015–2025. [Google Scholar] [CrossRef]
- Gonzalez, L.J.; Shields, C.N.; Leucht, P.; Konda, S.R.; Egol, K.A. Fracture-dislocations of the elbow: A comparison of Monteggia and terrible triad fracture patterns. Orthopedics 2022, 2, 1–6. [Google Scholar] [CrossRef]
- Siebenlist, S.; Buchholz, A.; Braun, K.F. Fractures of the proximal ulna: Current concepts in surgical management. EFORT Open Rev. 2019, 4, 1–9. [Google Scholar] [CrossRef]






| Age Statistics | Monteggia-like | Transolecranon | ||||
|---|---|---|---|---|---|---|
| Overall | Female | Male | Overall | Female | Male | |
| Minimum | 22.0 | 30.0 | 22.0 | 19.0 | 62.0 | 19.0 |
| Maximum | 79.0 | 79.0 | 58.0 | 73.0 | 62.0 | 73.0 |
| Median | 48.0 | 55.0 | 31.0 | 40.0 | 62.0 | 40.0 |
| Mean | 45.2 | 55.7 | 36.5 | 43.7 | 62.0 | 42.7 |
| Standard deviation | 16.1 | 14.1 | 12.3 | 16.3 | 0.0 | 16.1 |
| Coefficient of variation | 0.36 | 0.25 | 0.34 | 0.37 | 0.00 | 0.38 |
| Type | Medial Column (Sublime Tubercle/Anterior Band of MCL) | Intermediate Column (Coronoid Process/Anterior Capsule) | Lateral Column (Supinator Crest/LUCL) |
|---|---|---|---|
| IA | − | − | − |
| IB | − | + | − |
| IIA | + | − | − |
| IIB | + | + | − |
| IIIA | − | − | + |
| IIIB | − | + | + |
| IV | + | + | + |
| Rater | Absolute Agreement | Weighted Kappa (95% CI) | Kendall Coefficient |
|---|---|---|---|
| R1 | 0.82 | 0.82 (0.69; 0.90) ‡ | 0.82 ‡ |
| R2 | 0.87 | 0.91 (0.83; 0.95) ‡ | 0.84 ‡ |
| R3 | 0.82 | 0.92 (0.85; 0.96) ‡ | 0.90 ‡ |
| Assessment Round | Agreement Measure | R1–R2 | R1–R3 | R2–R3 | R1, R2, and R3 |
|---|---|---|---|---|---|
| 1 | Absolute agreement | 0.79 | 0.77 | 0.77 | 0.77 |
| Weighted kappa ‡ | 0.75 (0.45; 0.85) | 0.75 (0.44; 0.82) | 0.78 (0.49; 0.83) | 0.76 (0.59; 0.86) | |
| Kendall coefficient ‡ | 0.78 | 0.77 | 0.72 | - | |
| 2 | Absolute agreement | 0.82 | 0.77 | 0.79 | 0.77 |
| Weighted kappa ‡ | 0.77 (057; 0.88) | 0.75 (0.33; 0.81) | 0.77 (0.44; 0.87) | 0.78 (0.63; 0.88) | |
| Kendall coefficient ‡ | 0.78 | 0.77 | 0.78 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Labronici, P.J.; Belangero, W.D.; Zublin, C.M.; Gonçalves, L.B.J.; Fajardo, H.; Pires, R.E.; Giordano, V. Morphological Characteristics of Proximal Ulna Fractures: A Proposal for a New Classification and Agreement for Validation. Healthcare 2023, 11, 693. https://doi.org/10.3390/healthcare11050693
Labronici PJ, Belangero WD, Zublin CM, Gonçalves LBJ, Fajardo H, Pires RE, Giordano V. Morphological Characteristics of Proximal Ulna Fractures: A Proposal for a New Classification and Agreement for Validation. Healthcare. 2023; 11(5):693. https://doi.org/10.3390/healthcare11050693
Chicago/Turabian StyleLabronici, Pedro José, William Dias Belangero, Carlos Miguel Zublin, Lucas Braga Jaques Gonçalves, Humberto Fajardo, Robinson Esteves Pires, and Vincenzo Giordano. 2023. "Morphological Characteristics of Proximal Ulna Fractures: A Proposal for a New Classification and Agreement for Validation" Healthcare 11, no. 5: 693. https://doi.org/10.3390/healthcare11050693
APA StyleLabronici, P. J., Belangero, W. D., Zublin, C. M., Gonçalves, L. B. J., Fajardo, H., Pires, R. E., & Giordano, V. (2023). Morphological Characteristics of Proximal Ulna Fractures: A Proposal for a New Classification and Agreement for Validation. Healthcare, 11(5), 693. https://doi.org/10.3390/healthcare11050693







