To Admit or Not to Admit to the Emergency Department: The Disposition Question at a Tertiary Teaching and Referral Hospital
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Inclusion Criteria
2.3. Setting of the Study
2.4. The Tool Description
2.5. Statistical Analysis
3. Results
3.1. Patients’ Demographic and Socioeconomic Characteristics
3.2. Patients’ Clinical Conditions and Characteristics
3.3. Multivariate Analysis Results
4. Discussion
5. Contribution and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ED | Emergency Department |
| SAR | Saudi Arabia Riyals |
| KAMC-KF | King Abdulaziz Medical City-King Fahad hospital |
| NGHA | National Guard Health Affairs |
| JCI | Joint Commission of International Standard |
| QUT | Queensland University of Technology |
| IRB | Institutional Review Board |
| KAIMRC | King Abdullah International Medical Research Center |
References
- Manuel, J.I.; Lee, J. Gender differences in discharge dispositions of emergency department visits involving drug misuse and abuse—2004–2011. Subst. Abuse Treat. Prev. Policy 2017, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Healthcare Cost and Utilization Project (HCUP). HCUP Nationwide Emergency Department Sample (NEDS); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016. [Google Scholar]
- Dinh, M.M.; Russell, S.B.; Bein, K.J.; Rogers, K.; Muscatello, D.; Paoloni, R.; Hayman, J.; Chalkley, D.R.; Ivers, R. The Sydney Triage to Admission Risk Tool (START) to predict Emergency Department Disposition: A derivation and internal validation study using retrospective state-wide data from New South Wales, Australia. BMC Emerg. Med. 2016, 16, 46. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Hilton, J.A.; Weber, E.J.; Alkemade, A.J.; Al Shabanah, H.; Anderson, P.D.; Bernhard, M.; Bertini, A.; Gries, A.; Ferrandiz, S. International perspectives on emergency department crowding. Acad. Emerg. Med. 2011, 18, 1358–1370. [Google Scholar] [CrossRef] [PubMed]
- Bakarman, M.A.; Njaifan, N.K. Assessment of non-emergency cases attending emergency department at King Fahad General Hospital, Jeddah; pattern and outcomes. Life Sci. J. 2014, 11, 20–25. [Google Scholar]
- Alsirafy, S.A.; Raheem, A.A.; Al-Zahrani, A.S.; Mohammed, A.A.; Sherisher, M.A.; El-Kashif, A.T.; Ghanem, H.M. Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidability. Am. J. Hosp. Palliat. Med. 2016, 33, 658–662. [Google Scholar] [CrossRef]
- Alyasin, A.; Douglas, C. Reasons for non-urgent presentations to the emergency department in Saudi Arabia. Int. Emerg. Nurs. 2014, 22, 220–225. [Google Scholar] [CrossRef]
- Alghanim, S.A.; Alomar, B.A. Frequent use of emergency departments in Saudi public hospitals: Implications for primary health care services. Asia Pac. J. Public Health 2015, 27, NP2521–NP2530. [Google Scholar] [CrossRef]
- Rehmani, R.; Norain, A. Trends in emergency department utilization in a hospital in the Eastern region of Saudi Arabia. Saudi Med. J. 2007, 28, 236–240. [Google Scholar]
- Dawoud, S.O.; Ahmad, A.M.K.; Alsharqi, O.Z.; Al-Raddadi, R.M. Utilization of the emergency department and predicting factors associated with its use at the Saudi Ministry of Health General Hospitals. Glob. J. Health Sci. 2016, 8, 90. [Google Scholar] [CrossRef]
- Shalabi, A.; Alsharqi, O.; Alnujaidi, M.; Alosaimy, R.; Altalhi, E.; Kashmeeri, R.; Aldibane, R. Factors predicting hospital admission for non-urgent patients presenting to the emergency department. Saudi J. Emerg. Med. 2021, 2, 133–141. [Google Scholar] [CrossRef]
- Rutkowski, R.A.; Salwei, M.; Barton, H.; Wust, K.; Hoonakker, P.; Brenny-Fitzpatrick, M.; King, B.; Shah, M.N.; Pulia, M.S.; Patterson, B.W. Physician Perceptions of Disposition Decision-making for Older Adults in the Emergency Department: A Preliminary Analysis. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Virtual, 5–9 October 2020; SAGE Publications: Los Angeles, CA, USA, 2020; Volume 64, pp. 648–652. [Google Scholar]
- Boudi, Z.; Lauque, D.; Alsabri, M.; Östlundh, L.; Oneyji, C.; Khalemsky, A.; Lojo Rial, C.; Liu, S.W.; Camargo, C.A., Jr.; Aburawi, E.; et al. Association between boarding in the emergency department and in-hospital mortality: A systematic review. PLoS ONE 2020, 15, e0231253. [Google Scholar] [CrossRef] [PubMed]
- Janke, A.T.; Melnick, E.R.; Venkatesh, A.K. Hospital Occupancy and Emergency Department Boarding During the COVID-19 Pandemic. JAMA Netw. Open 2022, 5, e2233964. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.T.; Snyder, A.; Hollen, P.J.; Anderson, J.G.; Caterino, J.M. Analyzing the usability of the 5-level Canadian triage and acuity scale by paramedics in the prehospital environment. J. Emerg. Nurs. 2015, 41, 489–495. [Google Scholar] [CrossRef]
- Toloo, S.; FitzGerald, G.; Aitken, P.; Ting, J.; Tippett, V.; Chu, K. Emergency Health Services: Demand and Service Delivery Models: Monograph 1: Literature Review and Activity Trends; Queensland University of Technology: Brisbane, QLD, Australia, 2011. [Google Scholar]
- Richards, J.R.; Ferrall, S.J. Triage ability of emergency medical services providers and patient disposition: A prospective study. Prehospital Disaster Med. 1999, 14, 67–72. [Google Scholar] [CrossRef]
- Sun, Y.; Heng, B.H.; Tay, S.Y.; Seow, E. Predicting hospital admissions at emergency department triage using routine administrative data. Acad. Emerg. Med. 2011, 18, 844–850. [Google Scholar] [CrossRef]
- de la Granda, M.B.M.; Gutiérrez, G.G.; Fernández, M.F.; Jaurrieta, J.J.S. Impacto del paciente anciano en los servicios de urgencias hospitalarios. Rev. Esp. Geriatría Gerontol. 2018, 53, 145–148. [Google Scholar] [CrossRef]
- Samaras, N.; Chevalley, T.; Samaras, D.; Gold, G. Older patients in the emergency department: A review. Ann. Emerg. Med. 2010, 56, 261–269. [Google Scholar] [CrossRef]
- Khan, Y.; Glazier, R.H.; Moineddin, R.; Schull, M.J. A population-based study of the association between socioeconomic status and emergency department utilization in Ontario, Canada. Acad. Emerg. Med. 2011, 18, 836–843. [Google Scholar] [CrossRef]
- Morganti, K.G.; Bauhoff, S.; Blanchard, J.C.; Abir, M.; Iyer, N.; Smith, A.; Vesely, J.V.; Okeke, E.N.; Kellermann, A.L. The evolving role of emergency departments in the United States. Rand Health Q. 2013, 3, 3. [Google Scholar]
- Miravitlles, M.; Guerrero, T.; Mayordomo, C.; Sánchez-Agudo, L.; Nicolau, F.; Segú, J.L. Factors Associated with Increased Risk of Exacerbation and Hospital Admission in a Cohort of Ambulatory COPD Patients: A Multiple Logistic Regression Analysis. Respiration 2000, 67, 495–501. [Google Scholar] [CrossRef]
- Opara, N.U.; Hensley, B.M.; Judy, C. Evaluating the Benefits of Viral Respiratory Panel Test in the Reduction of Emergency Department Throughput Time for Patients With Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Cureus 2021, 13, e19213. [Google Scholar] [CrossRef]
- Chang, J.L.; Reyes, R.; Matte, M.; Ntaro, M.; Mulogo, E.; Wiens, M.O.; Meshnick, S.R.; Siedner, M.J.; Boyce, R.M. Who stays and who goes: Predictors of admission among patients presenting with febrile illness and a positive malaria rapid diagnostic test in a rural Ugandan health center. Am. J. Trop. Med. Hyg. 2018, 99, 1080. [Google Scholar] [CrossRef]
- Le Conte, P.; Riochet, D.; Batard, E.; Volteau, C.; Giraudeau, B.; Arnaudet, I.; Labastire, L.; Levraut, J.; Thys, F.; Lauque, D. Death in emergency departments: A multicenter cross-sectional survey with analysis of withholding and withdrawing life support. Intensive Care Med. 2010, 36, 765–772. [Google Scholar] [CrossRef]
- Hu, Z.; Siddiqui, F.J.; Fan, Q.; Lian, S.W.; Liu, N.; Ong, M.E. Trends of chronic illness in emergency department admissions among elderly adults in a tertiary hospital over ten years. BMC Health Serv. Res. 2021, 21, 1305. [Google Scholar] [CrossRef]
- Vilpert, S.; Monod, S.; Jaccard Ruedin, H.; Maurer, J.; Trueb, L.; Yersin, B.; Büla, C. Differences in triage category, priority level and hospitalization rate between young-old and old-old patients visiting the emergency department. BMC Health Serv. Res. 2018, 18, 456. [Google Scholar] [CrossRef]
- Zachariasse, J.M.; van der Hagen, V.; Seiger, N.; Mackway-Jones, K.; van Veen, M.; Moll, H.A. Performance of triage systems in emergency care: A systematic review and meta-analysis. BMJ Open 2019, 9, e026471. [Google Scholar] [CrossRef]
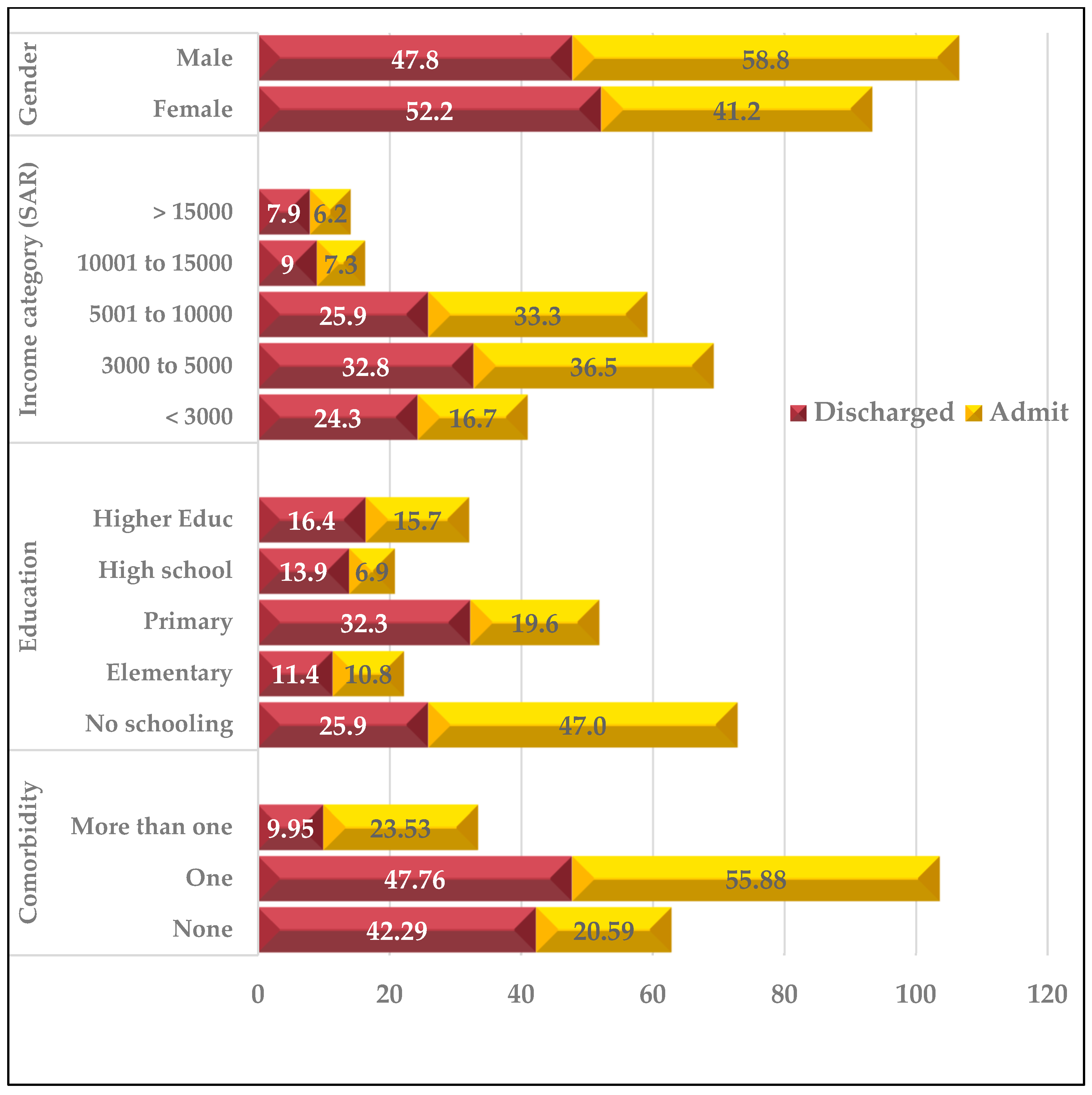
| Variable | Discharged Home (n = 201) | Admitted to Bed (n = 102) | All Patients (n = 303) | p-Value | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Age category | <50 years | 109 (54.23) | 31 (30.39) | 140 (46.2) | 0.001 * |
| ≥50 years | 92 (45.77) | 71 (69.61) | 163 (53.8) | ||
| Gender | Female | 105 (52.24) | 42 (41.18) | 147 (48.51) | 0.044 * |
| Male | 96 (47.76) | 60 (58.82) | 156 (51.49) | ||
| Marital status | Others | 69 (34.33) | 28 (27.45) | 97 (32.01) | 0.139 |
| Married | 132 (65.67) | 74 (72.55) | 206 (67.99) | ||
| Residence | Out of Riyadh | 32 (16.24) | 15 (14.71) | 47 (15.72) | 0.434 |
| Riyadh | 165 (83.76) | 87 (85.29) | 252 (84.28) | ||
| Schooling level | No schooling | 52 (25.87) | 48 (47.06) | 100 (33) | 0.003 * |
| Elementary | 23 (11.44) | 11 (10.78) | 34 (11.22) | ||
| Primary | 65 (32.34) | 20 (19.61) | 85 (28.05) | ||
| High school | 28 (13.93) | 7 (6.86) | 35 (11.55) | ||
| Higher Education | 33 (16.42) | 16 (15.69) | 49 (16.17) | ||
| Household income (SAR) | <3000 | 46 (24.34) | 16 (16.67) | 62 (21.75) | 0.469 |
| 3000 to 5000 | 62 (32.8) | 35 (36.46) | 97 (34.04) | ||
| 5001 to 10,000 | 49 (25.93) | 32 (33.33) | 81 (28.42) | ||
| 10,001 to 15,000 | 17 (8.99) | 7 (7.29) | 24 (8.42) | ||
| ≥15,000 | 15 (7.94) | 6 (6.25) | 21 (7.37) | ||
| Employed | No | 156 (77.61) | 81 (79.41) | 237 (78.22) | 0.42 |
| Yes | 45 (22.39) | 21 (20.59) | −21.78 | ||
| Insurance NGHA | No | 15 (7.46) | 7 (6.86) | 22 (7.26) | 0.526 |
| Yes | 186 (92.54) | 95 (93.14) | 281 (92.74) |
| Variable | Discharged Home (n = 201) | Admitted to Bed (n = 102) | All Patients (n = 303) | p-Value | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||
| History of hospitalization | No | 143 (71.14) | 51 (50) | 194 (64.03) | <0.001 * | |
| Yes | 58 (28.86) | 51 (50) | 109 (35.97) | |||
| Frequency of ED visits in a year | <4 visits | 123 (63.4) | 58 (57.43) | 181 (61.36) | 0.191 | |
| ≥4 or more | 71 (36.6) | 43 (42.57) | 114 (38.64) | |||
| Health status | Poor | 5 (2.51) | 11 (11) | 16 (5.35) | <0.001 * | |
| V.good/Excellent | 81 (40.7) | 22 (22) | 103 (34.45) | |||
| Fair/good | 113 (56.78) | 67 (67) | 180 (60.2) | |||
| Get care when needed | No | 55 (27.36) | 22 (21.57) | 77 (25.41) | 0.17 | |
| Yes | 146 (72.64) | 80 (78.43) | 226 (74.59) | |||
| Mode arrival at ED | Others | 5 (2.53) | 3 (2.97) | 8 (2.68) | <0.001 * | |
| Ambulance | 12 (6.06) | 9 (8.91) | 21 (7.02) | |||
| Own car | 120 (60.61) | 37 (36.63) | 157 (52.51) | |||
| Fam/friend car | 61 (30.81) | 52 (51.49) | 113 (37.79) | |||
| Urgency of clinical condition | Not urgent | 148 (73.63) | 42 (41.18) | 190 (62.71) | <0.001 * | |
| Urgent | 53 (26.37) | 60 (58.82) | 113 (37.29) | |||
| Comorbidity | None | 85 (42.29) | 21 (20.59) | 106 (34.98) | <0.001 * | |
| One | 96 (47.76) | 57 (55.88) | 153 (50.5) | |||
| More than one | 20 (9.95) | 24 (23.53) | 44 (14.52) | |||
| Triage Acute Scale | Priority I | 10 (5.0) | 16 (16.5) | 26 (8.8) | <0.001 * | |
| Priority II | 131 (66.2) | 72 (74.2) | 203 (68.8) | |||
| Priority III | 57 (28.8) | 9 (9.3) | 66 (22.4) | |||
| Variable | OR | 95% CI | p-Value | ||
|---|---|---|---|---|---|
| Intercept | 0.232 | 0.015 | 3.649 | 0.299 | |
| Mode of arrival at ED (Ambulance = reference) | |||||
| Others | 0.685 | 0.083 | 5.676 | 0.726 | |
| Own car | 0.623 | 0.172 | 2.258 | 0.471 | |
| Family/friend car | 1.356 | 0.362 | 5.088 | 0.651 | |
| Clinical condition (Non-urgent = reference) | |||||
| Urgent | 2.370 | 1.181 | 4.756 | 0.015 * | |
| Comorbidity (None = reference) | |||||
| One | 0.952 | 0.393 | 2.304 | 0.913 | |
| Two | 1.356 | 0.378 | 4.863 | 0.640 | |
| Gender (Female = reference) | |||||
| Male | 1.271 | 0.624 | 2.592 | 0.509 | |
| Age category (≤ 50 years = reference) | |||||
| ≥50 years | 1.689 | 0.654 | 4.357 | 0.279 | |
| Marital status (Others = reference) | |||||
| Married | 0.787 | 0.354 | 1.750 | 0.558 | |
| Residence (Outside Riyadh = reference) | |||||
| Riyadh | 1.419 | 0.580 | 3.473 | 0.443 | |
| Household income SAR (<3000 reference) | |||||
| 3000 to 5000 | 3.049 | 1.177 | 7.898 | 0.022 * | |
| 5001 to 10,000 | 5.367 | 1.922 | 14.989 | 0.001 * | |
| 10,001 to 15,000 | 3.434 | 0.725 | 16.269 | 0.120 | |
| >15,000 | 1.436 | 0.242 | 8.512 | 0.690 | |
| Schooling level (No schooling = reference) | |||||
| Elementary | 0.541 | 0.164 | 1.784 | 0.313 | |
| Primary | 0.657 | 0.204 | 2.116 | 0.481 | |
| High school | 0.359 | 0.117 | 1.104 | 0.074 | |
| Higher Education | 0.625 | 0.165 | 2.371 | 0.490 | |
| Employement (Otherwise = reference) | |||||
| Employment | Employed | 1.525 | 0.534 | 4.356 | 0.431 |
| Insurance (Others = reference) | |||||
| Insurance | NGHA | 1.086 | 0.271 | 4.356 | 0.908 |
| Hospitalization (More than 12 months = reference) | |||||
| Last 12 months | 3.026 | 1.513 | 6.055 | 0.002 * | |
| Frequency of ED visits (Once = reference) | |||||
| Frequency of ED visits | More than once | 0.928 | 0.440 | 1.957 | 0.844 |
| Health status (Poor = reference) | |||||
| Very good/Excellent | 0.411 | 0.066 | 2.563 | 0.341 | |
| Fair/good | 0.595 | 0.125 | 2.835 | 0.515 | |
| Social healp (No care = reference) | |||||
| Get care when needed | 1.206 | 0.569 | 2.556 | 0.625 | |
| CTAS (High priority = reference) | |||||
| Moderate priority | 0.426 | 0.153 | 1.189 | 0.103 | |
| Lower priority | 0.277 | 0.077 | 0.996 | 0.049 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alahmary, K.; Kadasah, S.; Alsulami, A.; Alshehri, A.M.; Alsalamah, M.; Da’ar, O.B. To Admit or Not to Admit to the Emergency Department: The Disposition Question at a Tertiary Teaching and Referral Hospital. Healthcare 2023, 11, 667. https://doi.org/10.3390/healthcare11050667
Alahmary K, Kadasah S, Alsulami A, Alshehri AM, Alsalamah M, Da’ar OB. To Admit or Not to Admit to the Emergency Department: The Disposition Question at a Tertiary Teaching and Referral Hospital. Healthcare. 2023; 11(5):667. https://doi.org/10.3390/healthcare11050667
Chicago/Turabian StyleAlahmary, Khalid, Sarah Kadasah, Abdulrahman Alsulami, Ali M. Alshehri, Majid Alsalamah, and Omar B. Da’ar. 2023. "To Admit or Not to Admit to the Emergency Department: The Disposition Question at a Tertiary Teaching and Referral Hospital" Healthcare 11, no. 5: 667. https://doi.org/10.3390/healthcare11050667
APA StyleAlahmary, K., Kadasah, S., Alsulami, A., Alshehri, A. M., Alsalamah, M., & Da’ar, O. B. (2023). To Admit or Not to Admit to the Emergency Department: The Disposition Question at a Tertiary Teaching and Referral Hospital. Healthcare, 11(5), 667. https://doi.org/10.3390/healthcare11050667






