Health Status and Activity Discomfort among Elderly Drivers: Reality of Health Awareness
Abstract
1. Introduction
2. Materials and Methods
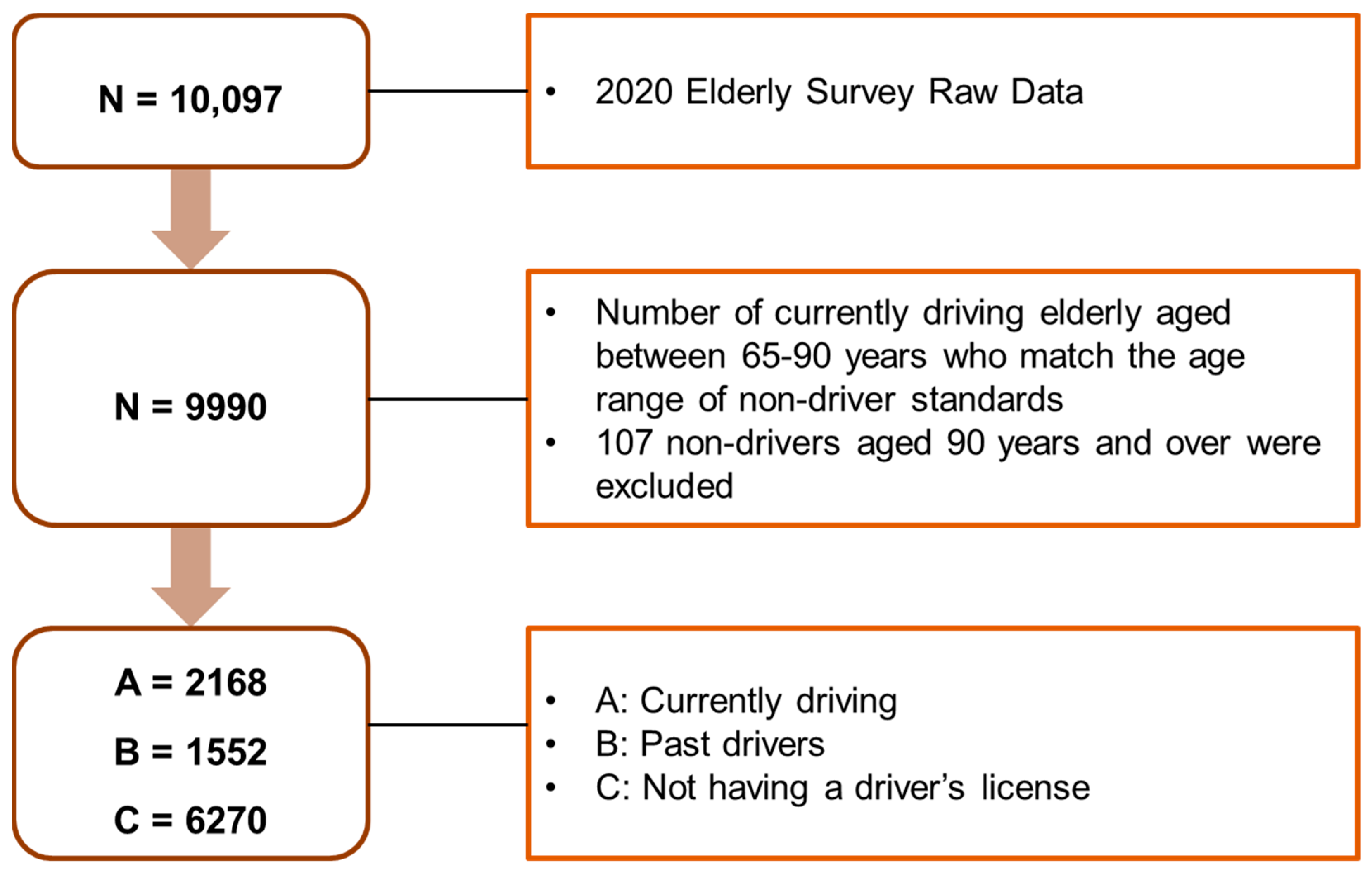
2.1. Study Design and Sampling
2.2. Data Variables
- (1)
- Driving status, which was divided into two groups: past drivers (not currently driving) and not having a driver’s license.
- (2)
- Health status and health behavior, which included thoughts on health in general; presence of chronic diseases (diseases lasting for more than 3 months as diagnosed by a doctor, namely circulatory diseases: high blood pressure, stroke (stroke, cerebral infarction), hyperlipidemia (dyslipidemia), angina pectoris, and myocardial infarction (heart failure and arrhythmia); endocrinal disease: diabetes and thyroid disease; musculoskeletal diseases: osteoarthritis (degenerative arthritis), rheumatoid arthritis, osteoporosis, low back pain, sciatica, fracture, dislocation, and after effects of accidents; respiratory diseases: chronic bronchitis, emphysema, asthma, pulmonary tuberculosis, and tuberculosis, neuropsychiatric diseases: depression, dementia, Parkinson’s disease, and insomnia; sensory diseases: cataract, glaucoma, chronic otitis media, senile deafness, skin disease, and cancer (malignant neoplasm); digestive diseases: gastroduodenal ulcer, hepatitis, and liver cirrhosis; genitourinary diseases: chronic kidney disease, prostatic hyperplasia, urinary incontinence, and anemia, etc.
- (3)
- State of physical function, including eyesight (watching TV, reading newspapers), hearing (talking on the phone, talking to the person next to you), chewing (chewing meat or hard things), and determining muscle strength (active movement (running about one lap (400 m) on the playground), walking around the playground (400 m), climbing 10 steps without a break, bending over, squatting, or kneeling, and reaching out for something higher than one’s head). Physical functioning was divided into lifting, moving, and disability determination.
- (4)
- Depressive symptoms were measured using the shortened geriatric depression scale (SGDS)-K15, which is a Korean translation of the SGDS developed by [19] to evaluate depressive symptoms in the elderly population (out of a total score of 15, individuals with a score of 8 or higher were classified as having depressive symptoms).
- (5)
- Social activities and discomfort in social activities were classified into two categories, namely, difficulty in using the information necessary for life and the inconvenience caused by using information technology in everyday life.
- (6)
- Economic activity was classified into current income, work, and desired work.
- (7)
- Precognitive function: cognitive function was confirmed and measured using the Mini-Mental State Examination for Dementia Screening (MMSE-DS) test tool. A representative screening test developed by [20] is widely used for simple and rapid measurement as well as screening for any cognitive impairment; the standardized Korean version of the mini-mental state examination (MMSE-K) [21], the Korean mini-mental state examination (K-MMSE) [22], and the mini-mental state examination-Korean children (MMSE-KC) [23] have been used in the Republic of Korea. A total mini-mental state examination (MMSE) score of 30 points is considered the cut-off point for cognitive impairment; a score of 0–10 indicates severe cognitive impairment, 10–20 indicates moderate cognitive impairment, 20–24 indicates mild cognitive impairment, and 24–30 indicates no cognitive impairment [14].
- (8)
- General characteristics, such as gender, height (cm), weight (kg), body mass index (kg/m²), drinking, smoking, education level, subjective age of the elderly, suicidal ideation, and health-type factors, were obtained.
2.3. Data Analysis
3. Results
3.1. General Characteristics
3.2. Current Disease Status and Their Treatment
3.3. Physical Function Status and Discomfort in Daily Life
3.4. Depressive Symptom
3.5. Economic Activity
3.6. Recognition Function
3.7. Current Drivers
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korean Statistical Information Service (KOSIS), 2019. Available online: http://kosis.kr/statHtmlstatHtml/statHtml.do?or-Id=101&tblId=DT_1BPA002&checkFlag=N/ (accessed on 5 October 2022).
- Baldock, M.R.; McLean, J. Older Drivers: Crash Involvement Rates and Causes; Centre for Automotive Safety Research: Adelaide, Australia, 2005. [Google Scholar]
- Gagliardi, C.; Marcellini, F.; Papa, R.; Giuli, C.; Mollenkopf, H. Associations of personal and mobility resources with subjective well-being among older adults in Italy and Germany. Arch Gerontol Geriatr. 2010, 50, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Park, H.C.; Yoo, M.H.; Lim, S.I.; Hwang, E.J.; Kim, E.S.; Choi, K.I.; Choi, K.J.; Lee, D.J. Driving status, habits and safety of older drivers. J. Korean Acad. Rehabil. Med. 2010, 34, 570–576. [Google Scholar]
- Lee, S.E. Factors affecting traffic accident anxiety of older drivers. (JNCIST) J. Next-Gener. Converg. Inf. Serv. Technol. 2019, 8, 263–272. [Google Scholar] [CrossRef]
- Ahmed, H.I.; Mohamed, E.E.; Aly, A.M. Effect of mobility on the quality of life among older adults in geriatric home at Makkah al-Mukarramah. Adv. Life Sci. Technol. 2014, 17, 39–50. [Google Scholar]
- Traffic Accident Analysis System (TAAS). 2019. Available online: http://taas.koroad.or.kr/sta/acs/gus/selectOdsnDrverTfcacd.do?menuId=WEB_KMP_OVT_MVT_TAS_ODT/ (accessed on 5 October 2022).
- Donorfio, L.K.M.; D’Ambrosio, L.A.; Coughlin, J.F.; Mohyde, M. To drive or not to drive, that isn’t the question—The meaning of self-regulation among older drivers. J. Safety Res. 2009, 40, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Heo, T.Y. Analysis on the auto accident risks of the old. Korean Soc. Transp. 2015, 33, 100–111. [Google Scholar] [CrossRef]
- Charlton, J.L. Characteristics of older drivers who adopt self-regulatory driving behaviours. Transp Res. F. 2006, 9, 363–373. [Google Scholar] [CrossRef]
- Choi, S.Y. Analyzing driving risk self-perception characteristics of elderly drivers. J. Converg. Inf. Technol. 2020, 10, 223–231. [Google Scholar] [CrossRef]
- Pachana, N.A.; Petriwskyj, A.M. Assessment of insight and self-awareness in older drivers. Clin. Gerontol. 2006, 30, 23–38. [Google Scholar] [CrossRef]
- Molnar, L.J.; Eby, D.W.; Kartje, P.S.; St Louis, R.M.S. Increasing self-awareness among older drivers: The role of self-screening. J. Safety Res. 2010, 41, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Donorfio, L.K.M.; Mohyde, M.; Coughlin, J.; D’Ambrosio, L. A qualitative exploration of self-regulation behaviors among older drivers. J. Aging Soc. Policy 2008, 20, 323–339. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.A.; Clay, O.J.; Edwards, J.D.; Ball, K.K.; Wadley, V.G.; Vance, D.E.; Cissell, G.M.; Roenker, D.L.; Joyce, J.J. Do older drivers at-risk for crashes modify their driving over time? J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, 163–170. [Google Scholar] [CrossRef]
- Factor, R.; Mahalel, D.; Yair, G. The social accident: A theoretical model and a research agenda for studying the influence of social and cultural characteristics on motor vehicle accidents. Accid. Anal. Prev. 2007, 39, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Lee, J.S.; Kim, S.K.; Cha, T.H.; Yoo, D.H.; Kim, H. Developing a self-questionnaire SAFE-DR to evaluate driving ability of Korean elderly driver. Asia Life Sci. 2020, 29, 1–14. [Google Scholar]
- Meuleners, L.B.; Harding, A.; Lee, A.H.; Legge, M. Fragility and crash over-representation among older drivers in Western Australia. Accid. Anal. Prev. 2006, 38, 1006–1010. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Folstein, M.F.; Robins, L.N.; Helzer, J.E. The Mini-Mental State Examination. Arch. Gen. Psychiatry 1983, 40, 812. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.C. Korean version of mini-mental state examination (MMSE-K). J. Korean Neurol. Assoc. 1989, 1, 123–135. [Google Scholar]
- Kang, Y.; NA, D.-L.; Hahn, S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J. Korean Neurol. Assoc. 1997, 15, 300–308. [Google Scholar]
- LEE, D.-Y.; LEE, K.-U.; LEE, J.-H.; KIM, K.-W.; JHOO, J.-H.; YOUN, J.-C.; KIM, S.-Y.; WOO, S.-I.; WOO, J.-I. A normative study of the mini-mental state examination in the Korean elderly. J. Korean Neuropsychiatr. Assoc. 2002, 41, 508–525. [Google Scholar]
| Characteristics | Driving | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Current Drivers | Past But Not Current Drivers | No Driver’s License | X2 3/H 4 | p-Value | |||||
| N 5/M 1 | %/SD 2 | N/M | %/SD | N/M | %/SD | ||||
| Sex | Man | 1729 | 79.8 | 1237 | 79.7 | 1045 | 16.7 | 3864.248 | <0.001 |
| Female | 439 | 20.2 | 315 | 20.3 | 5225 | 83.3 | |||
| Height (cm) | 167.68 | 6.77 | 166.22 | 6.92 | 157.29 | 7.13 | 3209.849 | <0.001 | |
| Weight (kg) | 66.74 | 7.56 | 65.02 | 7.78 | 58.29 | 7.98 | 1940.261 | <0.001 | |
| Body mass index (BMI) | 23.71 | 2.09 | 23.52 | 2.35 | 23.55 | 2.82 | 13.557 | 0.001 | |
| Age (years) | 69.34 | 4.22 | 74.08 | 5.74 | 74.58 | 6.54 | 1192.218 | <0.001 | |
| Recognition of elderly age criteria | 71.32 | 4.60 | 69.72 | 4.14 | 70.02 | 4.04 | 167.758 | <0.001 | |
| Education Level | Uneducated (not reading) | 0 | 0 | 7 | 0.5 | 297 | 4.7 | 2320.532 | <0.001 |
| Uneducated (reading) | 10 | 0.5 | 50 | 3.2 | 739 | 11.8 | |||
| Elementary school | 261 | 12.0 | 394 | 25.4 | 2694 | 43.0 | |||
| Middle school | 483 | 22.3 | 431 | 27.8 | 1447 | 23.1 | |||
| High school | 1109 | 51.2 | 544 | 35.1 | 1013 | 16.2 | |||
| College | 126 | 5.8 | 41 | 2.6 | 36 | 0.6 | |||
| University | 179 | 8.3 | 85 | 5.5 | 44 | 0.7 | |||
| Disability | Yes | 51 | 2.4 | 92 | 5.9 | 301 | 4.8 | 32.257 | <0.001 |
| No | 2117 | 97.6 | 1460 | 94.1 | 5969 | 95.2 | |||
| Degree of disability | Severe disability (1–3 degree) | 7 | 13.7 | 29 | 31.5 | 68 | 22.6 | 6.154 | 0.046 |
| Moderate disability (4–6 degree) | 44 | 86.3 | 63 | 68.5 | 233 | 77.4 | |||
| Disability type | Mental retardation | 32 | 62.7 | 50 | 54.3 | 175 | 58.1 | - | - |
| Brain lesion disorder | 1 | 2.0 | 8 | 8.7 | 19 | 6.3 | |||
| Visual impairment | 3 | 5.9 | 6 | 6.5 | 26 | 8.6 | |||
| Deafness | 11 | 21.6 | 16 | 17.4 | 51 | 16.9 | |||
| Speech disorders | 0 | 0.0 | 1 | 1.1 | 4 | 1.3 | |||
| Intellectual disability | 0 | 0.0 | 1 | 1.1 | 5 | 1.7 | |||
| Autistic disorders | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| Mental disorders | 0 | 0.0 | 1 | 1.1 | 6 | 2.0 | |||
| Renal failure | 1 | 2.0 | 2 | 2.2 | 6 | 2.0 | |||
| Heart disorders | 0 | 0.0 | 2 | 2.2 | 5 | 1.7 | |||
| Respiratory disorders | 2 | 3.9 | 3 | 3.3 | 1 | 0.3 | |||
| Hepatic impairment | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| Facial disorders | 0 | 0.0 | 1 | 1.1 | 0 | 0.0 | |||
| Stoma disorder | 1 | 2.0 | 1 | 1.1 | 2 | 0.7 | |||
| Epilepsy disorder | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | |||
| Regular exercise | Yes | 1364 | 62.9 | 910 | 58.6 | 2951 | 47.1 | 191.752 | <0.001 |
| No | 804 | 37.1 | 642 | 41.4 | 3319 | 52.9 | |||
| Exercise time(min) / (1 time) | 57 | 28 | 48 | 28 | 44 | 24 | 272.011 | <0.001 | |
| Exercise frequency in 1 week | 1 time | 40 | 2.9 | 15 | 1.6 | 58 | 2.0 | 25.204 | 0.014 |
| 2 times | 141 | 10.3 | 85 | 9.3 | 242 | 8.2 | |||
| 3 times | 287 | 21.0 | 207 | 22.7 | 595 | 20.2 | |||
| 4 times | 102 | 7.5 | 63 | 6.9 | 222 | 7.5 | |||
| 5 times | 370 | 27.1 | 212 | 23.3 | 794 | 26.9 | |||
| 6 times | 93 | 6.8 | 86 | 9.5 | 270 | 9.1 | |||
| 7 times | 331 | 24.3 | 242 | 26.6 | 770 | 26.1 | |||
| Smoking | Yes | 514 | 23.7 | 278 | 17.9 | 310 | 4.9 | 666.616 | <0.001 |
| No | 1654 | 76.3 | 1274 | 82.1 | 5960 | 95.1 | |||
| Average amount of alcohol consumed (oz) | 4.46 | 2.40 | 4.07 | 2.17 | 3.21 | 1.98 | 290.814 | <0.001 | |
| Health status | Very healthy | 247 | 11.4 | 54 | 3.5 | 131 | 2.1 | 889.457 | <0.001 |
| Healthy | 1351 | 62.5 | 695 | 45.6 | 2445 | 39.8 | |||
| Normal | 450 | 20.8 | 497 | 32.6 | 2139 | 34.8 | |||
| Bad | 113 | 5.2 | 234 | 15.4 | 1286 | 20.9 | |||
| Very bad | 1 | 0.0 | 43 | 2.8 | 145 | 2.4 | |||
| Characteristics | Driving | X2 3/H 4 | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Current Drivers | Past But Not Current Drivers | No Driver’s License | |||||||
| N 5/M 1 | %/SD 2 | N/M | %/SD | N/M | %/SD | ||||
| Doctor’s diagnosis of hypertension | Yes | 1134 | 52.3 | 899 | 57.9 | 3710 | 59.2 | 31.204 | <0.001 |
| No | 1034 | 47.7 | 653 | 42.1 | 2560 | 40.8 | |||
| Treatment of hypertension | Yes | 1121 | 98.9 | 893 | 99.3 | 3657 | 98.6 | 3.518 | 0.172 |
| No | 13 | 1.1 | 6 | 0.7 | 53 | 1.4 | |||
| Doctor’s diagnosis of stroke (Stroke, cerebral infarction) | Yes | 37 | 1.7 | 81 | 5.2 | 295 | 4.7 | 41.999 | <0.001 |
| No | 2131 | 98.3 | 1471 | 94.8 | 5975 | 95.3 | |||
| Treatment of stroke (Stroke, cerebral infarction) | Yes | 37 | 100.0 | 80 | 98.8 | 285 | 96.6 | 2.251 | 0.325 |
| No | 0 | 0.0 | 1 | 1.2 | 10 | 3.4 | |||
| Doctor’s diagnosis of hyperlipidemia (dyslipidemia) | Yes | 324 | 14.9 | 193 | 12.4 | 1188 | 18.9 | 46.082 | <0.001 |
| No | 1844 | 85.1 | 1359 | 87.6 | 5082 | 81.1 | |||
| Treatment of hyperlipidemia (dyslipidemia) | Yes | 313 | 96.6 | 190 | 98.4 | 1164 | 98.0 | 2.662 | 0.264 |
| No | 11 | 3.4 | 3 | 1.6 | 24 | 2.0 | |||
| Doctor’s diagnosis of angina pectoris and myocardial infarction | Yes | 76 | 3.5 | 69 | 4.4 | 312 | 5.0 | 8.050 | 0.018 |
| No | 2092 | 96.5 | 1483 | 95.6 | 5958 | 95.0 | |||
| Treatment of angina pectoris and myocardial infarction | Yes | 74 | 97.4 | 67 | 97.1 | 306 | 98.1 | 0.335 | 0.846 |
| No | 2 | 2.6 | 2 | 2.9 | 6 | 1.9 | |||
| Doctor’s diagnosis of heart diseases | Yes | 65 | 3.0 | 63 | 4.1 | 329 | 5.2 | 19.785 | <0.001 |
| No | 2103 | 97.0 | 1489 | 95.9 | 5941 | 94.8 | |||
| Treatment of heart diseases | Yes | 63 | 96.9 | 62 | 98.4 | 327 | 99.4 | 3.222 | 0.200 |
| No | 2 | 3.1 | 1 | 1.6 | 2 | 0.6 | |||
| Doctor’s diagnosis of diabetes | Yes | 421 | 19.4 | 401 | 25.8 | 1581 | 25.2 | 32.829 | <0.001 |
| No | 1747 | 80.6 | 1151 | 74.2 | 4689 | 74.8 | |||
| Treatment of diabetes | Yes | 419 | 99.5 | 401 | 100.0 | 1557 | 98.5 | 8.644 | 0.013 |
| No | 2 | 0.5 | 0 | 0.0 | 24 | 1.5 | |||
| Doctor’s diagnosis of thyroid disease | Yes | 36 | 1.7 | 38 | 2.4 | 235 | 3.7 | 25.968 | <0.001 |
| No | 2132 | 98.3 | 1514 | 97.6 | 6035 | 96.3 | |||
| Treatment of thyroid disease | Yes | 34 | 94.4 | 37 | 97.4 | 231 | 98.3 | 2.120 | 0.346 |
| No | 2 | 5.6 | 1 | 2.6 | 4 | 1.7 | |||
| Doctor’s diagnosis of osteoarthritis (Degenerative arthritis) | Yes | 140 | 6.5 | 143 | 9.2 | 1288 | 20.5 | 299.936 | <0.001 |
| No | 2028 | 93.5 | 1409 | 90.8 | 4982 | 79.5 | |||
| Treatment of osteoarthritis (Degenerative arthritis) | Yes | 126 | 90.0 | 133 | 93.0 | 1193 | 92.6 | 1.318 | 0.517 |
| No | 14 | 10.0 | 10 | 7.0 | 95 | 7.4 | |||
| Doctor’s diagnosis of osteoporosis | Yes | 50 | 2.3 | 73 | 4.7 | 701 | 11.2 | 198.134 | <0.001 |
| No | 2118 | 97.7 | 1479 | 95.3 | 5569 | 88.8 | |||
| Treatment of osteoporosis | Yes | 44 | 88.0 | 68 | 93.2 | 650 | 92.7 | 1.550 | 0.461 |
| No | 6 | 12.0 | 5 | 6.8 | 51 | 7.3 | |||
| Doctor’s diagnosis of low back pain and sciatica | Yes | 75 | 3.5 | 95 | 6.1 | 776 | 12.4 | 173.448 | <0.001 |
| No | 2093 | 96.5 | 1457 | 93.9 | 5494 | 87.6 | |||
| Treatment of low back pain and sciatica | Yes | 63 | 84.0 | 88 | 92.6 | 651 | 83.9 | 5.048 | 0.080 |
| No | 12 | 16.0 | 7 | 7.4 | 125 | 16.1 | |||
| Doctor’s diagnosis of fracture, dislocation, and aftereffects of accidents | Yes | 17 | 0.8 | 19 | 1.2 | 93 | 1.5 | 6.242 | 0.044 |
| No | 2151 | 99.2 | 1533 | 98.8 | 6177 | 98.5 | |||
| Treatment of fracture, dislocation, and aftereffects of accidents | Yes | 15 | 88.2 | 16 | 84.2 | 83 | 89.2 | 0.390 | 0.823 |
| No | 2 | 11.8 | 3 | 15.8 | 10 | 10.8 | |||
| Doctor’s diagnosis of fracture, chronic bronchitis, and emphysema | Yes | 37 | 1.7 | 34 | 2.2 | 51 | 0.8 | 24.973 | <0.001 |
| No | 2131 | 98.3 | 1518 | 97.8 | 6219 | 99.2 | |||
| Treatment of chronic bronchitis and emphysema | Yes | 34 | 91.9 | 33 | 97.1 | 45 | 88.2 | 2.111 | 0.348 |
| No | 3 | 8.1 | 1 | 2.9 | 6 | 11.8 | |||
| Doctor’s diagnosis of asthma | Yes | 19 | 0.9 | 40 | 2.6 | 116 | 1.9 | 16.151 | <0.001 |
| No | 2149 | 99.1 | 1512 | 97.4 | 6154 | 98.1 | |||
| Treatment of asthma | Yes | 17 | 89.5 | 37 | 92.5 | 110 | 94.8 | 0.924 | 0.630 |
| No | 2 | 10.5 | 3 | 7.5 | 6 | 5.2 | |||
| Doctor’s diagnosis of pulmonary tuberculosis | Yes | 1 | 0.0 | 4 | 0.3 | 7 | 0.1 | 3.477 | 0.176 |
| No | 2167 | 100.0 | 1548 | 99.7 | 6263 | 99.9 | |||
| Treatment of pulmonary tuberculosis | Yes | 0 | 0.0 | 3 | 75.0 | 7 | 100.0 | 6.600 | 0.037 |
| No | 1 | 100.0 | 1 | 25.0 | 0 | 0.0 | |||
| Doctor’s diagnosis of depression | Yes | 6 | 0.3 | 22 | 1.4 | 113 | 1.8 | 26.942 | <0.001 |
| No | 2162 | 99.7 | 1530 | 98.6 | 6157 | 98.2 | |||
| Treatment of depression | Yes | 6 | 100.0 | 18 | 81.8 | 100 | 88.5 | 1.634 | 0.442 |
| No | 0 | 0.0 | 4 | 18.2 | 13 | 11.5 | |||
| Doctor’s diagnosis of dementia | Yes | 8 | 0.4 | 27 | 1.7 | 137 | 2.2 | 31.401 | <0.001 |
| No | 2160 | 99.6 | 1525 | 98.3 | 6133 | 97.8 | |||
| Treatment of dementia | Yes | 7 | 87.5 | 27 | 100.0 | 131 | 95.6 | 2.635 | 0.268 |
| No | 1 | 12.5 | 0 | 0.0 | 6 | 4.4 | |||
| Doctor’s diagnosis of Parkinson’s disease | Yes | 0 | 0.0 | 17 | 1.1 | 32 | 0.5 | 22.371 | <0.001 |
| No | 2168 | 100.0 | 1535 | 98.9 | 6238 | 99.5 | |||
| Treatment of Parkinson’s disease | Yes | 0 | 0.0 | 17 | 100.0 | 32 | 100.0 | - | - |
| No | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| Doctor’s diagnosis of insomnia | Yes | 29 | 1.3 | 31 | 2.0 | 130 | 2.1 | 4.764 | 0.092 |
| No | 2139 | 98.7 | 1521 | 98.0 | 6140 | 97.9 | |||
| Treatment of insomnia | Yes | 22 | 75.9 | 25 | 80.6 | 106 | 81.5 | 0.488 | 0.784 |
| No | 7 | 24.1 | 6 | 19.4 | 24 | 18.5 | |||
| Doctor’s diagnosis of cataract | Yes | 93 | 4.3 | 70 | 4.5 | 282 | 4.5 | 0.177 | 0.915 |
| No | 2075 | 95.7 | 1482 | 95.5 | 5988 | 95.5 | |||
| Treatment of cataract | Yes | 78 | 83.9 | 57 | 81.4 | 205 | 72.7 | 6.008 | 0.050 |
| No | 15 | 16.1 | 13 | 18.6 | 77 | 27.3 | |||
| Doctor’s diagnosis of glaucoma | Yes | 18 | 0.8 | 21 | 1.4 | 50 | 0.8 | 4.465 | 0.107 |
| No | 2150 | 99.2 | 1531 | 98.6 | 6220 | 99.2 | |||
| Treatment of glaucoma | Yes | 14 | 77.8 | 20 | 95.2 | 40 | 80.0 | 2.914 | 0.233 |
| No | 4 | 22.2 | 1 | 4.8 | 10 | 20.0 | |||
| Doctor’s diagnosis of chronic otitis media | Yes | 16 | 0.7 | 13 | 0.8 | 27 | 0.4 | 5.261 | 0.072 |
| No | 2152 | 99.3 | 1539 | 99.2 | 6243 | 99.6 | |||
| Treatment of chronic otitis media | Yes | 16 | 100.0 | 13 | 100.0 | 26 | 96.3 | 1.094 | 0.579 |
| No | 0 | 0.0 | 0 | 0.0 | 1 | 3.7 | |||
| Doctor’s diagnosis of senile deafness | Yes | 15 | 0.7 | 48 | 3.1 | 146 | 2.3 | 30.050 | <0.001 |
| No | 2153 | 99.3 | 1504 | 96.9 | 6124 | 97.7 | |||
| Treatment of senile deafness | Yes | 9 | 60.0 | 33 | 68.8 | 83 | 56.8 | 2.129 | 0.345 |
| No | 6 | 40.0 | 15 | 31.3 | 63 | 43.2 | |||
| Doctor’s diagnosis of skin disease | Yes | 23 | 1.1 | 15 | 1.0 | 29 | 0.5 | 11.072 | 0.004 |
| No | 2145 | 98.9 | 1537 | 99.0 | 6241 | 99.5 | |||
| Treatment of skin disease | Yes | 20 | 87.0 | 15 | 100.0 | 23 | 79.3 | 3.478 | 0.173 |
| No | 3 | 13.0 | 0 | 0.0 | 6 | 20.7 | |||
| Doctor’s diagnosis of cancer (malignant neoplasm) | Yes | 33 | 1.5 | 39 | 2.5 | 95 | 1.5 | 7.911 | 0.019 |
| No | 2135 | 98.5 | 1513 | 97.5 | 6175 | 98.5 | |||
| Treatment of cancer (malignant neoplasm) | Yes | 30 | 90.9 | 36 | 92.3 | 81 | 85.3 | 1.345 | 0.548 |
| No | 3 | 9.1 | 3 | 7.7 | 14 | 14.7 | |||
| Doctor’s diagnosis of gastroduodenal ulcer | Yes | 94 | 4.3 | 69 | 4.4 | 272 | 4.3 | 0.037 | 0.982 |
| No | 2074 | 95.7 | 1483 | 95.6 | 5998 | 95.7 | |||
| Treatment of gastroduodenal ulcer | Yes | 90 | 95.7 | 66 | 95.7 | 253 | 93.0 | 1.314 | 0.518 |
| No | 4 | 4.3 | 3 | 4.3 | 19 | 7.0 | |||
| Doctor’s diagnosis of hepatitis | Yes | 6 | 0.3 | 5 | 0.3 | 22 | 0.4 | 0.273 | 0.873 |
| No | 2162 | 99.7 | 1547 | 99.7 | 6248 | 99.6 | |||
| Treatment of hepatitis | Yes | 5 | 83.3 | 3 | 60.0 | 21 | 95.5 | 4.675 | 0.056 |
| No | 1 | 16.7 | 2 | 40.0 | 1 | 4.5 | |||
| Doctor’s diagnosis of liver cirrhosis | Yes | 5 | 0.2 | 11 | 0.7 | 15 | 0.2 | 9.434 | 0.009 |
| No | 2163 | 99.8 | 1541 | 99.3 | 6255 | 99.8 | |||
| Treatment of liver cirrhosis | Yes | 5 | 100.0 | 11 | 100.0 | 14 | 93.3 | 1.428 | 1.000 |
| No | 0 | 0.0 | 0 | 0.0 | 1 | 6.7 | |||
| Doctor’s diagnosis of chronic kidney disease | Yes | 9 | 0.4 | 30 | 1.9 | 55 | 0.9 | 23.091 | <0.001 |
| No | 2159 | 99.6 | 1522 | 98.1 | 6215 | 99.1 | |||
| Treatment of chronic kidney disease | Yes | 9 | 100.0 | 28 | 93.3 | 54 | 98.2 | 1.663 | 0.472 |
| No | 0 | 0.0 | 2 | 6.7 | 1 | 1.8 | |||
| Doctor’s diagnosis of prostatic hyperplasia | Yes | 118 | 5.4 | 123 | 7.9 | 100 | 1.6 | 185.803 | <0.001 |
| No | 2050 | 94.6 | 1429 | 92.1 | 6170 | 98.4 | |||
| Treatment of prostatic hyperplasia | Yes | 110 | 93.2 | 119 | 96.7 | 97 | 97.0 | 2.440 | 0.295 |
| No | 8 | 6.8 | 4 | 3.3 | 3 | 3.0 | |||
| Doctor’s diagnosis of urinary incontinence | Yes | 19 | 0.9 | 27 | 1.7 | 266 | 4.2 | 71.951 | <0.001 |
| No | 2149 | 99.1 | 1525 | 98.3 | 6004 | 95.8 | |||
| Treatment of urinary incontinence | Yes | 9 | 47.4 | 18 | 66.7 | 125 | 47.0 | 3.812 | 0.419 |
| No | 10 | 52.6 | 9 | 33.3 | 141 | 53.0 | |||
| Doctor’s diagnosis of anemia | Yes | 13 | 0.6 | 23 | 1.5 | 93 | 1.5 | 10.392 | 0.006 |
| No | 2155 | 99.4 | 1529 | 98.5 | 6177 | 98.5 | |||
| Treatment of anemia | Yes | 10 | 76.9 | 22 | 95.7 | 76 | 81.7 | 3.279 | 0.175 |
| No | 3 | 23.1 | 1 | 4.3 | 17 | 18.3 | |||
| Doctor’s diagnosis of ETC | Yes | 40 | 1.8 | 24 | 1.5 | 128 | 2.0 | 1.704 | 0.426 |
| No | 2128 | 98.2 | 1528 | 98.5 | 6142 | 98.0 | |||
| Treatment of ETC | Yes | 36 | 90.0 | 24 | 100.0 | 122 | 95.3 | 2.670 | 0.273 |
| No | 4 | 10.0 | 0 | 0.0 | 6 | 4.7 | |||
| Doctor’s diagnosis total number | 1.37 | 1.24 | 1.78 | 1.50 | 2.02 | 1.50 | 356.311 | <0.001 | |
| Prescription medication that currently taking for more than 3 months | 1.31 | 1.20 | 1.78 | 1.74 | 1.94 | 1.55 | 315.923 | <0.001 | |
| Characteristics | Driving | X2 3/H 4 | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Current Drivers | Past But Not Current Drivers | No Driver’s License | |||||||
| N 1 | % 2 | N/M | % | N/M | % | ||||
| Assisted with eyesight | Yes | 1142 | 52.7 | 890 | 57.3 | 3247 | 51.8 | 15.459 | <0.001 |
| No | 1026 | 47.3 | 662 | 42.7 | 3023 | 48.2 | |||
| Assisted with hearing | Yes | 167 | 7.7 | 199 | 12.8 | 747 | 11.9 | 34.099 | <0.001 |
| No | 2001 | 92.3 | 1353 | 87.2 | 5523 | 88.1 | |||
| Assisted with chewing | Yes | 530 | 24.4 | 558 | 36.0 | 2546 | 40.6 | 181.906 | <0.001 |
| No | 1638 | 75.6 | 994 | 64.0 | 3724 | 59.4 | |||
| Discomfort of eyesight | Not uncomfortable | 1602 | 74.1 | 1015 | 66.6 | 3981 | 64.8 | 68.161 | <0.001 |
| Uncomfortable | 524 | 24.2 | 465 | 30.5 | 2039 | 33.2 | |||
| Very uncomfortable | 36 | 1.7 | 43 | 2.8 | 126 | 2.1 | |||
| Discomfort of hearing | Not uncomfortable | 1835 | 84.9 | 1140 | 74.9 | 4612 | 75.0 | 97.336 | <0.001 |
| Uncomfortable | 308 | 14.2 | 343 | 22.5 | 1400 | 22.8 | |||
| Very uncomfortable | 19 | 0.9 | 40 | 2.6 | 134 | 2.2 | |||
| Discomfort of chewing | Not uncomfortable | 1611 | 74.5 | 934 | 61.3 | 3608 | 58.7 | 173.696 | <0.001 |
| Uncomfortable | 501 | 23.2 | 522 | 34.3 | 2252 | 36.6 | |||
| Very uncomfortable | 50 | 2.3 | 67 | 4.4 | 286 | 4.7 | |||
| Muscle strength when sitting in a chair or bed and then getting up 5 times | Performed | 2008 | 92.6 | 1126 | 72.6 | 4174 | 66.6 | 586.185 | <0.001 |
| Tried but failed to perform (5 times not successful) | 82 | 3.8 | 302 | 19.5 | 1594 | 25.4 | |||
| Inability to even attempt to perform (elderly people with a vortex, or other disabilities that make it impossible to stand up) | 10 | 0.5 | 43 | 2.8 | 174 | 2.8 | |||
| Want to do it now | 68 | 3.1 | 81 | 5.2 | 328 | 5.2 | |||
| Difficulty in performing movements such as jumping one lap (400 m) on the playground | Not difficult at all | 576 | 26.6 | 189 | 12.2 | 454 | 7.2 | 1193.227 | <0.001 |
| Slightly difficult | 882 | 40.7 | 437 | 28.2 | 1371 | 21.9 | |||
| Very difficult | 508 | 23.4 | 580 | 37.4 | 2414 | 38.5 | |||
| Cannot do it at all | 163 | 7.5 | 304 | 19.6 | 1920 | 30.6 | |||
| Do now | 39 | 1.8 | 42 | 2.7 | 111 | 1.8 | |||
| Difficulty performing movements such as walking one lap (400 m) on the playground | Not difficult at all | 1606 | 74.1 | 807 | 52.0 | 2493 | 39.8 | 826.431 | <0.001 |
| Slightly difficult | 414 | 19.1 | 477 | 30.7 | 2107 | 33.6 | |||
| Very difficult | 124 | 5.7 | 187 | 12.0 | 1157 | 18.5 | |||
| Cannot do it at all | 16 | 0.7 | 72 | 4.6 | 469 | 7.5 | |||
| Do now | 8 | 0.4 | 9 | 0.6 | 44 | 0.7 | |||
| Difficulty in climbing 10 steps without a break | Not difficult at all | 1465 | 67.6 | 639 | 41.2 | 2030 | 32.4 | 907.291 | <0.001 |
| Slightly difficult | 550 | 25.4 | 567 | 36.5 | 2391 | 38.1 | |||
| Very difficult | 129 | 6.0 | 271 | 17.5 | 1415 | 22.6 | |||
| Cannot do it at all | 20 | 0.9 | 70 | 4.5 | 394 | 6.3 | |||
| Do now | 4 | 0.2 | 5 | 0.3 | 40 | 0.6 | |||
| Difficulty performing movements such as bending, squatting, or kneeling | Not difficult at all | 1535 | 70.8 | 722 | 46.5 | 2449 | 39.1 | 682.021 | <0.001 |
| Slightly difficult | 482 | 22.2 | 551 | 35.5 | 2410 | 38.4 | |||
| Very difficult | 126 | 5.8 | 219 | 14.1 | 1096 | 17.5 | |||
| Cannot do it at all | 22 | 1.0 | 58 | 3.7 | 293 | 4.7 | |||
| Do now | 3 | 0.1 | 2 | 0.1 | 22 | 0.4 | |||
| Difficulty performing movements such as reaching out for something above the head | Not difficult at all | 1729 | 79.8 | 895 | 57.7 | 3139 | 50.1 | 590.074 | <0.001 |
| Slightly difficult | 330 | 15.2 | 474 | 30.5 | 2162 | 34.5 | |||
| Very difficult | 93 | 4.3 | 142 | 9.1 | 749 | 11.9 | |||
| Cannot do it at all | 13 | 0.6 | 38 | 2.4 | 197 | 3.1 | |||
| Do now | 3 | 0.1 | 3 | 0.2 | 23 | 0.4 | |||
| Difficulty in performing operations such as lifting or moving about 8 kg of rice | Not difficult at all | 1478 | 68.2 | 694 | 44.7 | 2097 | 33.4 | 855.233 | <0.001 |
| Slightly difficult | 496 | 22.9 | 519 | 33.4 | 2316 | 36.9 | |||
| Very difficult | 166 | 7.7 | 254 | 16.4 | 1304 | 20.8 | |||
| Cannot do it at all | 25 | 1.2 | 79 | 5.1 | 521 | 8.3 | |||
| Do now | 3 | 0.1 | 6 | 0.4 | 32 | 0.5 | |||
| Characteristics | Driving | X2 3/H 4 | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Current Drivers | Past But Not Current Drivers | No Driver’s License | |||||||
| N 1 | % 2 | N/M | % | N/M | % | ||||
| Current economic activity | Currently working | 1432 | 66.1 | 448 | 28.9 | 1898 | 30.3 | 1305.474 | <0.001 |
| Previously worked but not currently | 676 | 31.2 | 1041 | 67.1 | 3116 | 49.7 | |||
| Not working | 60 | 2.8 | 63 | 4.1 | 1256 | 20.0 | |||
| Current work | Farmers and fisheries | 353 | 24.7 | 77 | 17.2 | 482 | 25.4 | 854.529 | <0.001 |
| Cost facilities management | 159 | 11.1 | 92 | 20.5 | 132 | 7.0 | |||
| Cleaning | 59 | 4.1 | 65 | 14.5 | 468 | 24.7 | |||
| Production | 83 | 5.8 | 27 | 6.0 | 69 | 3.6 | |||
| Household care | 21 | 1.5 | 3 | 0.7 | 82 | 4.3 | |||
| Driving transport | 160 | 11.2 | 8 | 1.8 | 8 | 0.4 | |||
| Professions | 69 | 4.8 | 8 | 1.8 | 20 | 1.1 | |||
| Office | 37 | 2.6 | 7 | 1.6 | 8 | 0.4 | |||
| Cooking and food | 148 | 10.3 | 33 | 7.4 | 242 | 12.8 | |||
| Courier and delivery | 20 | 1.4 | 3 | 0.7 | 4 | 0.2 | |||
| Site management | 46 | 3.2 | 16 | 3.6 | 22 | 1.2 | |||
| Environmental landscaping | 27 | 1.9 | 27 | 6.0 | 114 | 6.0 | |||
| Construction machinery | 135 | 9.4 | 23 | 5.1 | 28 | 1.5 | |||
| Culture and arts | 9 | 0.6 | 0 | 0.0 | 3 | 0.2 | |||
| Maintaining public order | 14 | 1.0 | 16 | 3.6 | 69 | 3.6 | |||
| Waste paper collection | 5 | 0.3 | 8 | 1.8 | 24 | 1.3 | |||
| ETC | 87 | 6.1 | 35 | 7.8 | 123 | 6.5 | |||
| Work status | Don’t want to work | 804 | 37.2 | 1006 | 66.1 | 4298 | 69.9 | 867.564 | <0.001 |
| Continue with current job | 1135 | 52.5 | 334 | 21.9 | 1339 | 21.8 | |||
| Seeking different work | 82 | 3.8 | 53 | 3.5 | 130 | 2.1 | |||
| Do not work now, but want to work | 141 | 6.5 | 130 | 8.5 | 379 | 6.2 | |||
| Characteristics | Education Level | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0–3 Years | 4–6 Years | 7–12 Years | 13 Years or More | |||||||
| Male | Female | Male | Female | Male | Female | Male | Female | |||
| Current drivers | Age | 65–69 | 30 (2) | 30 (1) | 27 (73) | 27 (40) | 27 (776) | 27 (272) | 28 (165) | 29 (39) |
| 70–74 | 30 (2) | 25 (1) | 26 (60) | 25 (14) | 26 (344) | 27 (40) | 29 (66) | 28 (5) | ||
| 75–79 | 27 (2) | 24 (1) | 25 (45) | 26 (7) | 27 (120) | 26 (9) | 26 (16) | 29 (2) | ||
| 80 over | 22 (3) | 16 (1) | 23 (15) | 23 (4) | 27 (30) | 6 (1) | 28 (10) | 30 (2) | ||
| Past but not current drivers | 65–69 | 26 (1) | 23 (1) | 24 (42) | 25 (16) | 25 (185) | 27 (126) | 24 (14) | 28 (15) | |
| 70–74 | 21 (5) | 25 (1) | 25 (71) | 26 (15) | 25 (249) | 27 (62) | 26 (32) | 27 (4) | ||
| 75–79 | 22 (11) | 25 (4) | 24 (117) | 26 (20) | 25 (211) | 25 (19) | 26 (29) | 25 (6) | ||
| 80 over | 20 (29) | 15 (4) | 23 (96) | 23 (9) | 24 (114) | 24 (11) | 25 (31) | 29 (2) | ||
| No driver’s license | 65–69 | 21 (6) | 23 (41) | 26 (36) | 25 (385) | 24 (141) | 26 (1097) | 26 (10) | 26 (37) | |
| 70–74 | 25 (9) | 22 (132) | 23 (94) | 24 (602) | 23 (147) | 25 (513) | 28 (8) | 25 (16) | ||
| 75–79 | 23 (14) | 21 (256) | 23 (113) | 23 (616) | 23 (106) | 24 (241) | 27 (9) | 24 (14) | ||
| 80 over | 22 (72) | 20 (514) | 22 (180) | 22 (627) | 21 (91) | 23 (129) | 26 (9) | 24 (5) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, S.-H.; Kim, E.-Y.; Lee, S.-J.; Choi, W.-J.; Oh, C.; Sung, H.-J.; Kim, J. Health Status and Activity Discomfort among Elderly Drivers: Reality of Health Awareness. Healthcare 2023, 11, 563. https://doi.org/10.3390/healthcare11040563
Jeong S-H, Kim E-Y, Lee S-J, Choi W-J, Oh C, Sung H-J, Kim J. Health Status and Activity Discomfort among Elderly Drivers: Reality of Health Awareness. Healthcare. 2023; 11(4):563. https://doi.org/10.3390/healthcare11040563
Chicago/Turabian StyleJeong, Sang-Hoon, Eun-Yeob Kim, Seung-Jin Lee, Woo-June Choi, Chilhwan Oh, Hwa-Jung Sung, and Jaeyoung Kim. 2023. "Health Status and Activity Discomfort among Elderly Drivers: Reality of Health Awareness" Healthcare 11, no. 4: 563. https://doi.org/10.3390/healthcare11040563
APA StyleJeong, S.-H., Kim, E.-Y., Lee, S.-J., Choi, W.-J., Oh, C., Sung, H.-J., & Kim, J. (2023). Health Status and Activity Discomfort among Elderly Drivers: Reality of Health Awareness. Healthcare, 11(4), 563. https://doi.org/10.3390/healthcare11040563







