Resident Impact of the Single Site Order Restricting Staff Mobility across Long-Term Care Homes in British Columbia, Canada
Abstract
:1. Introduction
1.1. LTC in Canada and International Context
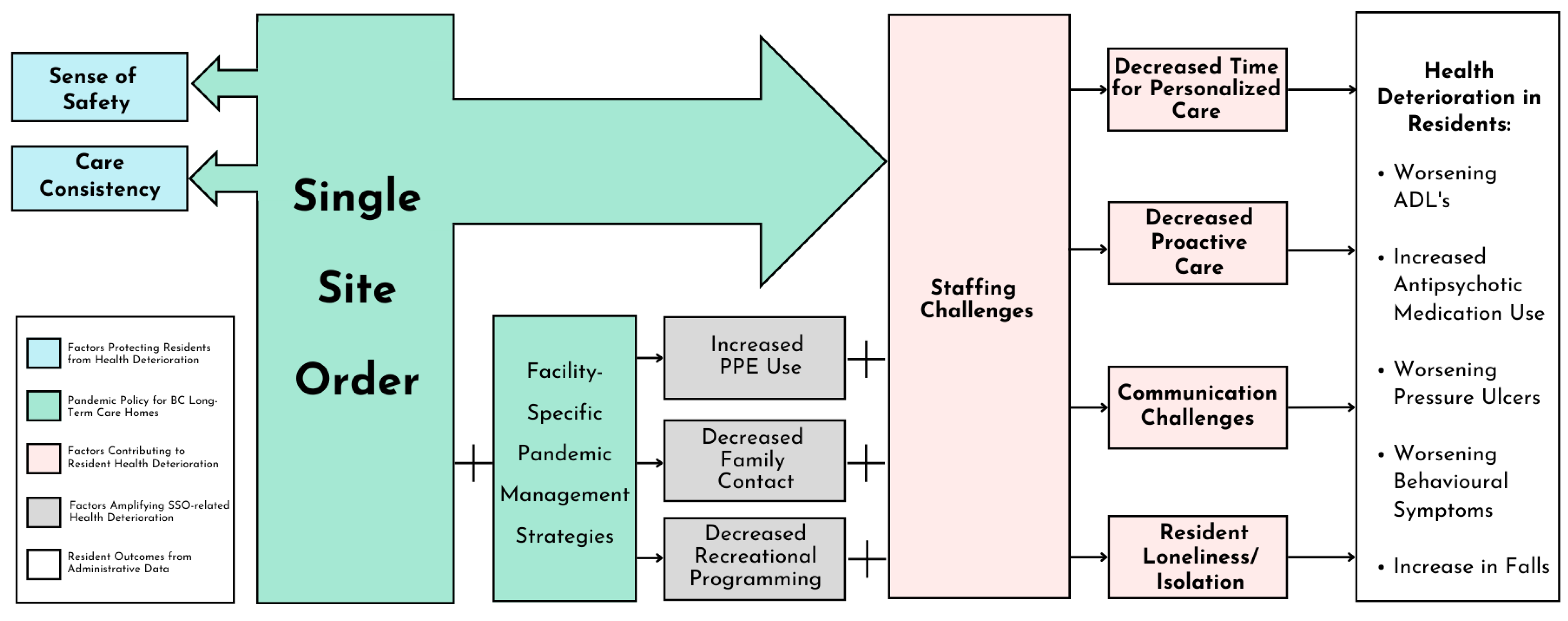
1.2. Single Site Order
2. Materials and Methods
2.1. Qualitative Methods
2.2. Quantitative Methods
3. Results
3.1. Qualitative
I’m very much for the [SSO]. Especially for any of the residents [with] dementia. The routine is so so important and knowing who it is [giving the care]. Every so often my father [resident] will say, ‘well, I don’t know you’ to the [caregiver], ‘why are you giving me pills’, and ‘what pills are you giving me’. … one of his nurses [had] asked me if I noticed any difference in [my father] and [the nurse] says ‘well he’s becoming more resistant to taking medications’. … On his yearly Parkinson’s visit with [the doctor] … the nurse who most often does the night shift with [resident] stayed on after her shift so that she could talk with [the doctor to explain those changes]. It’s just that level of care that having that individual who knows the resident is so important, in my opinion. [Family Member 2, The Manor]
During [the first wave], there were a lot of LTC homes that had fairly widespread [infection], they had to go through lockdown … and it was a very terrifying experience for families. So, [the SSO] is a very welcoming decision. … we’re dealing with the vulnerable aging population… I think the one site policy is the best policy. [Family Member 2, Rosewood]
When [care staff] work a lot of overtime because of lack of staff, staff get burned out and you can’t fill the overtime slots anymore. [This] increased [the] frequency [of] calling in sick too. [Leader 2, Lake Bay]
There [are] only so many [residents] that the clinical staff can care for in a given day. There’s only so much they can do and honestly coming back here [after not visiting due to visitation restrictions] … he had broken eyeglasses [and] no hearing aids. [His] hair wasn’t cut. So many details that aren’t life threatening but are many activities of daily living were not to the standard that he had been accustomed to. [Family Member 4, Lake Bay]
Agency [staff] that don’t speak the [same] language, it will be very difficult to know the needs of the resident that in turn makes the resident very anxious when they are not able to express their needs or being understood about what they want. [Other staff] will be shouldering or [bearing] the responsibility of our work happening [with the] resident, so it takes some time for the agency staff to know the procedure, [to] start learning a little bit of very basic [language] in order to communicate. [Leader 2, Rosewood]
I think [the reason for decline in residents is] the lack of interaction with the world, [the] isolation. … One lady she wears pearls and in June she’s walking around she always sits in the same chair and [says hello to me, but] when [I returned to the facility I noticed] she’s just gone downhill so quickly. You notice people disappearing, … If you’re really paying attention, you know that the residents are suffering. [Family Member 1, Lake Bay].
[When] nobody could move and gather [for performances], the recreation staff would go to their [assigned] particular floors. … Then [the recreation team] were entertaining even more than before [the pandemic] to make [residents] happy not lonely. And the LPNs also [helped with] phone calls from family members on their birthdays and [the nurses would] dress [up the residents] and bring [them] to the windows and they’ll go in the parking lot and [get] birthday wishes and balloons [the residents] can see [their family from] afar. As well, the pastor who’s helping to do one thing or another [for residents]. [Staff Member 0, Seaside]
All of a sudden, my staff had to be the family in many ways and that’s the only reason we staffed up because I don’t have that person that came in every day to help them have lunch. Somebody has to do [it]…the staffing has been a real challenge. [Leader 1, Seaside]
It was really challenging. …when you try to talk nobody hears you so it’s so hard to have to start raising your voice and the communication is impaired. Even if I smile to the elders or to my team, nobody can see. [Staff Member 0, Seaside]
When we were in outbreak… all the residents had to be isolated in their own suite. That’s the time that we found increase [in] falls. And given the fact that [staff must don and doff] before we can reach [residents], even if we hear the bed alarm ring. In fact, the residents do not really have [anything else to] do other than staying [in their] room, so they get bored they get up and they didn’t have [access to] exercise so [they fall]. [Leader 1, Rosewood]
3.2. Quantitative
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. UN Department of Economic and Social Affairs Issue Brief: Older Persons and COVID-19; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Sepulveda, E.R.; Stall, N.M.; Sinha, S.K. A Comparison of COVID-19 Mortality Rates among Long-Term Care Residents in 12 OECD Countries. J. Am. Med. Dir. Assoc. [CrossRef]
- Canadian Institute for Health Information. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months; CIHI: Ottawa, ON, Canada, 2021; pp. 1–34. [Google Scholar]
- Liu, M.; Maxwell, C.J.; Armstrong, P.; Schwandt, M.; Moser, A.; McGregor, M.J.; Bronskill, S.E.; Dhalla, I.A. COVID-19 in Long-Term Care Homes in Ontario and British Columbia. Can. Med. Assoc. J. 2020, 192, E1540–E1546. [Google Scholar] [CrossRef]
- Ernst & Young LLP. BC Ministry of Health Long-Term Care COVID-19 Response Review; Ernst & Young LLP: London, UK, 2020. [Google Scholar]
- Jones, A.; Watts, A.G.; Khan, S.U.; Forsyth, J.; Brown, K.A.; Costa, A.P.; Bogoch, I.I.; Stall, N.M. Impact of a Public Policy Restricting Staff Mobility between Nursing Homes in Ontario, Canada During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Staempfli, S.; Havaei, F.; Phinney, A.; MacPhee, M. Unintended Consequences of Pandemic Management Strategies on Residents and Family in One Long-Term Care Home in British Columbia: A Patient-Supported Qualitative Study. Innov. Aging 2022, 6, igac036. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute for Health Information. Long Term Care Homes in Canada, How Many, and Who Owns Them. Available online: https://www.cihi.ca/en/long-term-care-homes-in-canada-how-many-and-who-owns-them (accessed on 16 October 2023).
- Health Canada. Long-Term Facilities-Based Care. Available online: https://www.canada.ca/en/health-canada/services/home-continuing-care/long-term-facilities-based-care.html (accessed on 13 October 2023).
- Estabrooks, C.A.; Straus, S.E.; Flood, C.M.; Keefe, J.; Armstrong, P.; Donner, G.J.; Boscart, V.; Ducharme, F.; Silvius, J.L.; Wolfson, M.C. Restoring Trust: COVID-19 and the Future of Long-Term Care in Canada. FACETS 2020, 5, 651–691. [Google Scholar] [CrossRef]
- OECD. Who Cares? Attracting and Retaining Care Workers for the Elderly; Organisation for Economic Co-Operation and Development: Paris, France, 2020. [Google Scholar]
- Hsu, A.T.; Lane, N.; Sinha, S.; Dunning, J.; Dhuper, M.; Kahiel, Z.; Sveistrup, H. Understanding the Impact of COVID-19 on Residents of Canada’s Long-Term LTC Homes Ongoing Challenges and Policy Responses; Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE. Available online: https://ltccovid.org/wp-content/uploads/2020/06/LTCcovid-country-reports_Canada_June-4-2020.pdf (accessed on 4 June 2020).
- Canadian Institute for Health Information. LTC Quick Stats 2021–2022; CIHI: Ottawa, ON, Canada, 2022. [Google Scholar]
- Song, Y.; Hoben, M.; Norton, P.; Estabrooks, C.A. Association of Work Environment with Missed and Rushed Care Tasks among Care Aides in Nursing Homes. JAMA Netw. Open 2020, 3, e1920092. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Iaconi, A.; Song, Y.; Norton, P.G.; Squires, J.E.; Keefe, J.; Cummings, G.G.; Estabrooks, C.A. Care Aides Working Multiple Jobs: Considerations for Staffing Policies in Long-Term Care Homes During and After the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 1390–1391. [Google Scholar] [CrossRef] [PubMed]
- Lorenz-Dant, K.; Fischer, T.; Hämel, K. LTCcovid, Care Policy and Evaluation Centre, London School of Economics and Political Science: COVID-19 and the Long-Term Care System in Germany. Available online: https://ltccovid.org/country/germany/ (accessed on 13 October 2023).
- Giannasi, W.; Hystad, J. BC Care Providers Association Review of the Response to COVID 19 in Seniors Care and Living; HoweGroup: British Columbia, Canada, 2020. [Google Scholar]
- Robinson, O.C. Sampling in Interview-Based Qualitative Research: A Theoretical and Practical Guide. Qual. Res. Psychol. 2014, 11, 25–41. [Google Scholar] [CrossRef]
- Sundler, A.J.; Lindberg, E.; Nilsson, C.; Palmér, L. Qualitative Thematic Analysis Based on Descriptive Phenomenology. Nurs. Open 2019, 6, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 160940691773384. [Google Scholar] [CrossRef]
- Baumbusch, J.; Phinney, A. Invisible Hands: The Role of Highly Involved Families in Long-Term Residential Care. J. Fam. Nurs. 2014, 20, 73–97. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.B.; Weinberg, T.; McRae, S.; Pollack, C.; Dutton, D. Long-Term Care Staffing Policies Pre-COVID-19 and Pandemic Responses: A Case Comparison of Ontario and British Columbia. Can. Public Policy 2020, 49, 94–113. [Google Scholar] [CrossRef]
- Perruchoud, E.; Weissbrodt, R.; Verloo, H.; Fournier, C.-A.; Genolet, A.; Rosselet Amoussou, J.; Hannart, S. The Impact of Nursing Staffs’ Working Conditions on the Quality of Care Received by Older Adults in Long-Term Residential Care Facilities: A Systematic Review of Interventional and Observational Studies. Geriatrics 2021, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]

| LTC Homes | Details | ||||
|---|---|---|---|---|---|
| LTC #1 | LTC #2 | LTC #3 | LTC #4 | ||
| Pseudonym | Seaside | Lake Bay | The Manor | Rosewood | |
| Municipality | Mission | Vancouver | Richmond | Vancouver | |
| # of staff | ~250 | ~400 | ~280 | ~160 | |
| # of residents | ~151 | ~250 | ~250 | ~130 | |
| Resident Interviews | (n = 2) | (n = 2) | (n = 2) | (n = 0) | Age 61–92 Female n = 2, Male n = 4 Lived in home for 1 to 20 years |
| Family Interviews | (n = 2) | (n = 4) | (n = 2) | (n = 2) | Age 56–74 Female n = 9, Male n = 1 Relationship to residents: Daughter, wife, husband |
| Staff Interviews | (n = 5) | (n = 5) | (n = 5) | (n = 3) | n = 14 > 40 years old Female n = 17, Male n = 1 Employed at home for 6 months to 37 years Job titles: Registered Nurse, Care Aide, Laundry Aide, Chef, Housekeeping Services |
| Leadership Interviews | (n = 2) | (n = 4) | (n = 2) | (n = 2) | Female n = 8, Male n = 2 Job titles: Chief Executive Officer, Executive Director, Nurse Manager, Care Aide Manager, Director of Human Resources, Clinical Operations Supervisor |
| Resident Data Indicator | Definition |
|---|---|
| Resident demographics | |
| Sex (female) | The proportion of active residents that were female expressed as a percentage. |
| Age | Mean age of an LTC home’s active residents in years. Age is calculated based on residents’ age at the midpoint of each quarter. |
| Stay length | Mean stay length of an LTC home’s discharged residents in days or converted to years. |
| Resident behaviours | |
| Index of Social Engagement | Mean Index of Social Engagement (ISE) score for an LTC home’s assessed residents. |
| Quality indicators * | |
| Worsened/remained dependent in mid-loss ADL | Incidence indicator; the proportion of assessed residents that had worsened or remained dependent in mid-loss activities of daily living (ADLs) in percentage as representation of functional dependence. |
| Worsened behavioural symptoms | Incidence indicator; the proportion of assessed residents that had worsened behavioural symptoms in percentage. |
| Antipsychotics | Prevalence indicator; the proportion of assessed residents that had taken antipsychotics without a diagnosis of psychosis in percentage. |
| Fall in 30 days | Prevalence indicator; the proportion of assessed residents that had fallen in the last 30 days in percentage. |
| Worsened stage 2 to 4 pressure ulcer | Incidence indicator; the proportion of assessed residents that had stage 2 to 4 pressure ulcers that had worsened from the last assessment in percentage. |
| Daily physical restraints | Prevalence indicator; the proportion of assessed residents that were in physical restraints daily in percentage. |
| Weight loss | Prevalence indicator; the proportion of assessed residents that had had weight loss in percentage. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Havaei, F.; Staempfli, S.; Ma, A.; Sims-Gould, J.; Franke, T.; Park, M. Resident Impact of the Single Site Order Restricting Staff Mobility across Long-Term Care Homes in British Columbia, Canada. Healthcare 2023, 11, 3190. https://doi.org/10.3390/healthcare11243190
Havaei F, Staempfli S, Ma A, Sims-Gould J, Franke T, Park M. Resident Impact of the Single Site Order Restricting Staff Mobility across Long-Term Care Homes in British Columbia, Canada. Healthcare. 2023; 11(24):3190. https://doi.org/10.3390/healthcare11243190
Chicago/Turabian StyleHavaei, Farinaz, Sabina Staempfli, Andy Ma, Joanie Sims-Gould, Thea Franke, and Minjeong Park. 2023. "Resident Impact of the Single Site Order Restricting Staff Mobility across Long-Term Care Homes in British Columbia, Canada" Healthcare 11, no. 24: 3190. https://doi.org/10.3390/healthcare11243190
APA StyleHavaei, F., Staempfli, S., Ma, A., Sims-Gould, J., Franke, T., & Park, M. (2023). Resident Impact of the Single Site Order Restricting Staff Mobility across Long-Term Care Homes in British Columbia, Canada. Healthcare, 11(24), 3190. https://doi.org/10.3390/healthcare11243190









