Patent and Bibliometric Analysis of the Scientific Landscape of the Use of Pulse Oximeters and Their Prospects in the Field of Digital Medicine
Abstract
:1. Introduction
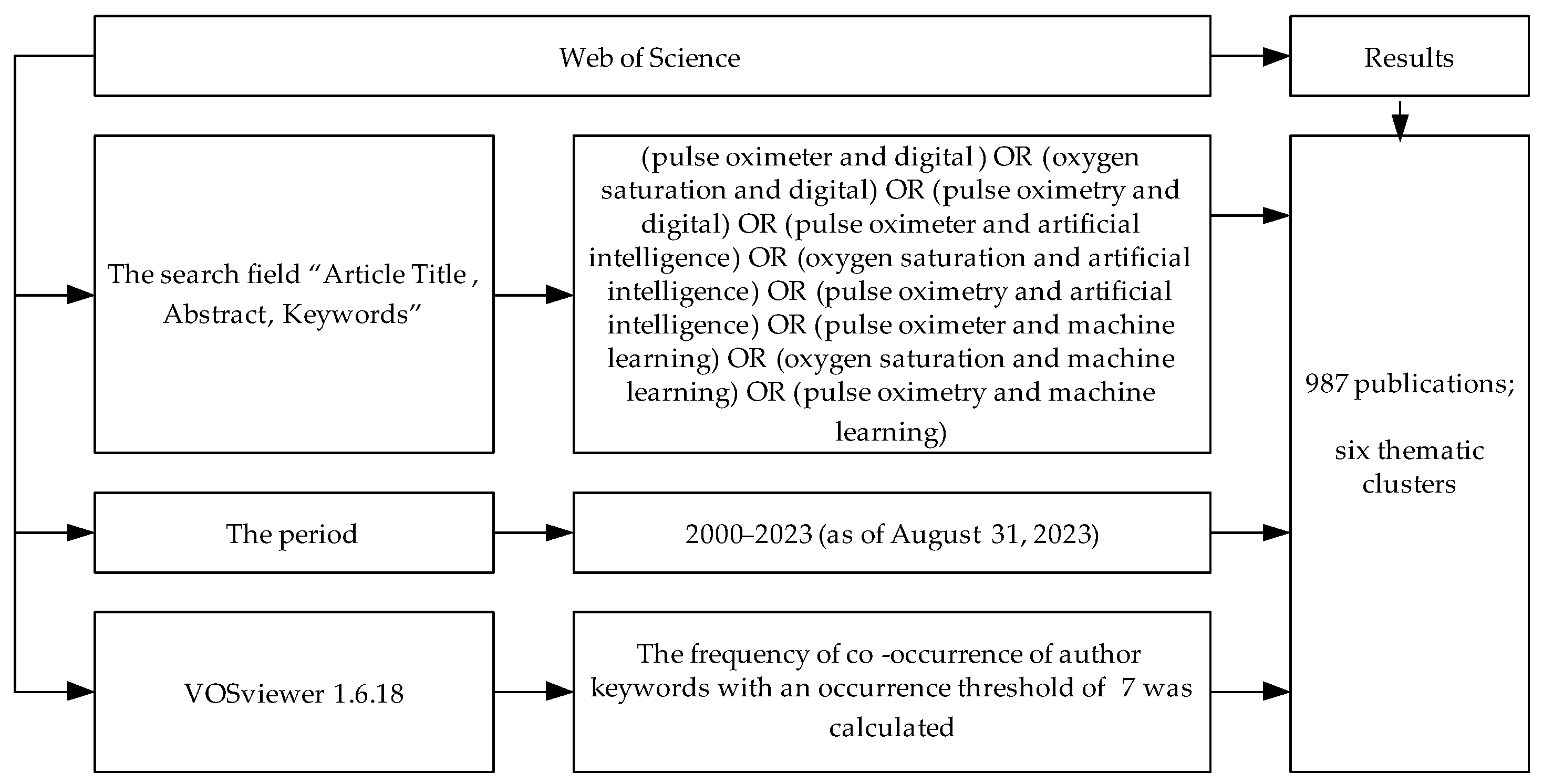
2. Materials and Methods
2.1. Patent Analysis
2.2. Bibliometric Analysis
3. Results
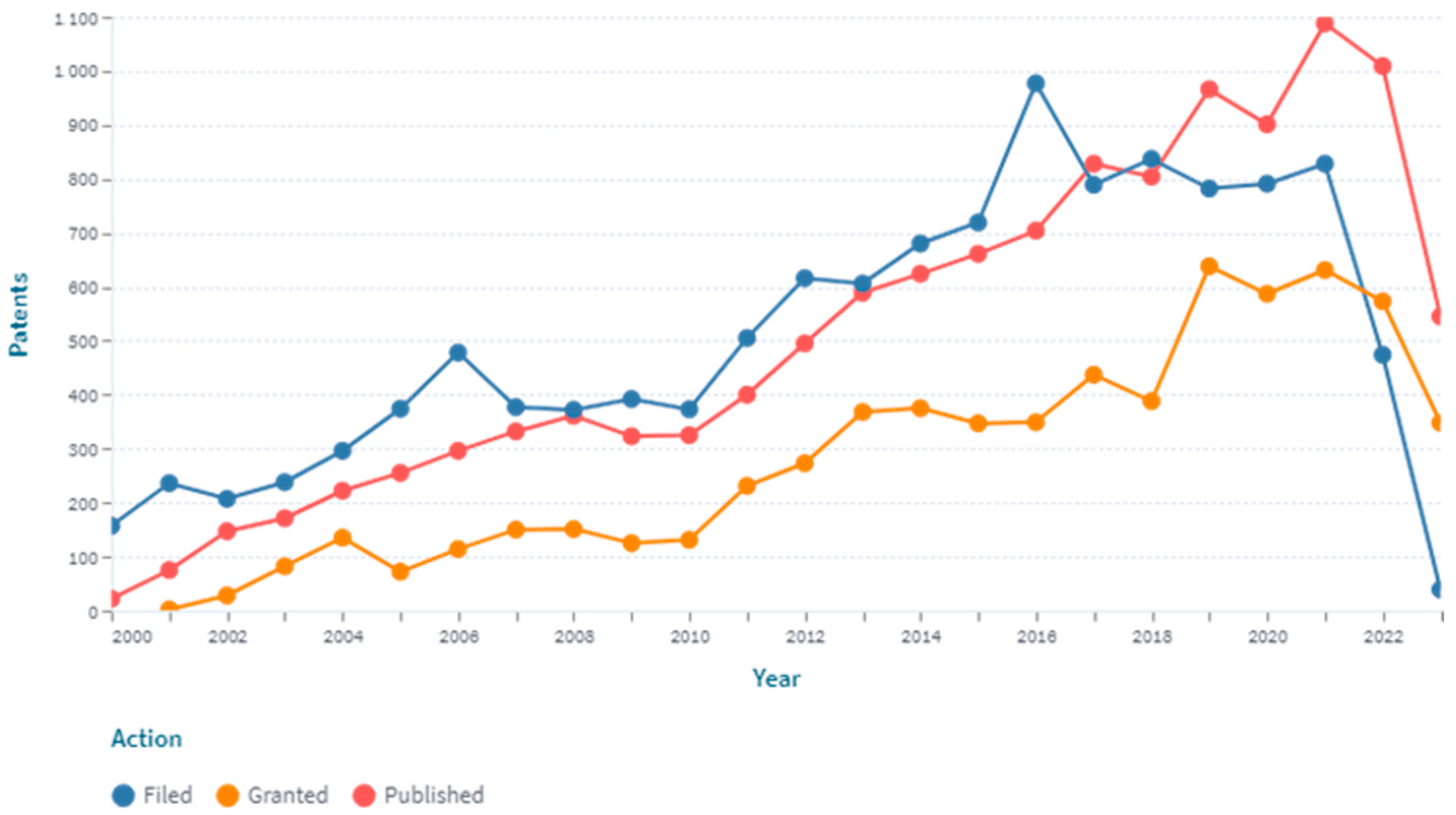
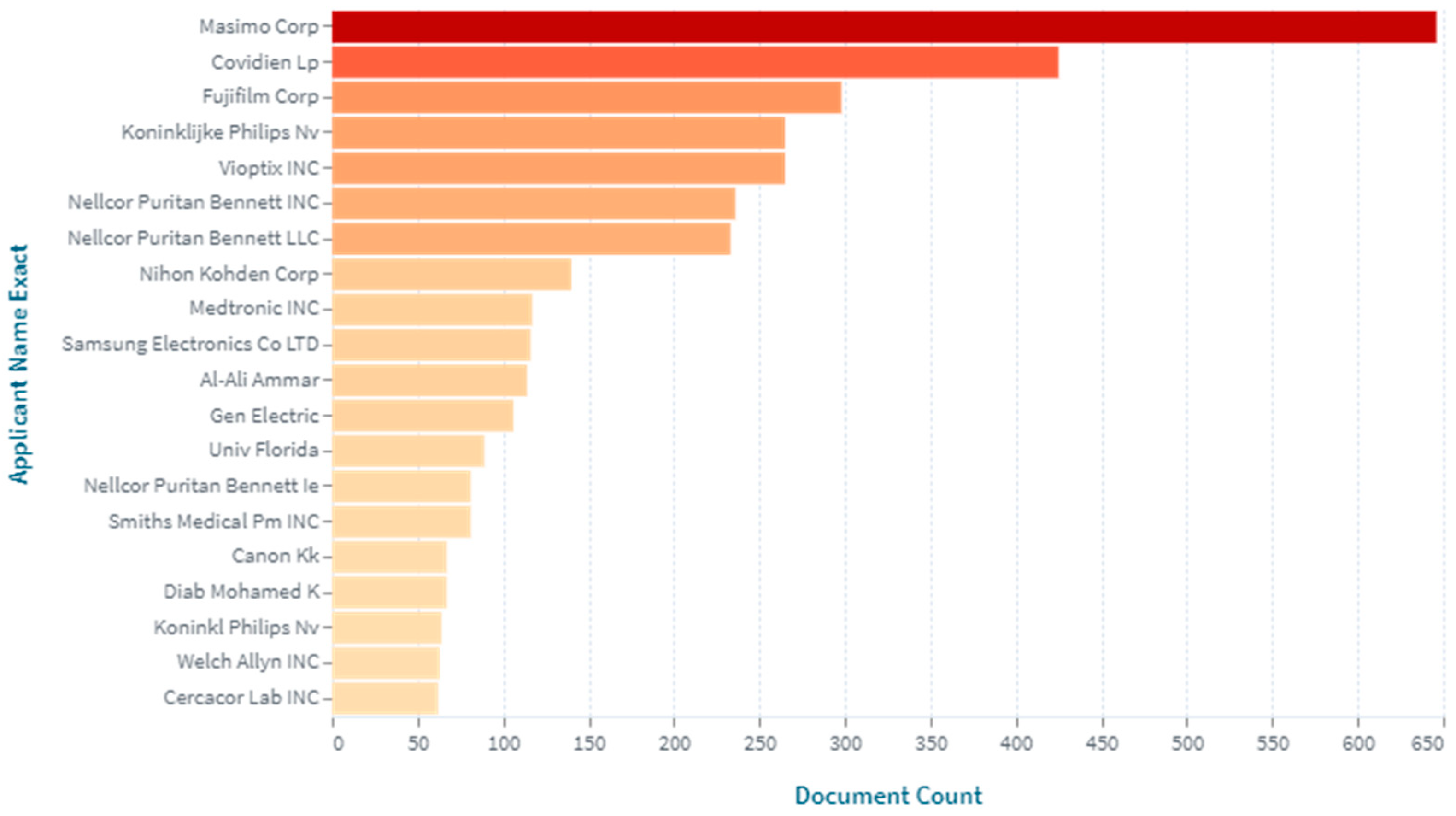
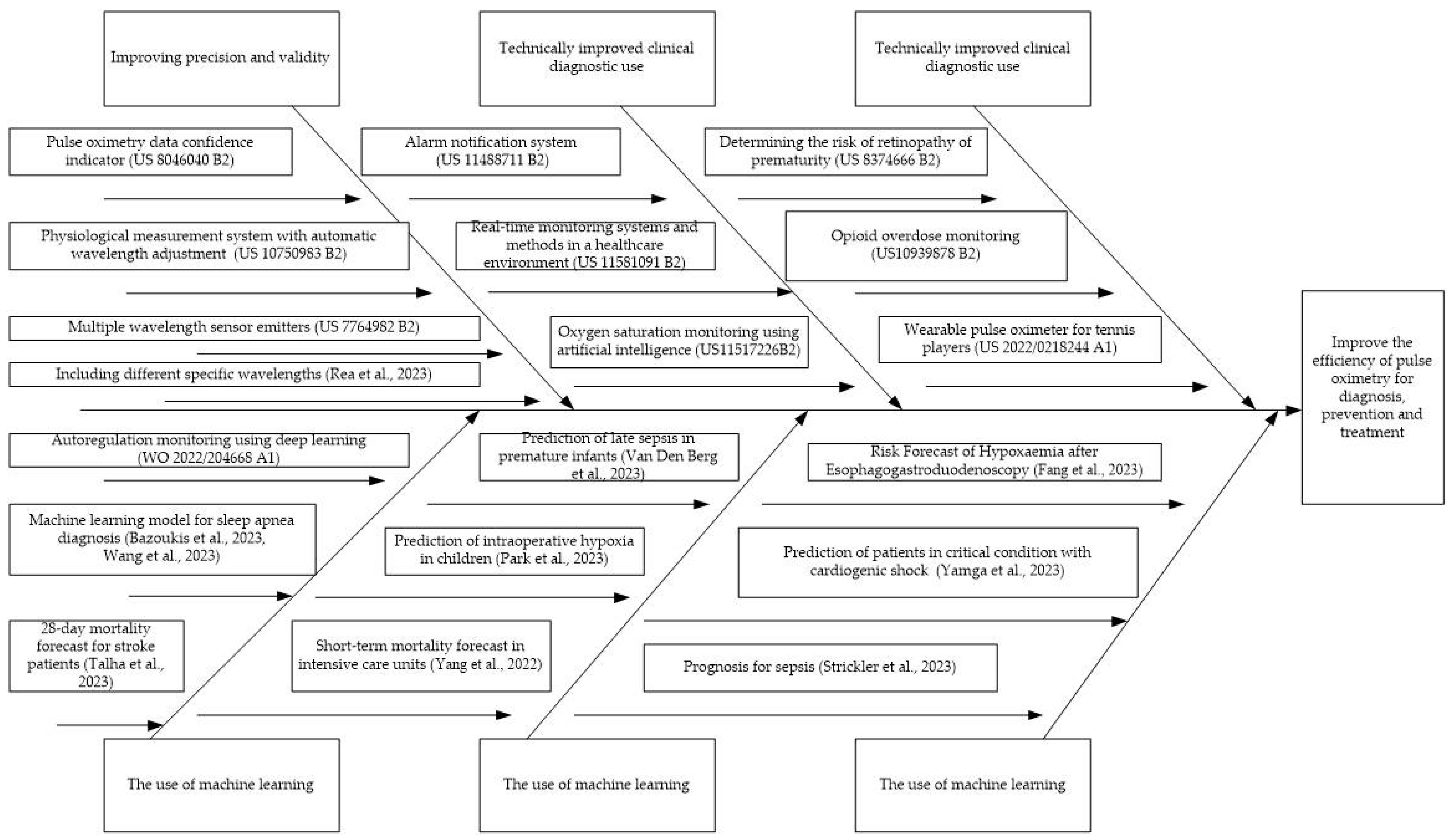
3.1. Patent Analysis
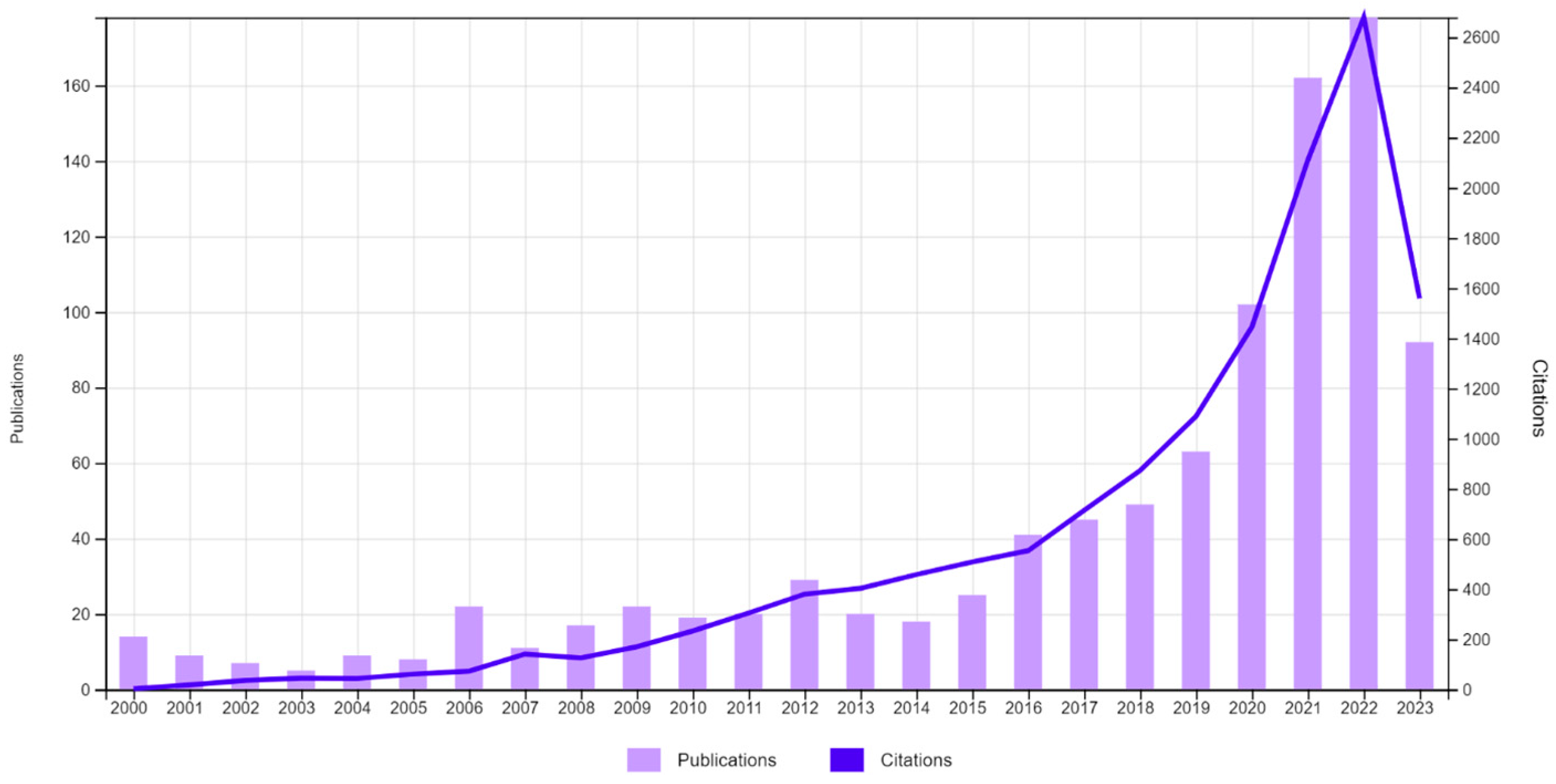
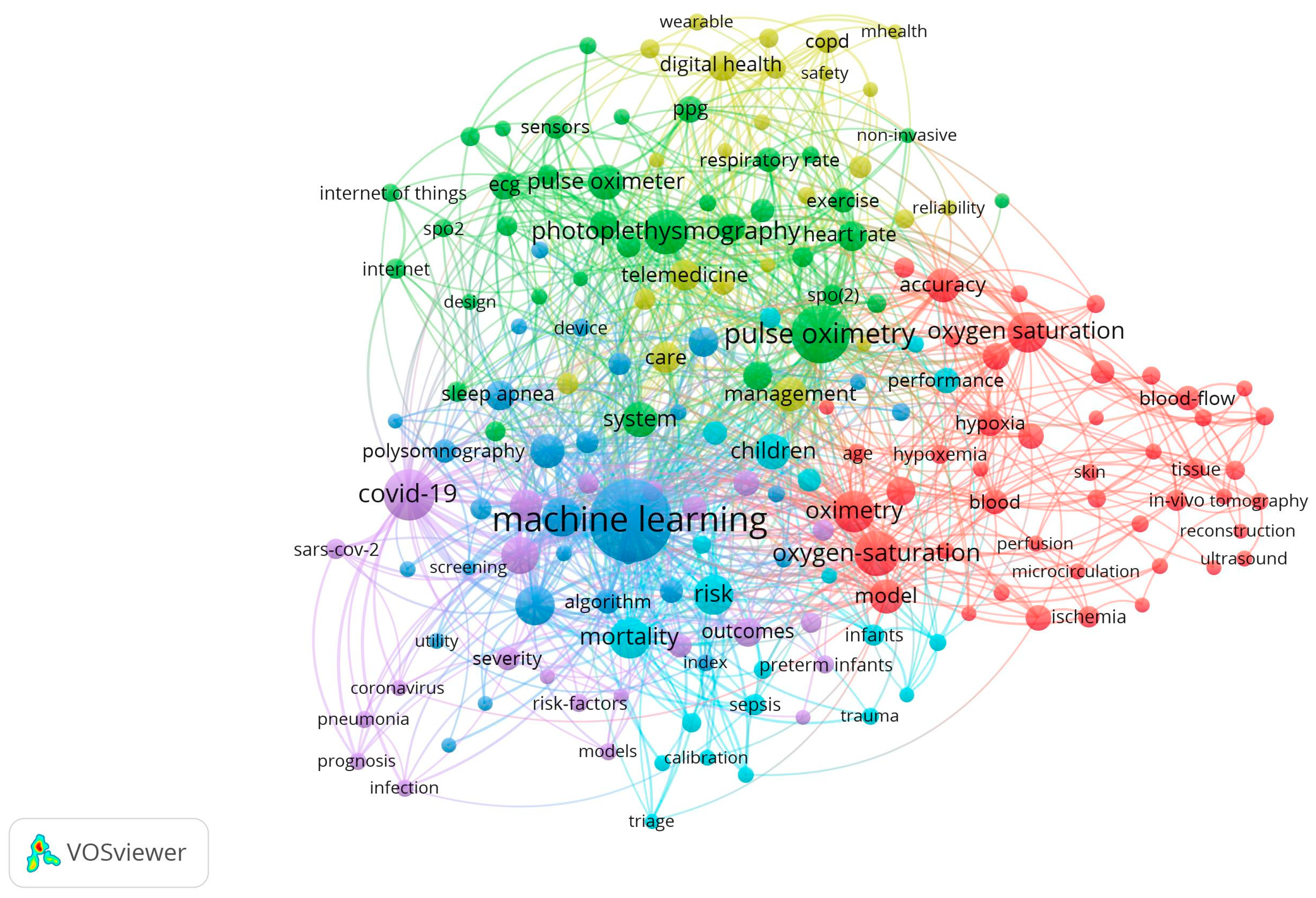
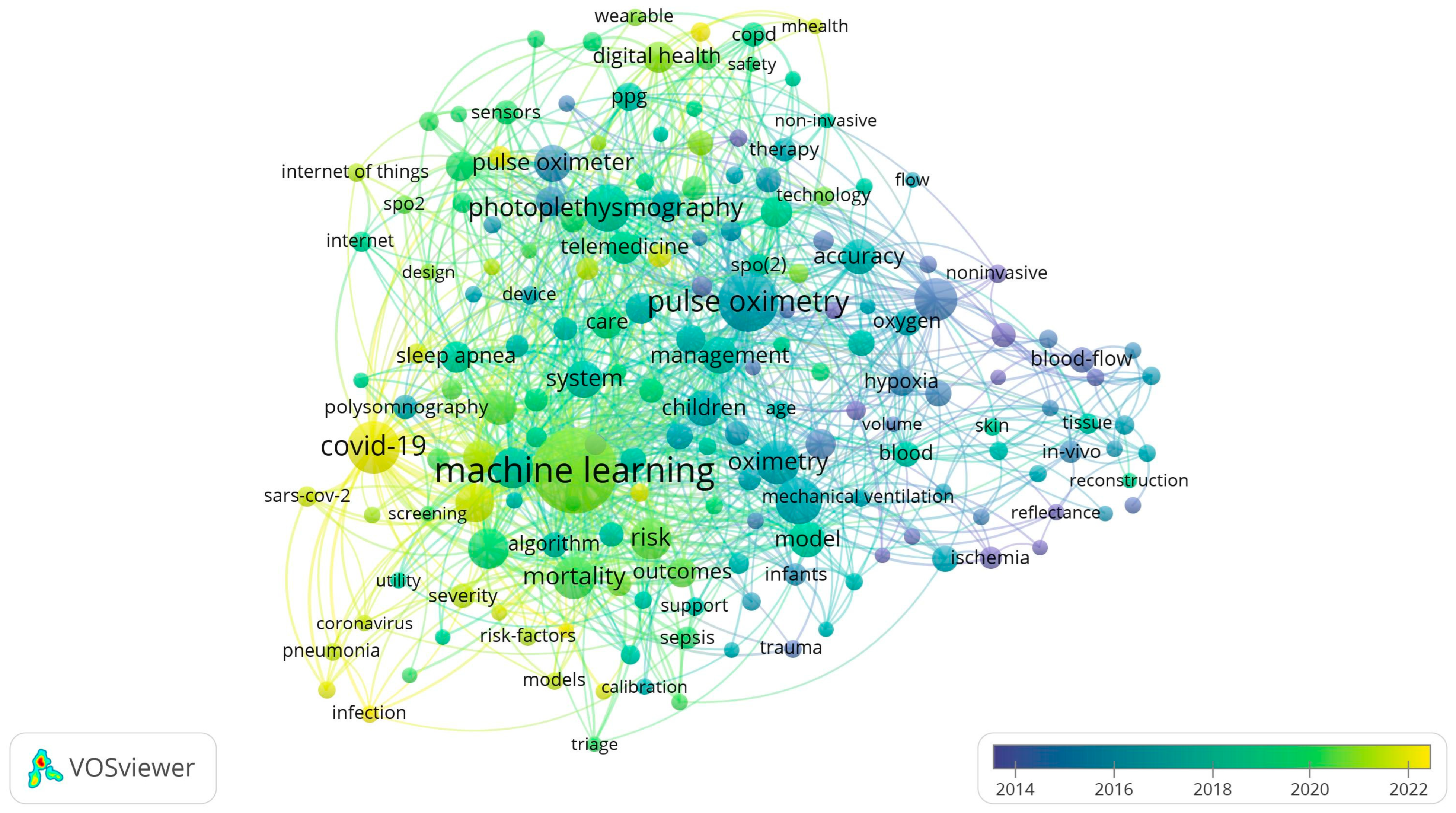
3.2. Bibliometric Analysis
4. Discussion
- Pulse oximeters are used by prescription and have passed clinical trials. They are used most often in hospitals and doctors’ offices, and less often for home use.
- Over-the-counter pulse oximeters. They do not pass FDA review and are more often intended for general wellness, sports, or aviation purposes.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tekin, K.; Karadogan, M.; Gunaydin, S.; Kismet, K. Everything About Pulse Oximetry—Part 2: Clinical Applications, Portable/Wearable Pulse Oximeters, Remote Patient Monitoring, and Recent Advances. J. Intensive Care Med. 2023, 38, 08850666231189175. [Google Scholar] [CrossRef] [PubMed]
- WHO Pulse Oximetry Training Manual. World Health Organization 2011. Available online: https://cdn.who.int/media/docs/default-source/patient-safety/pulse-oximetry/who-ps-pulse-oxymetry-training-manual-en.pdf?sfvrsn=322cb7ae_6 (accessed on 24 September 2023).
- Jubran, A. Pulse Oximetry. Crit. Care 2015, 19, 272. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, T.; Kainulainen, S.; Korkalainen, H.; Sillanmäki, S.; Kulkas, A.; Töyräs, J.; Nikkonen, S. Pulse Oximetry: The Working Principle, Signal Formation, and Applications. In Advances in the Diagnosis and Treatment of Sleep Apnea; Penzel, T., Hornero, R., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2022; Volume 1384, pp. 205–218. [Google Scholar] [CrossRef]
- Sobel, J.A.; Levy, J.; Almog, R.; Reiner-Benaim, A.; Miller, A.; Eytan, D.; Behar, J.A. Descriptive Characteristics of Continuous Oximetry Measurement in Moderate to Severe COVID-19 Patients. Sci. Rep. 2023, 13, 442. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.; Ewer, A.K. New Born Pulse Oximetry Screening: A Global Perspective. Early Hum. Dev. 2021, 162, 105457. [Google Scholar] [CrossRef]
- Jullien, S. Newborn Pulse Oximetry Screening for Critical Congenital Heart Defects. BMC Pediatr. 2021, 21 (Suppl. S1), 305. [Google Scholar] [CrossRef] [PubMed]
- Shaw, D.M.; Harrell, J.W. Integrating Physiological Monitoring Systems in Military Aviation: A Brief Narrative Review of Its Importance, Opportunities, and Risks. Ergonomics 2023, 66, 1–13. [Google Scholar] [CrossRef]
- Jebakumari, S.C.; Aarthi, K.; Darshan, S.; Karan, S. Firefighter Safety Using IoT. In Advances in Parallel Computing; Rajesh, M., Vengatesan, K., Gnanasekar, M., Sitharthan, R., Pawar, A.B., Kalvadekar, P.N., Saiprasad, P., Eds.; IOS Press: Amsterdam, The Netherlands, 2021. [Google Scholar] [CrossRef]
- Kramer, M.; Lobbestael, A.; Barten, E.; Eian, J.; Rausch, G. Wearable Pulse Oximetry Measurements on the Torso, Arms, and Legs: A Proof of Concept. Mil. Med. 2017, 182 (Suppl. S1), 92–98. [Google Scholar] [CrossRef]
- Dünnwald, T.; Kienast, R.; Niederseer, D.; Burtscher, M. The Use of Pulse Oximetry in the Assessment of Acclimatization to High Altitude. Sensors 2021, 21, 1263. [Google Scholar] [CrossRef]
- Kelleher, J.F. Pulse oximetry. J. Clin. Monitor Comput. 1989, 5, 37–62. [Google Scholar] [CrossRef]
- Tremper, K.K.; Barker, S.J. Pulse Oximetry. Anesthesiology 1989, 70, 98–108. [Google Scholar] [CrossRef]
- Torp, K.D.; Modi, P.; Pollard, E.J.; Simon, L.V. Pulse Oximetry. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK470348/ (accessed on 1 November 2023).
- Gelb, A.W.; Morriss, W.W.; Johnson, W.; Merry, A.F. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Anesth. Analg. 2018, 126, 2047–2055. [Google Scholar] [CrossRef] [PubMed]
- Pulse Oximeters Market. Forecast–2031. Available online: https://www.alliedmarketresearch.com/pulse-oximeter-market (accessed on 24 September 2023).
- Hanchinal, S.S. Efficacy of a Pocket Pulse Oximeter and a Digital Pulse Oximeter as Screening Tools for Type 2 Diabetes Patients with Asymptomatic Lower Extremity Arterial Disease. Maedica 2021, 16, 362–367. [Google Scholar] [CrossRef]
- Fischer, C.; Knüsli, J.; Lhopitallier, L.; Tenisch, E.; Meuwly, M.-G.; Douek, P.; Meuwly, J.-Y.; D’Acremont, V.; Kronenberg, A.; Locatelli, I.; et al. Pulse Oximetry as an Aid to Rule Out Pneumonia among Patients with a Lower Respiratory Tract Infection in Primary Care. Antibiotics 2023, 12, 496. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.; Flott, K.; Fernandez Crespo, R.; Ashrafian, H.; Fontana, G.; Benger, J.; Darzi, A.; Elkin, S. Assessing the Safety of Home Oximetry for COVID-19: A Multisite Retrospective Observational Study. BMJ Open 2021, 11, e049235. [Google Scholar] [CrossRef] [PubMed]
- Alboksmaty, A.; Beaney, T.; Elkin, S.; Clarke, J.M.; Darzi, A.; Aylin, P.; Neves, A.-L. Effectiveness and Safety of Pulse Oximetry in Remote Patient Monitoring of Patients with COVID-19: A Systematic Review. Lancet Digit. Health 2022, 4, e279–e289. [Google Scholar] [CrossRef]
- Terrill, P.I. A Review of Approaches for Analysing Obstructive Sleep Apnoea-related Patterns in Pulse Oximetry Data. Respirology 2020, 25, 475–485. [Google Scholar] [CrossRef]
- Aggarwal, A.N.; Agarwal, R.; Dhooria, S.; Prasad, K.T.; Sehgal, I.S.; Muthu, V. Impact of Fingernail Polish on Pulse Oximetry Measurements: A Systematic Review. Respir Care 2023, 68, 1271–1280. [Google Scholar] [CrossRef]
- Cabanas, A.M.; Fuentes-Guajardo, M.; Latorre, K.; León, D.; Martín-Escudero, P. Skin Pigmentation Influence on Pulse Oximetry Accuracy: A Systematic Review and Bibliometric Analysis. Sensors 2022, 22, 3402. [Google Scholar] [CrossRef]
- Jamali, H.; Castillo, L.T.; Morgan, C.C.; Coult, J.; Muhammad, J.L.; Osobamiro, O.O.; Parsons, E.C.; Adamson, R. Racial Disparity in Oxygen Saturation Measurements by Pulse Oximetry: Evidence and Implications. Ann. Am. Thorac. Soc. 2022, 19, 1951–1964. [Google Scholar] [CrossRef]
- Kyriacou, P.A. Optical Crosstalk and Other Forms of Light Interference in Pulse Oximeter Comparison Studies. J. Clin. Monit. Comput. 2023; ahead of print. [Google Scholar] [CrossRef]
- Review of Pulse Oximeters and Factors that can Impact their Accuracy. FDA Executive Summary. Prepared for the November 1, 2022, Meeting of the Anesthesiology Devices Advisory Committee Center for Devices and Radiological Health (CDRH) United States Food and Drug Administration. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRL/rl.cfm?start_search=1&showList=1&establishmentName=®Num=&StateName=&CountryName=&OwnerOperatorNumber=9031881&OwnerOperatorName=&ProductCode=&DeviceName=&ProprietaryName=&establishmentType=&PAGENUM=10&SortColumn=EstablishmentName20%25ASC&RegistrationNumber=3019388613 (accessed on 24 September 2023).
- Knight, S.; Lipoth, J.; Namvari, M.; Gu, C.; Hedayati, M.; Syed-Abdul, S.; Spiteri, R.J. The Accuracy of Wearable Photoplethysmography Sensors for Telehealth Monitoring: A Scoping Review. Telemed. e-Health 2023, 29, 813–828. [Google Scholar] [CrossRef]
- Ben Sason, Y.; Levy, J.; Oksenberg, A.; Sobel, J.; Behar, J.A. Positional Sleep Apnea Phenotyping Using Machine Learning and Digital Oximetry Biomarkers. Physiol. Meas. 2023, 44, 085001. [Google Scholar] [CrossRef] [PubMed]
- Elgendi, M.; Fletcher, R.R.; Tomar, H.; Allen, J.; Ward, R.; Menon, C. The Striking Need for Age Diverse Pulse Oximeter Databases. Front. Med. 2021, 8, 782422. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.; Álvarez, D.; Rosenberg, A.A.; Alexandrovich, A.; Del Campo, F.; Behar, J.A. Digital Oximetry Biomarkers for Assessing Respiratory Function: Standards of Measurement, Physiological Interpretation, and Clinical Use. npj Digit. Med. 2021, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, N.J.; Waltman, L. Software Survey: VOSviewer, a Computer Program for Bibliometric Mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- Masimo. Available online: https://www.masimo.com/company/masimo/awards/ (accessed on 24 September 2023).
- Ali, A.A.; Carothers, D.; Dalke, D.; Diab, M.K.; Goldman, J.; Kiani, M.E.; Lee, M.; Novak, J.; Smith, R.; Vaden, V.E. Dual-Mode Pulse Oximeter. U.S. Patent 6770028 B1, 3 August 2004. [Google Scholar]
- Ali, A.A. Low Power Pulse Oximeter. U.S. Patent 7295866 B2, 13 November 2007. [Google Scholar]
- Diab, M.K.; Ali, A.A. Pulse Oximeter Probe-Off Detector. U.S. Patent 7471969 B2, 30 December 2008. [Google Scholar]
- Ali, A.A.; Weber, W.M.; Mchale, R.T. System and Method for Monitoring the Life of a Physiological Sensor. U.S. Patent 7880626 B2, 1 February 2011. [Google Scholar]
- Kiani, M.J.E.; Diab, M.K.; Lamego, M.M. Robust Alarm System. U.S. Patent 7962188 B2, 14 June 2011. [Google Scholar]
- Kiani, M.E. Virtual Display. U.S. Patent 7990382 B2, 2 August 2011. [Google Scholar]
- Diab, M.K. Plethysmograph Pulse Recognition Processor. U.S. Patent 7988637 B2, 2 August 2011. [Google Scholar]
- Ali, A.A.; Breed, D.S.; Novak, J.J.; Kiani, M.E. Pulse Oximetry Data Confidence Indicator. U.S. Patent 8046040 B2, 25 October 2011. [Google Scholar]
- Ali, A.A.; Raths, C.; Usman, M. Systems and Methods for Patient Fall Detection. U.S. Patent 11089963 B2, 17 August 2021. [Google Scholar]
- Ali, A.A.; Kiani, J.; Diab, M.; Olsen, G.; Wu, R.; Fishel, R. Noninvasive Multi-Parameter Patient Monitor. U.S. Patent 8190223 B2, 29 May 2012. [Google Scholar]
- Ali, A.A.; Kinast, E.K.; Muhsin, B. Medical Monitoring Hub. U.S. Patent 11179114 B2, 23 November 2021. [Google Scholar]
- Ali, A.A.; Kinast, E.K.; Muhsin, B.; Dejong, C.A. Wireless Patient Monitoring Device. U.S. Patent 10149616 B2, 11 December 2018. [Google Scholar]
- Ali, A.A.; Indorf, K.W.; Kashif, F.; Usman, M. Patient Monitoring Device with Improved User Interface. U.S. Patent 11406286 B2, 9 August 2022. [Google Scholar]
- Muhsin, B.; Kiani, M.J.E.; Housel, P.S. System for Misplaying Medical Monitoring Data. U.S. Patent 11417426 B2, 16 August 2022. [Google Scholar]
- Diab, M.K.; Weber, W.M.; Ali, A.A. Method and Apparatus for Demodulating Signals in a Pulse Oximetry System. U.S. Patent 8185180 B2, 22 May 2012. [Google Scholar]
- Weber, W.M.; Ali, A.A. Physiological Measurement System with Automatic Wavelength Adjustment. U.S. Patent 10750983 B2, 25 August 2020. [Google Scholar]
- Perea, P.; Ali, A.A.; Kiani, M.J.E. Robust Fractional Saturation Determination. U.S. Patent 11089982 B2, 17 August 2021. [Google Scholar]
- Iyengar, P.; Novak, J.; Chandran, P.R. Physiological Measurement Calibration. U.S. Patent 10827961 B1, 10 November 2020. [Google Scholar]
- Ali, A.A. Patient Monitor Capable of Monitoring the Quality of Attached Probes and Accessories. U.S. Patent 9949676 B2, 24 April 2018. [Google Scholar]
- Ali, A.A. Variable Mode Pulse Indicator. U.S. Patent 10064562 B2, 4 September 2018. [Google Scholar]
- Ali, A.A.; Majmudar, A. Plethysmographic Respiration Rate Detection. U.S. Patent 11399722 B2, 2 August 2022. [Google Scholar]
- Ali, A.A.; Kiani, M.E.; Weber, W.M. Patient Monitor Having Context-Based Sensitivity Adjustments. U.S. Patent 8337403 B2, 25 December 2012. [Google Scholar]
- Muhsin, B.; Hwang, S.; Triman Benjamin, C. Physiological Monitor with Mobile Computing Device Connectivity. U.S. Patent 10736507 B2, 11 August 2020. [Google Scholar]
- Muhsin, B.; Hwang, S.; Triman Benjamin, C. Physiological Monitoring System. U.S. Patent 11504002 B2, 22 November 2022. [Google Scholar]
- Ali, A.A. Low Power Pulse Oximeter. U.S. Patent 10980455 B2, 20 April 2021. [Google Scholar]
- Ali, A.A.; Smith, R.A.; Mccarthy, R.J. Multipurpose Sensor Port. U.S. Patent 11020029 B2, 1 June 2021. [Google Scholar]
- Ali, A.A.; Kiani, M.E.; Weber, W.M. Application Identification Sensor. U.S. Patent 7438683 B2, 21 October 2008. [Google Scholar]
- Ali, A.A.; Weber, W.M.; Kiani, J.E. Configurable Physiological Measurement System. U.S. Patent 7729733 B2, 1 June 2010. [Google Scholar]
- Smith, R.; Dalke, D.; Ali, A.A.; Diab, M.; Lamego, M. Multiple Wavelength Sensor Emitters. U.S. Patent 7764982 B2, 27 July 2010. [Google Scholar]
- Dyell, D.; Rogowski, C.; Kahler, S.; Milan, J. Real-Time Monitoring Systems and Methods in a Healthcare Environment. U.S. Patent 11581091 B2, 14 February 2023. [Google Scholar]
- Kiani, M.J.E.; Cebada, S.L.; Olsen, G.A. Alarm suspend system. U.S. Patent 8203438 B2, 19 June 2012. [Google Scholar]
- Poeze, J.; Lamego, M.; Merritt, S.; Dalvi, C.; Vo, H.; Bruinsma, J.; Lesmana, F.; Kiani, M.J.E. User-Worn Device for Noninvasively Measuring a Physiological Parameter of a User. U.S. Patent 11484230 B2, 22 November 2022. [Google Scholar]
- Poeze, J.; Lamego, M.; Merritt, S.; Dalvi, C.; Vo, H.; Bruinsma, J.; Lesmana, F.; Kiani, M.J.E.; Olsen, G. Multi-Stream Data Collection System for Noninvasive Measurement of Blood Constituents. U.S. Patent 10758166 B2, 1 September 2020. [Google Scholar]
- Castillo, A.; Deulofeut, R.; Critz, A.; Sola, A. Prevention of Retinopathy of Prematurity in Preterm Infants through Changes in Clinical Practice and SpO2 Technology. Acta Paediatr. 2011, 100, 188–192. [Google Scholar] [CrossRef]
- Zhao, Q.; Ma, X.; Ge, X.; Liu, F.; Yan, W.; Wu, L.; Ye, M.; Liang, X.; Zhang, J.; Gao, Y.; et al. Pulse Oximetry with Clinical Assessment to Screen for Congenital Heart Disease in Neonates in China: A Prospective Study. Lancet 2014, 384, 747–754. [Google Scholar] [CrossRef]
- McGrath, S.P.; Taenzer, A.H.; Karon, N.; Blike, G. Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 293–302. [Google Scholar] [CrossRef]
- Anand, S.; Bilal, M. Intelligent Medical Escalation Process. U.S. Patent 10833983 B2, 10 November 2020. [Google Scholar]
- Ali, A.A. Physiological Measurement Logic Engine. U.S. Patent 11399774 B2, 2 August 2022. [Google Scholar]
- Sampath, A.; Muhsin, B.; Housel, P.S. Medical Communication Protocol Translator. U.S. Patent 11145408 B2, 21 October 2021. [Google Scholar]
- Sampath, A.; Kiani, M.J.E.; Muhsin, B. Medical Monitoring System. U.S. Patent 11133105 B2, 28 September 2021. [Google Scholar]
- Muhsin, B.; Sultanov, E.; Quong, S. Alarm Notification System. U.S. Patent 11488711 B2, 1 November 2022. [Google Scholar]
- Ali, A.A. Physiological Measurement Communications Adapter. U.S. Patent 7844315 B2, 30 November 2010. [Google Scholar]
- Sampath, A.; Muhsin, B. Systems and Methods for Storing, Analyzing, and Retrieving Medical Data. U.S. Patent 8274360 B2, 25 September 2012. [Google Scholar]
- Muhsin, B.; Ali, A.A.; Kiani, M.J.E.; Housel, P.S. System for Displaying Medical Monitoring Data. U.S. Patent 9943269 B2, 17 April 2018. [Google Scholar]
- Kiani, M.J.E.; Muhsin, B.; Ali, A.A.; Indorf, K.W.; Ahmed, O.; Novak, J.; Weber, W.M. Opioid Overdose Monitoring. U.S. Patent 10939878 B2, 9 March 2021. [Google Scholar]
- Kiani, M.J.E.; Muhsin, B. Wearable Pulse Oximeter for Tennis Players. U.S. Application 2022/0218244 A1, 22 January 2022. [Google Scholar]
- Nellcor. Available online: https://everipedia.org/wiki/lang_en/Nellcor (accessed on 24 September 2023).
- Berson, T.A.; Olson, B.; Fein, M.E.; Mannheimer, P.D.; Porges, C.E.; Schloemer, D. Sensor with signature of data relating to sensor. U.S. Patent 6708049 B1, 16 March 2004. [Google Scholar]
- Swedlow, D.B.; Daleo, S.L.; Yorkey, T.J.; Richards, E.M.; Porges, C.; Stuart, C.; Nemits, D.M.; Delonzor, R.L. Method and Circuit for Storing and Providing Historical Physiological Data. U.S. Patent 6463310 B1, 8 October 2002. [Google Scholar]
- Porges, C.; Baker, C.; Yorkey, T.J.; Bernstein, M.; Mannheimer, P. Method and Circuit for Indicating Quality and Accuracy of Physiological Measurements. U.S. Patent 6675031 B1, 6 January 2004. [Google Scholar]
- Mannheimer, P.D.; Fein, M.E.; Porges, C.E. Pulse Oximeter Sensor with Piece-Wise Function. U.S. Patent 6801797 B2, 5 October 2004. [Google Scholar]
- Fein, M.E.; Mannheimer, P.D.; Merchant, A.; Porges, C.; Swedlow, D. Oximeter Sensor with Digital Memory Recording Sensor Data. U.S. Patent 6591123 B2, 8 July 2003. [Google Scholar]
- Smit, P.C.; Antunes, A.; Montgomery, D.; Addison, P.S. Oxygen Saturation Monitoring Using Artificial Intelligence. U.S. Patent 11517226 B2, 6 December 2022. [Google Scholar]
- Graboi, D.G.; Doyle, P. Retinopathy of Prematurity Determination and Alarm System. U.S. Patent 8374666 B2, 12 February 2013. [Google Scholar]
- Montgomery, D.; Addison, P.S.; Antunes, A. Autoregulation Monitoring Using Deep Learning. WO 2022/204668 A1, 21 March 2022. [Google Scholar]
- Miyasaka, K.; Shelley, K.; Takahashi, S.; Kubota, H.; Ito, K.; Yoshiya, I.; Yamanishi, A.; Cooper, J.B.; Steward, D.J.; Nishida, H.; et al. Tribute to Dr. Takuo Aoyagi, Inventor of Pulse Oximetry. J. Anesth. 2021, 35, 671–709. [Google Scholar] [CrossRef]
- Aoyagi, T.; Fuse, M.; Kobayashi, N.; Ukawa, T. Pulse Oximeter. U.S. Patent 7206621 B2, 17 April 2007. [Google Scholar]
- Sugo, Y.; Kobayashi, N.; Takeda, S. Method and Apparatus for Measuring Pulse Rate and Oxygen Saturation Achieved during Exercise. U.S. Patent 8649837 B2, 11 February 2014. [Google Scholar]
- Koyama, Y. Patient Monitor. U.S. Patent 11291414 B2, 5 April 2022. [Google Scholar]
- Yokota, T.; Zalar, P.; Kaltenbrunner, M.; Jinno, H.; Matsuhisa, N.; Kitanosako, H.; Tachibana, Y.; Yukita, W.; Koizumi, M.; Someya, T. Ultraflexible Organic Photonic Skin. Sci. Adv. 2016, 2, e1501856. [Google Scholar] [CrossRef]
- Shelley, K.H. Photoplethysmography: Beyond the Calculation of Arterial Oxygen Saturation and Heart Rate. Anesth. Analg. 2007, 105, S31–S36. [Google Scholar] [CrossRef]
- Desautels, T.; Calvert, J.; Hoffman, J.; Jay, M.; Kerem, Y.; Shieh, L.; Shimabukuro, D.; Chettipally, U.; Feldman, M.D.; Barton, C.; et al. Prediction of Sepsis in the Intensive Care Unit With Minimal Electronic Health Record Data: A Machine Learning Approach. JMIR Med. Inform. 2016, 4, e28. [Google Scholar] [CrossRef] [PubMed]
- Reisner, A.; Shaltis, P.A.; McCombie, D.; Asada, H.H.; Warner, D.S.; Warner, M.A. Utility of the Photoplethysmogram in Circulatory Monitoring. Anesthesiology 2008, 108, 950–958. [Google Scholar] [CrossRef]
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol. 2017, 15, e2001402. [Google Scholar] [CrossRef]
- Cabanas, A.M.; Martín-Escudero, P.; Shelley, K.H. Improving pulse oximetry accuracy in dark-skinned patients: Technical aspects and current regulations. Br. J. Anaesth. 2023, 131, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.T.; Poh, S.C. Noninvasive Oximetry in Pigmented Patients. Ann. Acad. Med. Singap. 1985, 14, 427–429. [Google Scholar] [PubMed]
- Bothma, P.A.; Joynt, G.M.; Lipman, J.; Hon, H.; Mathala, B.; Scribante, J.; Kromberg, J. Accuracy of pulse oximetry in pigmented patients. S. Afr. Med. J. 1996, 86, 594–596. [Google Scholar] [PubMed]
- Silverston, P.; Ferrari, M.; Quaresima, V. Pulse oximetry and the pandemic. BMJ 2022, 378, e071474. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, S.G.; Daggubati, V.; Alexandrakis, G. Innovative Technology to Eliminate the Racial Bias in Non-Invasive, Point-of-Care (POC) Haemoglobin and Pulse Oximetry Measurements. BMJ Innov. 2023, 9, 73–77. [Google Scholar] [CrossRef]
- Matos, J.; Struja, T.; Gallifant, J.; Charpignon, M.-L.; Cardoso, J.S.; Celi, L.A. Shining Light on Dark Skin: Pulse Oximetry Correction Models. In Proceedings of the 2023 IEEE 7th Portuguese Meeting on Bioengineering (ENBENG), Porto, Portugal, 22–23 June 2023; pp. 211–214. [Google Scholar] [CrossRef]
- Ostojic, D.; Guglielmini, S.; Moser, V.; Fauchère, J.C.; Bucher, H.U.; Bassler, D.; Wolf, M.; Kleiser, S.; Scholkmann, F.; Karen, T. Reducing False Alarm Rates in Neonatal Intensive Care: A New Machine Learning Approach. In Oxygen Transport to Tissue XLI; Ryu, P.-D., LaManna, J.C., Harrison, D.K., Lee, S.-S., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2020; Volume 1232, pp. 285–290. [Google Scholar] [CrossRef]
- Rea, M.S.; Bierman, A. Light source spectra are the likely cause of systematic bias in pulse oximeter readings for individuals with darker skin pigmentation. Br. J. Anaesth. 2023, 131, e101–e103. [Google Scholar] [CrossRef]
- Oteo, A.; Daneshvar, H.; Baldacchino, A.; Matheson, C. Overdose Alert and Response Technologies: State-of-the-Art Review. J. Med. Internet Res. 2023, 25, e40389. [Google Scholar] [CrossRef]
- Massoomi, M.R.; Handberg, E.M. Increasing and Evolving Role of Smart Devices in Modern Medicine. Eur. Cardiol. 2019, 14, 181–186. [Google Scholar] [CrossRef]
- Garmin. Available online: https://www.garmin.com/en-US/c/wearables-smartwatches/?sorter=productName-asc¤tPage=1 (accessed on 24 September 2023).
- Mitro, N.; Argyri, K.; Pavlopoulos, L.; Kosyvas, D.; Karagiannidis, L.; Kostovasili, M.; Misichroni, F.; Ouzounoglou, E.; Amditis, A. AI-Enabled Smart Wristband Providing Real-Time Vital Signs and Stress Monitoring. Sensors 2023, 23, 2821. [Google Scholar] [CrossRef]
- Windisch, P.; Schröder, C.; Förster, R.; Cihoric, N.; Zwahlen, D.R. Accuracy of the Apple Watch Oxygen Saturation Measurement in Adults: A Systematic Review. Cureus 2023, 15, e35355. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Elgalad, A.; Cardoso, C.; Perin, E.C. Using the Apple Watch to Record Multi-ple-Lead Electrocardiograms in Detecting Myocardial Infarction: Where Are We Now? Tex. Heart Inst. J. 2022, 49, e227845. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.apple.com/au/newsroom/2021/05/ecg-app-and-irregular-rhythm-notification-now-available-on-apple-watch/ (accessed on 1 November 2023).
- Available online: https://webgate.ec.europa.eu/udi-helpdesk/en/other-relevant-information/medical-device-classification.html (accessed on 1 November 2023).
- Bazoukis, G.; Bollepalli, S.C.; Chung, C.T.; Li, X.; Tse, G.; Bartley, B.L.; Batool-Anwar, S.; Quan, S.F.; Armoundas, A.A. Application of Artificial Intelligence in the Diagnosis of Sleep Apnea. J. Clin. Sleep Med. 2023, 19, 1337–1363. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xuan, W.; Chen, D.; Gu, Y.; Liu, F.; Chen, J.; Xia, S.; Dong, S.; Luo, J. Machine Learning Assisted Wearable Wireless Device for Sleep Apnea Syndrome Diagnosis. Biosensors 2023, 13, 483. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Tang, K.; Hsu, Y.-C.; Huang, T.; Wang, D.; Li, W.; Savitz, S.I.; Jiang, X.; Shams, S. Non-Invasive Arterial Blood Pressure Measurement and SpO2 Estimation Using PPG Signal: A Deep Learning Framework. BMC Med. Inform. Decis. Mak. 2023, 23, 131. [Google Scholar] [CrossRef]
- Huang, J.; Chen, H.; Deng, J.; Liu, X.; Shu, T.; Yin, C.; Duan, M.; Fu, L.; Wang, K.; Zeng, S. Interpretable Machine Learning for Predicting 28-Day All-Cause in-Hospital Mortality for Hypertensive Ischemic or Hemorrhagic Stroke Patients in the ICU: A Multi-Center Retrospective Cohort Study with Internal and External Cross-Validation. Front. Neurol. 2023, 14, 1185447. [Google Scholar] [CrossRef]
- Kerexeta, J.; Larburu, N.; Escolar, V.; Lozano-Bahamonde, A.; Macía, I.; Beristain Iraola, A.; Graña, M. Prediction and Analysis of Heart Failure Decompensation Events Based on Telemonitored Data and Artificial Intelligence Methods. J. Cardiovasc. Dev. Dis. 2023, 10, 48. [Google Scholar] [CrossRef]
- Siao, R.M.; So, M.J.; Gomez, M.H. Pulse Oximetry as a Screening Test for Hemodynamically Significant Lower Extremity Peripheral Artery Disease in Adults with Type 2 Diabetes Mellitus. J. ASEAN Fed. Endocr. Soc. 2018, 33, 130–136. [Google Scholar] [CrossRef]
- Ashfaq, Z.; Mumtaz, R.; Rafay, A.; Zaidi, S.M.H.; Saleem, H.; Mumtaz, S.; Shahid, A.; Poorter, E.D.; Moerman, I. Embedded AI-Based Digi-Healthcare. Appl. Sci. 2022, 12, 519. [Google Scholar] [CrossRef]
- Talha, S.; Lamrous, S.; Kassegne, L.; Lefebvre, N.; Zulfiqar, A.-A.; Tran Ba Loc, P.; Geny, M.; Meyer, N.; Hajjam, M.; Andrès, E.; et al. Early Hospital Discharge Using Remote Monitoring for Patients Hospitalized for COVID-19, Regardless of Need for Home Oxygen Therapy: A Descriptive Study. J. Clin. Med. 2023, 12, 5100. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L.; Ding, X.; Clifton, D.; Lu, H. Wearable Vital Signs Monitoring for Patients With Asthma: A Review. IEEE Sens. J. 2023, 23, 1734–1751. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Velardo, C.; Farmer, A.; Tarassenko, L. Exacerbations in Chronic Obstructive Pulmonary Disease: Identification and Prediction Using a Digital Health System. J. Med. Internet Res. 2017, 19, e69. [Google Scholar] [CrossRef]
- Gunasekeran, D.V.; Tseng, R.M.W.W.; Tham, Y.C.; Wong, T.Y. Applications of digital health for public health responses to COVID-19: A systematic scoping review of artificial intelligence, telehealth and related technologies. npj Digit. Med. 2021, 4, 40. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Torkamani, A.; Butte, A.J.; Glicksberg, B.S.; Schuller, B.; Rodriguez, B.; Ting, D.S.W.; Bates, D.; Schaden, E.; Peng, H.; et al. The promise of digital healthcare technologies. Front. Public Health 2023, 11, 1196596. [Google Scholar] [CrossRef]
- Atanasov, A.G. Exploration of Digital Health Technologies. Explor. Digit. Health Technol. 2023, 1, 1–3. [Google Scholar] [CrossRef]
- Sun, Y.; Salerno, S.; He, X.; Pan, Z.; Yang, E.; Sujimongkol, C.; Song, J.; Wang, X.; Han, P.; Kang, J.; et al. Use of Machine Learning to Assess the Prognostic Utility of Radiomic Features for In-Hospital COVID-19 Mortality. Sci. Rep. 2023, 13, 7318. [Google Scholar] [CrossRef]
- Boonnag, C.; Ittichaiwong, P.; Saengmolee, W.; Seesawad, N.; Chinkamol, A.; Rattanasomrerk, S.; Veerakanjana, K.; Thanontip, K.; Limpornchitwilai, W.; Wilaiprasitporn, T. PACMAN: A Framework for Pulse Oximeter Digit Detection and Reading in a Low-Resource Setting. IEEE Internet Things J. 2023, 10, 13196–13204. [Google Scholar] [CrossRef]
- Mathew, J.; Tian, X.; Wong, C.-W.; Ho, S.; Milton, D.K.; Wu, M. Remote Blood Oxygen Estimation From Videos Using Neural Networks. IEEE J. Biomed. Health Inform. 2023, 27, 3710–3720. [Google Scholar] [CrossRef]
- Villafuerte, N.; Manzano, S.; Ayala, P.; García, M.V. Artificial Intelligence in Virtual Telemedicine Triage: A Respiratory Infection Diagnosis Tool with Electronic Measuring Device. Future Internet 2023, 15, 227. [Google Scholar] [CrossRef]
- Van Den Berg, M.; Medina, O.; Loohuis, I.; Van Der Flier, M.; Dudink, J.; Benders, M.; Bartels, R.; Vijlbrief, D. Development and Clinical Impact Assessment of a Machine-Learning Model for Early Prediction of Late-Onset Sepsis. Comput. Biol. Med. 2023, 163, 107156. [Google Scholar] [CrossRef] [PubMed]
- Sabri, K.; Ells, A.L.; Lee, E.Y.; Dutta, S.; Vinekar, A. Retinopathy of Prematurity: A Global Perspective and Recent Developments. Pediatrics 2022, 150, e2021053924. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-B.; Lee, H.-J.; Yang, H.-L.; Kim, E.-H.; Lee, H.-C.; Jung, C.-W.; Kim, H.-S. Machine Learning-Based Prediction of Intraoperative Hypoxemia for Pediatric Patients. PLoS ONE 2023, 18, e0282303. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Lim, H.-G.; Park, W.; Kim, D.; Yoon, J.S.; Lee, S.-M.; Kim, K. Development of a Machine Learning Model for the Prediction of the Short-Term Mortality in Patients in the Intensive Care Unit. J. Crit. Care 2022, 71, 154106. [Google Scholar] [CrossRef]
- Fang, Z.; Zou, D.; Xiong, W.; Bao, H.; Zhao, X.; Chen, C.; Si, Y.; Zou, J. Dynamic Prediction of Hypoxemia Risk at Different Time Points Based on Preoperative and Intraoperative Features: Machine Learning Applications in Outpatients Undergoing Esophagogastroduodenoscopy. Ann. Med. 2023, 55, 1156–1167. [Google Scholar] [CrossRef]
- Yamga, E.; Mantena, S.; Rosen, D.; Bucholz, E.M.; Yeh, R.W.; Celi, L.A.; Ustun, B.; Butala, N.M. Optimized Risk Score to Predict Mortality in Patients With Cardiogenic Shock in the Cardiac Intensive Care Unit. J. Am. Heart Assoc. 2023, 12, e029232. [Google Scholar] [CrossRef]
- Strickler, E.A.T.; Thomas, J.; Thomas, J.P.; Benjamin, B.; Shamsuddin, R. Exploring a Global Interpretation Mechanism for Deep Learning Networks When Predicting Sepsis. Sci. Rep. 2023, 13, 3067. [Google Scholar] [CrossRef]


| Entity | Record Count | % |
|---|---|---|
| Affiliations | ||
| University of California system | 35 | 3.57 |
| Harvard University | 34 | 3.47 |
| University of Oxford | 22 | 2.25 |
| Massachusetts Institute of Technology | 18 | 1.84 |
| Massachusetts General Hospital | 17 | 1.74 |
| Journals | ||
| Sensors | 28 | 2.86 |
| Proceedings of SPIE | 23 | 2.35 |
| PLOS One | 18 | 1.84 |
| Scientific reports | 17 | 1.74 |
| Physiological measurement | 13 | 1.33 |
| Title | Year of Publication | Average per Year | Total Citations |
|---|---|---|---|
| Ultraflexible organic photonic skin | 2016 | 84.75 | 678 |
| Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate | 2007 | 17.65 | 300 |
| Prediction of sepsis in the intensive care unit with minimal electronic health record data: a machine learning approach | 2016 | 28.25 | 226 |
| Utility of the photoplethysmogram in circulatory monitoring | 2008 | 14.13 | 226 |
| Digital Health: tracking physiomes and activity using wearable biosensors reveals useful health-related information | 2017 | 30.29 | 212 |
| Keywords | Occurrences |
|---|---|
| Machine learning | 200 |
| Oxygen saturation | 109 |
| Pulse oximetry | 100 |
| COVID-19 | 76 |
| Photoplethysmography | 59 |
| Oximetry | 52 |
| Mortality | 49 |
| Prediction | 46 |
| Risk | 46 |
| Diagnosis | 45 |
| Artificial intelligence | 41 |
| Pulse oximeter | 37 |
| Management | 35 |
| Accuracy | 34 |
| Deep learning | 30 |
| Care | 28 |
| Telemedicine | 28 |
| Digital health | 27 |
| Sleep apnea | 27 |
| Outcomes | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Litvinova, O.; Hammerle, F.P.; Stoyanov, J.; Ksepka, N.; Matin, M.; Ławiński, M.; Atanasov, A.G.; Willschke, H. Patent and Bibliometric Analysis of the Scientific Landscape of the Use of Pulse Oximeters and Their Prospects in the Field of Digital Medicine. Healthcare 2023, 11, 3003. https://doi.org/10.3390/healthcare11223003
Litvinova O, Hammerle FP, Stoyanov J, Ksepka N, Matin M, Ławiński M, Atanasov AG, Willschke H. Patent and Bibliometric Analysis of the Scientific Landscape of the Use of Pulse Oximeters and Their Prospects in the Field of Digital Medicine. Healthcare. 2023; 11(22):3003. https://doi.org/10.3390/healthcare11223003
Chicago/Turabian StyleLitvinova, Olena, Fabian Peter Hammerle, Jivko Stoyanov, Natalia Ksepka, Maima Matin, Michał Ławiński, Atanas G. Atanasov, and Harald Willschke. 2023. "Patent and Bibliometric Analysis of the Scientific Landscape of the Use of Pulse Oximeters and Their Prospects in the Field of Digital Medicine" Healthcare 11, no. 22: 3003. https://doi.org/10.3390/healthcare11223003
APA StyleLitvinova, O., Hammerle, F. P., Stoyanov, J., Ksepka, N., Matin, M., Ławiński, M., Atanasov, A. G., & Willschke, H. (2023). Patent and Bibliometric Analysis of the Scientific Landscape of the Use of Pulse Oximeters and Their Prospects in the Field of Digital Medicine. Healthcare, 11(22), 3003. https://doi.org/10.3390/healthcare11223003








