Etiology of Exercise Injuries in Firefighters: A Healthcare Practitioners’ Perspective
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Procedures
2.4. Data Analysis
3. Results
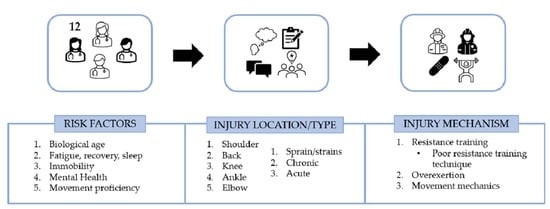
3.1. Injury Locations and Types
3.2. Risk Factors
3.3. Injury Mechanisms
4. Discussion
Clinical Significance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular disease in US firefighters: A systematic review. Cardiol. Rev. 2011, 19, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Lovejoy, S.; Gillespie, G.L.; Christianson, J. Exploring physical health in a sample of firefighters. Workplace Health Saf. 2015, 63, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Dennison, K.J.; Mullineaux, D.R.; Yates, J.W.; Abel, M.G. The effect of fatigue and training status on firefighter performance. J. Strength Cond. Res. 2012, 26, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.; Petrillo, J.T. Fatal firefighter injuries in the US in 2022. National Fire Protection Association. 2023. Available online: https://www.nfpa.org//-/media/Files/News-and-Research/Fire-statistics-and-reports/Emergency-responders/osFFF.pdf (accessed on 22 October 2023).
- Durand, G.; Tsismenakis, A.J.; Jahnke, S.A.; Baur, D.M.; Christophi, C.A.; Kales, S.N. Firefighters’ physical activity: Relation to fitness and cardiovascular disease risk. Med. Sci. Sports Exerc. 2011, 43, 1752–1759. [Google Scholar] [CrossRef]
- Poston, W.S.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J. Occup. Environ. Med. 2011, 53, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Michaelides, M.A.; Parpa, K.M.; Henry, L.J.; Thompson, G.B.; Brown, B.S. Assessment of physical fitness aspects and their relationship to firefighters’ job abilities. J. Strength Cond. Res. 2011, 25, 956–965. [Google Scholar] [CrossRef]
- Norris, M.S.; McAllister, M.; Gonzalez, A.E.; Best, S.A.; Pettitt, R.; Keeler, J.M.; Abel, M.G. Predictors of Work efficiency in structural firefighters. J. Occup. Environ. Med. 2021, 63, 622–628. [Google Scholar] [CrossRef]
- Rhea, M.R.; Alvar, B.A.; Gray, R. Physical fitness and job performance of firefighters. J. Strength Cond. Res. 2004, 18, 348–352. [Google Scholar] [CrossRef]
- Hollerbach, B.S.; Jahnke, S.A.; Poston, W.S.C.; Harmsc, C.A.; Heinrich, K.M. Examining a novel firefighter exercise training program on simulated fire ground test performance, cardiorespiratory endurance, and strength: A pilot investigation. J. Occup. Med. Toxicol. 2019, 14, 12. [Google Scholar] [CrossRef]
- Pawlak, R.; Clasey, J.L.; Palmer, T.; Symons, T.B.; Abel, M.G. The effect of a novel tactical training program on physical fitness and occupational performance in firefighters. J. Strength Cond. Res. 2015, 29, 578–588. [Google Scholar] [CrossRef]
- Wohlgemuth, K.J.; Gerstner, G.R.; Giuliani-Dewig, H.K.; Mota, J.A.; Smith-Ryan, A.E.; Ryan, E.D. The time course of health, fitness, and occupational performance changes in recruits across a fire academy. Med. Sci. Sports Exerc. 2023, 55, 1087–1096. [Google Scholar] [CrossRef] [PubMed]
- Dworsky, M.; Seabury, S.A.; Broten, N. The frequency and economic impact of musculoskeletal disorders for California firefighters: Trends and outcomes over the past decade. Rand Health Q. 2021, 9, 4. [Google Scholar] [PubMed]
- Poplin, G.S.; Roe, D.J.; Peate, W.; Harris, R.B.; Burgess, J.L. The association of aerobic fitness with injuries in the fire service. Am. J. Epidemiol. 2014, 179, 149–155. [Google Scholar] [CrossRef]
- Jahnke, S.A.; Poston, W.S.; Haddock, C.K.; Jitnarin, N. Injury among a population based sample of career firefighters in the central USA. Inj. Prev. 2013, 19, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Poplin, G.S.; Harris, R.B.; Pollack, K.M.; Peate, W.F.; Burgess, J.L. Beyond the fireground: Injuries in the fire service. Inj. Prev. 2012, 18, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Frost, D.M.; Beach, T.A.C.; Crosby, I.; McGill, S.M. Firefighter injuries are not just a fireground problem. Work 2015, 52, 835–842. [Google Scholar] [CrossRef]
- Walton, S.M.; Conrad, K.M.; Furner, S.E.; Samo, D.G. Cause, type, and workers’ compensation costs of injury to fire fighters. Am. J. Ind. Med. 2003, 43, 454–458. [Google Scholar] [CrossRef]
- Groenewald, T.A. Phenomenological research design illustrated. Int. J. Qual. Methods 2004, 3, 42–55. [Google Scholar] [CrossRef]
- Broomé, R.E.; Russell, E.J. What is it like to self-rescue from a building collapse as a firefighter: A phenomenological Inquiry? J. Phenomenol. Psychol. 2019, 50, 225–248. [Google Scholar] [CrossRef]
- McFarlane, A.C. The phenomenology of posttraumatic stress disorders following a natural disaster. J. Nerv. Ment. Dis. 1988, 176, 22–29. [Google Scholar] [CrossRef]
- Sinden, K.; MacDermid, J.; Buckman, S.; Davis, B.; Matthews, T.; Viola, C. A qualitative study on the experiences of female firefighters. Work 2013, 45, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Conrad, K.M.; Balch, G.I.; Reichelt, P.A.; Muran, S.; Oh, K. Musculoskeletal injuries in the fire service: Views from a focus group study. AAOHN J. 1994, 42, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Orr, R.; Simas, V.; Canetti, E.; Schram, B. A profile of injuries sustained by firefighters: A critical review. Int. J. Environ. Res. Public Health 2019, 16, 3931. [Google Scholar] [CrossRef] [PubMed]
- Trivisonno, A.J.; Laffan, M.R.; Giuliani, H.K.; Mota, J.A.; Gerstner, G.R.; Smith-Ryan, A.E.; Ryan, E.D. The influence of age on the recovery from worksite resistance exercise in career firefighters. Exp. Gerontol. 2021, 152, 111467. [Google Scholar] [CrossRef] [PubMed]
- Frontera, W.R. Physiologic changes of the musculoskeletal system with aging: A brief review. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Frost, D.M.; Beach, T.A.C.; Callaghan, J.P.; McGill, S.M. Exercise-based performance enhancement and injury prevention for firefighters. J. Strength Cond. Res. 2015, 29, 2441–2459. [Google Scholar] [CrossRef]
- Butler, R.J.; Contreras, M.; Burton, L.C.; Plisky, P.J.; Goode, A.; Kiesel, K. Modifiable risk factors predict injuries in firefighters during training academies. Work 2013, 46, 11–17. [Google Scholar] [CrossRef]
- Gerstner, G.R.; Mota, J.A.; Giuliani, H.K.; Weaver, M.A.; Shea, N.W.; Ryan, E.D. The impact of repeated bouts of shiftwork on rapid strength and reaction time in career firefighters. Ergonomics 2022, 65, 1086–1094. [Google Scholar] [CrossRef]
- Toczko, M.; Fyock-Martin, M.; McCrory, S.; Martin, J. Effects of fitness on self-reported physical and mental quality of life in professional firefighters: An exploratory study. Work 2023, in press. [CrossRef]
- Beach, T.A.C.; Frost, D.M.; McGill, S.M.; Callaghan, J.P. Physical fitness improvements and occupational low-back loading—An exercise intervention study with firefighters. Ergonomics 2014, 57, 744–763. [Google Scholar] [CrossRef]
- Kumar, S. Theories of musculoskeletal injury causation. Ergonomics 2001, 44, 17–47. [Google Scholar] [CrossRef] [PubMed]
- Le, A.B.; Smith, T.D.; McNulty, L.A.; Dyal, M.A.; Dejoy, D.M. Firefighter overexertion: A continuing problem found in an analysis of non-fatal injury among career firefighters. Int. J. Environ. Res. Public Health 2020, 17, 7906. [Google Scholar] [CrossRef] [PubMed]
| Subject # | Education | Clinical Credential | Years of Clinical Experience | Years of Experience with Tactical Population | Observed Firefighter Tasks | Firefighter Patient Encounters (Weekly) | Total Treatment Encounters |
|---|---|---|---|---|---|---|---|
| 1 | Bachelor’s | AT, CSCS | 15 | 12 | Yes | 25 | 15,600 |
| 2 | Doctorate | AT, CSCS | 10 | 2 | Yes | 45 | 4680 |
| 3 | Doctorate | AT | 5 | 5 | Yes | 80 | 20,800 |
| 4 | Master’s | AT | 7 | 3 | Yes | 30 | 4680 |
| 5 | Doctorate | PT, CSCS | 10 | 8 | Yes | 8 | 3328 |
| 6 | Doctorate | AT and PT | 11 | 4 | Yes | 5 | 1040 |
| 7 | Master’s | AT | 17 | 7 | Yes | 60 | 21,840 |
| 8 | Doctorate | PT | 5 | 5 | Yes | 2 | 520 |
| 9 | Doctorate | PT | 13 | 7 | Yes | 25 | 9100 |
| 10 | Master’s | AT | 5 | 2 | Yes | 12 | 1248 |
| 11 | Doctorate | NP | 42 | 16 | Yes | 8 | 6656 |
| 12 | Master’s | AT | 3 | 1 | Yes | - | - |
| Mean | 11.9 | 6.0 | 27.3 | 8135.6 | |||
| SD | 10.4 | 4.4 | 25.1 | 7809.1 | |||
| Main Code | Aim 1: Exercise Injuries | Aim 2: Exercise Injury Risk Factors | Aim 3: Exercise Injury Mechanisms |
|---|---|---|---|
| Injury type | X | ||
| Injury location | X | ||
| Injury setting | X | X | X |
| Risk factor | X | ||
| Injury mechanism | X |
| Main Code | Sub-Code |
|---|---|
| Injury Type | Acute |
| Chronic | |
| Tendonitis/tendinosis | |
| Sprain/strain | |
| Chronic to acute | |
| Injury Location | Ankle |
| Back | |
| Elbow | |
| Knee | |
| Shoulder | |
| Injury Setting | Exercise related |
| Occupationally related | |
| Personal | |
| Risk Factor | Biological age |
| Fatigue | |
| Immobility | |
| Recovery | |
| Mental health | |
| Movement proficiency | |
| Training age | |
| Nutrition | |
| Injury Mechanisms | Resistance training (poor lifting technique) |
| Movement mechanics | |
| Overexertion |
| Injury Anatomical Locations (18 Excerpts) | ||||
|---|---|---|---|---|
| Shoulder | Back | Knee | Ankle | Elbow |
| 83% | 73% | 28% | 17% | 11% |
| Type of Injury (17 Excerpts) | ||||
| Sprains/Strains | Chronic | Acute | ||
| 65% | 53% | 29% | ||
| Risk Factors | 73 Excerpts |
|---|---|
| Biological age | 21% |
| Fatigue, recovery, and sleep | 21% |
| Immobility | 19% |
| Mental health | 15% |
| Movement proficiency | 21% |
| Injury Mechanism | 35 Excerpts |
|---|---|
| Resistance training | 51% |
| a. Poor resistance training technique | 44% |
| Overexertion | 20% |
| Movement mechanics | 14% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eastman, A.Q.; Rous, B.; Langford, E.L.; Tatro, A.L.; Heebner, N.R.; Gribble, P.A.; Lanphere, R.; Abel, M.G. Etiology of Exercise Injuries in Firefighters: A Healthcare Practitioners’ Perspective. Healthcare 2023, 11, 2989. https://doi.org/10.3390/healthcare11222989
Eastman AQ, Rous B, Langford EL, Tatro AL, Heebner NR, Gribble PA, Lanphere R, Abel MG. Etiology of Exercise Injuries in Firefighters: A Healthcare Practitioners’ Perspective. Healthcare. 2023; 11(22):2989. https://doi.org/10.3390/healthcare11222989
Chicago/Turabian StyleEastman, Alyssa Q., Beth Rous, Emily L. Langford, Anne Louise Tatro, Nicholas R. Heebner, Phillip A. Gribble, Rosie Lanphere, and Mark G. Abel. 2023. "Etiology of Exercise Injuries in Firefighters: A Healthcare Practitioners’ Perspective" Healthcare 11, no. 22: 2989. https://doi.org/10.3390/healthcare11222989
APA StyleEastman, A. Q., Rous, B., Langford, E. L., Tatro, A. L., Heebner, N. R., Gribble, P. A., Lanphere, R., & Abel, M. G. (2023). Etiology of Exercise Injuries in Firefighters: A Healthcare Practitioners’ Perspective. Healthcare, 11(22), 2989. https://doi.org/10.3390/healthcare11222989