Adapting a Clinical Practice Guideline for Management of Patients with Knee and Hip Osteoarthritis by Hong Kong Physiotherapists
Abstract
:1. Introduction
2. Materials and Methods
2.1. Phase 1: Setup
2.2. Phase 2: Adaptation
2.2.1. Scope and Purpose Module
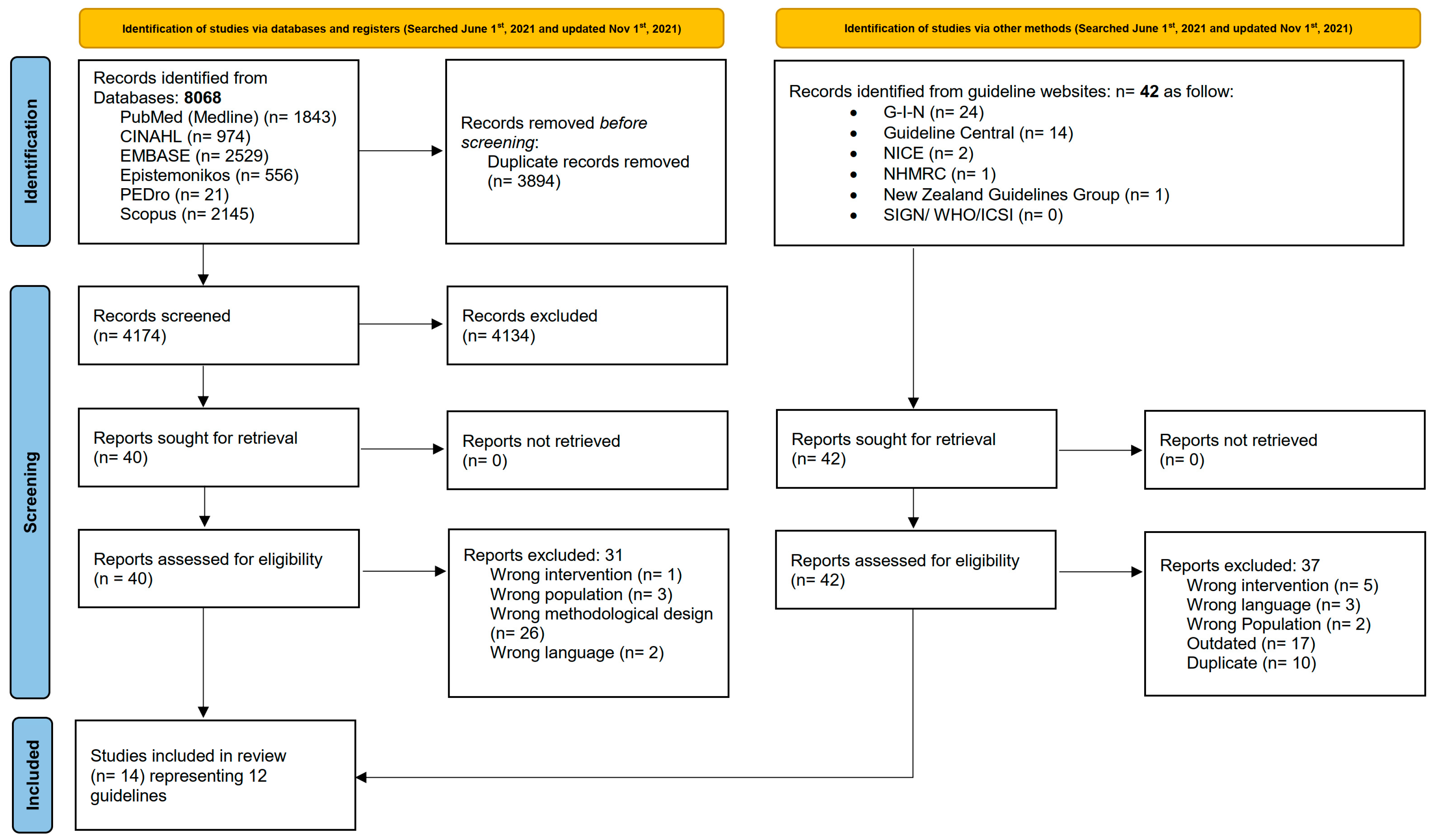
2.2.2. Search and Screen Module
2.2.3. Quality Assessment Module
2.2.4. Extracting Recommendations from High-Quality CPGs
2.3. Phase 3: Finalization
3. Results
3.1. Phase 1: Setup
3.2. Phase 2: Adaptation
Search and Screen Module
3.3. Quality Assessment Module
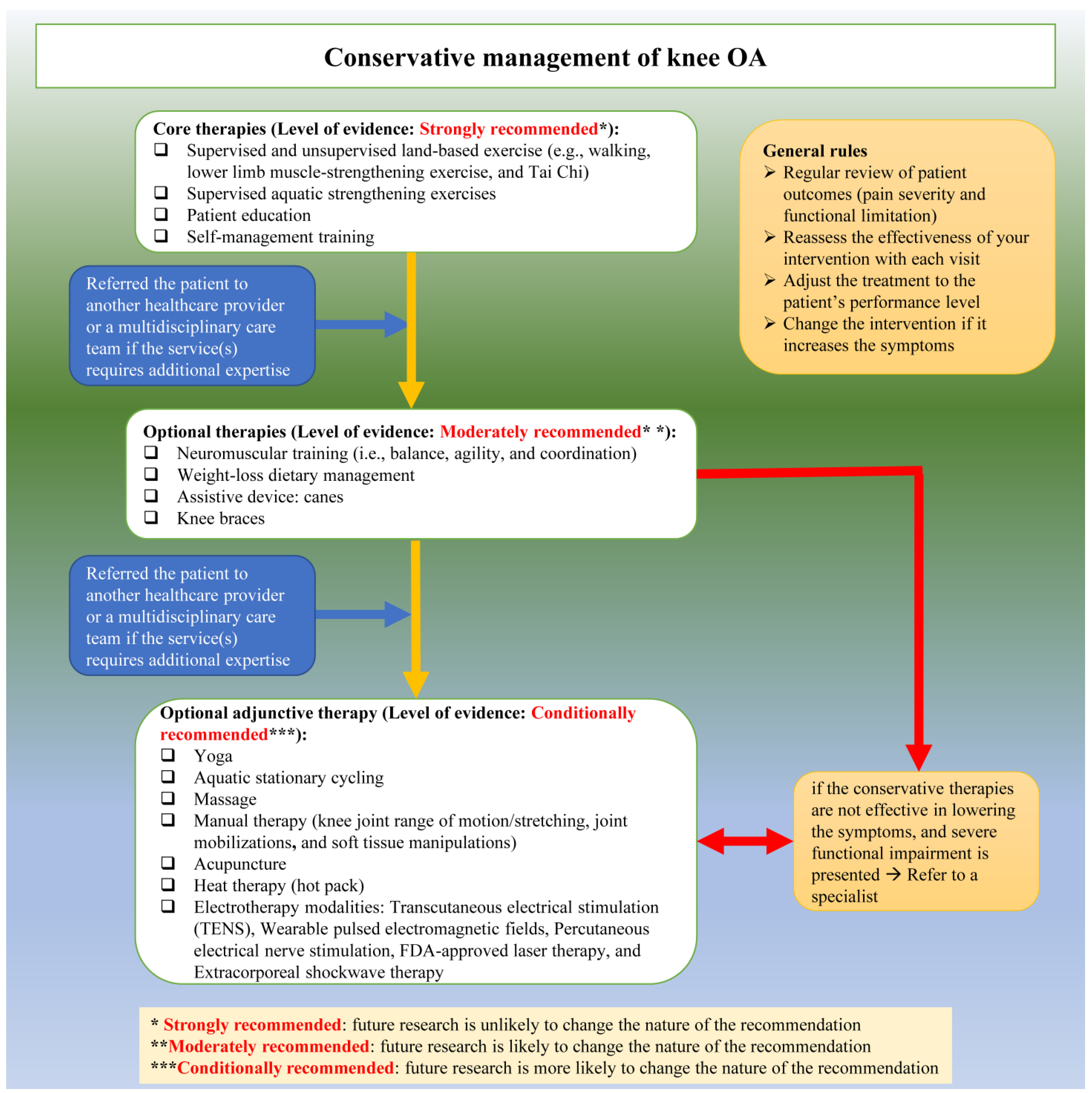
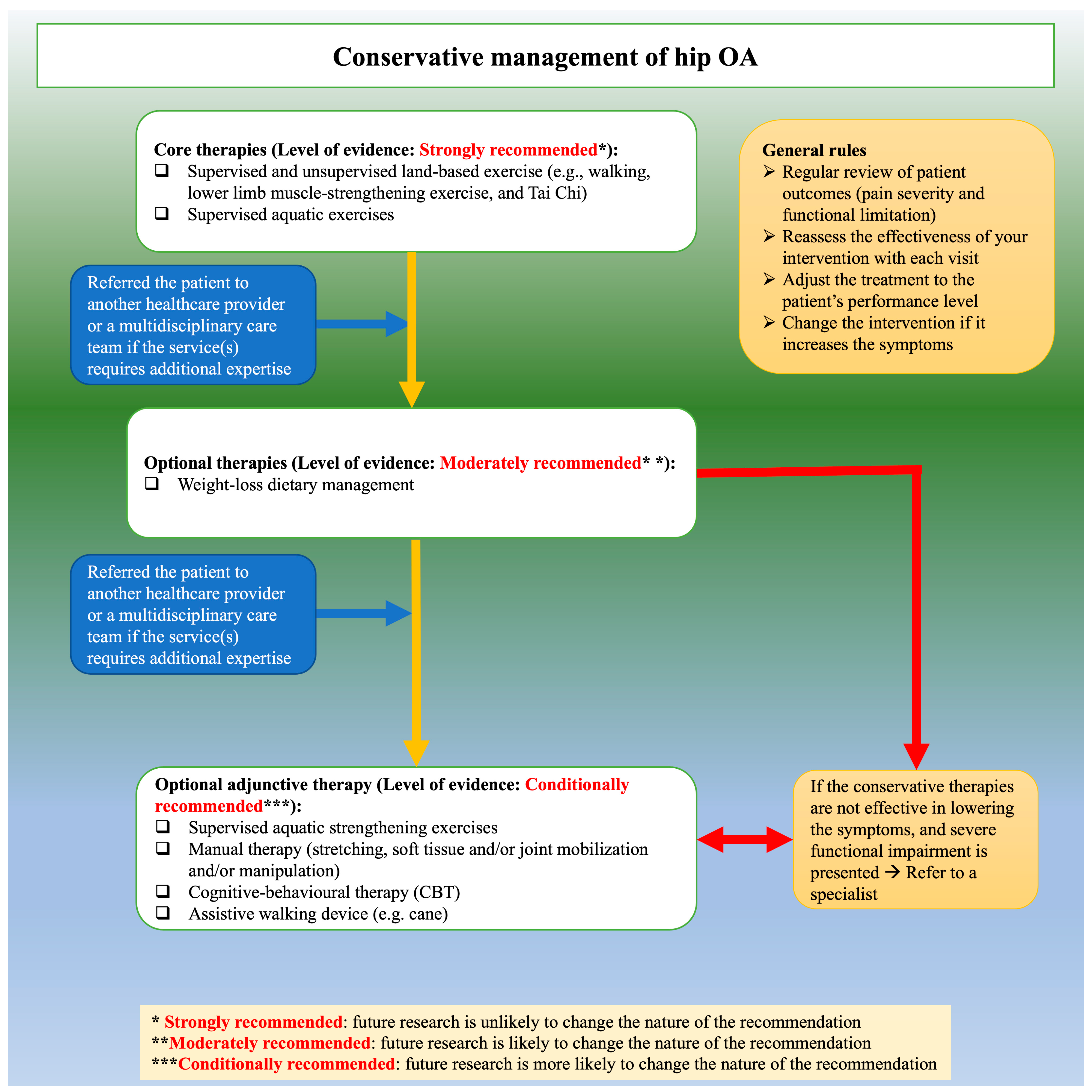
3.4. Phase 3: Finalization
3.5. Plan for Updating the Guideline
4. Discussion
4.1. Similarities and Differences with Recommendations from the Original CPGs
4.2. Stakeholder Considerations
4.3. Cultural and Clinical Context
4.4. Dissemination and Implementation Plan
4.5. Future Research
4.6. Strengths and Weaknesses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| HK | Hong Kong |
| CPG | Clinical Practice Guidelines |
| AGREE | Appraisal of Guidelines for Research and Evaluation |
| PIPOH | Population, Interventions, Professionals, Outcomes, Healthcare settings |
| AAOS | American Academy of Orthopaedic Surgeons |
| TLAR | Turkish League Against Rheumatism |
| APTA | American Physical Therapy Association |
| KNGF | Royal Dutch Society for Physical Therapy |
| OARSI | Osteoarthritis Research Society International |
| ACR | American College of Rheumatology |
| EULAR | European alliance of associations for rheumatology |
| PANLAR | Pan-American League of Associations for Rheumatology |
| RACGP | Royal Australian College of General Practitioners |
References
- GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.-A.; Smith, E.; Hill, C.; Bettampadi, D.; Mansournia, M.A.; Hoy, D.; Ashrafi-Asgarabad, A.; Sepidarkish, M.; Almasi-Hashiani, A.; et al. Global, regional and national burden of osteoarthritis 1990–2017: A systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 819–828. [Google Scholar] [CrossRef]
- Schram, B.; Orr, R.; Pope, R.; Canetti, E.; Knapik, J. Risk factors for development of lower limb osteoarthritis in physically demanding occupations: A narrative umbrella review. J. Occup. Health 2019, 62, e12103. [Google Scholar] [CrossRef] [PubMed]
- The Chinese University of Hong Kong. Osteoarthritis in Hong Kong Chinese—Prevalence, Aetiology and Prevention. 2001. Available online: http://www.cuhk.edu.hk/ipro/010306e.htm (accessed on 21 October 2021).
- Woo, J.; Lau, E.; Lau, C.S.; Lee, P.; Zhang, J.; Kwok, T.; Chan, C.; Chiu, P.; Chan, K.M.; Chan, A.; et al. Socioeconomic impact of osteoarthritis in Hong Kong: Utilization of health and social services, and direct and indirect costs. Arthritis Rheum. 2003, 49, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.C.; Cooper, C.; Lam, D.; Chan, V.N.H.; Tsang, K.K.; Sham, A. Factors associated with osteoarthritis of the hip and knee in Hong Kong Chinese: Obesity, joint injury, and occupational activities. Am. J. Epidemiol. 2000, 152, 855–862. [Google Scholar] [CrossRef]
- Kumta, S.M.; Lau, E. Risk factors for primary osteoarthritis of the hip and knee in the Hong Kong Chinese population. Hong Kong Med. J. 2007, 13, S9–S14. [Google Scholar]
- Yuen, W.H. Osteoarthritis of knees: The disease burden in Hong Kong and means to alleviate it. Hong Kong Med. J. 2014, 20, 5–6. [Google Scholar] [CrossRef]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- World Confederation for Physical Therapy. Policy Statement: Evidence-Based Practice. 2019. Available online: https://world.physio/policy/ps-ebp (accessed on 30 October 2023).
- Woolf, S.H.; Grol, R.; Hutchinson, A.; Eccles, M.; Grimshaw, J. Clinical guidelines: Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999, 318, 527–530. [Google Scholar] [CrossRef]
- Department of Community and Family Medicine. Clinical Guidelines for Managing Lower-Limb Osteoarthritis in Hong Kong Primary Care Setting; Department of Community and Family Medicine, Chinese University of Hong Kong: Hong Kong, China, 2004. [Google Scholar]
- Zhang, Z.; Huang, C.; Jiang, Q.; Zheng, Y.; Liu, Y.; Liu, S.; Chen, Y.; Mei, Y.; Ding, C.; Chen, M.; et al. Guidelines for the diagnosis and treatment of osteoarthritis in China (2019 edition). Ann. Transl. Med. 2020, 8, 1213. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Fretheim, A.; Oxman, A.D. Improving the use of research evidence in guideline development: 13. Applicability, transferability and adaptation. Health Res. Policy Syst. 2006, 4, 25. [Google Scholar] [CrossRef]
- Fervers, B.; Burgers, J.S.; Voellinger, R.; Brouwers, M.; Browman, G.P.; Graham, I.D.; Harrison, M.B.; Latreille, J.; Mlika-Cabane, N.; Paquet, L.; et al. Guideline adaptation: An approach to enhance efficiency in guideline development and improve utilisation. BMJ Qual. Saf. 2011, 20, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Norris, S.L.; Bero, L. The advantages and limitations of guideline adaptation frameworks. Implement. Sci. 2018, 13, 72. [Google Scholar] [CrossRef]
- Chakraborty, S.P.; Jones, K.M.; Mazza, D. Adapting lung cancer symptom investigation and referral guidelines for general practitioners in Australia: Reflections on the utility of the ADAPTE framework. J. Eval. Clin. Pract. 2014, 20, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Harstall, C.; Taenzer, P.; Zuck, N.; Angus, D.K.; Moga, C.; Scott, N.A. Adapting low back pain guidelines within a multidisciplinary context: A process evaluation. J. Eval. Clin. Pract. 2013, 19, 773–781. [Google Scholar] [CrossRef] [PubMed]
- González-Lamuño, D.; Rodríguez, A.L.; Yanes, M.I.L.; Barrio, S.M.-D.; Díaz-Guerra, G.M.; Peris, P. Clinical practice recommendations for the diagnosis and treatment of X-linked hypophosphatemia: A consensus based on the ADAPTE method. Med. Clin. 2021, 159, 152.e1–152.e12. [Google Scholar] [CrossRef]
- Hoedl, M.; Schoberer, D.; Halfens, R.J.G.; Lohrmann, C. Adaptation of evidence-based guideline recommendations to address urinary incontinence in nursing home residents according to the ADAPTE-process. J. Clin. Nurs. 2018, 27, 2974–2983. [Google Scholar] [CrossRef]
- Hurtado, M.M.; Quemada, C.; García-Herrera, J.M.; Morales-Asencio, J.M. Use of the ADAPTE method to develop a clinical guideline for the improvement of psychoses and schizophrenia care: Example of involvement and participation of patients and family caregivers. Health Expect. 2021, 24, 516–524. [Google Scholar] [CrossRef]
- Lovell, M.; Luckett, T.; Boyle, F.; Stubbs, J.; Phillips, J.; Davidson, P.M.; Olver, I.; von Dincklage, J.; Agar, M. Adaptation of international guidelines on assessment and management of cancer pain for the Australian context. Asia Pac. J. Clin. Oncol. 2015, 11, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Pringsheim, T.; Addington, D. Canadian Schizophrenia Guidelines: Introduction and Guideline Development Process. Can. J. Psychiatry 2017, 62, 586–593. [Google Scholar] [CrossRef]
- Roberge, P.; Fournier, L.; Brouillet, H.; Delorme, A.; Beaucage, C.; Côté, R.; Demers, P.; Gervais, M.; Laflamme, F.; Latulippe, L.; et al. A provincial adaptation of clinical practice guidelines for depression in primary care: A case illustration of the ADAPTE method. J. Eval. Clin. Pract. 2015, 21, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Selby, P.; Hunter, K.; Rogers, J.; Lang-Robertson, K.; Soklaridis, S.; Chow, V.; Tremblay, M.; Koubanioudakis, D.; Dragonetti, R.; Hussain, S.; et al. How to adapt existing evidence-based clinical practice guidelines: A case example with smoking cessation guidelines in Canada. BMJ Open 2017, 7, e016124. [Google Scholar] [CrossRef]
- Mack, S.; Hahn, S.; Palli, C.; Findling, T.; Lohrmann, C. Adaptation of Clinical Practice Guideline Recommendations in Hospitals for People Living With Dementia and Their Caregivers. Worldviews Evid. Based Nurs. 2019, 16, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ayhan Baser, D.; Kahveci, R.; Baydar Artantas, A.; Yasar, İ.; Aksoy, H.; Koc, E.M.; Kasim, İ.; Kunnamo, I.; Özkara, A. Exploring guideline adaptation strategy for Turkey: Is “ADAPTE” feasible or does it need adaptation as well? J. Eval. Clin. Pract. 2018, 24, 97–104. [Google Scholar] [CrossRef]
- Amer, Y.S.; Elzalabany, M.M.; Omar, T.I.; Ibrahim, A.G.; Dowidar, N.L. The ‘Adapted ADAPTE’: An approach to improve utilization of the ADAPTE guideline adaptation resource toolkit in the Alexandria Center for Evidence-Based Clinical Practice Guidelines. J. Eval. Clin. Pract. 2015, 21, 1095–1106. [Google Scholar] [CrossRef]
- Amer, Y.S.; Wahabi, H.A.; Elkheir, M.M.A.; Bawazeer, G.A.; Iqbal, S.M.; Titi, M.A.; Ekhzaimy, A.; Alswat, K.A.; Alzeidan, R.A.; Al-Ansary, L.A. Adapting evidence-based clinical practice guidelines at university teaching hospitals: A model for the Eastern Mediterranean Region. J. Eval. Clin. Pract. 2019, 25, 550–560. [Google Scholar] [CrossRef]
- Bashiri, F.A.; Albatti, T.H.; Hamad, M.H.; Al-Joudi, H.F.; Daghash, H.F.; Al-Salehi, S.M.; Varnham, J.L.; Alhaidar, F.; Almodayfer, O.; Alhossein, A.; et al. Adapting evidence-based clinical practice guidelines for people with attention deficit hyperactivity disorder in Saudi Arabia: Process and outputs of a national initiative. Child Adolesc. Psychiatry Ment. Health 2021, 15, 6. [Google Scholar] [CrossRef]
- Irajpour, A.; Hashemi, M.; Taleghani, F. Clinical practice guideline for end-of-life care in patients with cancer: A modified ADAPTE process. Support. Care Cancer 2022, 30, 2497–2505. [Google Scholar] [CrossRef]
- Hu, J.; Yu, L.; Jiang, L.; Yuan, W.; Bian, W.; Yang, Y.; Ruan, H. Developing a Guideline for Endotracheal Suctioning of Adults With Artificial Airways in the Perianesthesia Setting in China. J. PeriAnesthesia Nurs. 2019, 34, 160–168.e4. [Google Scholar] [CrossRef] [PubMed]
- The ADAPTE Collaboration. The ADAPTE Process: Resource Toolkit for Guideline Adaptation. Version 2.0: Guideline International Network. 2009. Available online: http://www.g-i-n.net (accessed on 26 June 2021).
- Bichsel, D.; Liechti, F.D.; Schlapbach, J.M.; Wertli, M.M. Cross-sectional analysis of recommendations for the treatment of hip and knee osteoarthritis in clinical guidelines. Arch. Phys. Med. Rehabil. 2021, 103, 559–569. [Google Scholar] [CrossRef]
- Feuerstein, J.D.; Pelsis, J.R.; Lloyd, S.; Cheifetz, A.S.; Stone, K.R. Systematic analysis of the quality of the scientific evidence and conflicts of interest in osteoarthritis of the hip and knee practice guidelines. Semin. Arthritis Rheum. 2016, 45, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Bierma-Zeinstra, S.; van Middelkoop, M.; Runhaar, J.; Schiphof, D. Nonpharmacological and nonsurgical approaches in OA. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101564. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Hanna, S.E.; Makarski, J.; et al. Development of the AGREE II, part 2: Assessment of validity of items and tools to support application. Can. Med. Assoc. J. 2010, 182, E472–E478. [Google Scholar] [CrossRef] [PubMed]
- AGREE Next Steps Consortium. The AGREE II Instrument [Electronic Version]. 2017. Available online: http://www.agreetrust.org (accessed on 3 July 2021).
- Tuncer, T.; Cay, F.H.; Altan, L.; Gurer, G.; Kacar, C.; Ozcakir, S.; Atik, S.; Ayhan, F.; Durmaz, B.; Eskiyurt, N.; et al. 2017 update of the Turkish League Against Rheumatism (TLAR) evidence-based recommendations for the management of knee osteoarthritis. Rheumatol. Int. 2018, 38, 1315–1331. [Google Scholar] [CrossRef]
- Osthoff, A.-K.R.; Niedermann, K.; Braun, J.; Adams, J.; Brodin, N.; Dagfinrud, H.; Duruoz, T.; Esbensen, B.A.; Günther, K.-P.; Hurkmans, E.; et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann. Rheum. Dis. 2018, 77, 1251–1260. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part one: Introduction, and mind-body exercise programs. Clin. Rehabil. 2017, 31, 582–595. [Google Scholar] [CrossRef]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part three: Aerobic exercise programs. Clin. Rehabil. 2017, 31, 612–624. [Google Scholar] [CrossRef]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: Strengthening exercise programs. Clin. Rehabil. 2017, 31, 596–611. [Google Scholar] [CrossRef]
- Brosseau, L.; Wells, G.A.; Pugh, A.G.; Smith, C.A.; Rahman, P.; Gallardo, I.C.Á.; Toupin-April, K.; Loew, L.; De Angelis, G.; Cavallo, S.; et al. Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercise in the management of hip osteoarthritis. Clin. Rehabil. 2016, 30, 935–946. [Google Scholar] [CrossRef]
- Rillo, O.; Riera, H.; Acosta, C.; Liendo, V.; Bolaños, J.; Monterola, L.; Nieto, E.; Arape, R.; Franco, L.M.; Vera, M.; et al. PANLAR Consensus Recommendations for the Management in Osteoarthritis of Hand, Hip, and Knee. Am. J. Clin. Oncol. 2016, 22, 345–354. [Google Scholar] [CrossRef]
- van Doormaal, M.C.; Meerhoff, G.A.; Vlieland, T.P.V.; Peter, W.F. A clinical practice guideline for physical therapy in patients with hip or knee osteoarthritis. Musculoskelet. Care 2020, 18, 575–595. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.; Bennell, K.; Austin, M.; Briggs, A.; Buchbinder, R.; Bunker, S.; Choong, P.; Ewald, D.; Fallon, K.; Harris, B.; et al. Guideline for the Management of Knee and Hip Osteoarthritis, 2nd ed.; with Consumer Summary; Royal Australian College of General Practitioners: Melbourne, Australia, 2018. Available online: https://www.racgp.org.au/getattachment/71ab5b77-afdf-4b01-90c3-04f61a910be6/Guideline-for-the-management-of-knee-and-hip-osteoarthritis.aspx (accessed on 3 January 2022).
- Cibulka, M.T.; Bloom, N.J.; Enseki, K.R.; Macdonald, C.W.; Woehrle, J.; McDonough, C.M. Hip Pain and Mobility Deficits—Hip Osteoarthritis: Revision 2017. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A37. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Hip Evidence-Based Clinical Practice Guideline; American Academy of Orthopaedic Surgeons: Rosemount, IL, USA, 2017; Available online: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-hip/oa-hip-cpg_6-11-19.pdf (accessed on 16 January 2022).
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Knee (Non-Arthroplasty) Evidence-Based Clinical Practice Guideline; American Academy of Orthopaedic Surgeons: Rosemount, IL, USA, 2021; Available online: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-knee/oak3cpg.pdf (accessed on 23 January 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Tittlemier, B.J.; Wittmeier, K.D.; Webber, S.C. Quality and content analysis of clinical practice guidelines which include nonpharmacological interventions for knee osteoarthritis. J. Eval. Clin. Pract. 2021, 27, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Ahamed, Y.; Jull, G.; Bryant, C.; Hunt, M.A.; Forbes, A.B.; Kasza, J.; Akram, M.; Metcalf, B.; Harris, A.; et al. Physical Therapist–Delivered Pain Coping Skills Training and Exercise for Knee Osteoarthritis: Randomized Controlled Trial. Arthritis Care Res. 2016, 68, 590–602. [Google Scholar] [CrossRef]
- Saffari, M.; Meybodi, M.K.E.; Sanaeinasab, H.; Karami, A.; Pakpour, A.H.; Koenig, H.G. A theory of planned behavior-based intervention to improve quality of life in patients with knee/hip osteoarthritis: A randomized controlled trial. Clin. Rheumatol. 2018, 37, 2505–2515. [Google Scholar] [CrossRef]
- Marconcin, P.; Espanha, M.; Teles, J.; Bento, P.; Campos, P.; André, R.; Yázigi, F. A randomized controlled trial of a combined self-management and exercise intervention for elderly people with osteoarthritis of the knee: The PLE2NO program. Clin. Rehabil. 2018, 32, 223–232. [Google Scholar] [CrossRef]
- Coleman, S.; Briffa, N.K.; Carroll, G.; Inderjeeth, C.; Cook, N.; McQuade, J. A randomised controlled trial of a self-management education program for osteoarthritis of the knee delivered by health care professionals. Arthritis Res. Ther. 2012, 14, R21. [Google Scholar] [CrossRef]
- Lim, Y.; Wong, J.; Hussain, S.M.; Estee, M.; Zolio, L.; Page, M.; Harrison, C.; Wluka, A.; Wang, Y.; Cicuttini, F. AB0979 Recommendations for weight management in osteoarthritis: A systematic review of clinical practice guidelines. Rheumatology 2022, 81 (Suppl. S1), 1616. [Google Scholar] [CrossRef]
- Hopayian, K.; Notley, C. A systematic review of low back pain and sciatica patients’ expectations and experiences of health care. Spine J. 2014, 14, 1769–1780. [Google Scholar] [CrossRef] [PubMed]
- Wong, V. Cultural influence on psychoeducation in Hong Kong. Int. Psychiatry 2010, 7, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Schoeb, V. Healthcare Service in Hong Kong and its Challenges: The Role of Health Professionals within a Social Model of Health. China Perspect. 2016, 4, 51–58. [Google Scholar] [CrossRef]
- Chung, V.; Wong, E.; Woo, J.; Vi Lo, S.; Griffiths, S. Use of Traditional Chinese Medicine in the Hong Kong Special Administrative Region of China. J. Altern. Complement. Med. 2007, 13, 361–368. [Google Scholar] [CrossRef]
- Tsang, V.H.M.; Lo, P.H.W.; Lam, F.T.; Chung, L.S.W.; Tang, T.Y.; Lui, H.M.; Lau, J.T.G.; Yee, H.F.; Lun, Y.K.; Chan, H.T.; et al. Perception and use of complementary and alternative medicine for low back pain. J. Orthop. Surg. 2017, 25, 2309499017739480. [Google Scholar] [CrossRef] [PubMed]
- Fan, R. Which Care? Whose Responsibility? And Why Family? A Confucian Account of Long-Term Care for the Elderly. J. Med. Philos. A Forum Bioeth. Philos. Med. 2007, 32, 495–517. [Google Scholar] [CrossRef]
- Cycyk, L.M.; De Anda, S.; Moore, H.; Huerta, L. Cultural and Linguistic Adaptations of Early Language Interventions: Recommendations for Advancing Research and Practice. Am. J. Speech Lang. Pathol. 2021, 30, 1224–1246. [Google Scholar] [CrossRef]
- Ma, J.K.; Floegel, T.A.; Li, L.C.; Leese, J.; De Vera, M.A.; Beauchamp, M.R.; Taunton, J.; Liu-Ambrose, T.; Allen, K.D. Tailored physical activity behavior change interventions: Challenges and opportunities. Transl. Behav. Med. 2021, 11, 2174–2181. [Google Scholar] [CrossRef]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.-L.; Pomey, M.-P. Engaging patients to improve quality of care: A systematic review. Implement. Sci. 2018, 13, 98. [Google Scholar] [CrossRef]
- Hong Kong Physiotherapy Association. World Confederation for Physical Therapy. Available online: https://world.physio/membership/hong-kong (accessed on 24 October 2023).
- Hong Kong Physiotherapy Association. “Direct Access for Physiotherapy “The Blueprint” in Primary Healthcare”. 29 December 2022. Available online: https://www.hongkongpa.com.hk/notices/direct-access-for-physiotherapy-the-blueprint-in-primary-healthcare/ (accessed on 24 October 2023).
- South China Morning Post. “Staff Shortages in Hong Kong Threaten Quality of Care for Elderly”. 15 July 2015. Available online: www.scmp.com/news/hong-kong/health-environment/article/1839255/staff-shortages-hong-kong-threaten-quality-care (accessed on 24 October 2023).
- US Department of Health & Human Services, Agency for Healthcare Research and Quality. In “National Healthcare Disparities Report 2008”, Washington, 2008, Access to Healthcare; AHRQ Publication: Rockville, MD, USA, 2008; Chapter 3, No. 09-0002. Available online: https://archive.ahrq.gov/research/findings/nhqrdr/nhdr08/Chap3.html (accessed on 24 October 2023).
- Zadro, J.; O’keeffe, M.; Maher, C. Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open 2019, 9, e032329. [Google Scholar] [CrossRef]
- Zadro, J.R.; Ferreira, G. Has physical therapists’ management of musculoskeletal conditions improved over time? Braz. J. Phys. Ther. 2020, 24, 458–462. [Google Scholar] [CrossRef]
- Paci, M.; Faedda, G.; Ugolini, A.; Pellicciari, L. Barriers to evidence-based practice implementation in physiotherapy: A system-atic review and meta-analysis. Int. J. Qual. Health Care 2021, 33, mzab093. [Google Scholar] [CrossRef] [PubMed]
- Straus, S.E.; Sackett, D.L. Using research findings in clinical practice. BMJ 1998, 317, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, A.R.; Marshall, C.; Huckson, S.; James, R.; Moore, V. Developing a checklist for guideline implementation planning: Review and synthesis of guideline development and implementation advice. Implement. Sci. 2015, 10, 19. [Google Scholar] [CrossRef] [PubMed]
- Al Zoubi, F.; Wong, Y.L.; Cheing, G.; Cheung, J.P.Y.; Fu, S.N.; Tsang, H.; Law KY, R.; So, C.L.; Tsang, R.; Tsang, M.H.; et al. Management of hip and knee osteoarthritis: An adapted clinical practice guideline for Hong Kong physiotherapists. In Proceedings of the World Physiotherapy Asia Western Pacific Regional Congress, Hong Kong, China, 18–20 June 2022. [Google Scholar]
- Darzi, A.; Abou-Jaoude, E.A.; Agarwal, A.; Lakis, C.; Wiercioch, W.; Santesso, N.; Brax, H.; El-Jardali, F.; Schünemann, H.J.; Akl, E.A. A methodological survey identified eight proposed frameworks for the adaptation of health related guidelines. J. Clin. Epidemiol. 2017, 86, 3–10. [Google Scholar] [CrossRef]
- Kimaro, H.C. Strategies for Developing Human Resource Capacity to Support Sustainability of ICT Based Health Information Systems: A Case Study from Tanzania. Electron. J. Inf. Syst. Dev. Ctries. 2006, 26, 1–23. [Google Scholar] [CrossRef]
- Dizon, J.M.; Machingaidze, S.; Grimmer, K. To adopt, to adapt, or to contextualise? The big question in clinical practice guide-line development. BMC Res. Notes 2016, 9, 442. [Google Scholar] [CrossRef]
- Alper, B.S.; Tristan, M.; Ramirez-Morera, A.; Vreugdenhil, M.M.; Van Zuuren, E.J.; Fedorowicz, Z. RAPADAPTE for rapid guideline development: High-quality clinical guidelines can be rapidly developed with limited resources. Int. J. Qual. Health Care 2016, 28, 268–274. [Google Scholar] [CrossRef]
- Florez, I.D.; Brouwers, M.C.; Kerkvliet, K.; Spithoff, K.; Alonso-Coello, P.; Burgers, J.; Cluzeau, F.; Férvers, B.; Graham, I.; Grimshaw, J.; et al. Assessment of the quality of recom-mendations from 161 clinical practice guidelines using the Appraisal of Guidelines for Research and Evaluation–Recommendations Excellence (AGREE-REX) instrument shows there is room for improvement. Implement. Sci. 2020, 15, 79. [Google Scholar] [CrossRef] [PubMed]
| # | Name of the Database | Country | Website |
|---|---|---|---|
| Medical databases | |||
| i | MEDLINE (PubMed) | USA | https://www.nlm.nih.gov/medline/medline_overview.html, accessed on 23 March 2021. |
| ii | CINAHL Complete (EbscoHost) | USA | https://www.ebsco.com/products/research-databases/cinahl-database, accessed on 23 March 2021 |
| iii | EMBASE | The Netherlands | https://www.embase.com/, accessed on 23 March 2021 |
| iv | Epistemonikos | Chile | https://www.epistemonikos.org/, accessed on 23 March 2021 |
| v | Scopus | International | https://www.scopus.com/home.uri, accessed on 23 March 2021 |
| vi | PEDro | Australia | https://pedro.org.au/, accessed on 23 March 2021 |
| Guideline Clearinghouse | |||
| i | Guidelines International Network (G-I-N) | International | http://www.g-i-n.net, accessed on 23 March 2021 |
| ii | Guideline Central | International | https://www.guidelinecentral.com/, accessed on 23 March 2021 |
| iii | National Institute for Health and Care Excellence (NICE) | UK | http://www.nice.org.uk/guidance/, accessed on 23 March 2021 |
| iv | National Health and Medical Research Council (NHMRC) | Australia | http://www.nhmrc.gov.au/guidelines-publications, accessed on 23 March 2021 |
| v | New Zealand Guidelines Group | New Zealand | https://www.health.govt.nz/, accessed on 23 March 2021 |
| vi | World Health Organization (WHO) | International | https://www.who.int/publications/who-guidelines, accessed on 23 March 2021 |
| vii | Scottish Intercollegiate Guidelines Network (SIGN) | UK | http://www.sign.ac.uk/guidelines/index.html, accessed on 23 March 2021 |
| viii | Institute for Clinical Systems Improvement (ICSI) | USA | https://www.icsi.org/guidelines/, accessed on 23 March 2021 |
| Developer | Location | Publication Date | End of Search Date | Type/Location of Arthritis |
|---|---|---|---|---|
| AAOS-Knee | USA | 2021 | 28 April 2020 | KOA |
| Dutch-KNGF | Netherlands | 2020 | December 2016–August 2017 | KOA + HOA |
| OARSI | International | 2019 | July 2018 | KOA + HOA + hand OA |
| ACR | USA | 2019 | August 2018 | KOA + HOA + hand OA |
| Australian-RACGP | Australia | 2018 | December 2016 | KOA + HOA |
| EULAR | Europe | 2018 | April 2017 | KOA + HOA, RA, spondylarthritis |
| Turkish | Turkey | 2018 | Jane 2015 | KOA |
| APTA | USA | 2017 | 2016 | HOA |
| OTTAWA Knee | Canada | 2017 | May 2016 | KOA |
| AAOS-Hip | USA | 2017 | March–April 2016 | HOA |
| PANLAR | South America | 2016 | 2014 | KOA + HOA + hand OA |
| OTTAWA Hip | Canada | 2016 | May 2015 | HOA |
| Guideline | Domain 1. Scope and Purpose | Domain 2. Stakeholder Involvement | Domain 3. Rigor of Devlopment | Domain 4. Clarity of Presentation | Domain 5. Applicability | Domain 6. Editorial Independence | Overall Quality Score |
|---|---|---|---|---|---|---|---|
| KNGF | 97% | 94% | 76% | 97% | 44% | 50% | 76% |
| RACGP | 100% | 61% | 86% | 89% | 23% | 42% | 67% |
| AAOS-Knee | 94% | 64% | 90% | 92% | 17% | 46% | 67% |
| OARSI | 81% | 78% | 60% | 81% | 4% | 92% | 66% |
| APTA | 69% | 67% | 65% | 100% | 27% | 58% | 64% |
| ACR | 89% | 86% | 68% | 83% | 4% | 25% | 59% |
| OTTAWA-Knee | 75% | 67% | 49% | 83% | 4% | 33% | 52% |
| EULAR | 86% | 83% | 50% | 81% | 25% | 25% | 58% |
| TLAR | 56% | 33% | 46% | 78% | 0% | 17% | 38% |
| PANLAR | 39% | 47% | 21% | 78% | 2% | 17% | 34% |
| Guideline | Domain 1. Scope and Purpose | Domain 2. Stakeholder Involvement | Domain 3. Rigor of Devlopment | Domain 4. Clarity of Presentation | Domain 5. Applicability | Domain 6. Editorial Independence | Overall Quality Score |
|---|---|---|---|---|---|---|---|
| KNGF | 97% | 94% | 76% | 97% | 44% | 50% | 76% |
| RACGP | 100% | 61% | 86% | 89% | 23% | 42% | 67% |
| AAOS-Hip | 83% | 75% | 92% | 72% | 50% | 75% | 75% |
| OARSI | 81% | 78% | 60% | 81% | 4% | 92% | 66% |
| APTA | 69% | 67% | 65% | 100% | 27% | 58% | 64% |
| ACR | 89% | 86% | 68% | 83% | 4% | 25% | 59% |
| OTTAWA-Hip | 81% | 47% | 55% | 78% | 4% | 29% | 49% |
| EULAR | 86% | 83% | 50% | 81% | 25% | 25% | 58% |
| PANLAR | 39% | 47% | 21% | 78% | 2% | 17% | 34% |
| *** | We strongly recommend supervised and unsupervised land-based exercise (e.g., walking, muscle-strengthening exercise, and Tai Chi) and/or aquatic exercises to improve pain and function among patients with knee OA. Remarks: All types of exercise were found to be significantly better than no exercise. However, the results were too mixed to determine which exercise program was superior. The exercise program should last for at least 6 weeks, and physiotherapists can use the frequency, intensity, time, and type (FITT) principle to prescribe exercises for individual patients. |
| *** | We strongly recommend supervised aquatic strengthening exercises to improve pain and function for patients with knee OA. Remarks: The recommended program consists of 30 min of supervised aquatic strengthening exercises, preceded by a 5-min warm-up and followed by a 5-min cool-down, twice a week for 6 weeks. |
| *** | We strongly recommend providing patient education to patients with knee OA as a means to reduce pain and improve function. Remarks: Patient education can be delivered through various modes, such as an educational pamphlet, a video, and one to several days of education per month. The content of the education could involve various forms of exercise, proven effective interventions, and self-management techniques for knee OA, including pain management, medication compliance, and stress management. |
| *** | We strongly recommend self-management training to improve pain and function for patients with knee OA in both the short and long term. Remarks: Self-management training should cover pain coping skills training, exercises, and behavioral weight management and should be provided to patients once a week for at least 6 weeks, with each session lasting at least 60 min. |
| ** | We moderately recommend providing neuromuscular training programs that include balance, agility, and coordination exercises, in addition to traditional exercises, to improve functions such as walking speed and balance for patients with knee OA. Remarks: Kinaesthesia and balance exercises (e.g., retro-walking, walking on toes, leaning to the sides, balance-board exercises, mini-trampoline exercises, plyometric exercises, etc.) combined with traditional strengthening exercises should be conducted three times a week for 8 weeks. |
| ** | We moderately recommend weight-loss dietary management combined with exercises to reduce pain and improve function for overweight and obese patients with knee OA. Remarks: Physiotherapists should encourage overweight (BMI ≥ 25 kg/m2) or obese (BMI ≥ 30 kg/m2) patients with knee OA to follow a weight-loss program to lose at least 5% of their body weight. The dietary program should be combined with exercise. |
| ** | We moderately recommend using canes to reduce pain and improve function for patients with knee OA, if indicated. Remarks: Wooden canes with a T-shaped handle can be used for patients with knee OA. |
| ** | We moderately recommend Knee braces can be used to reduce pain, improve function, and enhance the quality of life for patients with knee OA. Remarks: The Bioskin Patellar Tracking Q Brace (worn for as long as tolerated per day for 6 weeks) or the REBEL RELIEVER unloading knee brace (worn for at least 6 h/day for 6 weeks) can be used for patients with knee OA. |
| * | We conditionally recommend yoga to reduce pain and improve mobility in patients with knee OA. Remarks: Supervised yoga can be prescribed for 40 min per day over a period of 2 weeks. After the supervised sessions, patients should be advised to continue with 40-min yoga sessions at home for the next 10 weeks. The yoga program could include shithilikarana vyayamas or sakti vikasaka, followed by yoga asanas and relaxation techniques. |
| * | We conditionally recommend aquatic stationary cycling to improve function for some patients with knee OA. Remarks: Supervised (for a maximum of 4 patients), aquatic cycling should last for 45 min twice a week for 12 weeks. |
| * | We conditionally recommend massage therapy combined with usual care to reduce pain and improve function for patients with knee OA. Remarks: A 60-min total body massage could be offered once a week for 8 weeks, or effleurage and petrissage techniques could be applied to the knee joint in the direction of lymph drainage for 15–20 min, twice a week for 3 weeks. |
| * | We conditionally recommend manual therapy in combination with a standardized knee exercise program to reduce pain and improve function for patients with knee OA. This should be considered only as an adjunctive treatment to enable engagement with active management. Remarks: Manual therapy may include knee accessory joint mobilizations, knee joint range of motion/stretching, and soft tissue manipulations of the quadriceps, rectus femoris, hamstring, and gastrocnemius muscles twice a week for a period of 4 weeks as an adjunctive treatment. |
| * | Transcutaneous electrical stimulation might be used as an adjunctive treatment to reduce pain and improve function in patients with knee OA. Remarks: Patients can use the device as much as needed using four electrodes around the knee joint line (two medially and two laterally) in continuous mode (program A: 110 Hz, 50 μs). All electrical pulses should be asymmetric and biphasic for 30 min, up to 6 weeks. |
| * | We conditionally recommend using a wearable pulsed electromagnetic field device to reduce pain and improve function for patients with knee OA. Remarks: A wearable pulsed radiofrequency energy device (ActiPatch) can be used as adjunctive therapy. We suggest the following parameters for 12 h/day for 4 weeks: carrier frequency at 27.12 MHz; 1000 Hz pulse rate; 100 μs burst width; and peak burst output power ∼0.0098 W/surface area of ∼103 cm2. |
| * | We conditionally recommend percutaneous electrical nerve stimulation to reduce pain and improve function for patients with chronic knee OA. Remarks: Percutaneous electrical nerve stimulation could be used as an adjunctive therapy. We suggest using the following parameters for 20 min/day, three times/day for 8 weeks: 2–6 Hz for frequency and 150 ms for pulses. |
| * | We conditionally recommend FDA-approved laser therapy to reduce pain and improve function for patients with knee OA. Remarks: Laser therapy can be used as an adjunctive therapy. We suggest either using (a) a 5-min stimulation time, 200-nanosecond maximum pulse duration, 2.5 kHz pulse frequency, 20 W maximum output/pulse, 10 mW average power, 1 cm2 surface, 3 J total energy, and 30 J accumulated dose, five times a week for 2 weeks; or (b) a Neodymium:Yttrium–Aluminum–Garnet (Nd:YAG) high-intensity laser therapy with 1064 nm wavelength on the medial and lateral sides of the knee joint line for 8 min, at a frequency of 30 Hz with a peak power of 5 W, a duty cycle of 70%, energy density of 60 J/cm2, and total energy of 2400 J/session, three times a week for 4 weeks. |
| * | We conditionally recommend extracorporeal shockwave therapy to reduce pain and improve function in patients with knee OA. Remarks: Extracorporeal shockwave therapy could be used as an adjunctive therapy. The parameters of therapy may include (a) 2000 pulses of 8-Hz frequency at 2.5 bars of pneumatic pressure, once a week for 4 weeks; (b) 4000 pulses at 0.25 mJ/mm2 and a frequency of 6 Hz/s, once a week for 12 weeks; or (c) 2500 pulses at a pressure of 3 bars and a frequency of 12 Hz, twice a week for 5 weeks. |
| * | We conditionally recommend acupuncture to improve pain and function. Remarks: Acupuncture can be accompanied by an electro-stimulator for an average of 8 weeks, twice a week for 20–30 min, using different acupuncture points. |
| * | We conditionally recommend heat therapy, such as using a hot pack as an adjunctive therapy or as part of the self-management home program, to reduce pain for patients with knee OA. |
| ? | Due to a lack of evidence, the committee decided not to make any recommendation/suggestion regarding the use of trigger point dry needling. |
| ? | Due to a lack of evidence, the committee decided not to make any recommendation/suggestion regarding the use of patellar taping. |
| ? | Due to a lack of evidence, the committee decided not to make any recommendation/suggestion regarding the use of shoe orthotics (medial wedge insoles, shock-absorbing insoles, and arch supports). |
| ? | Due to a lack of evidence, the committee decided not to make any recommendation/suggestion regarding the use of shortwave therapy. |
| * | We conditionally recommend against the provision of unloading shoes, minimalist footwear, or rocker-sole shoes for patients with knee OA. Instead, physiotherapists may advise patients with knee OA to use shock-absorbing footwear. |
| * | We conditionally recommend against the provision of kinesiotaping for patients with knee OA. |
| * | We conditionally recommend against the provision of cold therapy, such as using an ice pack, for patients with knee OA. |
| * | We conditionally recommend against the provision of interferential therapy for patients with knee OA. |
| *** | We strongly recommend against the provision of shoe orthotics (strapped or lateral wedged insoles) for patients with knee OA. |
| *** | Strongly recommended: future research is unlikely to change the nature of the recommendation. |
| ** | Moderately recommended: future research is likely to change the nature of the recommendation. |
| * | Conditionally recommended: future research is more likely to change the nature of the recommendation. |
| ? | Neutral: unable to recommend. |
| * | Conditionally recommend against: future research is more likely to change the “against” nature of the recommendation. |
| ** | Moderately recommend against: future research is likely to change the “against” nature of the recommendation. |
| *** | Strongly recommend against: future research is unlikely to change the “against” nature of the recommendation. |
| *** | We strongly recommend supervised and unsupervised land-based exercise (e.g., walking, muscle-strengthening exercise, and Tai Chi) and/or aquatic exercise to improve pain, function, and quality of life for patients with hip OA. Remarks: All types of exercises were found to be significantly better than no exercise. However, the results were too mixed to determine which exercise program was better than others. The exercise program should last at least 6 weeks. Physiotherapists can prescribe the exercises using the frequency, intensity, time, and type (FITT) principle. |
| ** | We moderately recommend weight-loss management to reduce pain and improve function in patients with hip OA who are overweight or obese. Remarks: Physiotherapists should encourage overweight (BMI ≥ 25 kg/m2) or obese (BMI ≥ 30 kg/m2) patients with hip OA to follow a weight-loss program to lose at least 5% of their body weight. The dietary program should be combined with exercise. |
| * | We conditionally recommend supervised aquatic strengthening exercises to improve pain, function, and quality of life for patients with hip OA. This will depend on individual preferences and the availability of pools in clinical settings. Remarks: The supervised aquatic strengthening exercises should last for 30–60 min, preceded by a 5-min warm-up and followed by a 5-min cool-down, 2–3 times a week for 6–12 weeks. |
| * | We conditionally recommend manual therapy (stretching, soft tissue, and/or joint mobilization and/or manipulation) to improve pain, function, and quality of life for patients with hip OA. This should be considered only as an adjunctive treatment to enable engagement with active management. Remarks: Manual therapy may include trigger point release therapy, muscular and fascial stretching, and joint manipulations (thrust, non-thrust, distraction, anterior-posterior glide, or posterior-anterior glide), performed 1–2 times per week for 6 weeks. This should only be considered an adjunctive treatment. |
| * | We conditionally recommend cognitive-behavioral therapy (CBT) combined with exercises to improve pain and function among patients with hip OA. Remarks: CBT may include relaxation techniques, pleasant imagery, pain coping skills training, and problem-solving techniques, with sessions lasting 35–45 min per week for 8 weeks. CBT may be provided in person or via online programs. |
| * | We conditionally recommend assistive walking devices such as canes be used for patients with hip OA, depending on their individual preferences and capabilities. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest self-management. However, physiotherapists should educate patients about the condition they manage, including its optimal care and prognosis. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of transcutaneous electrical stimulation (TENS). |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of shoe orthotics. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of massage therapy for patients with hip OA. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of pulsed electromagnetic therapy for patients with hip OA. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of shortwave therapy for patients with hip OA. |
| ? | Due to a lack of evidence, the committee decided not to recommend/suggest the use of therapeutic heat therapy (e.g., hot packs) for patients with hip OA. |
| * | We conditionally recommend against the use of laser therapy for patients with hip OA. |
| * | We conditionally recommend against the use of extracorporeal shockwave therapy for patients with hip OA. |
| * | We conditionally recommend against the use of interferential therapy for patients with hip OA. |
| * | We conditionally recommend against the use of therapeutic ultrasound for patients with hip OA. |
| * | We conditionally recommend against the use of local cold applications (e.g., ice packs) for patients with hip OA. |
| * | We conditionally recommend against the use of kinesiotaping for patients with hip OA. |
| * | We conditionally recommend against the use of acupuncture for patients with hip OA. |
| *** | Strongly recommended: future research is unlikely to change the nature of the recommendation. |
| ** | Moderately recommended: future research is likely to change the nature of the recommendation. |
| * | Conditionally recommended: future research is more likely to change the nature of the recommendation. |
| ? | Neutral: unable to recommend. |
| * | Conditionally recommend against: future research is more likely to change the “against” nature of the recommendation. |
| ** | Moderately recommend against: future research is likely to change the “against” nature of the recommendation. |
| *** | Strongly recommend against: future research is unlikely to change the “against” nature of the recommendation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Zoubi, F.M.; Wong, A.Y.L.; Cheing, G.L.Y.; Cheung, J.P.Y.; Fu, S.N.; Tsang, H.H.L.; Law, R.K.Y.; So, B.C.L.; Tsang, R.; Tsang, S.; et al. Adapting a Clinical Practice Guideline for Management of Patients with Knee and Hip Osteoarthritis by Hong Kong Physiotherapists. Healthcare 2023, 11, 2964. https://doi.org/10.3390/healthcare11222964
Al Zoubi FM, Wong AYL, Cheing GLY, Cheung JPY, Fu SN, Tsang HHL, Law RKY, So BCL, Tsang R, Tsang S, et al. Adapting a Clinical Practice Guideline for Management of Patients with Knee and Hip Osteoarthritis by Hong Kong Physiotherapists. Healthcare. 2023; 11(22):2964. https://doi.org/10.3390/healthcare11222964
Chicago/Turabian StyleAl Zoubi, Fadi M., Arnold Y. L. Wong, Gladys L. Y. Cheing, Jason P. Y. Cheung, Siu Ngor Fu, Helen H. L. Tsang, Rainbow K. Y. Law, Billy Chun Lung So, Raymond Tsang, Sharon Tsang, and et al. 2023. "Adapting a Clinical Practice Guideline for Management of Patients with Knee and Hip Osteoarthritis by Hong Kong Physiotherapists" Healthcare 11, no. 22: 2964. https://doi.org/10.3390/healthcare11222964
APA StyleAl Zoubi, F. M., Wong, A. Y. L., Cheing, G. L. Y., Cheung, J. P. Y., Fu, S. N., Tsang, H. H. L., Law, R. K. Y., So, B. C. L., Tsang, R., Tsang, S., Wen, C., Wong, M., Yau, Y. C., & Bussières, A. E. (2023). Adapting a Clinical Practice Guideline for Management of Patients with Knee and Hip Osteoarthritis by Hong Kong Physiotherapists. Healthcare, 11(22), 2964. https://doi.org/10.3390/healthcare11222964








