Abstract
Knee and hip osteoarthritis are common disabling conditions globally. Although numerous international clinical practice guidelines exist to guide physiotherapy management, not all recommendations issued from these guidelines can be translated to other contexts without considering the cultural acceptability and clinical implementability of targeted countries. Because the ADAPTE framework provides a robust methodology to adapt guidelines to the local context, this study used its methodology to adapt high-quality guideline recommendations to promote optimal physiotherapy care for knee and hip osteoarthritis in Hong Kong. The ADAPTE framework was used and modified to complete the adaptation process. International clinical practice guidelines were identified from eight guideline clearinghouses and six electronic databases. Two independent reviewers critically appraised the eligible guidelines using the AGREE II tool. We extracted and tabulated recommendations from high-quality guidelines. A voting-based consensus among interdisciplinary experts was conducted to decide on suitable recommendations for the Hong Kong context and whether there was a need to modify them. Pertinent recommendations were then translated into the traditional Chinese language. Our team members suggested modifying four tools and adding one to explore the patient’s feedback on the recommendations, to the ADAPTE framework. The adaptation was performed on three high-quality guidelines. We adapted 28 and 20 recommendations for treating knee and hip osteoarthritis, respectively. We recommend a multimodal treatment for managing knee and hip osteoarthritis. Land- and aquatic-based exercises, patient education, and self-management were strongly recommended for patients with knee osteoarthritis. Land- and aquatic-based exercises were strongly recommended for patients with hip osteoarthritis. This is the first adaptation study in Hong Kong. It provides guidance to local physiotherapists on managing patients with knee and hip osteoarthritis. Future studies should test the effectiveness of implementing this adapted guideline to improve local physiotherapy care in Hong Kong.
1. Introduction
Osteoarthritis (OA) is one of the most prevalent and disabling health conditions globally, affecting over 595 million patients in 2020 [1]. The prevalence of joints with OA differs across geographical regions. For instance, the age-standardized prevalence of knee and hip OA is the highest in North America and the high-income Asia Pacific region, while it is the lowest in Sub-Saharan Africa [2]. A 2020 umbrella review found that knee and hip OA were associated with overweight/obese, older age, females, low levels of strength or fitness, athletic competition-related joint injuries, heavy lifting at the workplace, climbing, squatting, and kneeling [3].
In Hong Kong (HK), the prevalence of OA was greatest in the knee, followed by the hip [4]. In addition to previously reported risk factors for developing knee and hip OA [3], people in HK with lower education and socioeconomic status have more severe OA conditions [5,6,7]. The estimated direct and indirect costs of OA have caused significant individual, societal, and economic burdens in HK [8]. The direct costs of OA are similar to those in high-income countries; however, this burden is predominantly covered by the government [5].
Globally, it has been estimated that over 344 million patients with OA need rehabilitation services, including non-pharmacological management provided by physiotherapists [9]. To reduce ineffective or unsafe practices, physiotherapists are expected to adopt evidence-based practice approaches in their management of musculoskeletal conditions [10]. Evidence-based clinical practice guidelines (CPGs) aim to improve the effectiveness of healthcare services while reducing costly and undesirable practices [11].
To date, only two Chinese CPGs have been published on the management of knee and hip OA. The first, now outdated, was developed in 2004 [12], targeting family doctors without physiotherapy-related recommendations. The second more generic CPG was published in 2019 [13], targeting all clinicians across all Chinese regions. While it contained recommendations for all osteoarthritic joints, this more recent CPG recommended physiotherapy as a non-pharmacological therapeutic option instead of a distinct profession that can deliver a broad spectrum of therapeutic interventions. Thus, these two CPGs are not appropriate to guide the physiotherapy practice in HK.
There are three commonly used approaches for developing CPGs: creating a new guideline, adopting an existing high-quality CPG as is, or adapting high-quality CPGs while taking into account the cultural, clinical, and organizational contexts of the local community [14,15].
Adapting CPG may better suit the HK context, given the cultural and clinical variations between Western and HK rehabilitation practices. For instance, HK physiotherapy schools teach acupuncture. Therefore, a CPG recommending the use of acupuncture to manage patients with OA would likely be perceived as a facilitator among HK physiotherapists but as a possible barrier for the majority of Western physiotherapists. Guideline adaptation represents a paramount solution to avoid work duplication and time-wasting [16].
There are many frameworks that have been used to adapt CPGs to the local context. Our team selected the ADAPTE framework [15] as it is the most developed and used process which has been used in different cultures and countries [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. In addition, this framework has a toolkit with a user manual to facilitate the use of each step [33].
Against this background, the current study had two objectives. First, to describe the adaptation methods using the ADAPTE framework and its toolkit to adapt CPG to the HK context. Second, to improve the management of knee and hip OA among HK physiotherapists by adapting relevant CPG recommendations on knee and hip OA treatments.
2. Materials and Methods
This study used the ADAPTE framework (version 2.0) [15] and the Adaptation Resource Toolkit provided by the Guideline International Network [33]. The ADAPTE framework consists of 24 steps distributed in 3 phases: setup, adaptation, and finalization.
2.1. Phase 1: Setup
An organizing committee consisting of three people (AB, AW, and FAZ) was formed to oversee the entire ADAPTE process. This committee consisted of methodologists with expertise in developing and implementing CPGs, conducting systematic reviews and quality appraisals of CPGs, and two members familiar with physiotherapy practice in HK. The committee focused on recommendations related to the non-pharmacological therapeutic options routinely delivered by physiotherapists for the management of ‘knee and hip OA’ because of its high prevalence among HK people [4]. Therefore, pharmacological and surgical interventions were excluded, as these interventions are not within the scope of the practice of physiotherapists.
To check whether the adaptation was feasible, we first conducted an exploratory search of the literature. While several recent CPGs and overviews of CPGs for the management of OA [34,35,36] were identified, the search failed to uncover CPGs focusing on non-pharmacological interventions that can be provided by physiotherapists in managing knee and hip OA in China or HK.
A guideline adaptation panel was tasked with the adaptation process. The panel was composed of 13 stakeholders, with expert clinicians having personal experience in managing patients with OA; policy, administrative, or management expertise; researchers with methodological expertise; critical appraisal of the literature; implementation science; and HK culture. Specifically, this multidisciplinary panel included musculoskeletal physiotherapists (RL, RT, MW), physiotherapy researchers (FAZ, AW, HC, AF, BS, ST), rheumatologists (HT, JW), orthopedists (JC, CW), a nurse (CY), as well as a representative from the HK Physiotherapy Association (RT). The views and preferences of patients with knee and hip OA were explored after formulating the recommendations.
2.2. Phase 2: Adaptation
2.2.1. Scope and Purpose Module
In this phase, we used the PIPOH format (Population, Interventions, Professionals, Outcomes, and Healthcare settings) [33] to identify a specific health question for this guideline. Our research question was: What are the conservative non-pharmacological treatments that can be recommended for the management of patients with knee and hip OA and provided by HK physiotherapists?
2.2.2. Search and Screen Module
After formatting the research question, literature search strategies were developed with the consultation of a health librarian (see Table S1a). We searched six key electronic databases: MEDLINE (PubMed), EMBASE, CINHAL (Complete EbscoHost), PEDro, Scopus, and Epistemonikos. Additionally, we searched several guidelines clearinghouses, but only a few of them were still updating their guidelines lists. Table 1 presents the full list of electronic databases and guideline clearinghouses that were searched. These databases were first searched on 1 June 2021 and again on 1 November 2021.

Table 1.
A list of the medical databases and guideline clearinghouses that have been searched.
We included CPGs that were (a) published within the past 5 years (2016–2021), (b) available in English or Chinese, (c) designed based on systematic reviews that answered specific research questions, and (d) focused on conservative non-pharmacological management options that are within the scope of physiotherapy practice for managing knee and hip OA in all healthcare settings. We excluded CPGs that were (a) targeting the pediatric population, (b) based on consensus, and (c) focusing on surgical or pharmaceutical interventions.
Two reviewers (FAZ and a trained research assistant) independently applied the eligibility criteria to screen titles and abstracts. Reviewers resolved any disagreements through discussions, and a third reviewer (AB) adjudicated any persistent disagreements.
2.2.3. Quality Assessment Module
All included CPGs were critically appraised for methodological quality by two independent appraisers (FAZ and AW) using the Appraisal of Guidelines for Research and Evaluation (AGREE) II tool [37]. The AGREE II tool is a reliable and valid evaluation tool containing 23 items in 6 domains (scope and practice, stakeholder involvement, rigor of development, clarity of presentation, applicability, and editorial independence) [37]. Each item of the AGREE II tool was rated on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). The domain scores range from 0 to 100%, with higher scores representing stronger between-reviewer agreements. The domain scores were calculated using the formulas in the AGREE II manual [38]. To identify a guideline of high quality, the organizing committee proposed two criteria: (a) a cut-off score ≥ 60% for at least 4 out of 6 of the AGREE II domains; and (b) a score of ≥75% for the domain ‘methodological rigor’. The two appraisers initially appraised the included CPGs. If the discrepancy in the rating of any individual item was ≥2, a discussion was held until consensus was reached.
2.2.4. Extracting Recommendations from High-Quality CPGs
We extracted recommendations only from eligible, high-quality CPGs. Recommendations judged to be unrelated to knee and hip OA were excluded. Two independent reviewers (FAZ and ST) categorized high-quality CPGs’ recommendations into three groups: non-pharmacological treatments mainly provided by HK physiotherapists (✓), non-pharmacological treatments partly provided by HK physiotherapists as the intervention requires certain postgraduate training (?), and other treatments not provided by HK physiotherapists/not within the scope of practice (✗). Only recommendations that were judged by both reviewers to be (✓) or (?) were included.
Next, the similarities and differences across recommendations from the identified high-quality guidelines were tabulated in matrices. These matrices were presented to the guideline adaptation panel to assess the applicability (e.g., organizational and system barriers, treatment availability, and resource availability in HK) and acceptability (e.g., whether the recommendations are compatible with HK culture and values) of the recommendations.
Members of the guideline adaptation panel attended an online meeting in November 2021. Prior to the meeting, the panel committee received the working plan, the adaptation process, all eligible high-quality guidelines, and the matrices. During the meeting, two members of the organizing committee (FAZ and AW) encouraged the discussion among the panel members to reach a consensus about the feasibility, implementability, and applicability of the recommendations in HK. Panel members then received a link to anonymously vote on each guideline using a 3-point scale (accept as is, accept with modification, reject this guideline). Members were informed a priori that at least 75% of the panel had to vote and reach an 80% agreement for a given recommendation to be retained. If no consensus was reached, we encouraged further discussion among panelists prior to conducting additional rounds (n = 1–2) of voting to reach an agreement. If the panel decided that one of the guidelines was superior to others, our plan was to contact the original authors and ask for permission to adapt their guideline recommendations. If two or more guidelines were deemed acceptable, we planned to invite the panel to consider each recommendation in terms of quality, strength, wording, and relevance to the HK practice and then vote anonymously on the recommendations using an online tool (https://strawpoll.com/, accessed on 17 November 2022).
All these steps were recorded, and all modifications to the recommendations were documented. The final draft of the adapted guideline provided an account of the steps taken to reach an agreement on recommendations, along with related documentation. The statements generated by the committee were categorized as strongly recommended, moderately recommended, conditionally recommended, neutral, conditionally against, moderately against, and strongly against.
2.3. Phase 3: Finalization
The final draft of the adapted guideline was sent to an external review panel composed of all relevant stakeholders, including local researchers, practicing physiotherapists, policymakers, and experts from professional bodies. A purposive sampling method was employed to recruit a total of 10–15 external reviewers from different healthcare settings and representatives of multiple HK geographical areas. This final phase allowed for the formal endorsement of the guideline by key local stakeholders. Endorsement by professional bodies may boost guideline uptake among their members. External reviewers were encouraged to provide their comments, feedback, and appraisals of the adapted CPG using a survey.
In addition, we translated the recommendations to Chinese by two members of this guideline and sent them to a convenient sample of five patients with knee OA and three with hip OA to obtain their feedback. Patients were recruited from our team members’ networks and encouraged to read the recommendations and comment on the perceived applicability and feasibility of implementing those recommendations. The feedback received from the external reviewers and patient samples was considered by the organizing committee, which addressed each comment and further refined the adapted CPG. The final version of the adapted CPG was submitted for publication in a peer-reviewed journal and presented at national and international conferences.
3. Results
3.1. Phase 1: Setup
The ADAPTE framework started by checking whether the adaptation was feasible, followed by establishing a committee, and then selecting a topic. The order of these steps is not rational, as we need to first establish a committee, then select the topic, and finally check the feasibility of adaptation.
3.2. Phase 2: Adaptation
Search and Screen Module
Figure 1 presents the PRISMA flowchart illustrating the results of searching, screening, and full-text reviewing. Our search retrieved a total of 8068 citations from the six electronic databases. After removing the duplicates (n = 3894), 4174 titles and abstracts were screened, resulting in the exclusion of 4134 citations. Thirty-one CPGs were excluded with reasons after the full-text reviews, yielding nine eligible guidelines [39,40,41,42,43,44,45,46,47] (Table S2). Our search on the guideline clearinghouse websites identified 36 guidelines, of which 31 were ineligible and 5 were included [48,49,50,51,52] (Table S1b).
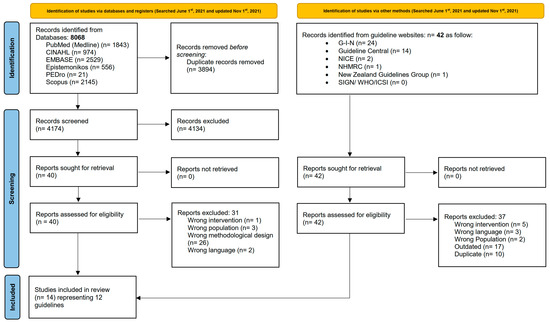
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases, registers, and other sources [53].
In total, we included 14 publications representing 12 guidelines because the Ottawa guideline for knee OA was published in 3 separate publications [43,44,45]. Three guidelines only targeted knee OA and were developed by the American Academy of Orthopedic Surgeons (AAOS) [52], the Turkish League Against Rheumatism (TLAR) [39], and the Ottawa panel [43,44,45]. Three guidelines targeted hip OA alone and were developed by the AAOS [51], the American Physical Therapy Association (APTA) [50], and the Ottawa Panel [46]. Lastly, six guidelines targeting a mixed population of OA were developed by the Royal Dutch Society for Physical Therapy (KNGF) [48], the Osteoarthritis Research Society International (OARSI) [42], the American College of Rheumatology (ACR) [41], the European Alliance of Associations for Rheumatology (EULAR) [40], the Pan-American League of Associations for Rheumatology (PANLAR) [47], and the Royal Australian College of General Practitioners (RACGP) [49]. Table 2 presents the characteristics of the included guidelines.

Table 2.
Characteristic of the included guidelines.
3.3. Quality Assessment Module
Table 3 and Table 4 present the quality assessment results of guidelines using the AGREE II tool for knee and hip OA, respectively. The overall quality scores ranged from 34% for the PANLAR guideline [47] to 76% for the KNGF guideline [48]. Three guidelines met our criteria for high-quality guidelines for both knee and hip OA: RACGP [49], AAOS [52], and KNGF [48].

Table 3.
Domain and total scores of the knee osteoarthritis guidelines using the AGREE II tool.

Table 4.
Domain and total scores of the hip osteoarthritis guidelines using the AGREE II tool.
To assess the content of these high-quality guidelines, we created matrices listing all clinical recommendations for knee and hip OA. For knee OA, a total of 100 recommendations were extracted and classified as non-pharmacological treatments mainly provided by HK physiotherapists (n = 39), non-pharmacological treatments partly provided by HK physiotherapists (n = 12), and other treatments that are not provided by HK physiotherapists or not within the scope of the practice (n = 49). For hip OA, a total of 79 recommendations were extracted and classified as non-pharmacological treatments mainly provided by HK physiotherapists (n = 27), non-pharmacological treatments partly provided by HK physiotherapists (n = 3), and other treatments that are not provided by HK physiotherapists or not within the scope of the practice (n = 49). Table S3 presents the results of the categorization for knee and hip OA, respectively. Table S4 presents the guidelines’ recommendations for knee and hip OA, respectively.
Following the reviews and discussions of both the quality appraisal and the matrices, the adaptation panel voted (9 of 11 members, 82%) to include recommendations for knee OA treatments only from the RACGP [49] and AAOS [52] guidelines. In addition, the panel voted to modify the recommendations’ content of the exercises and modalities parameters (9/11, 82%). For hip OA, the panel voted (10/11, 91%) to include recommendations only from the RACGP [49] and AAOS [52] guidelines and excluded KNGF [48]. The panel voted to modify the recommendations’ content of the exercise and modalities parameters (10/11, 91%).
To modify the recommendations’ content, two reviewers (FAZ and CY) reviewed all the randomized controlled trials included in the RACGP [49] and AAOS [52] guidelines to extract their contents. The organizing committee decided to keep trials that were found to be clinically significant by these two guidelines’ developers. In addition, any recommendations that were based on a consensus among guideline panelists or used a non-randomized controlled trial design were discarded. Accordingly, the organizing committee rephrased the recommendations to reflect these criteria and add further details.
Table S5 presents summaries of trials that met these criteria for both knee and hip OA, respectively. In total, 28 and 20 recommendations for knee and hip OA were deemed suitable for adaptation, respectively. Table 5 and Table 6 present summaries of the key recommendations for the adapted CPG for the non-pharmacological treatments that can be provided by physiotherapists for knee and hip OA, respectively.

Table 5.
Summary of the key recommendations for the adapted clinical practice guideline for the non-pharmacological treatments that can be provided by physiotherapists for knee OA.

Table 6.
Summary of the key recommendations for the adapted clinical practice guideline for the non-pharmacological treatments that can be provided by physiotherapists for hip OA.
Table S6 presents the differences between the original recommendations suggested by the RACGP [49] and AAOS [52] guidelines and our modified recommendations for knee and hip OA, respectively.
3.4. Phase 3: Finalization
The final draft of the adapted guideline was sent to eight external review panels, representing the audience for this guideline. We also sent the traditional Chinese-translated recommendations to five patients with knee OA and one with hip OA. The comments and feedback arising from the panel and patients were reviewed and discussed by the panel members. Where relevant, clarifications were made to the recommendations and future implementation plans.
The adapted guideline, all its pertained documents, a summary of recommendations, and a translation of the recommendations into the traditional Chinese language will be accessible on the official website of the HK Physiotherapy Association: https://www.hongkongpa.com.hk/, accessed on 29 October 2023.
3.5. Plan for Updating the Guideline
The adaptation panel plans to update the adapted guideline five years after publication.
4. Discussion
This study adapted the published guidelines for the non-pharmacological treatments for knee and hip OA management that can be recommended to physiotherapists in HK. Our systematic search identified a total of 12 guidelines, of which three were of high quality [48,49,52]. With the availability of high-quality guidelines in the literature, the need to adapt them becomes more practical than developing new ones [15].
4.1. Similarities and Differences with Recommendations from the Original CPGs
For knee OA, the current guideline strongly recommends supervised and unsupervised land-based exercise (e.g., walking, muscle-strengthening exercise, and Tai Chi), aquatic exercise, patient education, and self-management. We moderately recommend neuromuscular training (i.e., balance, agility, coordination), weight management, canes, and braces. We conditionally recommend the following treatments: yoga, aquatic stationary cycling, massage therapy, manual therapy, transcutaneous electrical stimulation, wearable pulsed electromagnetic field devices, percutaneous electrical nerve stimulation, laser therapy, extracorporeal shockwave therapy, acupuncture, and heat. Generally, all recent guidelines share similar recommendations to ours, including patient education, weight management, supervised and unsupervised exercises, and reducing the loading on the knee using canes for patients with knee OA [54,55]. Our recommendations were generally identical to the ones recommended by either one of the AAOS [52] or RACGP [49]. If a recommendation was only synthesized by one of the two guidelines but not the other, then we relied on it to design our recommendation. An example of that is yoga, which was conditionally recommended by RACGP [49] but not discussed by AAOS [52]. If both guidelines synthesized a similar recommendation, our team would accept the recommendation from both guidelines. For instance, both of them highly recommend land-based exercises. If both guidelines synthesized contradicting recommendations, our team looked at the trials used by each guideline to synthesize relevant recommendations. Most of the time, we accepted the AAOS [52] recommendations as they included more recent and high-quality trials than RACGP [49]. For example, AAOS [52] highly recommended providing self-management education, while RACGP [49] was unable to provide recommendations/suggestions on it. We relied on the AAOS recommendation as it included recent moderate-to-high-quality trials [56,57,58], compared to the older and very low-quality trials [59] included by RACGP.
For hip OA, the current guideline strongly recommends both supervised and unsupervised land-based exercise (e.g., walking, muscle-strengthening exercise, and Tai Chi) and aquatic exercise. We moderately recommend weight-loss management for overweight and obese patients. We conditionally recommend supervised aquatic strengthening exercises, manual therapy, cognitive-behavioral therapy, and assistive walking devices such as canes.
Our recommendations were generally based on reviewing the ones recommended by the KNGF [48] and RACGP [49]. Although it was published in 2018 compared to KNGF (published in 2020), we relied more on recommendations from RACGP as they conducted systematic searches for each research question, while KNGF searched previously published systematic reviews first. In the event that these reviews were not available, they investigated trials or textbooks. A lack of extensive literature searches was the major limitation of the KNGF [48], as declared by the developers, which may have influenced the strength of the recommendations.
On the other hand, our reliance on RACGP recommendations was not blind. As we set out our criteria, we mainly relied on evidence obtained from high-quality randomized controlled trials. Nonetheless, the content and strength of our recommendations were comparable to those of the RACGP, with the exception of weight management, transcutaneous electrical nerve stimulation, massage therapy, heat therapy, and transcutaneous electrical stimulation. Even though there are no published trials on weight management, our panel agreed that weight management is essential for overweight and obese individuals. The majority of osteoarthritis guidelines concur on the importance of weight management [60]. However, because of the lack of trials for hip OA, we lowered the strength of the recommendation to moderately recommended.
As our panel members suggested modifying the recommendations by providing more details on the interventions’ parameters, we added remarks and statements to the original recommendations. We expect that this will boost the use of the recommendation among local physiotherapists, as the suggestion came from local expert clinicians who are familiar with the local needs and preferred language to design recommendations. This consideration of the trans-contextual issues of the local stakeholders is the core concept of adapting CPGs [16].
4.2. Stakeholder Considerations
As we recommend multimodal management for patients with knee and hip OA, it is important for individual physiotherapists to select the appropriate combination of therapies by considering their effectiveness (i.e., on pain levels and function), any potential risks to the patient (e.g., the suitability of the exercise to the age of the patient), and costs (e.g., the ability of the patient to bear the cost of yoga or Tai Chi classes). In addition to that, the physiotherapist shall consider the patient’s satisfaction with the provided treatment over time [61]. Current evidence provided by this guideline supports non-pharmacological interventions that can be provided by any physiotherapist in all HK health sectors: hospital authorities, non-governmental organizations, and private clinics. Yoga and Tai Chi may be the only two exceptions, as the government may not financially cover them. In addition, they may require a certified registered physiotherapist to provide them to patients.
4.3. Cultural and Clinical Context
The cultural adaptation of clinical practice guidelines can significantly impact the recommendations for physiotherapists managing patients with knee or hip OA. By acknowledging and accounting for cultural and clinical contexts, physiotherapists can tailor their recommendations to align with the cultural values, preferences, and expectations of their patients in HK, resulting in more effective and patient-centered care.
In HK’s cultural context, there are several cultural factors that can impact the acceptance and adherence to recommended treatments [62]. These include traditional health beliefs, family involvement, language and communication, and socioeconomic and environmental factors. Physiotherapists need to take cultural nuances into account and address them in order to ensure that the recommendations are meaningful and relevant to the local population. By implementing these practices, it fosters a strong sense of trust between physiotherapists and their patients. This, in turn, promotes active participation from patients, leading to better treatment results [14,15].
Regarding traditional health beliefs, individuals in HK prefer a comprehensive approach that integrates complementary and alternative therapies with conventional physiotherapy interventions [63]. Physiotherapists have the option to incorporate traditional Chinese medicine techniques, such as acupuncture, into the treatment plan to accommodate patients’ cultural preferences. Due to its perceived safety compared to Western medicine, traditional Chinese medicine enjoys high regard among the general public in HK [64], with a large majority of patients with low back pain opting for complementary and alternative therapies such as traditional Chinese medicine and acupuncture [65]. While most physiotherapists in HK have received comprehensive training in complementary and alternative therapies, such as acupuncture, as part of their undergraduate education, those who obtained their degrees from universities overseas may require further training to effectively address patients’ needs in the local community.
Additionally, acknowledging the significance of family involvement in decision-making and considering the support systems within the cultural context can help optimize treatment outcomes. The interdependence and connectedness of family members are deeply rooted in Chinese Confucian beliefs [66]. Language and communication play a vital role in cultural contexts. Translating and adapting the recommendations into the local language, along with using culturally appropriate examples and analogies during patient education, can enhance comprehension and foster patient cooperation [67].
Furthermore, socioeconomic and environmental factors influenced by culture can affect the feasibility and accessibility of treatments [68,69]. Physiotherapists should consider these when tailoring recommendations for patients. For example, suggesting exercises that can be performed in small living spaces, considering financial constraints when recommending assistive devices, or highlighting community resources for ongoing support and follow-up care can all enhance the cultural appropriateness of the recommendations.
In HK’s clinical context, the cultural adaptation of CPGs should consider the applicability of recommendations at the policy level [14,15]. While patients in Western countries have direct access to physiotherapy services, the traditional hierarchical structure in HK requires patients with knee and hip OA to obtain a medical referral [70]. Soon, however, patients will be able to access physiotherapy services directly (i.e., without a medical referral) [71]. While this is a significant professional development for physiotherapists, it will increase their pressure to deliver evidence-based practice. The objective of the present study was to assist healthcare professionals in effectively managing patients diagnosed with knee and hip OA. At the request of our expert clinicians, we have revised the recommendations to incorporate parameters for non-pharmacological modalities. This will help ensure that the recommendations are easily understood and can be implemented effectively.
Another concern is the shortage of physiotherapists in HK, which is impacting the availability of services for older individuals. Specifically, 34% of the 174 elderly services units are unable to fill their open vacancies [72]. There is an increasing demand for physiotherapists to see a higher number of patients per day in public settings, which could potentially impact the quality of healthcare services provided [73]. Furthermore, due to the shortage of physiotherapists, patients with knee OA who consult a general practitioner and receive a referral to see a physiotherapist may experience significant delays in accessing their services, with wait times of up to 6 months in public settings. Hence, physiotherapists may need to explore the implementation of group-based supervised interventions as a means to effectively manage a larger number of patients while maintaining close monitoring of their progress.
4.4. Dissemination and Implementation Plan
A 2019 systematic review revealed that many interventions provided by physiotherapists to manage musculoskeletal conditions, including knee OA, were not recommended [74]. This trend has not changed over the past three decades, with almost 40% of the provided physiotherapy treatments not recommended [75]. There are several individual (lack of knowledge, lack of English proficiency, lack of skills about research and statistics, lack of interest) and organizational (lack of time, lack of access, lack of resources, and generalizability of the recommendations to other contexts) factors that impede the use of recommended care in clinical practice among physiotherapists [76]. Knowledge translation is a process used to tackle such factors and bridge the gap between recommended care and clinical practice [77]. The closure of this gap is possible by developing and implementing knowledge translation strategies targeting physiotherapists, patients with knee and hip OA, and healthcare organizations [78]. Thus, to facilitate the implementation of our guideline, we considered the Guideline Implementation Planning Checklist [78]. To increase the local physiotherapists’ awareness, the HK Physiotherapy Association will endorse this guideline and help disseminate its content and resources via its website (https://www.hongkongpa.com.hk/, accessed on 29 October 2023). The implementation tools include handouts for patients with knee and hip OA and physiotherapists (Table 5 and Table 6), algorithms (Figure 2 and Figure 3), regional and local conferences [79], and seminars.
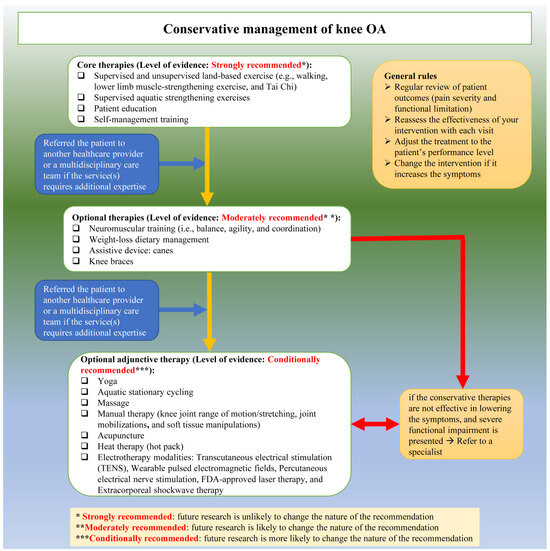
Figure 2.
Conservative management of knee OA algorithms.
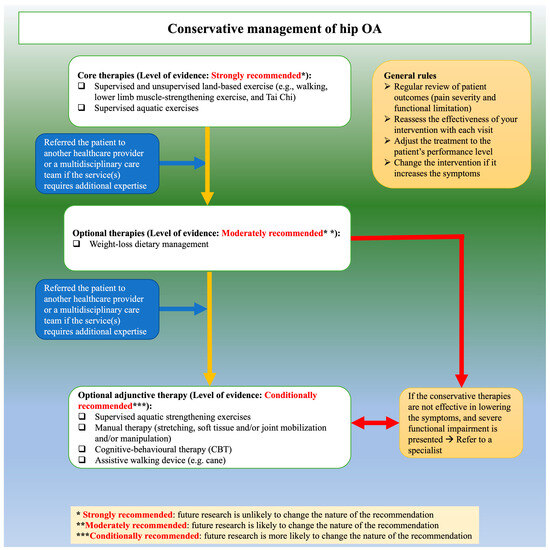
Figure 3.
Conservative management of hip OA algorithms.
The ADAPTE framework and other frameworks are limited in providing a dissemination and implementation methodology to allow for the uptake of the adapted recommendations into the local context. Therefore, we recommend developing post-hoc, clear, and detailed methods to implement the adapted guidelines. In addition, although the ADAPTE framework provides a sample survey to seek the external review committee’s feedback on the adapted guideline (Tool 17), we have modified this tool to meet our needs (see Table S7). However, there is no tool to seek the patients’ feedback on the recommendations. To overcome this issue, we have developed our own tool to achieve this mission (see Table S8).
4.5. Future Research
There are several frameworks that may be used to adapt CPGs to the local context [80]. A recent systematic review identified eight frameworks [80], of which half—RAPADAPTE, Adapted ADAPTE, MAGIC, and CAN-IMPLEMENT—were derived from the ADAPTE framework. These adaptation frameworks consider the trans-contextual issues of the local settings for the adapting countries [16]. This is of paramount importance as it is considered the cornerstone to facilitate the guideline implementation [81].
The ADAPTE framework has been utilized across different medical conditions [80] in both developed [17,18,19,20,21,22,23,24,25,26] and developing [27,28,29,30,31,32] countries. Importantly, the ADAPTE framework considers the local needs, medical priorities, different policies, and availability of resources for the targeted country/setting/organization [80]. Furthermore, it comes with a detailed resource toolkit and a user manual [33].
In our opinion, the ADAPTE framework has a rigorously well-developed, structured, and resilient approach to handling the differences between developing and adapting contexts. Nevertheless, we found that it needs to be modified in some of its steps or tools. For instance, in the setup phase, the order of the steps was to check the feasibility of the adaptation, establish a committee, and then select a topic. However, the logical way should be to select the topic first and then check its adaptation feasibility. Furthermore, some of the tools need amendments or further expansion. For example, although Tool 2 provides a list of guideline clearinghouses and resources to find CPGs, most of these clearinghouses are either inaccessible or have not been updated for a long time due to insufficient funding. In addition, these resources mainly focus on the medical literature rather than other healthcare disciplines, such as physiotherapy. These issues have also been raised by other adaptation studies using the ADAPTE framework [17,27,28].
Despite these limitations, the ADAPTE framework developers allowed their users to either use, ignore, or modify the original steps or tools. Further, most of the prior adaptation studies that used the ADPATE framework benefited from these flexibility options, mostly by modifying the tools and/or steps [27,28,29,30] and being less likely to use them as is [26,32]. Therefore, we have proposed some major and minor modifications to the ADAPTE framework to facilitate and shorten the adaptation process (see Table S9). This practicability and friendliness of the ADPATE framework may explain its popularity over other frameworks [80].
Our adaptation panel members were clinically skilled and methodologically experts in the field of knee and hip OA. This enriched the discussion and feedback from the panel members, which allowed the modification of the content and changes to the recommendations to suit local needs. This is another feature suggested by the ADAPTE framework: using a multidisciplinary team. However, the framework does not provide any definition of the meaning of ‘experts,’ their level of expertise, or how to choose them among other peers. This concern has also been reported previously by other colleagues [17], recommending further refinements on future updates of the ADPTE framework. We agree with this recommendation and suggest further distinguishing between decision-makers and only skilled ‘experts’.
Research that uncovers the practice patterns of local physiotherapists to explore how they manage patients with knee and hip OA is needed. This will help explore the gaps in practice compared to recommended care. This, in turn, will allow for the design of a knowledge translation strategy that can be tailored to the local needs of physiotherapists [78].
4.6. Strengths and Weaknesses
There are several strengths in our work. First, use a comprehensive search covering the main electronic databases and clearinghouse websites to identify potential guidelines. Second, using the ADAPTE framework [15] over the other frameworks provided a clear path with useful resources to adapt guidelines on knee and hip OA. Third, modify the recommendations to provide more clinically useful recommendations by only including interventions with parameters proven to be effective from clinical trials. As suggested by local senior clinicians, this is important to allow the recommendations to be implementable and more trustworthy, as it shows the reliance on a high level of evidence. Fourth, although this is our first experience with adaptation studies, the adaptation process (see Table S10) took around 25 months, which is considered to be comparable with the development of a de novo guideline (~2–3 years) [82]. Other studies that used the ADAPTE framework reported different durations to accomplish their projects, ranging from 6 months [83] to 36 months [28].
Nevertheless, our study has some limitations. First, our search was limited to guidelines published in English or Chinese. We identified several guidelines published in other languages, which might have limited the comprehensiveness of our recommendations. Second, the AGREE II tool has some limitations related to its assessment of clinical credibility. The AGREE II developers have also developed AGREE-REX: Recommendation Excellence [84], which was designed to evaluate the clinical credibility and implementability of the guidelines’ recommendations. We have not used AGREE-REX, as it is not mentioned in the ADAPTE framework. Instead, the ADAPTE framework relies on the discussion within the adaptation panel. We plan to include AGREE-REX in our future adaptation studies to evaluate its usefulness. Third, we found that the ADAPTE framework was lengthy and required thorough training among its users. This observation has been described by almost all prior users of the ADAPTE framework [17,18,27,29,30,32,83].
5. Conclusions
This is the first study to provide a detailed description of the use of the ADAPTE framework in physiotherapy research. We found the ADAPTE framework to be efficient, well-structured, and rigorously guided in the cross-cultural adaptation of guidelines to the local context. Furthermore, this framework allows modifications to be applied to the adaptation process according to contextual needs [15]. This flexibility allowed us to add further steps to modify the recommendations based on our panel’s preferences and needs.
Current evidence on the effectiveness of conservative management of knee and hip OA suggests the use of all forms of supervised or unsupervised exercises. Considering patient preferences and the availability of resources, physiotherapists can offer a multimodal intervention to patients with knee or hip OA. A continual monitoring of the outcomes of the patients with knee and hip OA (pain intensity and functional disability) should regularly guide the physiotherapist about the progress of the provided interventions.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare11222964/s1. Table S1a: Search strategies used for the electronic databases. Table S1b: Search strategies used for the guideline clearinghouses. Table S2: List of the excluded studies from electronic databases with reasons. Table S3: Results of categorizing the recommendations from high-quality guidelines. Table S4: Visual presentation of the recommendations of the three high-quality guidelines. Table S5: Summary of the included trials for the knee and hip osteoarthritis recommendations. Table S6: Comparison between the original and modified recommendations for knee and hip osteoarthritis (OA). Table S7: External review panel survey. Table S8: Patient feedback survey. Table S9: Changes applied to the ADAPTE framework methodology to suit the Hong Kong context. Table S10: Work plan—Knee and hip osteoarthritis guideline panel.
Author Contributions
F.M.A.Z., A.E.B. and A.Y.L.W. developed the idea for research and designed the methodology. F.M.A.Z. was responsible for the literature search, collection/processing of data, and data analysis. F.M.A.Z. and A.Y.L.W. screened citations, included eligible guidelines, and appraised them using the AGREE II tool. F.M.A.Z. wrote the manuscript versions. F.M.A.Z., A.Y.L.W., G.L.Y.C., J.P.Y.C., S.N.F., H.H.L.T., R.K.Y.L., B.C.L.S., R.T., S.T., C.W., M.W., Y.C.Y. and A.E.B. contributed to the study design, interpretation of data, and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Funds were provided as start-up funding to Dr. Fadi Al Zoubi from the Department of Rehabilitation Sciences at The Hong Kong Polytechnic University (2020–2023) (Funding number: P0034815). The content of the guideline has not been influenced by the views of the funding organization. No conflict of interest were disclosed in relation to this study.
Institutional Review Board Statement
Ethical approval for this study was obtained from the Human Subjects Ethics Committee at The Hong Kong Polytechnic University (application number HSEARS20221027002). All participants (clinicians and patients) provided signed informed consent to participate in the survey.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used and analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors sincerely thank all the participants who have joined the study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| OA | Osteoarthritis |
| HK | Hong Kong |
| CPG | Clinical Practice Guidelines |
| AGREE | Appraisal of Guidelines for Research and Evaluation |
| PIPOH | Population, Interventions, Professionals, Outcomes, Healthcare settings |
| AAOS | American Academy of Orthopaedic Surgeons |
| TLAR | Turkish League Against Rheumatism |
| APTA | American Physical Therapy Association |
| KNGF | Royal Dutch Society for Physical Therapy |
| OARSI | Osteoarthritis Research Society International |
| ACR | American College of Rheumatology |
| EULAR | European alliance of associations for rheumatology |
| PANLAR | Pan-American League of Associations for Rheumatology |
| RACGP | Royal Australian College of General Practitioners |
References
- GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.-A.; Smith, E.; Hill, C.; Bettampadi, D.; Mansournia, M.A.; Hoy, D.; Ashrafi-Asgarabad, A.; Sepidarkish, M.; Almasi-Hashiani, A.; et al. Global, regional and national burden of osteoarthritis 1990–2017: A systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 819–828. [Google Scholar] [CrossRef]
- Schram, B.; Orr, R.; Pope, R.; Canetti, E.; Knapik, J. Risk factors for development of lower limb osteoarthritis in physically demanding occupations: A narrative umbrella review. J. Occup. Health 2019, 62, e12103. [Google Scholar] [CrossRef] [PubMed]
- The Chinese University of Hong Kong. Osteoarthritis in Hong Kong Chinese—Prevalence, Aetiology and Prevention. 2001. Available online: http://www.cuhk.edu.hk/ipro/010306e.htm (accessed on 21 October 2021).
- Woo, J.; Lau, E.; Lau, C.S.; Lee, P.; Zhang, J.; Kwok, T.; Chan, C.; Chiu, P.; Chan, K.M.; Chan, A.; et al. Socioeconomic impact of osteoarthritis in Hong Kong: Utilization of health and social services, and direct and indirect costs. Arthritis Rheum. 2003, 49, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.C.; Cooper, C.; Lam, D.; Chan, V.N.H.; Tsang, K.K.; Sham, A. Factors associated with osteoarthritis of the hip and knee in Hong Kong Chinese: Obesity, joint injury, and occupational activities. Am. J. Epidemiol. 2000, 152, 855–862. [Google Scholar] [CrossRef]
- Kumta, S.M.; Lau, E. Risk factors for primary osteoarthritis of the hip and knee in the Hong Kong Chinese population. Hong Kong Med. J. 2007, 13, S9–S14. [Google Scholar]
- Yuen, W.H. Osteoarthritis of knees: The disease burden in Hong Kong and means to alleviate it. Hong Kong Med. J. 2014, 20, 5–6. [Google Scholar] [CrossRef][Green Version]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- World Confederation for Physical Therapy. Policy Statement: Evidence-Based Practice. 2019. Available online: https://world.physio/policy/ps-ebp (accessed on 30 October 2023).
- Woolf, S.H.; Grol, R.; Hutchinson, A.; Eccles, M.; Grimshaw, J. Clinical guidelines: Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999, 318, 527–530. [Google Scholar] [CrossRef]
- Department of Community and Family Medicine. Clinical Guidelines for Managing Lower-Limb Osteoarthritis in Hong Kong Primary Care Setting; Department of Community and Family Medicine, Chinese University of Hong Kong: Hong Kong, China, 2004. [Google Scholar]
- Zhang, Z.; Huang, C.; Jiang, Q.; Zheng, Y.; Liu, Y.; Liu, S.; Chen, Y.; Mei, Y.; Ding, C.; Chen, M.; et al. Guidelines for the diagnosis and treatment of osteoarthritis in China (2019 edition). Ann. Transl. Med. 2020, 8, 1213. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Fretheim, A.; Oxman, A.D. Improving the use of research evidence in guideline development: 13. Applicability, transferability and adaptation. Health Res. Policy Syst. 2006, 4, 25. [Google Scholar] [CrossRef]
- Fervers, B.; Burgers, J.S.; Voellinger, R.; Brouwers, M.; Browman, G.P.; Graham, I.D.; Harrison, M.B.; Latreille, J.; Mlika-Cabane, N.; Paquet, L.; et al. Guideline adaptation: An approach to enhance efficiency in guideline development and improve utilisation. BMJ Qual. Saf. 2011, 20, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Norris, S.L.; Bero, L. The advantages and limitations of guideline adaptation frameworks. Implement. Sci. 2018, 13, 72. [Google Scholar] [CrossRef]
- Chakraborty, S.P.; Jones, K.M.; Mazza, D. Adapting lung cancer symptom investigation and referral guidelines for general practitioners in Australia: Reflections on the utility of the ADAPTE framework. J. Eval. Clin. Pract. 2014, 20, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Harstall, C.; Taenzer, P.; Zuck, N.; Angus, D.K.; Moga, C.; Scott, N.A. Adapting low back pain guidelines within a multidisciplinary context: A process evaluation. J. Eval. Clin. Pract. 2013, 19, 773–781. [Google Scholar] [CrossRef] [PubMed]
- González-Lamuño, D.; Rodríguez, A.L.; Yanes, M.I.L.; Barrio, S.M.-D.; Díaz-Guerra, G.M.; Peris, P. Clinical practice recommendations for the diagnosis and treatment of X-linked hypophosphatemia: A consensus based on the ADAPTE method. Med. Clin. 2021, 159, 152.e1–152.e12. [Google Scholar] [CrossRef]
- Hoedl, M.; Schoberer, D.; Halfens, R.J.G.; Lohrmann, C. Adaptation of evidence-based guideline recommendations to address urinary incontinence in nursing home residents according to the ADAPTE-process. J. Clin. Nurs. 2018, 27, 2974–2983. [Google Scholar] [CrossRef]
- Hurtado, M.M.; Quemada, C.; García-Herrera, J.M.; Morales-Asencio, J.M. Use of the ADAPTE method to develop a clinical guideline for the improvement of psychoses and schizophrenia care: Example of involvement and participation of patients and family caregivers. Health Expect. 2021, 24, 516–524. [Google Scholar] [CrossRef]
- Lovell, M.; Luckett, T.; Boyle, F.; Stubbs, J.; Phillips, J.; Davidson, P.M.; Olver, I.; von Dincklage, J.; Agar, M. Adaptation of international guidelines on assessment and management of cancer pain for the Australian context. Asia Pac. J. Clin. Oncol. 2015, 11, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Pringsheim, T.; Addington, D. Canadian Schizophrenia Guidelines: Introduction and Guideline Development Process. Can. J. Psychiatry 2017, 62, 586–593. [Google Scholar] [CrossRef]
- Roberge, P.; Fournier, L.; Brouillet, H.; Delorme, A.; Beaucage, C.; Côté, R.; Demers, P.; Gervais, M.; Laflamme, F.; Latulippe, L.; et al. A provincial adaptation of clinical practice guidelines for depression in primary care: A case illustration of the ADAPTE method. J. Eval. Clin. Pract. 2015, 21, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Selby, P.; Hunter, K.; Rogers, J.; Lang-Robertson, K.; Soklaridis, S.; Chow, V.; Tremblay, M.; Koubanioudakis, D.; Dragonetti, R.; Hussain, S.; et al. How to adapt existing evidence-based clinical practice guidelines: A case example with smoking cessation guidelines in Canada. BMJ Open 2017, 7, e016124. [Google Scholar] [CrossRef]
- Mack, S.; Hahn, S.; Palli, C.; Findling, T.; Lohrmann, C. Adaptation of Clinical Practice Guideline Recommendations in Hospitals for People Living With Dementia and Their Caregivers. Worldviews Evid. Based Nurs. 2019, 16, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ayhan Baser, D.; Kahveci, R.; Baydar Artantas, A.; Yasar, İ.; Aksoy, H.; Koc, E.M.; Kasim, İ.; Kunnamo, I.; Özkara, A. Exploring guideline adaptation strategy for Turkey: Is “ADAPTE” feasible or does it need adaptation as well? J. Eval. Clin. Pract. 2018, 24, 97–104. [Google Scholar] [CrossRef]
- Amer, Y.S.; Elzalabany, M.M.; Omar, T.I.; Ibrahim, A.G.; Dowidar, N.L. The ‘Adapted ADAPTE’: An approach to improve utilization of the ADAPTE guideline adaptation resource toolkit in the Alexandria Center for Evidence-Based Clinical Practice Guidelines. J. Eval. Clin. Pract. 2015, 21, 1095–1106. [Google Scholar] [CrossRef]
- Amer, Y.S.; Wahabi, H.A.; Elkheir, M.M.A.; Bawazeer, G.A.; Iqbal, S.M.; Titi, M.A.; Ekhzaimy, A.; Alswat, K.A.; Alzeidan, R.A.; Al-Ansary, L.A. Adapting evidence-based clinical practice guidelines at university teaching hospitals: A model for the Eastern Mediterranean Region. J. Eval. Clin. Pract. 2019, 25, 550–560. [Google Scholar] [CrossRef]
- Bashiri, F.A.; Albatti, T.H.; Hamad, M.H.; Al-Joudi, H.F.; Daghash, H.F.; Al-Salehi, S.M.; Varnham, J.L.; Alhaidar, F.; Almodayfer, O.; Alhossein, A.; et al. Adapting evidence-based clinical practice guidelines for people with attention deficit hyperactivity disorder in Saudi Arabia: Process and outputs of a national initiative. Child Adolesc. Psychiatry Ment. Health 2021, 15, 6. [Google Scholar] [CrossRef]
- Irajpour, A.; Hashemi, M.; Taleghani, F. Clinical practice guideline for end-of-life care in patients with cancer: A modified ADAPTE process. Support. Care Cancer 2022, 30, 2497–2505. [Google Scholar] [CrossRef]
- Hu, J.; Yu, L.; Jiang, L.; Yuan, W.; Bian, W.; Yang, Y.; Ruan, H. Developing a Guideline for Endotracheal Suctioning of Adults With Artificial Airways in the Perianesthesia Setting in China. J. PeriAnesthesia Nurs. 2019, 34, 160–168.e4. [Google Scholar] [CrossRef] [PubMed]
- The ADAPTE Collaboration. The ADAPTE Process: Resource Toolkit for Guideline Adaptation. Version 2.0: Guideline International Network. 2009. Available online: http://www.g-i-n.net (accessed on 26 June 2021).
- Bichsel, D.; Liechti, F.D.; Schlapbach, J.M.; Wertli, M.M. Cross-sectional analysis of recommendations for the treatment of hip and knee osteoarthritis in clinical guidelines. Arch. Phys. Med. Rehabil. 2021, 103, 559–569. [Google Scholar] [CrossRef]
- Feuerstein, J.D.; Pelsis, J.R.; Lloyd, S.; Cheifetz, A.S.; Stone, K.R. Systematic analysis of the quality of the scientific evidence and conflicts of interest in osteoarthritis of the hip and knee practice guidelines. Semin. Arthritis Rheum. 2016, 45, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Bierma-Zeinstra, S.; van Middelkoop, M.; Runhaar, J.; Schiphof, D. Nonpharmacological and nonsurgical approaches in OA. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101564. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Hanna, S.E.; Makarski, J.; et al. Development of the AGREE II, part 2: Assessment of validity of items and tools to support application. Can. Med. Assoc. J. 2010, 182, E472–E478. [Google Scholar] [CrossRef] [PubMed]
- AGREE Next Steps Consortium. The AGREE II Instrument [Electronic Version]. 2017. Available online: http://www.agreetrust.org (accessed on 3 July 2021).
- Tuncer, T.; Cay, F.H.; Altan, L.; Gurer, G.; Kacar, C.; Ozcakir, S.; Atik, S.; Ayhan, F.; Durmaz, B.; Eskiyurt, N.; et al. 2017 update of the Turkish League Against Rheumatism (TLAR) evidence-based recommendations for the management of knee osteoarthritis. Rheumatol. Int. 2018, 38, 1315–1331. [Google Scholar] [CrossRef]
- Osthoff, A.-K.R.; Niedermann, K.; Braun, J.; Adams, J.; Brodin, N.; Dagfinrud, H.; Duruoz, T.; Esbensen, B.A.; Günther, K.-P.; Hurkmans, E.; et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann. Rheum. Dis. 2018, 77, 1251–1260. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part one: Introduction, and mind-body exercise programs. Clin. Rehabil. 2017, 31, 582–595. [Google Scholar] [CrossRef]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part three: Aerobic exercise programs. Clin. Rehabil. 2017, 31, 612–624. [Google Scholar] [CrossRef]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: Strengthening exercise programs. Clin. Rehabil. 2017, 31, 596–611. [Google Scholar] [CrossRef]
- Brosseau, L.; Wells, G.A.; Pugh, A.G.; Smith, C.A.; Rahman, P.; Gallardo, I.C.Á.; Toupin-April, K.; Loew, L.; De Angelis, G.; Cavallo, S.; et al. Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercise in the management of hip osteoarthritis. Clin. Rehabil. 2016, 30, 935–946. [Google Scholar] [CrossRef]
- Rillo, O.; Riera, H.; Acosta, C.; Liendo, V.; Bolaños, J.; Monterola, L.; Nieto, E.; Arape, R.; Franco, L.M.; Vera, M.; et al. PANLAR Consensus Recommendations for the Management in Osteoarthritis of Hand, Hip, and Knee. Am. J. Clin. Oncol. 2016, 22, 345–354. [Google Scholar] [CrossRef]
- van Doormaal, M.C.; Meerhoff, G.A.; Vlieland, T.P.V.; Peter, W.F. A clinical practice guideline for physical therapy in patients with hip or knee osteoarthritis. Musculoskelet. Care 2020, 18, 575–595. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.; Bennell, K.; Austin, M.; Briggs, A.; Buchbinder, R.; Bunker, S.; Choong, P.; Ewald, D.; Fallon, K.; Harris, B.; et al. Guideline for the Management of Knee and Hip Osteoarthritis, 2nd ed.; with Consumer Summary; Royal Australian College of General Practitioners: Melbourne, Australia, 2018. Available online: https://www.racgp.org.au/getattachment/71ab5b77-afdf-4b01-90c3-04f61a910be6/Guideline-for-the-management-of-knee-and-hip-osteoarthritis.aspx (accessed on 3 January 2022).
- Cibulka, M.T.; Bloom, N.J.; Enseki, K.R.; Macdonald, C.W.; Woehrle, J.; McDonough, C.M. Hip Pain and Mobility Deficits—Hip Osteoarthritis: Revision 2017. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A37. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Hip Evidence-Based Clinical Practice Guideline; American Academy of Orthopaedic Surgeons: Rosemount, IL, USA, 2017; Available online: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-hip/oa-hip-cpg_6-11-19.pdf (accessed on 16 January 2022).
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Knee (Non-Arthroplasty) Evidence-Based Clinical Practice Guideline; American Academy of Orthopaedic Surgeons: Rosemount, IL, USA, 2021; Available online: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-knee/oak3cpg.pdf (accessed on 23 January 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Tittlemier, B.J.; Wittmeier, K.D.; Webber, S.C. Quality and content analysis of clinical practice guidelines which include nonpharmacological interventions for knee osteoarthritis. J. Eval. Clin. Pract. 2021, 27, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Ahamed, Y.; Jull, G.; Bryant, C.; Hunt, M.A.; Forbes, A.B.; Kasza, J.; Akram, M.; Metcalf, B.; Harris, A.; et al. Physical Therapist–Delivered Pain Coping Skills Training and Exercise for Knee Osteoarthritis: Randomized Controlled Trial. Arthritis Care Res. 2016, 68, 590–602. [Google Scholar] [CrossRef]
- Saffari, M.; Meybodi, M.K.E.; Sanaeinasab, H.; Karami, A.; Pakpour, A.H.; Koenig, H.G. A theory of planned behavior-based intervention to improve quality of life in patients with knee/hip osteoarthritis: A randomized controlled trial. Clin. Rheumatol. 2018, 37, 2505–2515. [Google Scholar] [CrossRef]
- Marconcin, P.; Espanha, M.; Teles, J.; Bento, P.; Campos, P.; André, R.; Yázigi, F. A randomized controlled trial of a combined self-management and exercise intervention for elderly people with osteoarthritis of the knee: The PLE2NO program. Clin. Rehabil. 2018, 32, 223–232. [Google Scholar] [CrossRef]
- Coleman, S.; Briffa, N.K.; Carroll, G.; Inderjeeth, C.; Cook, N.; McQuade, J. A randomised controlled trial of a self-management education program for osteoarthritis of the knee delivered by health care professionals. Arthritis Res. Ther. 2012, 14, R21. [Google Scholar] [CrossRef]
- Lim, Y.; Wong, J.; Hussain, S.M.; Estee, M.; Zolio, L.; Page, M.; Harrison, C.; Wluka, A.; Wang, Y.; Cicuttini, F. AB0979 Recommendations for weight management in osteoarthritis: A systematic review of clinical practice guidelines. Rheumatology 2022, 81 (Suppl. S1), 1616. [Google Scholar] [CrossRef]
- Hopayian, K.; Notley, C. A systematic review of low back pain and sciatica patients’ expectations and experiences of health care. Spine J. 2014, 14, 1769–1780. [Google Scholar] [CrossRef] [PubMed]
- Wong, V. Cultural influence on psychoeducation in Hong Kong. Int. Psychiatry 2010, 7, 20–22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schoeb, V. Healthcare Service in Hong Kong and its Challenges: The Role of Health Professionals within a Social Model of Health. China Perspect. 2016, 4, 51–58. [Google Scholar] [CrossRef]
- Chung, V.; Wong, E.; Woo, J.; Vi Lo, S.; Griffiths, S. Use of Traditional Chinese Medicine in the Hong Kong Special Administrative Region of China. J. Altern. Complement. Med. 2007, 13, 361–368. [Google Scholar] [CrossRef]
- Tsang, V.H.M.; Lo, P.H.W.; Lam, F.T.; Chung, L.S.W.; Tang, T.Y.; Lui, H.M.; Lau, J.T.G.; Yee, H.F.; Lun, Y.K.; Chan, H.T.; et al. Perception and use of complementary and alternative medicine for low back pain. J. Orthop. Surg. 2017, 25, 2309499017739480. [Google Scholar] [CrossRef] [PubMed]
- Fan, R. Which Care? Whose Responsibility? And Why Family? A Confucian Account of Long-Term Care for the Elderly. J. Med. Philos. A Forum Bioeth. Philos. Med. 2007, 32, 495–517. [Google Scholar] [CrossRef]
- Cycyk, L.M.; De Anda, S.; Moore, H.; Huerta, L. Cultural and Linguistic Adaptations of Early Language Interventions: Recommendations for Advancing Research and Practice. Am. J. Speech Lang. Pathol. 2021, 30, 1224–1246. [Google Scholar] [CrossRef]
- Ma, J.K.; Floegel, T.A.; Li, L.C.; Leese, J.; De Vera, M.A.; Beauchamp, M.R.; Taunton, J.; Liu-Ambrose, T.; Allen, K.D. Tailored physical activity behavior change interventions: Challenges and opportunities. Transl. Behav. Med. 2021, 11, 2174–2181. [Google Scholar] [CrossRef]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.-L.; Pomey, M.-P. Engaging patients to improve quality of care: A systematic review. Implement. Sci. 2018, 13, 98. [Google Scholar] [CrossRef]
- Hong Kong Physiotherapy Association. World Confederation for Physical Therapy. Available online: https://world.physio/membership/hong-kong (accessed on 24 October 2023).
- Hong Kong Physiotherapy Association. “Direct Access for Physiotherapy “The Blueprint” in Primary Healthcare”. 29 December 2022. Available online: https://www.hongkongpa.com.hk/notices/direct-access-for-physiotherapy-the-blueprint-in-primary-healthcare/ (accessed on 24 October 2023).
- South China Morning Post. “Staff Shortages in Hong Kong Threaten Quality of Care for Elderly”. 15 July 2015. Available online: www.scmp.com/news/hong-kong/health-environment/article/1839255/staff-shortages-hong-kong-threaten-quality-care (accessed on 24 October 2023).
- US Department of Health & Human Services, Agency for Healthcare Research and Quality. In “National Healthcare Disparities Report 2008”, Washington, 2008, Access to Healthcare; AHRQ Publication: Rockville, MD, USA, 2008; Chapter 3, No. 09-0002. Available online: https://archive.ahrq.gov/research/findings/nhqrdr/nhdr08/Chap3.html (accessed on 24 October 2023).
- Zadro, J.; O’keeffe, M.; Maher, C. Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open 2019, 9, e032329. [Google Scholar] [CrossRef]
- Zadro, J.R.; Ferreira, G. Has physical therapists’ management of musculoskeletal conditions improved over time? Braz. J. Phys. Ther. 2020, 24, 458–462. [Google Scholar] [CrossRef]
- Paci, M.; Faedda, G.; Ugolini, A.; Pellicciari, L. Barriers to evidence-based practice implementation in physiotherapy: A system-atic review and meta-analysis. Int. J. Qual. Health Care 2021, 33, mzab093. [Google Scholar] [CrossRef] [PubMed]
- Straus, S.E.; Sackett, D.L. Using research findings in clinical practice. BMJ 1998, 317, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, A.R.; Marshall, C.; Huckson, S.; James, R.; Moore, V. Developing a checklist for guideline implementation planning: Review and synthesis of guideline development and implementation advice. Implement. Sci. 2015, 10, 19. [Google Scholar] [CrossRef] [PubMed]
- Al Zoubi, F.; Wong, Y.L.; Cheing, G.; Cheung, J.P.Y.; Fu, S.N.; Tsang, H.; Law KY, R.; So, C.L.; Tsang, R.; Tsang, M.H.; et al. Management of hip and knee osteoarthritis: An adapted clinical practice guideline for Hong Kong physiotherapists. In Proceedings of the World Physiotherapy Asia Western Pacific Regional Congress, Hong Kong, China, 18–20 June 2022. [Google Scholar]
- Darzi, A.; Abou-Jaoude, E.A.; Agarwal, A.; Lakis, C.; Wiercioch, W.; Santesso, N.; Brax, H.; El-Jardali, F.; Schünemann, H.J.; Akl, E.A. A methodological survey identified eight proposed frameworks for the adaptation of health related guidelines. J. Clin. Epidemiol. 2017, 86, 3–10. [Google Scholar] [CrossRef]
- Kimaro, H.C. Strategies for Developing Human Resource Capacity to Support Sustainability of ICT Based Health Information Systems: A Case Study from Tanzania. Electron. J. Inf. Syst. Dev. Ctries. 2006, 26, 1–23. [Google Scholar] [CrossRef]
- Dizon, J.M.; Machingaidze, S.; Grimmer, K. To adopt, to adapt, or to contextualise? The big question in clinical practice guide-line development. BMC Res. Notes 2016, 9, 442. [Google Scholar] [CrossRef]
- Alper, B.S.; Tristan, M.; Ramirez-Morera, A.; Vreugdenhil, M.M.; Van Zuuren, E.J.; Fedorowicz, Z. RAPADAPTE for rapid guideline development: High-quality clinical guidelines can be rapidly developed with limited resources. Int. J. Qual. Health Care 2016, 28, 268–274. [Google Scholar] [CrossRef]
- Florez, I.D.; Brouwers, M.C.; Kerkvliet, K.; Spithoff, K.; Alonso-Coello, P.; Burgers, J.; Cluzeau, F.; Férvers, B.; Graham, I.; Grimshaw, J.; et al. Assessment of the quality of recom-mendations from 161 clinical practice guidelines using the Appraisal of Guidelines for Research and Evaluation–Recommendations Excellence (AGREE-REX) instrument shows there is room for improvement. Implement. Sci. 2020, 15, 79. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).